Thoracic lymphatic drainage US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thoracic lymphatic drainage. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thoracic lymphatic drainage US Medical PG Question 1: A 34-year-old patient presents with severe pain in the right upper quadrant that radiates to the right shoulder. During laparoscopic cholecystectomy, which of the following anatomical spaces must be carefully identified to prevent bile duct injury?
- A. Foramen of Winslow
- B. Lesser sac
- C. Calot's triangle (Correct Answer)
- D. Morrison's pouch
Thoracic lymphatic drainage Explanation: ***Calot's triangle***
- **Calot's triangle** is the critical anatomical landmark containing the **cystic artery** and **cystic duct**, whose proper identification is essential to prevent injury to the hepatic artery or bile ducts during cholecystectomy.
- Its boundaries are the **cystic duct** (lateral), the **common hepatic duct** (medial), and the **inferior border of the liver** (superior, sometimes described as the cystic artery).
*Foramen of Winslow*
- The **Foramen of Winslow** (epiploic foramen) is an opening connecting the **greater and lesser sacs** of the peritoneal cavity.
- It is not directly relevant to identifying structures during cholecystectomy, but rather to accessing the lesser sac or for surgical procedures involving structures like the portal triad.
*Lesser sac*
- The **lesser sac** (omental bursa) is a peritoneal cavity posterior to the stomach and lesser omentum.
- It is explored in procedures involving the pancreas, posterior gastric wall, or for assessing fluid collections, but not for direct identification of cystic structures during standard cholecystectomy.
*Morrison's pouch*
- **Morrison's pouch** is the **hepatorenal recess**, a potential space between the posterior aspect of the liver and the right kidney and adrenal gland.
- It is a common site for **fluid accumulation** (e.g., ascites, blood) but is not directly incised or dissected for preventing bile duct injury during cholecystectomy.
Thoracic lymphatic drainage US Medical PG Question 2: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Thoracic lymphatic drainage Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
Thoracic lymphatic drainage US Medical PG Question 3: A 32-year-old man comes to the emergency department because of a wound in his foot. Four days ago, he stepped on a nail while barefoot at the beach. Examination of the plantar surface of his right foot shows a purulent puncture wound at the base of his second toe with erythema and tenderness of the surrounding skin. The afferent lymphatic vessels from the site of the lesion drain directly into which of the following groups of regional lymph nodes?
- A. Popliteal
- B. Deep inguinal
- C. Anterior tibial
- D. Superficial inguinal (Correct Answer)
- E. External iliac
Thoracic lymphatic drainage Explanation: ***Superficial inguinal***
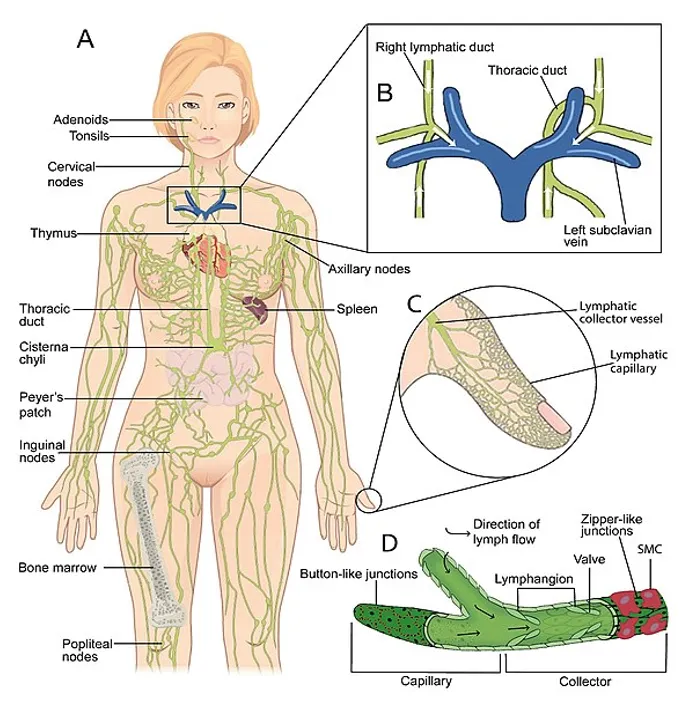
- Lymph from the **plantar surface of the foot** (including the base of the toes) drains into the **superficial inguinal lymph nodes**.
- The **medial and central plantar surfaces** specifically follow the medial superficial lymphatic vessels that accompany the great saphenous vein system to reach these nodes.
- These nodes are the **primary drainage site** and crucial in the initial immune response to infections of the lower limb.
*Popliteal*
- The **popliteal lymph nodes** primarily drain lymph from the **lateral foot and heel**, posterior leg, and knee.
- They are located within the popliteal fossa and would not be the direct drainage site for a wound on the plantar surface of the second toe.
*Deep inguinal*
- **Deep inguinal lymph nodes** receive lymph from the superficial inguinal nodes, as well as from deeper structures of the thigh and glans penis/clitoris.
- They are considered a **secondary drainage site** and not the primary destination for superficial foot infections.
*Anterior tibial*
- There are no well-defined major lymph nodes specifically termed "anterior tibial" that serve as a primary drainage site for the foot.
- Lymphatics generally follow venous drainage patterns, and the anterior tibial vessels drain superiorly, not to a specific nodal group at this level.
*External iliac*
- **External iliac lymph nodes** receive lymph primarily from the deep inguinal nodes and pelvic organs.
- They are a more **proximal group** in the lymphatic chain and not the direct initial drainage site for a foot infection.
Thoracic lymphatic drainage US Medical PG Question 4: A mother brings her 1-week-old son to the pediatrician because she is concerned about the child’s umbilicus. She notes that there appears to be fluid draining from the child’s umbilicus several times a day. The child has been breastfeeding normally. On exam, a small amount of clear light yellow fluid drains from the child’s umbilical stump when pressure is applied to the child’s lower abdomen. No bilious or feculent drainage is noted. Which of the following embryologic structures is associated with this patient’s condition?
- A. Paramesonephric duct
- B. Urachus (Correct Answer)
- C. Umbilical vein
- D. Ductus venosus
- E. Omphalomesenteric duct
Thoracic lymphatic drainage Explanation: ***Urachus***
- The draining of clear, light yellow fluid from the umbilical stump on abdominal pressure is characteristic of a **patent urachus**, which is a remnant of the **allantois**.
- A patent urachus connects the **umbilical cord** to the **bladder**, allowing urine to leak through the umbilicus.
*Paramesonephric duct*
- The paramesonephric (Müllerian) duct develops into female reproductive structures like the **fallopian tubes**, **uterus**, and **upper vagina**.
- It is not associated with umbilical drainage or the urinary system.
*Umbilical vein*
- The umbilical vein carries **oxygenated blood** from the placenta to the fetus and typically obliterates to form the **ligamentum teres hepatis**.
- Its patency would lead to vascular issues, not fluid drainage from the umbilicus.
*Ductus venosus*
- The ductus venosus shunts **oxygenated blood** from the umbilical vein directly to the inferior vena cava, bypassing the liver.
- It obliterates to form the **ligamentum venosum** and is not involved in umbilical fluid leakage.
*Omphalomesenteric duct*
- The omphalomesenteric (vitelline) duct connects the **fetal midgut** to the **yolk sac** during early development.
- A patent omphalomesenteric duct would typically present with **feculent** or **bilious drainage** from the umbilicus, not clear, light yellow fluid, as it is connected to the digestive tract.
Thoracic lymphatic drainage US Medical PG Question 5: A 14-year-old boy is brought to the emergency department because of acute left-sided chest pain and dyspnea following a motor vehicle accident. His pulse is 122/min and blood pressure is 85/45 mm Hg. Physical examination shows distended neck veins and tracheal displacement to the right side. The left chest is hyperresonant to percussion and there are decreased breath sounds. This patient would most benefit from needle insertion at which of the following anatomical sites?
- A. 5th left intercostal space along the midclavicular line
- B. 8th left intercostal space along the posterior axillary line
- C. 2nd left intercostal space along the midclavicular line (Correct Answer)
- D. Subxiphoid space in the left sternocostal margin
- E. 5th left intercostal space along the midaxillary line
Thoracic lymphatic drainage Explanation: ***2nd left intercostal space along the midclavicular line***
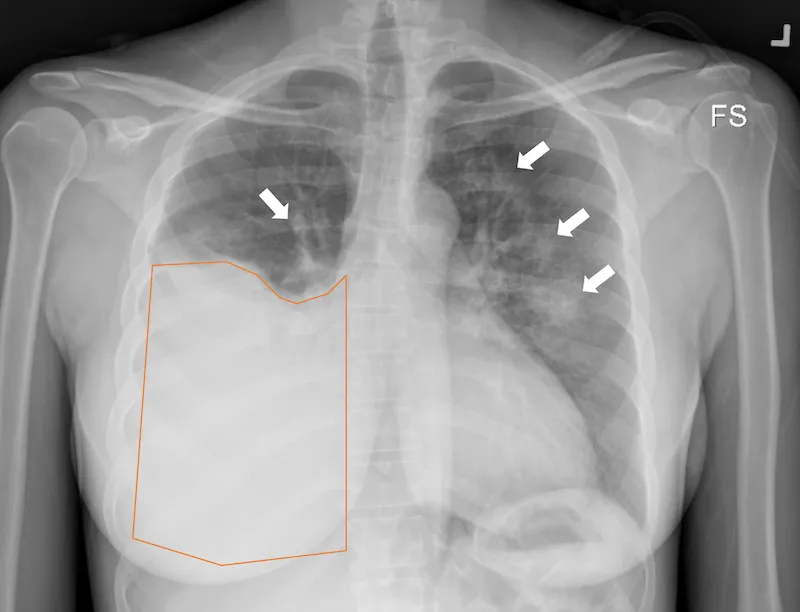
- The patient's symptoms (chest pain, dyspnea, hypotension, distended neck veins, tracheal deviation, hyperresonance, and decreased breath sounds on the left) are classic signs of a **tension pneumothorax**.
- Immediate treatment for **tension pneumothorax** involves needle decompression at the **2nd intercostal space** in the midclavicular line to relieve pressure and restore hemodynamic stability.
*5th left intercostal space along the midclavicular line*
- This location is typically used for **chest tube insertion** in a more controlled setting, not for emergent needle decompression of a tension pneumothorax.
- While it's a safe location for pleural access, it is not the **first-line site** for immediate life-saving decompression.
*8th left intercostal space along the posterior axillary line*
- This site is too low and posterior for effective needle decompression of a tension pneumothorax, which requires rapid access to the **apex of the lung**.
- It is more commonly used for **thoracentesis** to drain fluid from the pleural cavity.
*Subxiphoid space in the left sternocostal margin*
- This location is primarily used for **pericardiocentesis** to drain fluid from the pericardial sac in cases of cardiac tamponade.
- It is not appropriate for addressing a **pneumothorax**, which involves air in the pleural space.
*5th left intercostal space along the midaxillary line*
- This site is a common alternative for **chest tube insertion** but is not the preferred or most immediate site for needle decompression of a tension pneumothorax.
- While it offers pleural access, the **2nd intercostal space** anteriorly is chosen for expediency and safety in an emergency.
Thoracic lymphatic drainage US Medical PG Question 6: A 50-year-old man undergoes parathyroidectomy for treatment-resistant hyperparathyroidism. The procedure is complicated by brisk bleeding from the superior thyroid artery near the external branch of the superior laryngeal nerve. To stop the bleeding, the artery is ligated at its origin. Which of the following is most likely the origin of the artery that was injured in this patient?
- A. Thyrocervical trunk
- B. Ascending pharyngeal artery
- C. Internal carotid artery
- D. Subclavian artery
- E. External carotid artery (Correct Answer)
Thoracic lymphatic drainage Explanation: ***External carotid artery***
- The **superior thyroid artery** is the first branch to arise from the **external carotid artery** in the neck.
- Ligation of this artery at its origin is a common surgical maneuver to control bleeding during thyroid or parathyroid surgery.
*Thyrocervical trunk*
- The **thyrocervical trunk** is a branch of the **subclavian artery** and gives rise to the inferior thyroid artery, not the superior thyroid artery.
- Injury to the superior thyroid artery would not necessitate ligation of a vessel originating from the thyrocervical trunk.
*Ascending pharyngeal artery*
- The **ascending pharyngeal artery** is a small artery that branches from the **external carotid artery** but supplies the pharynx, not the thyroid gland.
- It is not typically implicated in bleeding during parathyroidectomy or in relation to the superior laryngeal nerve.
*Internal carotid artery*
- The **internal carotid artery** primarily supplies the brain and does not have branches in the neck that supply the thyroid or parathyroid glands.
- It arises from the common carotid artery but does not give off the superior thyroid artery.
*Subclavian artery*
- The **subclavian artery** gives rise to the **thyrocervical trunk**, which then supplies the inferior thyroid artery, but not directly the superior thyroid artery.
- The superior thyroid artery originates higher up from the external carotid artery.
Thoracic lymphatic drainage US Medical PG Question 7: A 72-year-old man presents with shortness of breath and right-sided chest pain. Physical exam reveals decreased breath sounds and dull percussion at the right lung base. Chest X-ray reveals a right-sided pleural effusion. A thoracentesis was performed, removing 450 mL of light pink fluid. Pleural fluid analysis reveals:
Pleural fluid to serum protein ratio: 0.35
Pleural fluid to serum LDH ratio: 0.49
Lactate dehydrogenase (LDH): 105 IU (serum LDH Reference: 100–190)
Which of the following disorders is most likely in this patient?
- A. Congestive heart failure (Correct Answer)
- B. Uremia
- C. Chylothorax
- D. Pancreatitis
- E. Sarcoidosis
Thoracic lymphatic drainage Explanation: ***Congestive heart failure***
- The **pleural fluid to serum protein ratio of 0.35** and **LDH ratio of 0.49** fall within the criteria for a **transudative effusion** (ratios < 0.5 for protein and < 0.6 for LDH).
- **Congestive heart failure (CHF)** is a common cause of transudative pleural effusions due to increased hydrostatic pressure.
*Uremia*
- **Uremic pleuritis** typically causes an **exudative effusion**, characterized by higher protein and LDH levels in the pleural fluid.
- While patients with uremia may have pleural effusions, the fluid analysis here is not consistent with that diagnosis.
*Chylothorax*
- A **chylothorax** is characterized by a **milky-white fluid** with very high triglyceride levels (>110 mg/dL), resulting from lymphatic leakage.
- The described fluid is "light pink" and does not have the typical biochemical profile of a chylothorax.
*Pancreatitis*
- **Pancreatitis-induced pleural effusions** are almost always **exudative** and typically have **elevated amylase levels**.
- The transudative nature of the effusion rules out pancreatitis as the most likely cause.
*Sarcoidosis*
- **Sarcoidosis** can cause **pleural effusions**, but these are usually **exudative** and often accompanied by other systemic manifestations like lymphadenopathy or skin lesions.
- The presented fluid analysis does not support a diagnosis of sarcoidosis.
Thoracic lymphatic drainage US Medical PG Question 8: A 23-year-old man is brought to the emergency department by a coworker for an injury sustained at work. He works in construction and accidentally shot himself in the chest with a nail gun. Physical examination shows a bleeding wound in the left hemithorax at the level of the 4th intercostal space at the midclavicular line. Which of the following structures is most likely injured in this patient?
- A. Right atrium of the heart
- B. Inferior vena cava
- C. Left upper lobe of the lung (Correct Answer)
- D. Left atrium of the heart
- E. Superior vena cava
Thoracic lymphatic drainage Explanation: ***Left upper lobe of the lung***
- The **left upper lobe of the lung** extends to the 4th intercostal space at the midclavicular line, making it the most probable structure to be traversed by a penetrating injury at this location.
- The **pleural cavity** and lung tissue are superficially located in this region, making them highly susceptible to injury from a nail gun.
*Right atrium of the heart*
- The **right atrium** is located predominantly on the right side of the sternum, more centrally, and slightly to the right of the midclavicular line.
- An injury at the **left 4th intercostal space at the midclavicular line** would typically be too lateral and superior to directly injure the right atrium.
*Inferior vena cava*
- The **inferior vena cava (IVC)** enters the right atrium from below, primarily located within the abdomen and passing through the diaphragm at the level of T8.
- Its position is far too **inferior and posterior** relative to the 4th intercostal space to be directly injured by this wound.
*Left atrium of the heart*
- The **left atrium** is the most posterior chamber of the heart and is largely covered by the left ventricle.
- Although part of the heart is on the left, an injury at the **4th intercostal space, midclavicular line**, would likely impact the left ventricle or lung tissue before reaching the left atrium, which is located more posteriorly and medially.
*Superior vena cava*
- The **superior vena cava (SVC)** is located to the right of the midline, formed by the brachiocephalic veins behind the right first costal cartilage.
- Its position is too **medial and superior**, on the right side, to be directly injured by a nail penetrating the left 4th intercostal space at the midclavicular line.
Thoracic lymphatic drainage US Medical PG Question 9: A 44-year-old woman undergoes radical hysterectomy for stage IB2 cervical cancer. During surgery, the gynecologic oncologist notes aberrant lymphatic drainage patterns possibly related to the patient's history of pelvic inflammatory disease and previous cesarean section. Frozen section of a lymph node from the obturator fossa shows metastatic disease. Synthesizing knowledge of primary and collateral cervical lymphatic drainage, which nodal group represents the most critical next level of drainage that would impact surgical decision-making?
- A. Presacral nodes via uterosacral ligament pathway
- B. Common iliac and para-aortic nodes via external iliac pathway (Correct Answer)
- C. Internal iliac nodes only
- D. Inguinal nodes via deep femoral pathway
- E. Superficial inguinal nodes via round ligament pathway
Thoracic lymphatic drainage Explanation: ***Common iliac and para-aortic nodes via external iliac pathway***
- The **common iliac nodes** serve as the primary drainage destination from both the **external iliac** and **obturator nodes**, making them the critical next level when **obturator metastasis** is confirmed.
- Lymphatic spread in cervical cancer typically follows a regular pattern: primary pelvic nodes (obturator, external/internal iliacs) move toward the **common iliac** and then **para-aortic** regions.
*Superficial inguinal nodes via round ligament pathway*
- Drainage to these nodes occurs primarily from the **uterine horns** or the **vulva**, not typically the cervix unless the tumor involves the lower vagina.
- These nodes are not part of the standard cephalad **retroperitoneal spread** pathway for stage IB2 cervical cancer.
*Presacral nodes via uterosacral ligament pathway*
- These nodes provide a minor primary drainage route via the **uterosacral ligaments**, but they are anatomically distinct from the lateral **obturator fossa** chain.
- They do not represent the "next level" of drainage that would indicate **systemic progression** beyond the pelvic basin.
*Internal iliac nodes only*
- The **internal iliac nodes** are primary pelvic nodes and are considered on the **same drainage tier** as the obturator nodes already found to be positive.
- Assessing these nodes only would not provide enough information regarding the **cephalad extent** of the disease required for surgical modification.
*Inguinal nodes via deep femoral pathway*
- The **deep femoral pathway** primarily drains the lower limb and vulva rather than the **cervical stroma** and parametrium.
- Involvement of these nodes would be an exception and would not help in determining the transition to **extended-field radiation** for retroperitoneal disease.
Thoracic lymphatic drainage US Medical PG Question 10: A 67-year-old man with squamous cell carcinoma of the anal canal presents for staging. Physical examination reveals a 3 cm tumor at the dentate line extending both above and below it. Inguinal lymphadenopathy is palpable bilaterally. CT shows both inguinal and pelvic lymph node enlargement. Evaluating the lymphatic drainage of the anal canal, which treatment approach best addresses the dual drainage patterns of this tumor location?
- A. Chemoradiation targeting both inguinal and pelvic nodal basins (Correct Answer)
- B. Pelvic lymph node dissection only, following inferior mesenteric pathways
- C. Sequential surgery: abdominoperineal resection then inguinal dissection
- D. Radiation to inguinal nodes only with surgical resection of pelvic nodes
- E. Inguinal lymph node dissection only, as anal tumors drain superficially
Thoracic lymphatic drainage Explanation: ***Chemoradiation targeting both inguinal and pelvic nodal basins***
- Tumors at the **dentate line** exhibit dual lymphatic drainage: the area above drains to **internal iliac** and **perirectal nodes**, while the area below drains to **superficial inguinal nodes**.
- The standard of care for anal **squamous cell carcinoma** (SCC) is the **Nigro protocol**, which uses **definitive chemoradiotherapy** to treat both the primary tumor and all involved regional nodal basins.
*Inguinal lymph node dissection only, as anal tumors drain superficially*
- While the area below the dentate line drains to **inguinal nodes**, the area above drains into the **pelvis**, meaning a dissection limited to the groin would miss half of the drainage pathway.
- Surgical dissection is not the primary treatment for anal SCC, as **chemoradiation** offers high rates of cure while preserving anal sphincter function.
*Pelvic lymph node dissection only, following inferior mesenteric pathways*
- This approach neglects the **superficial inguinal nodes**, which are already palpably enlarged in this patient and are the primary drainage route for the inferior anal canal.
- **Pelvic lymph node dissection** is technically difficult and carries high morbidity; it has been largely superseded by targeted **radiotherapy** in the management of this malignancy.
*Sequential surgery: abdominoperineal resection then inguinal dissection*
- **Abdominoperineal resection (APR)** is now considered **salvage therapy** for persistent or recurrent disease after definitive chemoradiotherapy rather than a first-line treatment.
- Sequential surgeries increase the risk of **wound complications** and **lymphedema** without offering a survival benefit over conservative chemoradiation in SCC.
*Radiation to inguinal nodes only with surgical resection of pelvic nodes*
- Splitting treatment between radiation for one basin and surgery for another increases **treatment toxicity** and delays the start of systemic chemotherapy.
- Both **inguinal and pelvic nodal basins** are exquisitely **radiosensitive** in anal SCC, so the entire region is standardly managed with integrated radiation fields.
More Thoracic lymphatic drainage US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.