Basal ganglia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Basal ganglia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Basal ganglia US Medical PG Question 1: A 38-year-old woman comes to the physician because of a 3-week history of involuntary movements of her extremities. One year ago, she was fired from her position as an elementary school teacher because she had stopped preparing lessons and was frequently absent without notice. She now lives with her mother. She appears emaciated and malodorous. Examination shows rapid, nonrepetitive jerks of her limbs and face that frequently end with the patient covering her face and yawning. She has an unsteady gait. Genetic testing shows a mutation on chromosome 4. This patient's condition is most likely associated with increased levels of which of the following substances?
- A. Gamma-aminobutyric acid
- B. N-acetyl aspartate
- C. Glutamate (Correct Answer)
- D. Dopamine
- E. Acetylcholine
Basal ganglia Explanation: ***Glutamate***
- **Huntington's disease** is characterized by **chorea, psychiatric symptoms, and cognitive decline**, caused by CAG repeat expansion on chromosome 4 producing abnormal huntingtin protein.
- The mutant huntingtin protein leads to **glutamate excitotoxicity** through multiple mechanisms: impaired glutamate reuptake, enhanced NMDA receptor sensitivity, and mitochondrial dysfunction.
- **Increased glutamatergic activity and extracellular glutamate levels** contribute to progressive neuronal death, particularly of GABAergic medium spiny neurons in the striatum.
- This glutamate-mediated excitotoxicity is the primary mechanism driving neurodegeneration in Huntington's disease.
*Gamma-aminobutyric acid (GABA)*
- GABAergic neurons in the striatum are preferentially lost in Huntington's disease, resulting in **decreased GABA levels**, not increased.
- The loss of GABAergic inhibition contributes to **disinhibition of motor pathways** and the characteristic choreiform movements.
*N-acetyl aspartate (NAA)*
- NAA is a neuronal marker that is **decreased** in neurodegenerative diseases like Huntington's, reflecting **neuronal loss and dysfunction**.
- Reduced NAA is seen on MR spectroscopy but does not cause the motor symptoms.
*Dopamine*
- While there is **relative dopamine hyperactivity** in the striatum due to loss of GABAergic inhibition, dopamine levels themselves are not necessarily increased.
- Dopamine-depleting agents (e.g., **tetrabenazine, deutetrabenazine**) are used therapeutically to reduce chorea by decreasing dopaminergic transmission.
*Acetylcholine*
- Acetylcholine levels are **not primarily elevated** in Huntington's disease pathophysiology.
- Cholinergic function may be affected in advanced disease contributing to cognitive symptoms, but this is not the primary mechanism of chorea.
Basal ganglia US Medical PG Question 2: A 74-year-old man is brought to the physician by his wife for progressively worsening confusion and forgetfulness. Vital signs are within normal limits. Physical examination shows a flat affect and impaired short-term memory. An MRI of the brain is shown. Further evaluation of this patient is most likely to show which of the following findings?
- A. Postural instability
- B. Pill-rolling tremor
- C. Choreiform movements
- D. Broad-based gait (Correct Answer)
- E. Papilledema
Basal ganglia Explanation: ***Broad-based gait***
- The patient's symptoms of **confusion**, **forgetfulness (dementia)**, and the MRI finding of **hydrocephalus** (dilated ventricles without sulcal effacement) are classic for **Normal Pressure Hydrocephalus (NPH)**.
- A hallmark triad of NPH includes **dementia**, **gait disturbance** (often described as broad-based or magnetic), and **urinary incontinence**.
*Postural instability*
- While patients with NPH can have **postural instability**, a more specific and prominent gait disturbance is typically observed.
- **Postural instability** is also a feature of many other neurological conditions, making it less specific than a broad-based gait for NPH.
*Pill-rolling tremor*
- A **pill-rolling tremor** is a characteristic feature of **Parkinson's disease**, which presents with a different constellation of symptoms, including bradykinesia and rigidity, and is not directly associated with hydrocephalus.
- This type of tremor is a **resting tremor** and is not typically seen in NPH.
*Choreiform movements*
- **Choreiform movements** are involuntary, brief, abrupt, and irregular movements, characteristic of conditions like **Huntington's disease**.
- These movements are not a typical manifestation of NPH, which primarily involves gait, cognition, and continence.
*Papilledema*
- **Papilledema** is swelling of the optic disc due to **increased intracranial pressure**.
- While hydrocephalus can cause increased intracranial pressure, NPH is characterized by **normal intracranial pressure**, hence papilledema is not expected.
Basal ganglia US Medical PG Question 3: A 73-year-old man presents to your office accompanied by his wife. He has been experiencing a tremor in his right hand for the last several months that seems to be worsening. He does not have any other complaints and says he’s “fine.” His wife thinks that he has also had more difficulty walking. His history is significant for hypertension and an ischemic stroke of the right middle cerebral artery 2 years ago. His medications include hydrochlorothiazide and daily aspirin. On physical exam you note that the patient speaks with a soft voice and has decreased facial expressions. He has a resting tremor that is worse on the right side. He has increased resistance to passive movement when you flex and extend his relaxed wrist. He has 5/5 strength bilaterally. Neuronal degeneration in which of the following locations is most likely responsible for the progression of this disease?
- A. Vermis
- B. Substantia nigra pars compacta (Correct Answer)
- C. Frontotemporal lobe
- D. Caudate and putamen
- E. Subthalamic nucleus
Basal ganglia Explanation: ***Substantia nigra pars compacta***
- The patient's symptoms, including **resting tremor**, **bradykinesia** (soft voice, decreased facial expressions, difficulty walking), and **rigidity** (increased resistance to passive movement), are classic signs of **Parkinson's disease**.
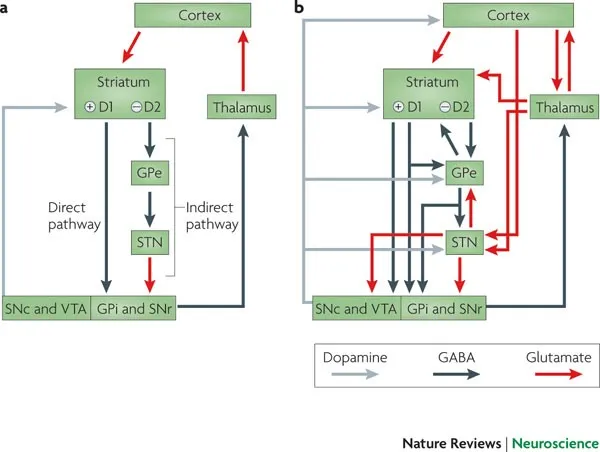
- Parkinson's disease is primarily caused by the degeneration of **dopaminergic neurons** in the **substantia nigra pars compacta**, leading to a lack of dopamine in the basal ganglia.
*Vermis*
- The **vermis** is a part of the cerebellum primarily involved in coordinating **truncal movements** and maintaining **posture**.
- Damage to the vermis typically causes **ataxia**, truncal instability, and gait disturbances, which are not the primary features described here.
*Frontotemporal lobe*
- The **frontotemporal lobe** is associated with cognitive functions, personality, and language.
- Degeneration in this area is characteristic of **frontotemporal dementia**, presenting with prominent behavioral changes, language difficulties, or progressive memory loss, which are not the main symptoms in this patient.
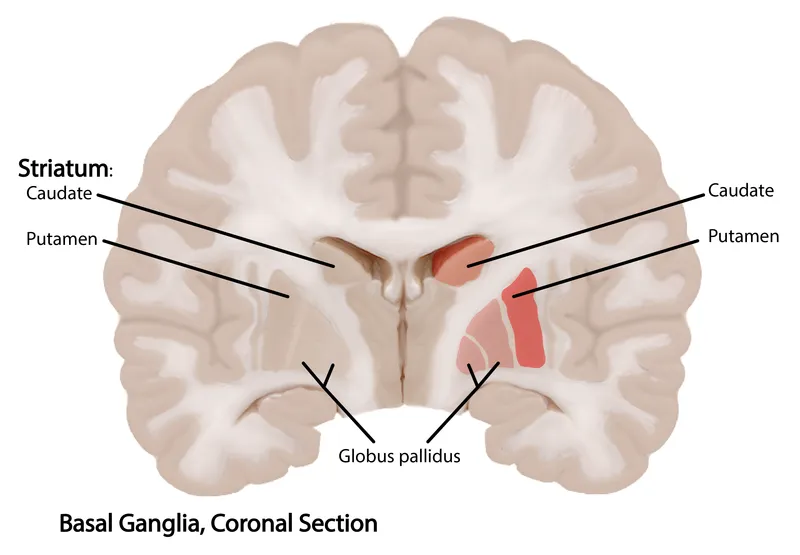
*Caudate and putamen*
- The **caudate and putamen** are components of the **striatum**, which receives dopaminergic input from the substantia nigra.
- While the lack of dopamine in the striatum contributes to Parkinsonian symptoms, the primary neuronal degeneration occurs *before* this in the substantia nigra pars compacta, which *projects* to the striatum.
*Subthalamic nucleus*
- The **subthalamic nucleus** is part of the basal ganglia circuit, and its overactivity can contribute to motor symptoms in Parkinson's disease.
- **Deep brain stimulation (DBS)** targeting the subthalamic nucleus is a treatment for Parkinson's, but the primary site of neuronal degeneration in the disease itself is not the subthalamic nucleus.
Basal ganglia US Medical PG Question 4: A 40-year-old man is brought to the emergency department after sustaining multiple lacerations during a bar fight. The patient’s wife says that he has been showing worsening aggression and has been involved in a lot of arguments and fights for the past 2 years. The patient has no significant past medical or psychiatric history and currently takes no medications. The patient cannot provide any relevant family history since he was adopted as an infant. His vitals are within normal limits. On physical examination, the patient looks apathetic and grimaces repeatedly. Suddenly, his arms start to swing by his side in an uncontrolled manner. Which area of the brain is most likely affected in this patient?
- A. Cerebral cortex
- B. Caudate nucleus (Correct Answer)
- C. Cerebellum
- D. Medulla oblongata
- E. Substantia nigra
Basal ganglia Explanation: **Caudate nucleus**
- The patient exhibits features like **worsening aggression**, **apathy**, and **uncontrolled, sudden movements** of the limbs, which are characteristic of Huntington's disease, a condition primarily affecting the **caudate nucleus**.
- **Huntington's disease** is an autosomal dominant neurodegenerative disorder linked to a trinucleotide repeat expansion (CAG) on chromosome 4, leading to atrophy of the **caudate and putamen**.
*Cerebral cortex*
- While damage to the cerebral cortex can cause personality changes and motor deficits, the specific combination of **choreiform movements** and progressive cognitive/behavioral decline seen here is more indicative of a basal ganglia disorder like Huntington's.
- Cortical lesions more commonly present with **focal neurological deficits** such as hemiparesis, aphasia, or sensory loss, which are not the primary features described.
*Cerebellum*
- Damage to the cerebellum typically results in **ataxia**, **dysmetria**, **intention tremor**, and problems with balance and coordination.
- The patient's **uncontrolled, sudden limb movements** are characteristic of chorea, not cerebellar dysfunction.
*Medulla oblongata*
- The medulla oblongata is crucial for vital autonomic functions such as **breathing, heart rate, and blood pressure regulation**.
- Lesions in this area would likely cause life-threatening symptoms, including **respiratory failure** or severe cardiovascular instability, which are not present in this patient.
*Substantia nigra*
- Damage or degeneration of the substantia nigra is primarily associated with **Parkinson's disease**, leading to symptoms like **bradykinesia**, **rigidity**, **resting tremor**, and **postural instability**.
- The patient's **hyperkinetic movements** (choreiform movements) are opposite to the hypokinetic presentation of Parkinson's disease.
Basal ganglia US Medical PG Question 5: A 22-year-old man is brought to the physician by his mother because of concerns about his recent behavior. Three months ago, the patient first reported hearing loud voices coming from the ceiling of his room. During this time, he has also become increasingly worried that visitors to the house were placing secret surveillance cameras. Mental status examination shows tangential speech with paranoid thoughts. Treatment for this patient's condition predominantly targets which of the following dopaminergic pathways?
- A. Mesocortical pathway
- B. Thalamocortical pathway
- C. Nigrostriatal pathway
- D. Corticostriatal pathway
- E. Mesolimbic pathway (Correct Answer)
Basal ganglia Explanation: ***Mesolimbic pathway***
- The patient's symptoms of **auditory hallucinations** and **paranoid delusions** are **positive symptoms** of psychosis consistent with **schizophrenia**.
- **Hyperactivity** of the **mesolimbic dopaminergic pathway** is strongly associated with the positive symptoms of schizophrenia, making it the primary target for antipsychotic treatment.
*Mesocortical pathway*
- The **mesocortical pathway** is primarily involved in **cognition, motivation, and executive functions**, originating from the ventral tegmental area and projecting to the prefrontal cortex.
- **Hypoactivity** in this pathway is thought to contribute to the **negative and cognitive symptoms** of schizophrenia, not the positive symptoms described.
*Thalamocortical pathway*
- The **thalamocortical pathway** connects the **thalamus to the cerebral cortex** and is crucial for sensory processing, arousal, and consciousness.
- While involved in neural circuits, it is not considered a primary dopaminergic pathway targeted for the treatment of positive psychotic symptoms.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** projects from the **substantia nigra to the striatum** and is primarily involved in **motor control**.
- Blocking dopamine receptors in this pathway by antipsychotic medications can cause **extrapyramidal symptoms (EPS)**, but it is not the main pathway responsible for positive psychotic symptoms or their treatment.
*Corticostriatal pathway*
- The **corticostriatal pathway** is **predominantly a glutamatergic pathway** connecting the **cerebral cortex to the striatum**, playing a role in motor control and habit formation.
- This is not a primary dopaminergic pathway and is not directly implicated in the positive symptoms of schizophrenia or their pharmacological treatment.
Basal ganglia US Medical PG Question 6: A 42-year-old woman is brought to the physician by her husband because of a 1-year history of abnormal behavior. During this time she has been irritable, restless, and has had multiple episodes of hearing voices. Over the past month, she has also had difficulty swallowing. She has a 2-year history of depression. She was let go by her employer 6 months ago because she could no longer handle all her tasks and often forgot about assignments. Her father committed suicide at the age of 50. The patient has smoked one pack of cigarettes daily over the past 20 years. She has a history of smoking cocaine for 8 years but stopped 1 year ago. Vital signs are within normal limits. On mental status examination, she is confused and oriented to person and place only. Neurologic examination shows a delayed return to neutral ankle position after triggering the plantar reflex. Physical examination shows irregular, nonrepetitive, and arrhythmic movements of the neck and head. The patient has poor articulation. Which of the following is the most likely diagnosis?
- A. Parkinson disease
- B. Multiple sclerosis
- C. Huntington disease (Correct Answer)
- D. Drug-induced chorea
- E. Sydenham chorea
Basal ganglia Explanation: ***Huntington disease***
- This patient presents with a classic triad of **motor dysfunction (chorea)**, **cognitive decline (dementia)**, and **psychiatric symptoms (irritability, restlessness, hallucinations, depression)**, which is highly characteristic of Huntington disease.
- The **family history of suicide** in her father at a relatively young age (50), along with the patient's early onset of symptoms (42 years old), suggests an autosomal dominant inheritance pattern typical of Huntington disease.
*Parkinson disease*
- Parkinson disease typically presents with **bradykinesia**, **rigidity**, **tremor at rest**, and **postural instability**, which are distinctly different from the choreiform movements described.
- While cognitive and psychiatric symptoms can occur, the prominent **chorea** and early onset of **dementia** are not typical primary features.
*Multiple sclerosis*
- Multiple sclerosis is characterized by **demyelination** in the central nervous system, leading to a variety of neurological symptoms that are often episodic, such as **visual disturbances**, **weakness**, **sensory deficits**, and **ataxia**.
- It does not typically present with the progressive chorea, cognitive decline, and psychiatric symptoms seen in this patient.
*Drug-induced chorea*
- Drug-induced chorea would typically manifest following the initiation or change in dose of certain medications, and usually resolves upon their discontinuation; this patient's chorea has been ongoing for a year without recent drug changes.
- While she has a history of cocaine use, she stopped 1 year ago, and the progressive nature of the symptoms, along with cognitive and psychiatric deterioration, points away from acute drug-induced effects.
*Sydenham chorea*
- Sydenham chorea is associated with **rheumatic fever** and typically presents in childhood or adolescence following a Group A streptococcal infection.
- The patient's age (42 years old) and the absence of other symptoms of rheumatic fever make Sydenham chorea unlikely.
Basal ganglia US Medical PG Question 7: A 80-year-old man is brought to the emergency department with complaints that he "can't control his left leg". His symptoms started a few hours ago. He was outside taking a walk with his wife when suddenly his leg shot out and kicked her. His past medical history is notable for diabetes, hypertension, and a myocardial infarction 5 years ago. He smokes 1-2 cigarettes/day. He does not use alcohol or illicit drugs. On exam, the patient has intermittent wide, flinging movements that affect his proximal left arm and left leg. Which of the following parts of his brain is most likely damaged?
- A. Ventral posterior thalamic nucleus
- B. Left internal capsule
- C. Right subthalamic nucleus (Correct Answer)
- D. Left subthalamic nucleus
- E. Right internal capsule
Basal ganglia Explanation: ***Right subthalamic nucleus***
- The patient's symptoms of sudden, uncontrolled, wide-flinging movements, affecting the contralateral (left) side of the body, are characteristic of **hemiballism**.
- **Hemiballism** is almost exclusively caused by a lesion in the **contralateral subthalamic nucleus (STN)**, or its afferent/efferent connections, most commonly due to a **lacunar infarct**.
*Ventral posterior thalamic nucleus*
- Damage to the **ventral posterior thalamic nucleus** primarily causes **sensory deficits**, such as loss of touch, pain, and temperature sensation, on the contralateral side of the body.
- While it can be involved in motor control, it does not typically cause the characteristic flinging movements seen in hemiballism.
*Left internal capsule*
- A lesion in the **left internal capsule** would result in contralateral (right-sided) motor and sensory deficits, including **hemiparesis** or **hemiplegia**, but not the ballistic, uncontrollable movements described.
- The internal capsule carries major motor and sensory pathways to and from the cerebral cortex.
*Left subthalamic nucleus*
- Damage to the **left subthalamic nucleus** would cause hemiballism on the **contralateral (right) side** of the body.
- The patient's symptoms are on the left side, indicating a lesion in the right subthalamic nucleus.
*Right internal capsule*
- A lesion in the **right internal capsule** would primarily cause contralateral (left-sided) motor and sensory deficits, such as **hemiparesis** or **hemiplegia**.
- While it affects the contralateral side as described in the patient, it would typically present as weakness rather than uncontrolled flinging movements.
Basal ganglia US Medical PG Question 8: A 62-year-old man is referred to neurology by his primary care physician. He is accompanied by his wife. The patient reports having a resting tremor in his left hand for over a year and some “stiffness” in his left arm. His wife notes that he has started to walk "funny" as well. He has a history of hypertension and hyperlipidemia. He takes aspirin, amlodipine, and rosuvastatin. On physical examination, you notice a repetitive circular movement of his left index finger and thumb that resolves with active movement of the hand. Passive motion of the left upper extremity is partially limited by rigidity. Gait is slow and shuffling. The patient is prescribed the most effective treatment for his disorder. Which of the following is the mechanism of a second drug given to prevent adverse effects of this therapy?
- A. Inhibits monoamine oxidase-B
- B. Activates dopamine receptors
- C. Inhibits catechol-O-methyltransferase
- D. Inhibits aromatic L-amino acid decarboxylase (Correct Answer)
- E. Blocks muscarinic acetylcholine receptors
Basal ganglia Explanation: ***Inhibits aromatic L-amino acid decarboxylase***
- The patient's symptoms (resting tremor, rigidity, shuffling gait, bradykinesia) are classical for **Parkinson's disease**, which is treated with **levodopa**.
- Levodopa is often co-administered with a peripheral **aromatic L-amino acid decarboxylase (AADC) inhibitor** (e.g., carbidopa) to prevent its peripheral conversion to dopamine, reducing side effects and increasing levodopa's bioavailability in the brain.
*Inhibits monoamine oxidase-B*
- **Monoamine oxidase-B (MAO-B) inhibitors** (e.g., selegiline, rasagiline) are used in Parkinson's disease to reduce dopamine breakdown, but they are not primarily given to prevent adverse effects of levodopa itself; instead, they act to prolong the effect of available dopamine.
- While they can be used adjunctively, their main role is to increase dopamine levels rather than directly mitigating levodopa's peripheral side effects.
*Activates dopamine receptors*
- **Dopamine receptor agonists** (e.g., pramipexole, ropinirole) are used in Parkinson's disease to directly stimulate dopamine receptors, either as monotherapy or adjunctively.
- They are a treatment for the disease itself, not a co-medication specifically designed to prevent adverse effects of levodopa.
*Inhibits catechol-O-methyltransferase*
- **Catechol-O-methyltransferase (COMT) inhibitors** (e.g., entacapone, tolcapone) prolong the action of levodopa by blocking its peripheral metabolism by COMT.
- While they prevent levodopa breakdown and enhance its central availability, they are typically used to extend the "on" time and manage motor fluctuations, rather than primarily preventing immediate peripheral adverse effects.
*Blocks muscarinic acetylcholine receptors*
- **Anticholinergics** (e.g., benztropine, trihexyphenidyl) block muscarinic acetylcholine receptors and are primarily used to treat the **tremor-dominant** form of Parkinson's disease.
- They do not prevent the peripheral adverse effects of levodopa; their mechanism of action is distinct and targets a different neurochemical imbalance.
Basal ganglia US Medical PG Question 9: Arrange in sequence the structures involved in the direct pathway (1=Striatum, 2=GPi, 3=Thalamus, 4=Cortex output, 5=Cortex input):-
- A. 1,3,4,2,5
- B. 5,1,2,3,4 (Correct Answer)
- C. 1,2,3,4,5
- D. 5,4,2,3,1
- E. 5,1,3,2,4
Basal ganglia Explanation: ***5,1,2,3,4***
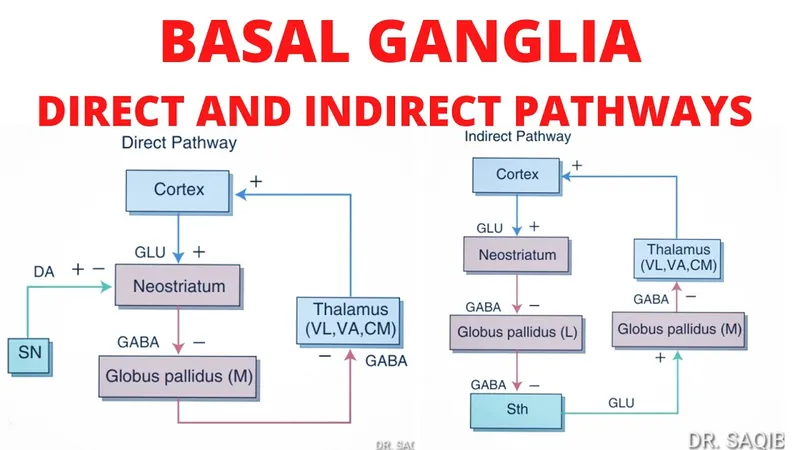
- The direct pathway of the basal ganglia begins with the **cortex** (5) sending excitatory signals to the **striatum** (1).
- The striatum then inhibits the **internal globus pallidus (GPi)** (2), which disinhibits the **thalamus** (3), leading to excitation of the **cortex** (4).
- This is the correct sequence: **Cortex input → Striatum → GPi → Thalamus → Cortex output**.
*1,3,4,2,5*
- This sequence is incorrect as it starts with the striatum instead of cortical input.
- The direct pathway does not begin with striatal activity; the cortex must first activate the striatum.
*1,2,3,4,5*
- This order is incorrect because it implies the pathway starts at the striatum rather than the cortex.
- The cortex should be the starting point (5) and the ending point (4) of the motor loop.
*5,4,2,3,1*
- This sequence is incorrect as it places cortex output (4) before the striatum receives input.
- This reverses the functional flow and does not follow the **disinhibitory mechanism** of the direct pathway.
*5,1,3,2,4*
- This sequence incorrectly places the thalamus (3) before the GPi (2).
- In the direct pathway, the striatum must first inhibit the GPi before the thalamus can be disinhibited.
Basal ganglia US Medical PG Question 10: Fibers from the marked structure terminate at which of the following?
- A. Red nucleus (Correct Answer)
- B. Subthalamus
- C. Inferior olivary nucleus
- D. Fastigial nucleus
Basal ganglia Explanation: ***Red nucleus***
- The arrow points to the **superior cerebellar peduncle**, which contains efferent fibers from the **dentate nucleus** of the cerebellum.
- A major projection of the superior cerebellar peduncle is to the **contralateral red nucleus**, forming part of the **dentato-rubro-thalamic pathway**.
*Subthalamus*
- The subthalamus is part of the **diencephalon** and is involved in motor control as part of the **basal ganglia circuit**.
- It does not receive direct efferent projections from the cerebellum via the superior cerebellar peduncle.
*Inferior olivary nucleus*
- The inferior olivary nucleus is a major source of **climbing fibers** to the cerebellum, providing **afferent input** for motor learning and coordination.
- It does not receive direct efferent output from the cerebellum's deep nuclei via the superior cerebellar peduncle.
*Fastigial nucleus*
- The fastigial nucleus is one of the **deep cerebellar nuclei**, located medially.
- Its primary efferent projections are via the **inferior cerebellar peduncle** to the vestibular nuclei and reticular formation, not typically receiving fibers from the superior cerebellar peduncle.
More Basal ganglia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.