Cerebral cortex and lobes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cerebral cortex and lobes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cerebral cortex and lobes US Medical PG Question 1: A 52-year-man is brought to the physician because of a 2-week history of memory loss. Three weeks ago, he had a cardiac arrest that required cardiopulmonary resuscitation and intravenous epinephrine. On mental status examination, he cannot recall objects shown to him 20 minutes earlier but vividly recalls memories from before the incident. The remainder of the examination shows no abnormalities. Which of the following structures of the brain is most likely affected?
- A. Internal pyramidal layer of the amygdala
- B. Microglial cells of dorsal midbrain
- C. Purkinje cells of the cerebellum
- D. Pyramidal cells of the hippocampus (Correct Answer)
- E. Astroglial cells of the putamen
Cerebral cortex and lobes Explanation: ***Pyramidal cells of the hippocampus***
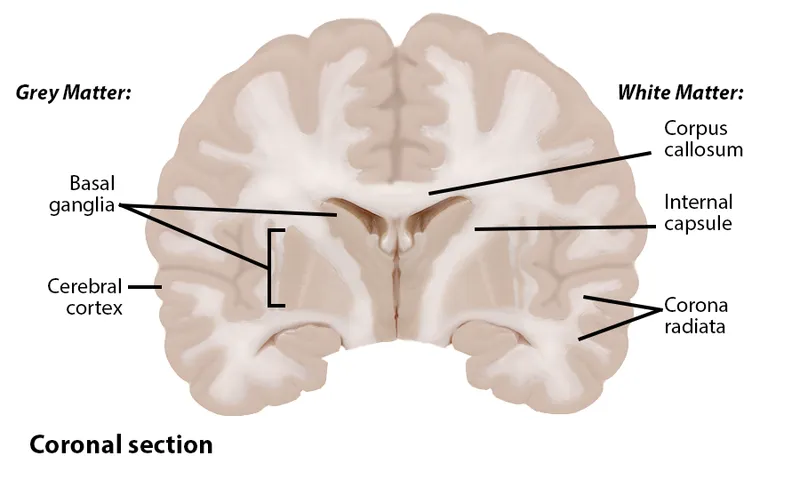
- The patient's inability to form new memories (anterograde amnesia) following a period of **hypoxia** suggests damage to the **hippocampus**, specifically its pyramidal cells.
- The **hippocampus** is highly vulnerable to **ischemic injury** due to the metabolic demands of its pyramidal cells.
*Internal pyramidal layer of the amygdala*
- The amygdala is primarily involved in **emotional processing**, particularly fear and anxiety, not memory encoding directly.
- Damage to the amygdala would likely manifest as altered emotional responses, rather than isolated memory loss.
*Microglial cells of dorsal midbrain*
- Microglial cells are the brain's resident immune cells and proliferate in response to injury, they are not the primary site of memory formation.
- The dorsal midbrain contains structures involved in visual and auditory reflexes, not directly memory consolidation.
*Purkinje cells of the cerebellum*
- Purkinje cells are specialized neurons in the **cerebellum** responsible for **motor coordination** and balance.
- Damage to these cells would result in ataxia and motor dysfunction, not memory deficits.
*Astroglial cells of the putamen*
- Astroglial cells are supportive cells throughout the brain; the putamen is involved in **motor control** and **procedural learning**.
- Dysfunction of the putamen typically leads to movement disorders like Parkinsonism, not specific memory loss.
Cerebral cortex and lobes US Medical PG Question 2: A 61-year-old man is brought to the emergency room with slurred speech. According to the patient's wife, they were watching a movie together when he developed a minor headache. He soon developed difficulty speaking in complete sentences, at which point she decided to take him to the emergency room. His past medical history is notable for hypertension and hyperlipidemia. He takes aspirin, lisinopril, rosuvastatin. The patient is a retired lawyer. He has a 25-pack-year smoking history and drinks 4-5 beers per day. His father died of a myocardial infarction, and his mother died of breast cancer. His temperature is 98.6°F (37°C), blood pressure is 143/81 mmHg, pulse is 88/min, and respirations are 21/min. On exam, he can understand everything that is being said to him and is able to repeat statements without difficulty. However, when asked to speak freely, he hesitates with every word and takes 30 seconds to finish a short sentence. This patient most likely has an infarct in which of the following vascular distributions?
- A. Proximal middle cerebral artery
- B. Inferior division of the middle cerebral artery
- C. Middle cerebral artery and posterior cerebral artery watershed area
- D. Superior division of the middle cerebral artery (Correct Answer)
- E. Anterior cerebral artery and middle cerebral artery watershed area
Cerebral cortex and lobes Explanation: ***Superior division of the middle cerebral artery***
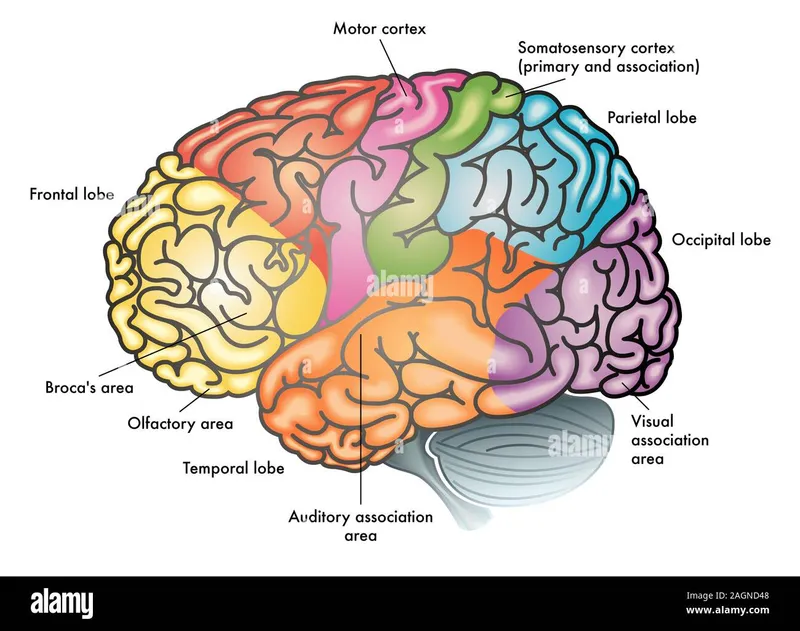
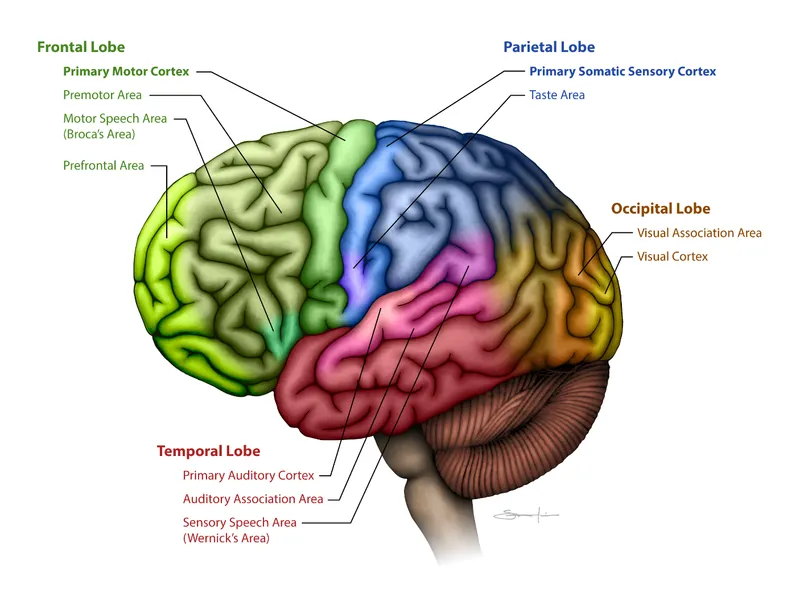
- The patient's inability to speak spontaneously coupled with intact comprehension and repetition is characteristic of **Broca's aphasia**, which results from damage to **Broca's area** in the dominant frontal lobe.
- Broca's area is supplied by the **superior division of the middle cerebral artery (MCA)**.
*Proximal middle cerebral artery*
- An infarct in the proximal MCA, or the main stem, would typically lead to global aphasia if the dominant hemisphere is affected, characterized by **severe deficits in comprehension, repetition, and speech production**.
- This presentation does not align with the patient's ability to understand and repeat statements.
*Inferior division of the middle cerebral artery*
- The inferior division of the MCA supplies Wernicke's area in the dominant hemisphere.
- Damage here causes **Wernicke's aphasia**, characterized by **fluent but nonsensical speech** with **impaired comprehension** and **repetition**, which is contrary to the patient's symptoms.
*Middle cerebral artery and posterior cerebral artery watershed area*
- Watershed infarcts, especially between the MCA and posterior cerebral artery (PCA), can cause **transcortical sensory aphasia** if in the dominant hemisphere.
- This type of aphasia involves impaired comprehension but **intact repetition**, which differs from Broca's aphasia where spontaneous speech is the main deficit.
*Anterior cerebral artery and middle cerebral artery watershed area*
- Infarcts in the watershed area between the anterior cerebral artery (ACA) and MCA can result in **transcortical motor aphasia** if in the dominant hemisphere.
- This condition presents with **non-fluent speech** and **intact repetition**, similar to Broca's aphasia, but Broca's area itself is located specifically within the MCA superior division territory.
Cerebral cortex and lobes US Medical PG Question 3: A 60-year-old man is brought to the emergency department by police officers because he was acting strangely in public. The patient was found talking nonsensically to characters on cereal boxes in the store. Past medical history is significant for multiple hospitalizations for alcohol-related injuries and seizures. The patient’s vital signs are within normal limits. Physical examination shows a disheveled male who is oriented to person, but not time or place. Neurologic examination shows nystagmus and severe gait ataxia. A T1/T2 MRI is performed and demonstrates evidence of damage to the mammillary bodies. The patient is given the appropriate treatment for recovering most of his cognitive functions. However, significant short-term memory deficits persist. The patient remembers events from his past such as the school and college he attended, his current job, and the names of family members quite well. Which of the following is the most likely diagnosis in this patient?
- A. Schizophrenia
- B. Korsakoff's syndrome (Correct Answer)
- C. Wernicke encephalopathy
- D. Delirium
- E. Delirium tremens
Cerebral cortex and lobes Explanation: ***Korsakoff's syndrome***
- The patient's history of **chronic alcohol abuse**, along with **gait ataxia**, **nystagmus**, and most notably, significant **anterograde amnesia** (inability to form new long-term memories) despite preserved remote memory, points to Korsakoff's syndrome.
- **Damage to the mammillary bodies** on MRI is a classic finding in Korsakoff's syndrome, a direct result of **thiamine deficiency**.
- The patient demonstrates the characteristic pattern: **impaired new memory formation** while retaining memories from his past (school, college, job, family names).
*Schizophrenia*
- Schizophrenia typically presents with **hallucinations and delusions** (e.g., talking to cereal box characters), but it is not commonly associated with physical signs like **nystagmus** or **gait ataxia**, nor with MRI findings of mammillary body damage.
- While the initial presentation of talking to cereal box characters might suggest psychosis, the complete clinical picture, especially the neurological deficits and persistent memory impairment, points away from schizophrenia as the primary diagnosis.
*Wernicke encephalopathy*
- Wernicke encephalopathy shares symptoms like **nystagmus** and **ataxia** with this patient and is also due to **thiamine deficiency** in alcoholics.
- However, Wernicke encephalopathy typically presents with more acute and severe symptoms, including **global confusion** and **ophthalmoplegia**, and represents the acute phase. The dominant chronic **anterograde amnesia** described here is characteristic of Korsakoff's syndrome, which represents the chronic sequela.
*Delirium*
- Delirium is characterized by an **acute disturbance in attention and cognition**, often with a fluctuating course, and can be seen in alcohol withdrawal.
- While the patient shows some disorientation, the chronic nature of the symptoms, the specific neurological deficits (nystagmus, ataxia), and particularly the persistent, isolated **anterograde amnesia** are not typical features of delirium.
*Delirium tremens*
- Delirium tremens is a severe form of **alcohol withdrawal** characterized by **autonomic hyperactivity**, severe delirium, hallucinations, and seizures.
- While the patient has a history of alcohol-related seizures, his current vital signs are normal, and the persistent, chronic memory deficits and specific MRI findings are not hallmarks of acute delirium tremens but rather a chronic neurological complication.
Cerebral cortex and lobes US Medical PG Question 4: A 67-year-old female patient is brought to the emergency department after her daughter noticed she has been having meaningless speech. When assessing the patient, she calls the chair a table, and at times would make up new words. She does not appear to be aware of her deficit, and is carrying on an empty conversation. Her speech is fluent, but with paraphasic errors. Her repetition is impaired. On physical examination, a right upper quadrant field-cut is appreciated, with impairment in comprehension and repetition. Which of the following structures is most likely involved in this patient’s presentation?
- A. Superior temporal gyrus (Correct Answer)
- B. Arcuate fasciculus
- C. Inferior frontal gyrus
- D. Frontal lobe, sparing Brodmann's area 44 and 45
- E. Arcuate fasciculus, inferior frontal gyrus, and superior temporal gyrus
Cerebral cortex and lobes Explanation: ***Superior temporal gyrus***
- The patient's presentation of **fluent aphasia** with **paraphasic errors**, **impaired comprehension**, **impaired repetition**, and **lack of awareness** of the deficit is classic for **Wernicke's aphasia**.
- **Wernicke's area**, located in the posterior part of the **superior temporal gyrus** (Brodmann area 22) in the dominant hemisphere, is responsible for language comprehension.
*Arcuate fasciculus*
- Damage to the **arcuate fasciculus** typically causes **conduction aphasia**, characterized by **impaired repetition** with relatively preserved comprehension and fluent speech.
- However, it does not explain the significant comprehension deficits and paraphasic errors seen in this patient to the same extent as a Wernicke's lesion.
*Inferior frontal gyrus*
- The **inferior frontal gyrus** (Brodmann areas 44 and 45) is commonly associated with **Broca's area**, responsible for language production.
- Damage here would result in **non-fluent aphasia** with effortful speech and relatively preserved comprehension, which is contrary to the patient's fluent speech.
*Frontal lobe, sparing Brodmann's area 44 and 45*
- While damage to other parts of the **frontal lobe** can cause various cognitive deficits, sparing Broca's area (44 and 45) would generally not result in the specific pattern of **fluent aphasia** with severe comprehension and repetition impairment seen here.
- This option does not precisely localize the critical language areas affected.
*Arcuate fasciculus, inferior frontal gyrus, and superior temporal gyrus*
- While damage to all these areas would certainly cause severe aphasia, the specific constellation of symptoms—**fluent speech**, **poor comprehension**, **poor repetition**, and **paraphasic errors**—points most directly and primarily to involvement of the **superior temporal gyrus** (Wernicke's area).
- While some level of repetition impairment (seen in Wernicke's aphasia) implies some involvement in the broader language network, a lesion centered in the superior temporal gyrus is the most parsimonious explanation for this classic presentation.
Cerebral cortex and lobes US Medical PG Question 5: A 67-year-old man is brought to the physician by his daughter because he frequently misplaces his personal belongings and becomes easily confused. His daughter mentions that his symptoms have progressively worsened for the past one year. On mental status examination, he is oriented to person, place, and time. He vividly recalls memories from his childhood but can only recall one of three objects presented to him after 5 minutes. His affect is normal. This patients' symptoms are most likely caused by damage to which of the following?
- A. Amygdala
- B. Superior temporal gyrus
- C. Hippocampus (Correct Answer)
- D. Ventral posterolateral nucleus
- E. Substantia nigra
Cerebral cortex and lobes Explanation: ***Hippocampus***
- The patient's inability to recall new information (only one of three objects after 5 minutes) despite intact long-term memory suggests **anterograde amnesia**, which is characteristic of hippocampal damage.
- The hippocampus is crucial for the **formation of new declarative memories**, such as facts and events. Progressive decline in this function over a year is consistent with neurodegenerative conditions affecting the hippocampus, such as **Alzheimer's disease**.
*Amygdala*
- The amygdala is primarily involved in **processing emotions** and fear, as well as emotional memory.
- Damage to the amygdala would typically manifest as deficits in recognizing or expressing emotions, or in forming emotional memories, which are not the primary symptoms described here.
*Superior temporal gyrus*
- The superior temporal gyrus contains the **primary auditory cortex** and is involved in processing auditory information and language comprehension (Wernicke's area).
- Damage to this area would primarily cause auditory processing difficulties, such as **Wernicke's aphasia**, rather than memory problems for new information.
*Ventral posterolateral nucleus*
- The ventral posterolateral (VPL) nucleus of the thalamus is a key relay station for **somatosensory information** (touch, pain, temperature) from the body to the cerebral cortex.
- Damage to the VPL nucleus would lead to sensory deficits on the contralateral side of the body, not issues with memory formation.
*Substantia nigra*
- The substantia nigra is part of the basal ganglia and is crucial for **motor control**, producing dopamine that projects to the striatum.
- Damage to the substantia nigra is characteristic of **Parkinson's disease**, leading to motor symptoms like tremor, rigidity, bradykinesia, and postural instability, which are not described in this patient.
Cerebral cortex and lobes US Medical PG Question 6: A 54-year-old man with hypertension and congenital blindness comes to the physician because he is unable to recognize objects by touch with his right hand. The symptoms started about 2 hours ago. When given a house key, he can feel the object in his right hand but is not able to identify what it is. This patient's condition is most likely caused by a lesion in which of the following locations?
- A. Ipsilateral cingulate gyrus
- B. Contralateral superior parietal lobule (Correct Answer)
- C. Ipsilateral inferior frontal gyrus
- D. Ipsilateral superior temporal gyrus
- E. Contralateral precentral gyrus
Cerebral cortex and lobes Explanation: ***Contralateral superior parietal lobule***
- The patient exhibits **astereognosis**, which is the inability to recognize objects by touch despite intact sensation, suggesting a lesion in the **parietal association cortex**.
- Since the deficit is in the **right hand**, the lesion must be on the **contralateral side**, which is the left superior parietal lobule.
*Ipsilateral cingulate gyrus*
- The **cingulate gyrus** is primarily involved in emotion, learning, and memory, and a lesion here would not typically cause isolated astereognosis.
- Furthermore, astereognosis with the right hand implies a contralateral lesion, not an ipsilateral one.
*Ipsilateral inferior frontal gyrus*
- The **inferior frontal gyrus** (Broca's area) is crucial for speech production; damage here usually results in **expressive aphasia**.
- A lesion in this area would not explain the patient's specific difficulty with tactile object recognition in the right hand.
*Ipsilateral superior temporal gyrus*
- The **superior temporal gyrus** (Wernicke's area) is concerned with language comprehension; damage typically causes **receptive aphasia**.
- This location is not associated with astereognosis, nor would an ipsilateral lesion explain a right-hand deficit.
*Contralateral precentral gyrus*
- The **precentral gyrus** is the primary motor cortex; a lesion here would cause **motor deficits** such as weakness or paralysis of the contralateral side, not an inability to recognize objects by touch while sensation is intact.
- The patient can feel the object, indicating intact sensation and motor function, merely difficulty identifying it.
Cerebral cortex and lobes US Medical PG Question 7: A 75-year-old woman presents with sudden loss of vision. She says that she was reading when suddenly she was not able to see the print on half of the page. Her symptoms started 4 hours ago and are accompanied by a severe posterior headache. Vital signs reveal the following: blood pressure 119/76 mm Hg, pulse 89/min, SpO2 98% on room air. The patient was unable to recognize her niece when she arrived to see her. A noncontrast CT of the head shows no evidence of hemorrhagic stroke. What is the most likely diagnosis in this patient?
- A. Lacunar stroke
- B. Middle cerebral artery stroke
- C. Vertebrobasilar stroke
- D. Subarachnoid hemorrhage
- E. Posterior cerebral artery stroke (Correct Answer)
Cerebral cortex and lobes Explanation: ***Posterior cerebral artery stroke***
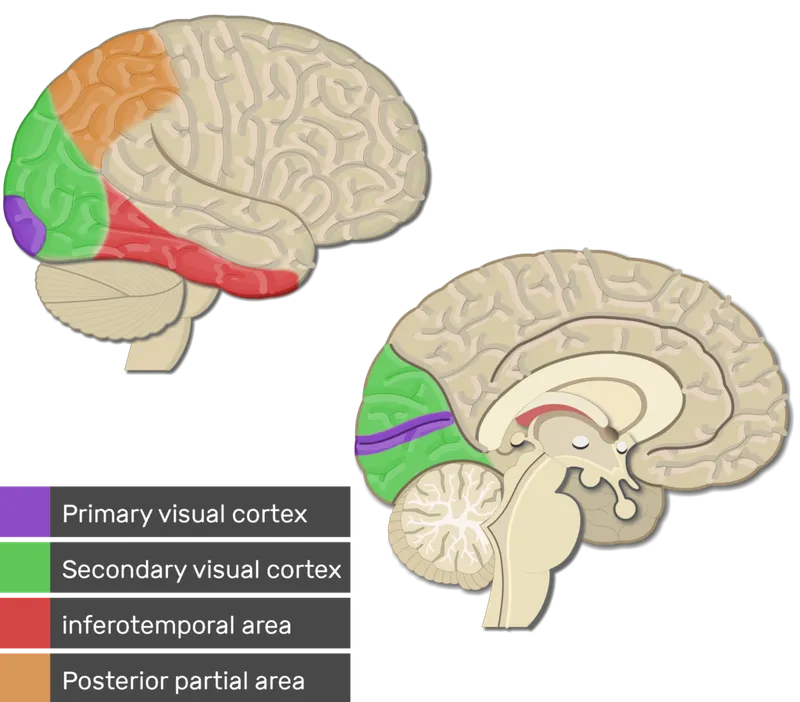
- The sudden severe posterior headache along with **unilateral vision loss** and **prosopagnosia** (inability to recognize familiar faces) are characteristic signs of a **posterior cerebral artery (PCA) stroke**.
- PCA occlusion often affects the **occipital lobe** (vision) and can extend to the **temporal lobe** (facial recognition).
*Lacunar stroke*
- This type of stroke results from the occlusion of small penetrating arteries and typically causes **pure motor** or **pure sensory deficits**, not complex visual or recognition problems.
- While headache can occur, the specific combination of symptoms points away from a lacunar infarct.
*Middle cerebral artery stroke*
- MCA stroke commonly presents with **contralateral hemiparesis**, **aphasia** (if dominant hemisphere), and **hemianopia** but usually not isolated unilateral vision loss or severe posterior headache with prosopagnosia.
- The symptoms are more consistent with involvement of the posterior circulation.
*Vertebrobasilar stroke*
- A vertebrobasilar stroke can cause **visual disturbances**, but it is typically associated with other **brainstem symptoms** like vertigo, ataxia, or cranial nerve deficits, which are not described here.
- The specific presentation of unilateral vision loss and prosopagnosia is less typical for a vertebrobasilar stroke affecting widespread brainstem structures.
*Subarachnoid hemorrhage*
- While a **sudden severe headache (thunderclap headache)** is a hallmark of SAH, it usually presents with meningeal irritation symptoms like **neck stiffness** and often altered mental status, and the visual deficits are usually different (e.g., oculomotor nerve palsy).
- The patient's focal neurological deficits, specifically prosopagnosia and unilateral visual field loss, are more indicative of an ischemic event in a specific vascular territory.
Cerebral cortex and lobes US Medical PG Question 8: Fibers from the marked structure terminate at which of the following?
- A. Red nucleus (Correct Answer)
- B. Subthalamus
- C. Inferior olivary nucleus
- D. Fastigial nucleus
Cerebral cortex and lobes Explanation: ***Red nucleus***
- The arrow points to the **superior cerebellar peduncle**, which contains efferent fibers from the **dentate nucleus** of the cerebellum.
- A major projection of the superior cerebellar peduncle is to the **contralateral red nucleus**, forming part of the **dentato-rubro-thalamic pathway**.
*Subthalamus*
- The subthalamus is part of the **diencephalon** and is involved in motor control as part of the **basal ganglia circuit**.
- It does not receive direct efferent projections from the cerebellum via the superior cerebellar peduncle.
*Inferior olivary nucleus*
- The inferior olivary nucleus is a major source of **climbing fibers** to the cerebellum, providing **afferent input** for motor learning and coordination.
- It does not receive direct efferent output from the cerebellum's deep nuclei via the superior cerebellar peduncle.
*Fastigial nucleus*
- The fastigial nucleus is one of the **deep cerebellar nuclei**, located medially.
- Its primary efferent projections are via the **inferior cerebellar peduncle** to the vestibular nuclei and reticular formation, not typically receiving fibers from the superior cerebellar peduncle.
Cerebral cortex and lobes US Medical PG Question 9: A 75-year-old woman is brought to the physician by her daughter for a 4-month history of increasing difficulty recognizing her friends and family. She has had to rely on recognizing haircuts, gait, and voices because she cannot remember their faces. Neurologic examination shows that she is able to recognize objects and name facial features such as the eyes and nose. On mental status examination, she is alert and has no deficits in cognition or short-term memory. An MRI of her head shows an inhomogeneous 2-cm mass with perifocal edema in her brain. Which of the following brain regions is most likely affected?
- A. Right posterior superior temporal cortex
- B. Right superior parietal cortex
- C. Right ventral occipitotemporal cortex (Correct Answer)
- D. Left posterior parietal cortex
- E. Left hippocampus
Cerebral cortex and lobes Explanation: ***Right ventral occipitotemporal cortex***
- The inability to recognize familiar faces, despite being able to identify facial features and objects, is characteristic of **prosopagnosia**.
- **Prosopagnosia** is most commonly associated with damage to the **fusiform gyrus**, located in the right ventral occipitotemporal cortex, also known as the fusiform face area.
*Right posterior superior temporal cortex*
- This region is primarily involved in **auditory processing** and **language comprehension** (Wernicke's area in the dominant hemisphere), not facial recognition.
- Damage here might lead to **auditory agnosia** or receptive aphasia, which are not described.
*Right superior parietal cortex*
- The superior parietal cortex is involved in **spatial awareness**, **attention**, and integrating sensory information.
- Lesions here could cause **neglect syndromes** or difficulties with spatial tasks, not specific facial recognition deficits.
*Left posterior parietal cortex*
- The left posterior parietal cortex plays a role in **praxis**, **arithmetic**, and certain aspects of **language**.
- Damage to this area is often associated with Gerstmann syndrome (acalculia, agraphia, finger agnosia, left-right disorientation), which is not evident here.
*Left hippocampus*
- The hippocampus is crucial for **memory formation** and recall, particularly **episodic memory**.
- Lesions in this area would primarily result in **anterograde amnesia** or difficulties with new memory acquisition, not isolated facial recognition deficits.
Cerebral cortex and lobes US Medical PG Question 10: A 68-year-old man is brought to the emergency department by ambulance after he was found to be altered at home. Specifically, his wife says that he fell and was unable to get back up while walking to bed. When she approached him, she found that he was unable to move his left leg. His past medical history is significant for hypertension, atrial fibrillation, and diabetes. In addition, he has a 20-pack-year smoking history. On presentation, he is found to still have difficulty moving his left leg though motor function in his left arm is completely intact. The cause of this patient's symptoms most likely occurred in an artery supplying which of the following brain regions?
- A. Motor cortex (ACA) (Correct Answer)
- B. Cerebellum (PICA/SCA)
- C. Occipital cortex (PCA)
- D. Brainstem (Vertebrobasilar)
- E. Motor cortex (MCA)
Cerebral cortex and lobes Explanation: ***Motor cortex (ACA)***
- The patient's inability to move his **left leg** while his **left arm** remains intact points to an injury in the **right cerebral hemisphere** affecting the leg area of the motor cortex.
- The leg area of the **primary motor cortex** is primarily supplied by the **anterior cerebral artery (ACA)**, making an ACA stroke the most likely cause.
*Motor cortex (MCA)*
- The **middle cerebral artery (MCA)** primarily supplies the motor cortex areas responsible for the **face and arm**, not typically isolated leg weakness.
- If the MCA were affected, you would expect to see involvement of the face and/or arm on the contralateral side in addition to leg weakness.
*Brainstem (Vertebrobasilar)*
- A **brainstem stroke** would likely present with more widespread neurological deficits, including **cranial nerve palsies**, ataxia, or altered consciousness.
- Isolated contralateral leg weakness without arm involvement is not characteristic of a brainstem lesion.
*Cerebellum (PICA/SCA)*
- The **cerebellum** is primarily involved in **coordination and balance**, not direct motor strength.
- A cerebellar stroke would present with symptoms like **ataxia**, dysarthria, or nystagmus, not isolated paralysis.
*Occipital cortex (PCA)*
- The **occipital cortex** is primarily responsible for **vision**.
- A posterior cerebral artery (PCA) stroke would typically cause **visual field defects** (e.g., contralateral homonymous hemianopia) rather than motor weakness.
More Cerebral cortex and lobes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.