Upper limb lymphatic drainage US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Upper limb lymphatic drainage. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Upper limb lymphatic drainage US Medical PG Question 1: A 49-year-old woman presents to her physician with complaints of breast swelling and redness of the skin over her right breast for the past 1 month. She also mentions that the skin above her right breast appears to have thickened. She denies any pain or nipple discharge. The past medical history is significant for a total abdominal hysterectomy at 45 years of age. Her last mammogram 1 year ago was negative for any pathologic changes. On examination, the right breast was diffusely erythematous with gross edema and tenderness and appeared larger than the left breast. The right nipple was retracted and the right breast was warmer than the left breast. No localized mass was palpated. Which of the following statements best describes the patient’s most likely condition?
- A. It shows predominant lymphatic spread.
- B. The lesion expresses receptors for estrogen and progesterone.
- C. The lesion is due to Streptococcal infection.
- D. It is a benign lesion.
- E. The inflammation is due to obstruction of dermal lymphatic vessels. (Correct Answer)
Upper limb lymphatic drainage Explanation: ***The inflammation is due to obstruction of dermal lymphatic vessels.***
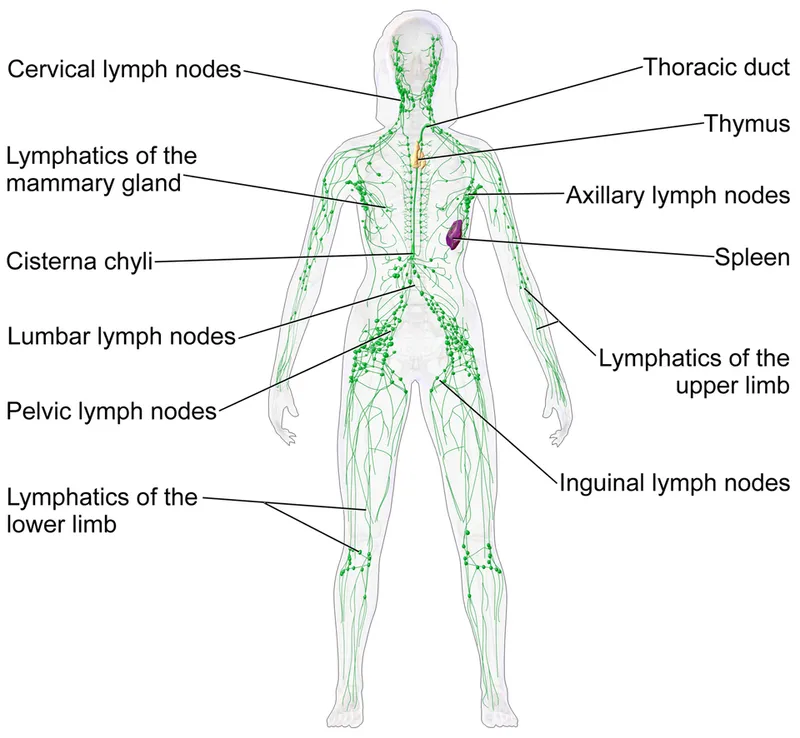
- The presentation of **rapid-onset breast swelling, redness, thickening of the skin, warmth, and nipple retraction** without a palpable mass is highly suggestive of **inflammatory breast cancer (IBC)**.
- IBC is characterized by the **obstruction of dermal lymphatic vessels by tumor cells**, leading to the classic inflammatory signs and **peau d'orange** appearance.
*It shows predominant lymphatic spread.*
- While IBC does involve **lymphatic spread**, this statement alone does not fully encompass the characteristic pathology of the condition causing the observed symptoms.
- The obstruction of the **dermal lymphatic vessels** is a more precise description of the immediate cause of the clinical presentation.
*The lesion expresses receptors for estrogen and progesterone.*
- Although some breast cancers are **hormone receptor-positive (ER/PR positive)**, there is no direct information in the vignette to suggest this specificity for the patient's condition.
- This statement refers to a **molecular characteristic** that is not a defining feature of the clinical presentation of IBC.
*The lesion is due to Streptococcal infection.*
- While a **bacterial infection** (like **streptococcal cellulitis**) can cause redness, swelling, and warmth, it typically presents with more acute symptoms, fever, and often a clearer response to antibiotics.
- The **thickening of the skin** and **nipple retraction** point away from a simple infection and towards a malignant process.
*It is a benign lesion.*
- The rapid progression of symptoms, pronounced skin changes, and nipple retraction are all **red flags for malignancy**, specifically inflammatory breast cancer.
- **Benign lesions** rarely cause such diffuse, severe, and rapidly progressing inflammatory signs.
Upper limb lymphatic drainage US Medical PG Question 2: A 52-year-old man presents to the emergency department because of pain and swelling in his left leg over the past few hours. He traveled from Sydney to Los Angeles 2 days ago. He has had type 2 diabetes mellitus for 10 years and takes metformin for it. He has smoked a pack of cigarettes daily for 25 years. His temperature is 36.9°C (98.4°F), the blood pressure is 140/90 mm Hg, and the pulse is 90/min. On examination, the left calf is 5 cm greater in circumference than the right. The left leg appears more erythematous than the right with dilated superficial veins. Venous duplex ultrasound shows non-compressibility. Which of the following best represents the mechanism of this patient’s illness?
- A. Impaired venous blood flow (Correct Answer)
- B. Subcutaneous soft-tissue infection that may extend to the deep fascia
- C. Infection of the dermis and subcutaneous tissues
- D. Impaired arterial blood flow
- E. Impaired lymphatic flow
Upper limb lymphatic drainage Explanation: ***Impaired venous blood flow***
- The patient's symptoms (unilateral leg pain and swelling, erythema, dilated superficial veins, recent long-haul travel) and the **venous duplex ultrasound** finding of **non-compressibility** are highly indicative of **deep vein thrombosis (DVT)**, which results from impaired venous outflow.
- Risk factors such as **long-haul travel** (venous stasis), **smoking** (endothelial damage), and potentially **diabetes** contribute to a hypercoagulable state.
*Impaired lymphatic flow*
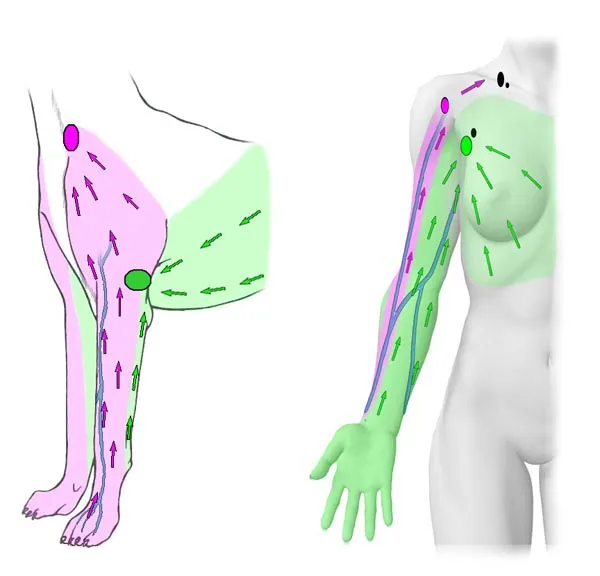
- This typically presents as **lymphedema**, characterized by chronic, often pitting edema, and skin changes like thickening (peau d'orange), but usually without acute erythema or dilated superficial veins in this context.
- **Venous duplex ultrasound** would not show non-compressibility in cases of impaired lymphatic flow, as veins themselves would be clear.
*Subcutaneous soft-tissue infection that may extend to the deep fascia*
- This describes **necrotizing fasciitis**, a severe infection often characterized by rapid progression, severe pain disproportionate to examination findings, blistering, and systemic toxicity, which are not clearly evident here.
- While there is erythema, the key diagnostic finding is the **non-compressible vein**, not signs of crepitus or rapidly spreading infection.
*Infection of the dermis and subcutaneous tissues*
- This describes **cellulitis**, which presents with localized redness, warmth, swelling, and tenderness, often with an entry point.
- While some symptoms overlap (erythema, swelling), the **venous duplex ultrasound finding of non-compressibility** definitively points away from a simple skin infection and towards a vascular obstruction.
*Impaired arterial blood flow*
- This presents as **acute limb ischemia**, characterized by the "6 Ps": pain, pallor, pulselessness, paresthesias, poikilothermia (coldness), and paralysis.
- The patient's leg is swollen and erythematous, not pale and cold, and the ultrasound directly implicates venous rather than arterial occlusion.
Upper limb lymphatic drainage US Medical PG Question 3: Which of the following cells in the body depends on dynein for its unique functioning?
- A. Small intestinal mucosal cell
- B. Skeletal muscle cell
- C. Adipocyte
- D. Lower esophageal mucosal cell
- E. Fallopian tube mucosal cell (Correct Answer)
Upper limb lymphatic drainage Explanation: ***Fallopian tube mucosal cell***
- Dynein is a **motor protein** that facilitates the movement of **cilia** along microtubules.
- The ciliary action in fallopian tube mucosal cells is crucial for **transporting the ovum** from the ovary to the uterus.
*Small intestinal mucosal cell*
- These cells primarily depend on **microvilli** for absorption, which are actin-based structures and do not directly involve dynein for their primary function of absorption.
- While they have some cilia, their unique and defining function is nutrient absorption, not movement dependent on dynein.
*Skeletal muscle cell*
- Skeletal muscle cells rely on the interaction of **actin and myosin** filaments for **contraction**.
- Dynein is not directly involved in the mechanism of muscle contraction.
*Adipocyte*
- Adipocytes are specialized in **lipid storage** and release, a process that does not involve dynein.
- Their unique function does not depend on intracellular or extracellular movement facilitated by dynein.
*Lower esophageal mucosal cell*
- These cells primarily provide a **protective barrier** against gastric acid reflux.
- Their function involves **stratified squamous epithelium** and mucus production, not ciliary movement dependent on dynein.
Upper limb lymphatic drainage US Medical PG Question 4: An investigator is studying the immune response and the spleen in a mouse model infected with Escherichia coli. Which of the following anatomical sites in the spleen is important for the secondary maturation and affinity maturation of B cells that will ultimately target Escherichia coli?
- A. Sinusoids
- B. Periarteriolar lymphatic sheaths
- C. Marginal zone
- D. Red pulp
- E. Germinal center (Correct Answer)
Upper limb lymphatic drainage Explanation: ***Germinal center***
- The **germinal centers** are the primary sites within secondary lymphoid organs, including the spleen, where B cells undergo **proliferation**, **somatic hypermutation**, and **affinity maturation** following antigen exposure.
- This process is crucial for generating high-affinity antibodies capable of effectively targeting pathogens like *Escherichia coli*.
*Sinusoids*
- **Sinusoids** are specialized vascular channels found throughout the spleen, particularly in the red pulp, responsible for filtering blood and removing old or damaged red blood cells.
- They are not directly involved in the secondary maturation or affinity maturation of B cells.
*Periarteriolar lymphatic sheaths*
- The **periarteriolar lymphatic sheaths (PALS)** are T-cell rich areas in the white pulp of the spleen, surrounding central arterioles.
- While important for T-cell activation, the main site for B-cell affinity maturation is the germinal center, which forms within B cell follicles adjacent to the PALS.
*Marginal zone*
- The **marginal zone** is a specialized area at the periphery of the white pulp, rich in unique B cell populations that respond rapidly to T-cell independent antigens.
- While it plays a role in initial immune responses, it is not the primary site for the secondary maturation and affinity maturation of B cells.
*Red pulp*
- The **red pulp** makes up the majority of the spleen and is primarily involved in filtering blood, removing old red blood cells, and storing platelets.
- While it contains macrophages and other immune cells, it is not the main site for B-cell secondary maturation and affinity maturation, which occurs in the white pulp's germinal centers.
Upper limb lymphatic drainage US Medical PG Question 5: A 32-year-old man comes to the physician because of a 3-week history of cough, weight loss, and night sweats. He migrated from Sri Lanka 6 months ago. He appears emaciated. His temperature is 38.1°C (100.5°F). Physical examination shows enlargement of the right supraclavicular lymph node. Chest and abdominal examination show no abnormalities. An interferon-gamma assay is positive. A biopsy specimen of the cervical lymph node is most likely to show the causal organism in which of the following locations?
- A. Mantle zone
- B. Medullary sinus
- C. Germinal center
- D. Subcapsular sinus
- E. Paracortex (Correct Answer)
Upper limb lymphatic drainage Explanation: ***Paracortex***
- The patient's symptoms (cough, weight loss, night sweats, fever), recent migration from an endemic area (Sri Lanka), **supraclavicular lymphadenopathy**, and positive **interferon-gamma release assay (IGRA)** strongly suggest **tuberculosis**.
- In tuberculous lymphadenitis, **caseating granulomas** containing *Mycobacterium tuberculosis* organisms characteristically form in the **paracortex** (T-cell zone).
- The **paracortex** is where **cell-mediated immunity** occurs, with T cells interacting with infected macrophages and dendritic cells to form the **epithelioid granulomas** with **Langhans giant cells** that are pathognomonic for TB.
- The organisms are found within these **granulomas**, which predominantly occur in the paracortical (interfollicular) region.
*Mantle zone*
- The **mantle zone** primarily contains **naïve B cells** surrounding germinal centers.
- This is a B-cell area not typically involved in granuloma formation or mycobacterial infection.
*Germinal center*
- **Germinal centers** are sites of B cell proliferation, somatic hypermutation, and antibody class switching.
- TB is a disease of **cell-mediated immunity** (T cells and macrophages), not humoral immunity, so granulomas do not form in germinal centers.
*Medullary sinus*
- The **medullary sinuses** are channels in the medulla of the lymph node through which lymph flows toward the efferent lymphatic vessels.
- While macrophages line these sinuses and may contain some organisms in acute infections, the characteristic **caseating granulomas** of chronic tuberculous lymphadenitis form in the **paracortex**, not in the sinuses.
*Subcapsular sinus*
- The **subcapsular sinus** is the initial entry point for afferent lymph into the lymph node.
- While this is where pathogens first enter, chronic granulomatous infections like TB develop their characteristic pathology deeper in the node, specifically in the **paracortex** where T-cell-mediated granuloma formation occurs.
Upper limb lymphatic drainage US Medical PG Question 6: A 39-year-old man presents with painless swelling of the right testis and a sensation of heaviness. The physical examination revealed an intra-testicular solid mass that could not be felt separately from the testis. After a thorough evaluation, he was diagnosed with testicular seminoma. Which of the following group of lymph nodes are most likely involved?
- A. Superficial inguinal lymph nodes (lateral group)
- B. Deep inguinal lymph nodes
- C. Superficial inguinal lymph nodes (medial group)
- D. Para-rectal lymph nodes
- E. Para-aortic lymph nodes (Correct Answer)
Upper limb lymphatic drainage Explanation: ***Para-aortic lymph nodes***
- The **testes** develop in the abdomen and descend into the scrotum, retaining their original lymphatic drainage. Therefore, **testicular cancer** typically metastasizes to the **para-aortic** (or retroperitoneal) lymph nodes, which are located near the renal veins at the level of L1-L2.
- This is the primary lymphatic drainage pathway for the testes.
*Superficial inguinal lymph nodes (lateral group)*
- These lymph nodes primarily drain the skin of the **scrotum**, perineum, and lower limbs, but not the **testes** themselves.
- Involvement would suggest spread to the scrotal skin or compromised lymphatic flow due to prior scrotal surgery or infection, which is not indicated here.
*Deep inguinal lymph nodes*
- **Deep inguinal lymph nodes** drain structures deeper in the leg and gluteal region, as well as receiving efferent vessels from the superficial inguinal nodes.
- They are not the primary drainage site for the **testes**.
*Superficial inguinal lymph nodes (medial group)*
- Similar to the lateral group, the **medial superficial inguinal lymph nodes** primarily drain the external genitalia (excluding the testes), perineum, and lower abdominal wall.
- They are not the direct drainage route for **testicular cancer**.
*Para-rectal lymph nodes*
- **Para-rectal lymph nodes** are located near the rectum and are involved in the drainage of the rectum and lower sigmoid colon.
- They have no direct connection to the lymphatic drainage of the **testes**.
Upper limb lymphatic drainage US Medical PG Question 7: A 93-year-old woman is brought to the physician because of a purple area on her right arm that has been growing for one month. She has not had any pain or itching of the area. She has hyperlipidemia, a history of basal cell carcinoma treated with Mohs surgery 2 years ago, and a history of invasive ductal carcinoma of the right breast treated with radical mastectomy 57 years ago. She has had chronic lymphedema of the right upper extremity since the mastectomy. Her only medication is simvastatin. She lives in an assisted living facility. She is content with her living arrangement but feels guilty that she is dependent on others. Vital signs are within normal limits. Physical examination shows extensive edema of the right arm. Skin exam of the proximal upper right extremity shows three coalescing, 0.5–1.0 cm heterogeneous, purple-colored plaques with associated ulceration. Which of the following is the most likely diagnosis?
- A. Lymphangiosarcoma (Correct Answer)
- B. Cellulitis
- C. Thrombophlebitis
- D. Kaposi sarcoma
- E. Lichen planus
Upper limb lymphatic drainage Explanation: ***Lymphangiosarcoma***
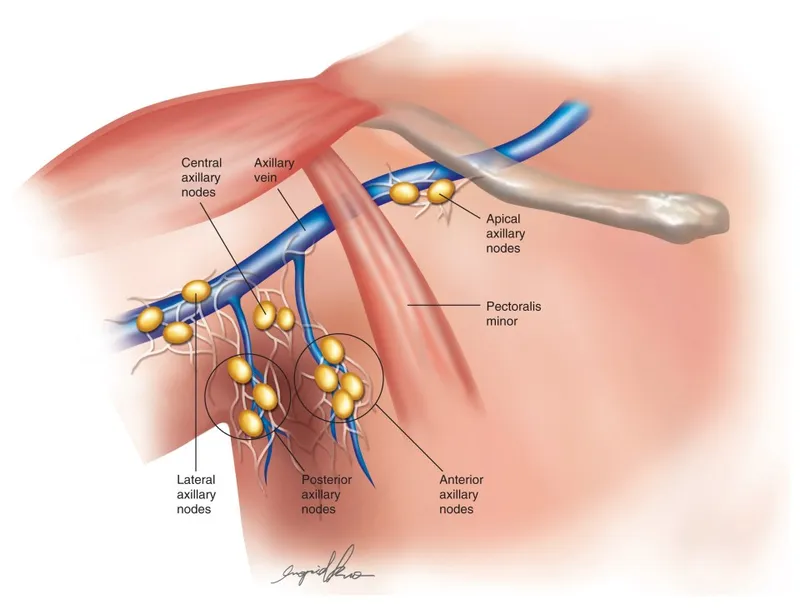
- This patient presents with a **purple area** with **ulceration** on an arm affected by chronic **lymphedema** following a mastectomy. This constellation of findings is highly suggestive of **Stewart-Treves syndrome**, which is a rare but aggressive form of angiosarcoma (lymphangiosarcoma) arising in the setting of chronic lymphedema.
- The history of **radical mastectomy 57 years ago** with subsequent **chronic right upper extremity lymphedema** strongly predisposes to this condition, especially given the lack of pain or itching and the progressive nature of the lesion.
*Cellulitis*
- Characterized by **erythema**, **warmth**, **pain**, and **tenderness**, often with fever and systemic symptoms, none of which are described.
- While lymphedema is a risk factor for cellulitis, the description of a **purple, ulcerated plaque** with a duration of one month is inconsistent with acute bacterial infection.
*Thrombophlebitis*
- Typically presents with **pain**, **tenderness**, **erythema**, and a palpable cord-like vein along the course of a superficial vein, which is not described.
- The lesion described is a spreading, **ulcerated plaque**, not a discrete inflamed vein.
*Kaposi sarcoma*
- While it can present with **purple lesions**, Kaposi sarcoma is typically associated with **immunosuppression** (e.g., HIV infection) or certain endemic regions, neither of which is mentioned.
- The strong association with **chronic lymphedema** in this case makes lymphangiosarcoma a more specific diagnosis.
*Lichen planus*
- A chronic inflammatory condition characterized by **pruritic, purple, polygonal, planar papules and plaques (the 6 Ps)**, often with fine white lines (Wickham's striae).
- It does not typically present as a growing, **ulcerated purple plaque** in the setting of chronic lymphedema, and itching is a prominent symptom.
Upper limb lymphatic drainage US Medical PG Question 8: An investigator is studying the clearance of respiratory particles in healthy non-smokers. An aerosol containing radio-labeled particles that are small enough to reach the alveoli is administered to the subjects via a non-rebreather mask. A gamma scanner is then used to evaluate the rate of particle clearance from the lungs. The primary mechanism of particle clearance most likely involves which of the following cell types?
- A. Goblet cells
- B. Macrophages (Correct Answer)
- C. Club cells
- D. Type I pneumocytes
- E. Neutrophils
Upper limb lymphatic drainage Explanation: ***Macrophages***
- **Alveolar macrophages** are the primary phagocytic cells in the alveoli responsible for clearing inhaled particles that reach this deepest part of the lung.
- They engulf and digest foreign substances, including pathogens and inert particles, protecting the delicate alveolar structures.
*Goblet cells*
- **Goblet cells** are found in the larger airways (trachea, bronchi), where they produce mucus to trap inhaled particles.
- They are not present in the alveoli, so they cannot clear particles that have reached this region.
*Club cells*
- **Club cells** (formerly Clara cells) are located in the bronchioles and secrete components of the surfactant-like material, but they do not primarily function in particle clearance.
- While they have some protective roles, they are not the main phagocytic cells for alveolar particles.
*Type I pneumocytes*
- **Type I pneumocytes** are flattened, thin cells that form the majority of the alveolar surface and are primarily involved in gas exchange.
- They are not phagocytic and do not play a direct role in clearing inhaled particles.
*Neutrophils*
- **Neutrophils** are acute inflammatory cells primarily involved in combating bacterial infections.
- While they can migrate to the lungs during inflammation, they are not the primary, routine phagocytic cells for clearing inhaled particles in healthy individuals.
Upper limb lymphatic drainage US Medical PG Question 9: A 6-year-old boy is brought to a primary care provider by his adoptive parents for evaluation of a 3-month history of jaw swelling. He has a travel history of recent immigration from equatorial Africa where his deceased mother was positive for HIV and died from related complications. On physical exam, extensive lymph node swelling on the left side of his jaw is noted. There is also an ulceration that appears to be infected. Fine needle biopsy of the lymph node yields a diagnosis of Burkitt’s lymphoma by the pathologist. Which of the following is most likely associated with the involvement of lymph nodes around his jaw?
- A. Ethnicity of the patient
- B. Close family member with HIV
- C. Gender of the patient
- D. Recent immigration from equatorial Africa (Correct Answer)
- E. Infected ulcer
Upper limb lymphatic drainage Explanation: ***Recent immigration from equatorial Africa***
- **Endemic Burkitt's lymphoma**, common in equatorial Africa, typically manifests as a **jaw mass** in children and is strongly associated with **Epstein-Barr virus (EBV)**.
- The patient's history of immigration from this region directly links to the presentation of Burkitt's lymphoma in his jaw.
*Ethnicity of the patient*
- While certain ethnic groups may have higher predispositions to specific diseases, ethnicity itself is not the primary determinant for the **endemic presentation of Burkitt's lymphoma** in the jaw.
- The **geographical region** (equatorial Africa) is a more direct and stronger risk factor for this specific clinical picture.
*Close family member with HIV*
- HIV infection can increase the risk of **immunodeficiency-associated lymphomas**, but it doesn't specifically explain the characteristic **jaw involvement** seen in endemic Burkitt's lymphoma.
- The mother's HIV status indicates a potential compromised immune system in the patient, which can be a predisposing factor for lymphomas in general, but not specifically for the jaw location of Burkitt's lymphoma.
*Gender of the patient*
- **Burkitt's lymphoma** does not show a significant predilection for one gender over the other to explain the specific jaw involvement.
- The presentation is more tied to **geographic and immunological factors** than to the patient's gender.
*Infected ulcer*
- The infected ulcer is a **secondary complication** or a symptom that may arise from the rapidly growing tumor, indicating opportunistic infection, rather than the primary cause or association for the specific location of the lymphoma.
- It doesn't explain why the lymphoma initially presented in the **jaw lymph nodes**.
Upper limb lymphatic drainage US Medical PG Question 10: An otherwise healthy 39-year-old woman presents to her primary care provider because of right-leg swelling, which started 4 months ago following travel to Kenya. The swelling has been slowly progressive and interferes with daily tasks. She denies smoking or alcohol use. Family history is irrelevant. Vital signs include: temperature 38.1°C (100.5°F), blood pressure 115/72 mm Hg, and pulse 99/min. Physical examination reveals non-pitting edema of the entire right leg. The overlying skin is rough, thick and indurated. The left leg is normal in size and shape. Which of the following is the most likely cause of this patient condition?
- A. Obstruction of lymphatic channels (Correct Answer)
- B. Hypoalbuminemia
- C. Lymphatic hypoplasia
- D. Venous thromboembolism
- E. Persistent elevation of venous pressures
Upper limb lymphatic drainage Explanation: ***Obstruction of lymphatic channels***
- The patient's history of travel to **Kenya**, along with **progressive, non-pitting edema** of the entire right leg and **rough, thick, indurated skin**, strongly suggests **filariasis**, a parasitic infection that obstructs lymphatic channels.
- **Obstruction of lymphatic channels** leads to **lymphedema**, which characteristically presents with the described symptoms and skin changes (e.g., **elephantiasis**).
*Hypoalbuminemia*
- **Hypoalbuminemia** typically causes **generalized, pitting edema** due to decreased plasma oncotic pressure, not localized, non-pitting edema in a single limb.
- There are no clinical signs to suggest **hepatic** or **renal dysfunction** that would cause significant hypoalbuminemia.
*Lymphatic hypoplasia*
- **Lymphatic hypoplasia** (primary lymphedema) is usually congenital or develops in early life and would not typically manifest acutely after travel in a 39-year-old.
- While it causes lymphedema, the travel history points to an acquired cause rather than a congenital defect.
*Venous thromboembolism*
- **Venous thromboembolism** (DVT) typically presents with acute onset of **painful, edematous** limb, often with **pitting edema**, and can be associated with warmth and erythema.
- The **slowly progressive** nature of the swelling over 4 months and **non-pitting edema** are less consistent with acute DVT.
*Persistent elevation of venous pressures*
- **Persistent elevation of venous pressures** (e.g., chronic venous insufficiency) leads to **pitting edema**, skin discoloration (**hyperpigmentation**), and **ulcerations**, not the rough, thick, indurated skin seen in this case.
- This condition is also typically associated with factors like prolonged standing or obesity, which are not mentioned here.
More Upper limb lymphatic drainage US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.