Cerebellum US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cerebellum. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cerebellum US Medical PG Question 1: A 67-year-old man presents to the emergency department for a headache. The patient states his symptoms started thirty minutes ago. He states he experienced a sudden and severe headache while painting his house, causing him to fall off the ladder and hit his head. He has also experienced two episodes of vomiting and difficulty walking since the fall. The patient has a past medical history of hypertension, obesity, and atrial fibrillation. His current medications include lisinopril, rivaroxaban, atorvastatin, and metformin. His temperature is 99.5°F (37.5°C), blood pressure is 150/105 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. On physical exam, the patient localizes his headache to the back of his head. Cardiac exam reveals a normal rate and rhythm. Pulmonary exam reveals minor bibasilar crackles. Neurological exam is notable for minor weakness of the muscles of facial expression. Examination of cranial nerve three reveals a notable nystagmus. Heel to shin exam is abnormal bilaterally. The patient's gait is notably ataxic. A non-contrast CT scan of the head is currently pending. Which of the following is the most likely diagnosis?
- A. Pontine hemorrhage
- B. Cerebellar hemorrhage (Correct Answer)
- C. Subarachnoid hemorrhage
- D. Thalamic hemorrhage
- E. Subdural hematoma
Cerebellum Explanation: ***Cerebellar hemorrhage***
- The sudden onset of a **severe headache**, localized to the back of the head, combined with **ataxia**, nystagmus, and minor facial weakness, in a patient on **anticoagulation** (rivaroxaban) for atrial fibrillation, strongly suggests a cerebellar hemorrhage.
- **Vomiting** and **difficulty walking** are common symptoms due to the cerebellar involvement and increased intracranial pressure.
*Pontine hemorrhage*
- Pontine hemorrhages typically present with **quadriplegia**, profound **coma**, and **pinpoint pupils**, which are not observed in this patient.
- While it can cause sudden headache and vomiting, the specific neurological deficits (ataxia, nystagmus, mild facial weakness) are less characteristic of a pontine lesion.
*Subarachnoid hemorrhage*
- Characterized by a **"thunderclap" headache** (sudden and severe), often described as the "worst headache of my life," and can cause focal neurological deficits depending on the location of rupture.
- While the sudden onset and severity fit, the specific cerebellar signs (**nystagmus**, **ataxia**, posterior headache) point more directly to a cerebellar lesion, and the fall causing head trauma suggests a hemorrhage within the brain parenchyma.
*Thalamic hemorrhage*
- Thalamic hemorrhages commonly present with **contralateral hemisensory loss**, hemiparesis, and sometimes pupillary abnormalities.
- The patient's presentation with prominent **ataxia**, nystagmus, and posterior headache is less typical for a thalamic hemorrhage.
*Subdural hematoma*
- Subdural hematomas usually result from **trauma** and can have a more **insidious onset** (especially chronic subdural hematomas in elderly or anticoagulated patients).
- While the fall might suggest this, the acute onset of severe headache and the specific neurological signs like **ataxia** and nystagmus are more indicative of an intraparenchymal hemorrhage (like cerebellar) rather than a subdural collection compressing the brain surface.
Cerebellum US Medical PG Question 2: A neurology resident sees a stroke patient on the wards. This 57-year-old man presented to the emergency department after sudden paralysis of his right side. He was started on tissue plasminogen activator within 4 hours, as his wife noticed the symptoms and immediately called 911. When the resident asks the patient how he is doing, he replies by saying that his apartment is on Main St. He does not seem to appropriately answer the questions being asked, but rather speaks off topic. He is able to repeat the word "fan." His consciousness is intact, and his muscle tone and reflexes are normal. Upon striking the lateral part of his sole, his big toe extends upward and the other toes fan out. Which of the following is the area most likely affected in his condition?
- A. Caudate nucleus
- B. Broca’s area
- C. Arcuate fasciculus
- D. Temporal lobe (Correct Answer)
- E. Cuneus gyrus
Cerebellum Explanation: ***Temporal lobe***
- The patient exhibits features of **Wernicke's aphasia**, characterized by **fluent but nonsensical speech** ("apartment is on Main St." when asked how he is), poor comprehension, and the ability to repeat words. **Wernicke's area**, responsible for language comprehension, is located in the **posterior part of the superior temporal gyrus**.
- **Sudden paralysis of the right side** indicates involvement of the left cerebral hemisphere (**contralateral motor cortex** lesion), while speech disturbances point to the dominant hemisphere, which is typically the **left temporal lobe**.
*Caudate nucleus*
- Lesions of the **caudate nucleus** are primarily associated with **movement disorders** (e.g., chorea) and **behavioral changes**, not typically with fluent aphasia as described.
- While it plays a role in cognitive functions, its direct involvement in the specific language deficits presented is less likely.
*Broca’s area*
- Damage to **Broca's area**, located in the **frontal lobe**, causes **Broca's aphasia**, characterized by **non-fluent, halting speech** with good comprehension and poor repetition.
- The patient's speech is **fluent**, though off-topic, which contrasts with the typical presentation of Broca's aphasia.
*Arcuate fasciculus*
- The **arcuate fasciculus** connects Broca's and Wernicke's areas, and damage to it typically causes **conduction aphasia**, characterized by **impaired repetition** despite fluent speech and good comprehension.
- While the patient has impaired comprehension, his ability to repeat "fan" makes conduction aphasia less likely than Wernicke's aphasia, where repetition can vary but comprehension is profoundly affected.
*Cuneus gyrus*
- The **cuneus gyrus** is located in the **occipital lobe** and is primarily involved in **visual processing**.
- Damage to this area would lead to **visual field deficits** (e.g., hemianopia) rather than the language and comprehension problems described.
Cerebellum US Medical PG Question 3: A 40-year-old man is brought to the emergency department after sustaining multiple lacerations during a bar fight. The patient’s wife says that he has been showing worsening aggression and has been involved in a lot of arguments and fights for the past 2 years. The patient has no significant past medical or psychiatric history and currently takes no medications. The patient cannot provide any relevant family history since he was adopted as an infant. His vitals are within normal limits. On physical examination, the patient looks apathetic and grimaces repeatedly. Suddenly, his arms start to swing by his side in an uncontrolled manner. Which area of the brain is most likely affected in this patient?
- A. Cerebral cortex
- B. Caudate nucleus (Correct Answer)
- C. Cerebellum
- D. Medulla oblongata
- E. Substantia nigra
Cerebellum Explanation: **Caudate nucleus**
- The patient exhibits features like **worsening aggression**, **apathy**, and **uncontrolled, sudden movements** of the limbs, which are characteristic of Huntington's disease, a condition primarily affecting the **caudate nucleus**.
- **Huntington's disease** is an autosomal dominant neurodegenerative disorder linked to a trinucleotide repeat expansion (CAG) on chromosome 4, leading to atrophy of the **caudate and putamen**.
*Cerebral cortex*
- While damage to the cerebral cortex can cause personality changes and motor deficits, the specific combination of **choreiform movements** and progressive cognitive/behavioral decline seen here is more indicative of a basal ganglia disorder like Huntington's.
- Cortical lesions more commonly present with **focal neurological deficits** such as hemiparesis, aphasia, or sensory loss, which are not the primary features described.
*Cerebellum*
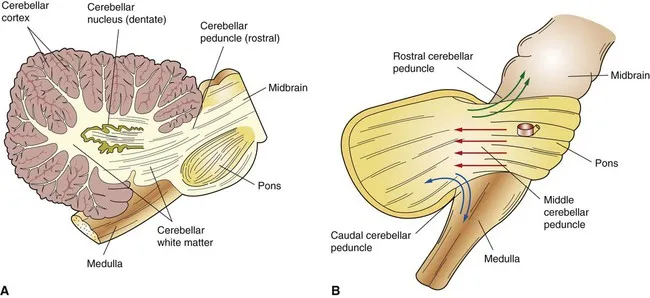
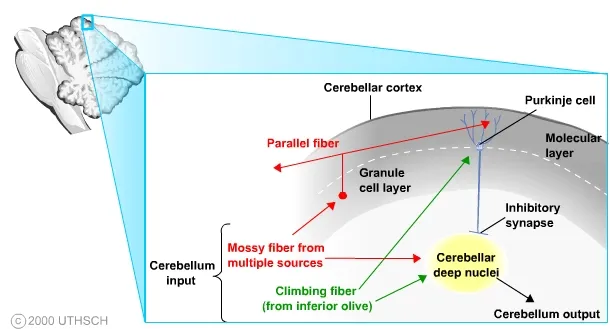
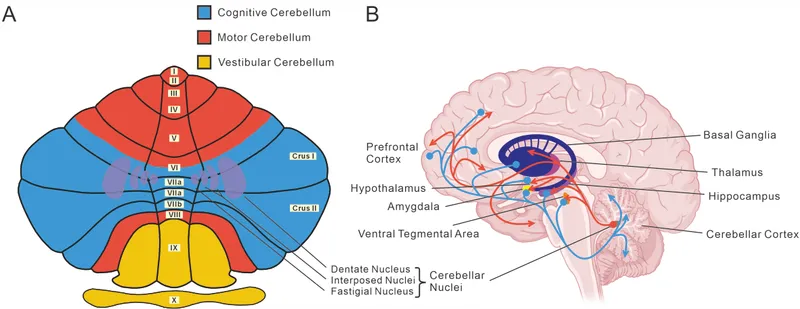
- Damage to the cerebellum typically results in **ataxia**, **dysmetria**, **intention tremor**, and problems with balance and coordination.
- The patient's **uncontrolled, sudden limb movements** are characteristic of chorea, not cerebellar dysfunction.
*Medulla oblongata*
- The medulla oblongata is crucial for vital autonomic functions such as **breathing, heart rate, and blood pressure regulation**.
- Lesions in this area would likely cause life-threatening symptoms, including **respiratory failure** or severe cardiovascular instability, which are not present in this patient.
*Substantia nigra*
- Damage or degeneration of the substantia nigra is primarily associated with **Parkinson's disease**, leading to symptoms like **bradykinesia**, **rigidity**, **resting tremor**, and **postural instability**.
- The patient's **hyperkinetic movements** (choreiform movements) are opposite to the hypokinetic presentation of Parkinson's disease.
Cerebellum US Medical PG Question 4: A 55-year-old man is brought to the emergency department by his wife after falling down. About 90 minutes ago, they were standing in their kitchen making lunch and chatting when he suddenly complained that he could not see as well, felt weak, and was getting dizzy. He began to lean to 1 side, and he eventually fell to the ground. He did not hit his head. In the emergency department, he is swaying while seated, generally leaning to the right. The general physical exam is unremarkable. The neurologic exam is notable for horizontal nystagmus, 3/5 strength in the right arm, ataxia of the right arm, and absent pinprick sensation in the left arm and left leg. The computed tomography (CT) scan of the head is unremarkable. Which of the following is the most likely single location of this patient's central nervous system lesion?
- A. Primary motor cortex
- B. Thalamus
- C. Lateral medulla (Correct Answer)
- D. Primary somatosensory cortex
- E. Anterior spinal cord
Cerebellum Explanation: ***Lateral medulla***
- The combination of **ipsilateral ataxia** and **weakness** (right arm) along with **contralateral pain and temperature sensory loss** (left arm and leg) is classic for a **lateral medullary syndrome (Wallenberg syndrome)**.
- **Horizontal nystagmus**, vertigo, and leaning to one side are also consistent with involvement of vestibular nuclei and cerebellar pathways in the lateral medulla.
*Primary motor cortex*
- A lesion here would cause **contralateral weakness or paralysis** but would not explain the ipsilateral ataxia, nystagmus, or contralateral pain and temperature loss.
- Sensory deficits would be minimal or absent, and would primarily affect discriminative touch.
*Thalamus*
- A thalamic lesion could cause **contralateral sensory loss** (affecting all modalities) and potentially some motor deficits or ataxia, but it typically does not cause **ipsilateral ataxia** or **nystagmus** in the pattern described.
- The specific combination of ipsilateral motor and contralateral sensory deficits points away from a pure thalamic lesion.
*Primary somatosensory cortex*
- A lesion in this area would primarily result in **contralateral deficits in discriminative touch, proprioception, and stereognosis**, not pain and temperature sensation.
- It would not explain the motor deficits, ataxia, or nystagmus seen in the patient.
*Anterior spinal cord*
- Damage to the anterior spinal cord (e.g., **anterior spinal artery syndrome**) would cause **bilateral motor weakness (paraplegia/quadriplegia)** and **bilateral loss of pain and temperature sensation** below the level of the lesion.
- It would not account for the nystagmus, vertigo, or the specific combination of ipsilateral and contralateral deficits observed in this patient, which are characteristic of brainstem involvement.
Cerebellum US Medical PG Question 5: An 82-year-old right-handed woman is brought in by ambulance after being found down in her home. On presentation, she is found to be awake but does not follow directions or respond to questions. She is able to speak and produces a fluent string of nonsensical words and sounds. She does not appear to be bothered by her deficits. Subsequent neurologic exam finds that the patient is unable to comprehend any instructions and is also unable to repeat phrases. CT scan reveals an acute stroke to her left hemisphere. Damage to which of the following structures would be most likely to result in this pattern of deficits?
- A. Precentral gyrus
- B. Superior temporal gyrus (Correct Answer)
- C. Arcuate fasciculus
- D. Inferior frontal gyrus
- E. Watershed zone
Cerebellum Explanation: ***Superior temporal gyrus***
- This patient presents with **fluent aphasia** (speaking nonsensical words), severely impaired **comprehension**, and impaired **repetition**. This triad is characteristic of **Wernicke's aphasia**.
- **Wernicke's area**, responsible for language comprehension, is located in the **posterior part of the superior temporal gyrus** in the dominant hemisphere (typically left).
*Precentral gyrus*
- The **precentral gyrus** contains the **primary motor cortex** and its damage would primarily cause contralateral motor deficits (e.g., **hemiparesis** or **hemiplegia**).
- This area is not directly involved in language comprehension or production of fluent but nonsensical speech.
*Arcuate fasciculus*
- Damage to the **arcuate fasciculus**, a white matter tract connecting Broca's and Wernicke's areas, results in **conduction aphasia**.
- In **conduction aphasia**, comprehension and fluency are relatively preserved, but **repetition is severely impaired**. This patient also has impaired comprehension.
*Inferior frontal gyrus*
- The **inferior frontal gyrus** houses **Broca's area**, which is responsible for **language production and motor aspects of speech**.
- Damage to this area typically causes **Broca's aphasia**, characterized by **non-fluent speech**, preserved comprehension, and impaired repetition. This patient has fluent speech.
*Watershed zone*
- **Watershed infarcts** occur at the borders between major arterial territories due to hypoperfusion, often leading to **transcortical aphasias**.
- While transcortical sensory aphasia involves impaired comprehension and fluent speech, **repetition is preserved**, which is not the case here.
Cerebellum US Medical PG Question 6: A 27-year-old man presents to a physician for evaluation of 3 months of increased vertigo. He says that occasionally he will experience several seconds of intense vertigo that makes him lose his balance. He came in for evaluation because this symptom is affecting his ability to drive to work. He has also been occasionally experiencing tinnitus. Physical exam reveals rotatory nystagmus that is delayed in onset and stops with visual fixation. The nerve that is most likely causing these symptoms exits the skull at which of the following locations?
- A. Internal auditory meatus (Correct Answer)
- B. Cribriform plate
- C. Foramen ovale
- D. Jugular foramen
- E. Foramen rotundum
Cerebellum Explanation: ***Internal auditory meatus***
- The symptoms described, particularly **vertigo** and **tinnitus**, are indicative of an issue with the **vestibulocochlear nerve (CN VIII)**.
- The **vestibulocochlear nerve** exits the skull through the **internal auditory meatus**, which is also the pathway for the **facial nerve (CN VII)**.
*Cribriform plate*
- The **cribriform plate** is associated with the passage of the **olfactory nerves (CN I)**, which are responsible for the sense of smell.
- Damage to this area would typically cause **anosmia**, not vertigo or tinnitus.
*Foramen ovale*
- The **foramen ovale** is the exit point for the **mandibular nerve (V3)**, a branch of the trigeminal nerve.
- Dysfunction here would lead to problems with **mastication** or altered sensation in the lower face, not vertigo.
*Jugular foramen*
- The **jugular foramen** transmits several cranial nerves: the **glossopharyngeal (CN IX)**, **vagus (CN X)**, and **accessory (CN XI)** nerves.
- Issues in this region would manifest as difficulties with **swallowing**, **speech**, or **shoulder/neck movement**, not balance or hearing.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, another branch of the trigeminal nerve.
- Damage to this nerve would primarily affect **sensation in the middle third of the face**, not balance or hearing.
Cerebellum US Medical PG Question 7: A man appearing to be in his mid-50s is brought in by ambulance after he was seen walking on railroad tracks. On further questioning, the patient does not recall being on railroad tracks and is only able to provide his name. Later on, he states that he is a railroad worker, but this is known to be false. On exam, his temperature is 99.9°F (37.7°C), blood pressure is 128/86 mmHg, pulse is 82/min, and respirations are 14/min. He appears disheveled, and his clothes smell of alcohol. The patient is alert, is only oriented to person, and is found to have abnormal eye movements and imbalanced gait when attempting to walk. Which of the following structures in the brain likely has the greatest reduction in the number of neurons?
- A. Mammillary bodies (Correct Answer)
- B. Cerebellar vermis
- C. Parietal-temporal cortex
- D. Frontal eye fields
- E. Basal ganglia
Cerebellum Explanation: ***Mammillary bodies***
- This patient presents with symptoms highly suggestive of **Wernicke-Korsakoff syndrome**, which includes **ophthalmoplegia** (abnormal eye movements), **ataxia** (imbalanced gait), and **confabulation** (making up stories, like being a railroad worker) with **anterograde amnesia** (not recalling being on railroad tracks).
- Wernicke-Korsakoff syndrome is primarily caused by **thiamine (vitamin B1) deficiency**, commonly seen in **chronic alcoholics**, and results in neuronal loss and necrosis, especially in the **mammillary bodies** and dorsomedial nucleus of the thalamus.
*Cerebellar vermis*
- While **alcoholism** can lead to cerebellar damage, particularly the **vermis**, causing **ataxia**, it does not fully explain the **memory deficits, confabulation, and ophthalmoplegia** seen in Wernicke-Korsakoff syndrome.
- Damage to the cerebellar vermis would primarily result in truncal ataxia and gait instability without the prominent amnesia and confabulation.
*Parietal-temporal cortex*
- Damage to the **parietal-temporal cortex** is associated with various cognitive deficits, including **aphasias** and **agnosias**, depending on the specific areas affected.
- While it can be affected by chronic alcoholism, it is not the primary site of damage in **Wernicke-Korsakoff syndrome** and does not typically present with the classic triad.
*Frontal eye fields*
- The **frontal eye fields** are involved in controlling **voluntary eye movements** and saccades. Damage here can cause specific patterns of gaze palsies.
- However, the abnormal eye movements seen in Wernicke-Korsakoff syndrome (e.g., nystagmus, ophthalmoplegia) are typically due to damage in brainstem nuclei and **mammillary bodies**, not primarily the frontal eye fields.
*Basal ganglia*
- The **basal ganglia** are primarily involved in motor control, learning, and executive functions. Damage to these structures can lead to **movement disorders** like Parkinsonism or Huntington's disease.
- While chronic alcoholism can have diffuse effects on the brain, the basal ganglia are not the primary site of pathology in **Wernicke-Korsakoff syndrome**, and damage here would not explain the memory and confabulation symptoms.
Cerebellum US Medical PG Question 8: At what age does maximum brain growth occur?
- A. 6 months (Correct Answer)
- B. 1 year
- C. 2 years
- D. 3 years
- E. 5 years
Cerebellum Explanation: ***6 months***
- **Brain growth** is most rapid during the early postnatal period, with the brain reaching almost **50% of its adult size by 6 months of age**.
- This period involves rapid **synaptogenesis** and myelination, crucial for early cognitive and motor development.
*1 year*
- While significant **brain growth** continues, the peak rate of increase in brain volume has typically passed by 1 year.
- At this age, the brain has reached approximately **75% of its adult size**.
*2 years*
- By 2 years, the brain is about **80% of its adult size**, indicating ongoing but slower growth compared to the first year.
- This period is more characterized by refinement of neural circuits rather than rapid volumetric expansion.
*3 years*
- At 3 years, the brain has attained around **90% of its adult size**, though important developmental changes continue.
- The rate of **neural development** at this stage largely focuses on strengthening existing connections and pruning less used ones.
*5 years*
- By 5 years, the brain has reached approximately **90-95% of its adult size**, with growth significantly slower than in earlier years.
- Development at this age focuses primarily on **synaptic pruning** and refinement of neural networks rather than volumetric growth.
Cerebellum US Medical PG Question 9: Arrange in sequence the structures involved in the direct pathway (1=Striatum, 2=GPi, 3=Thalamus, 4=Cortex output, 5=Cortex input):-
- A. 1,3,4,2,5
- B. 5,1,2,3,4 (Correct Answer)
- C. 1,2,3,4,5
- D. 5,4,2,3,1
- E. 5,1,3,2,4
Cerebellum Explanation: ***5,1,2,3,4***
- The direct pathway of the basal ganglia begins with the **cortex** (5) sending excitatory signals to the **striatum** (1).
- The striatum then inhibits the **internal globus pallidus (GPi)** (2), which disinhibits the **thalamus** (3), leading to excitation of the **cortex** (4).
- This is the correct sequence: **Cortex input → Striatum → GPi → Thalamus → Cortex output**.
*1,3,4,2,5*
- This sequence is incorrect as it starts with the striatum instead of cortical input.
- The direct pathway does not begin with striatal activity; the cortex must first activate the striatum.
*1,2,3,4,5*
- This order is incorrect because it implies the pathway starts at the striatum rather than the cortex.
- The cortex should be the starting point (5) and the ending point (4) of the motor loop.
*5,4,2,3,1*
- This sequence is incorrect as it places cortex output (4) before the striatum receives input.
- This reverses the functional flow and does not follow the **disinhibitory mechanism** of the direct pathway.
*5,1,3,2,4*
- This sequence incorrectly places the thalamus (3) before the GPi (2).
- In the direct pathway, the striatum must first inhibit the GPi before the thalamus can be disinhibited.
Cerebellum US Medical PG Question 10: A 12-year-old boy is brought to his primary care physician because he has been tripping and falling frequently over the past 2 months. He says that he feels like he loses his balance easily and finds it difficult to walk in tight spaces such as his school hallways. Furthermore, he says that he has been experiencing insomnia over the same time period. His past medical history is significant for some mild allergies, but otherwise he has been healthy. Physical exam reveals that his eyes are fixed downwards with nystagmus bilaterally. Which of the following structures is most likely affected by this patient's condition?
- A. Pineal gland (Correct Answer)
- B. Cerebellum
- C. Pituitary gland
- D. Thalamus
- E. 4th ventricle
Cerebellum Explanation: ***Pineal gland***
- This patient presents with the classic triad of **Parinaud syndrome** (dorsal midbrain syndrome): **downward gaze palsy** (eyes fixed downward), **bilateral nystagmus** (convergence-retraction type), and **ataxia**.
- Pineal region tumors (e.g., **germinoma**, **pineoblastoma**) compress the **tectal plate/superior colliculus** causing vertical gaze paralysis and pupillary light-near dissociation.
- **Insomnia** results from disruption of **melatonin production** by the pineal gland, which regulates circadian rhythms.
- **Ataxia** occurs secondary to **obstructive hydrocephalus** from compression of the **cerebral aqueduct** by the tumor.
- This is a **classic USMLE presentation** of a pineal region mass in a pediatric patient.
*Cerebellum*
- While cerebellar lesions cause **ataxia** and **nystagmus** (typically horizontal or rotatory), they do **NOT** cause **vertical gaze palsy** or downward fixation of eyes.
- Posterior fossa tumors like **medulloblastoma** present with coordination deficits but lack the characteristic **setting sun sign** (downward gaze) seen here.
- The combination of **downward gaze palsy + insomnia** specifically points away from isolated cerebellar pathology.
*Pituitary gland*
- Pituitary lesions primarily cause **endocrine abnormalities** (growth hormone deficiency, precocious puberty, diabetes insipidus) or **bitemporal hemianopsia** from optic chiasm compression.
- They do not typically cause **vertical gaze palsies** or the motor coordination deficits described.
*Thalamus*
- Thalamic lesions can cause **sensory deficits**, **movement disorders** (e.g., thalamic tremor), or **altered consciousness**.
- They do not cause the specific combination of **downward gaze palsy** and **insomnia** seen in this patient.
*4th ventricle*
- While **hydrocephalus** from 4th ventricle obstruction can cause headache, nausea, and papilledema, the ventricle itself is a **CSF-filled space** without neural tissue.
- The **specific downward gaze palsy** indicates tectal plate compression, which occurs with **pineal region masses**, not primary 4th ventricle pathology.
More Cerebellum US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.