Principles of lymphatic circulation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Principles of lymphatic circulation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
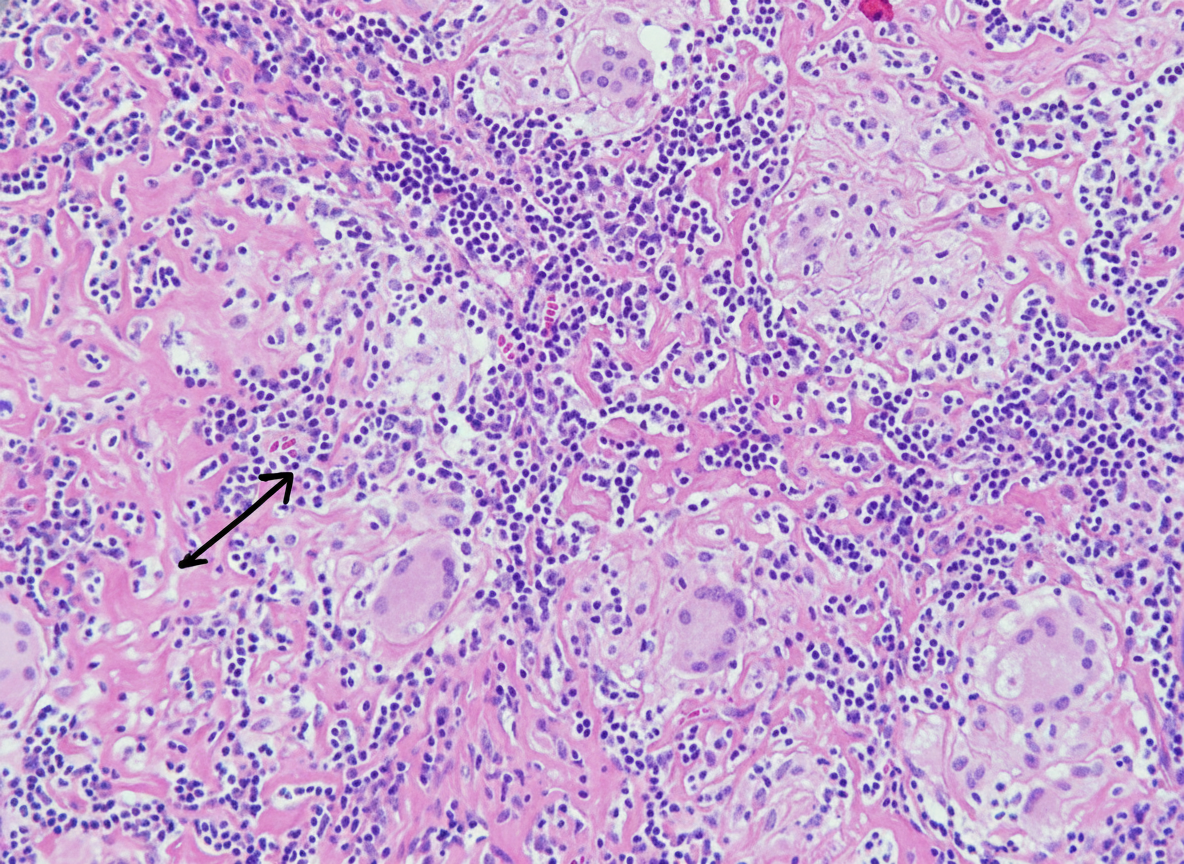
Principles of lymphatic circulation US Medical PG Question 1: A 32-year-old man who recently emigrated from Somalia comes to the physician because of a 4-week history of fever, cough, and chest pain. He has had a 5-kg (11-lb) weight loss over the last 3 months despite no changes in appetite. His temperature is 38.1°C (100.6°F). Physical examination shows enlarged cervical lymph nodes. The lungs are clear to auscultation. The results of an interferon-γ release assay are positive. An x-ray of the chest shows bilateral mediastinal lymphadenopathy. A transbronchial needle aspiration biopsy of a mediastinal lymph node is performed; a photomicrograph of the specimen is shown. The structure indicated by the arrow is most likely comprised of which of the following types of cells?
- A. Natural killer cells
- B. B cells
- C. Fibroblasts
- D. Neutrophils
- E. Macrophages (Correct Answer)
Principles of lymphatic circulation Explanation: ***Macrophages***
- The photomicrograph shows a **granuloma**, characterized by collections of **epithelioid histiocytes** (modified macrophages) and **multinucleated giant cells**, which are essentially fused macrophages.
- This morphology, coupled with the clinical picture of fever, cough, weight loss, positive interferon-γ release assay, and mediastinal lymphadenopathy in a patient from an endemic area, is highly suggestive of **tuberculosis**, a classic granulomatous disease.
*Natural killer cells*
- Natural killer cells are part of the innate immune system and are primarily involved in **killing virally infected cells** and **tumor cells**.
- They are not the primary cellular component forming the characteristic structure of a granuloma.
*B cells*
- B cells are responsible for **antibody production** and antigen presentation.
- While B cells may be present in the periphery of a granuloma, they do not form the core epithelioid and giant cell components.
*Fibroblasts*
- Fibroblasts produce **collagen** and the extracellular matrix, playing a role in **scar formation** and the fibrotic wall that can surround chronic granulomas.
- They do not constitute the primary cellular components of the inflammatory core of a granuloma.
*Neutrophils*
- Neutrophils are typically associated with **acute inflammation** and bacterial infections, characterized by pus formation.
- They are not the predominant cell type in the organized structure of a **granuloma** found in tuberculosis.
Principles of lymphatic circulation US Medical PG Question 2: An investigator is studying the clearance of respiratory particles in healthy non-smokers. An aerosol containing radio-labeled particles that are small enough to reach the alveoli is administered to the subjects via a non-rebreather mask. A gamma scanner is then used to evaluate the rate of particle clearance from the lungs. The primary mechanism of particle clearance most likely involves which of the following cell types?
- A. Goblet cells
- B. Macrophages (Correct Answer)
- C. Club cells
- D. Type I pneumocytes
- E. Neutrophils
Principles of lymphatic circulation Explanation: ***Macrophages***
- **Alveolar macrophages** are the primary phagocytic cells in the alveoli responsible for clearing inhaled particles that reach this deepest part of the lung.
- They engulf and digest foreign substances, including pathogens and inert particles, protecting the delicate alveolar structures.
*Goblet cells*
- **Goblet cells** are found in the larger airways (trachea, bronchi), where they produce mucus to trap inhaled particles.
- They are not present in the alveoli, so they cannot clear particles that have reached this region.
*Club cells*
- **Club cells** (formerly Clara cells) are located in the bronchioles and secrete components of the surfactant-like material, but they do not primarily function in particle clearance.
- While they have some protective roles, they are not the main phagocytic cells for alveolar particles.
*Type I pneumocytes*
- **Type I pneumocytes** are flattened, thin cells that form the majority of the alveolar surface and are primarily involved in gas exchange.
- They are not phagocytic and do not play a direct role in clearing inhaled particles.
*Neutrophils*
- **Neutrophils** are acute inflammatory cells primarily involved in combating bacterial infections.
- While they can migrate to the lungs during inflammation, they are not the primary, routine phagocytic cells for clearing inhaled particles in healthy individuals.
Principles of lymphatic circulation US Medical PG Question 3: Two weeks after undergoing low anterior resection for rectal cancer, a 52-year-old man comes to the physician because of swelling in both feet. He has not had any fever, chills, or shortness of breath. His temperature is 36°C (96.8°F) and pulse is 88/min. Physical examination shows a normal thyroid and no jugular venous distention. Examination of the lower extremities shows bilateral non-pitting edema that extends from the feet to the lower thigh, with deep flexion creases. His skin is warm and dry, and there is no erythema or rash. Microscopic examination of the interstitial space in this patient's lower extremities would be most likely to show the presence of which of the following?
- A. Neutrophilic, protein-rich fluid
- B. Lymphocytic, hemosiderin-rich fluid
- C. Lipid-rich, protein-rich fluid (Correct Answer)
- D. Protein-rich, glycosaminoglycan-rich fluid
- E. Acellular, protein-poor fluid
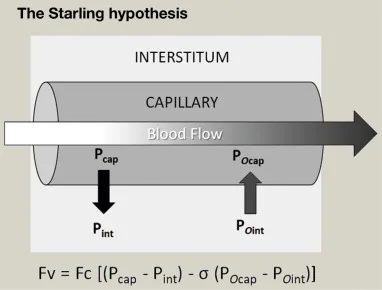
Principles of lymphatic circulation Explanation: ***Lipid-rich, protein-rich fluid***
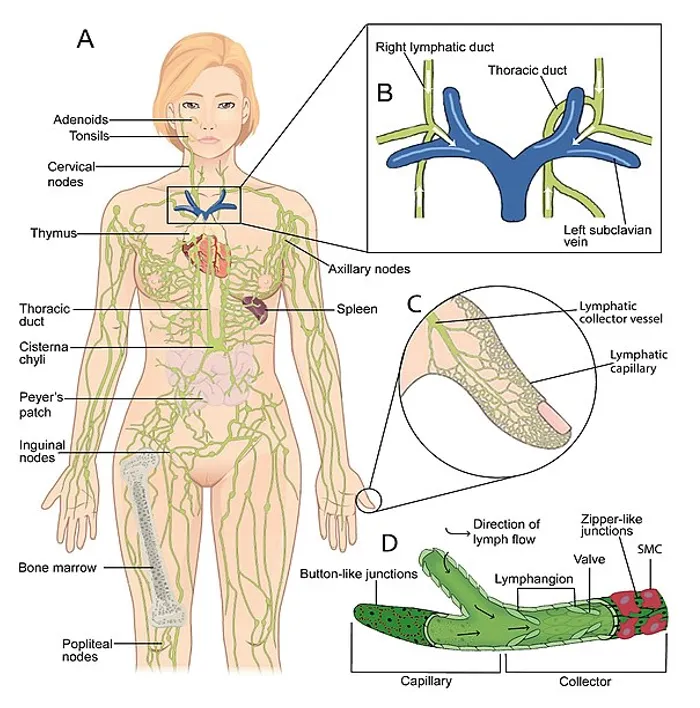
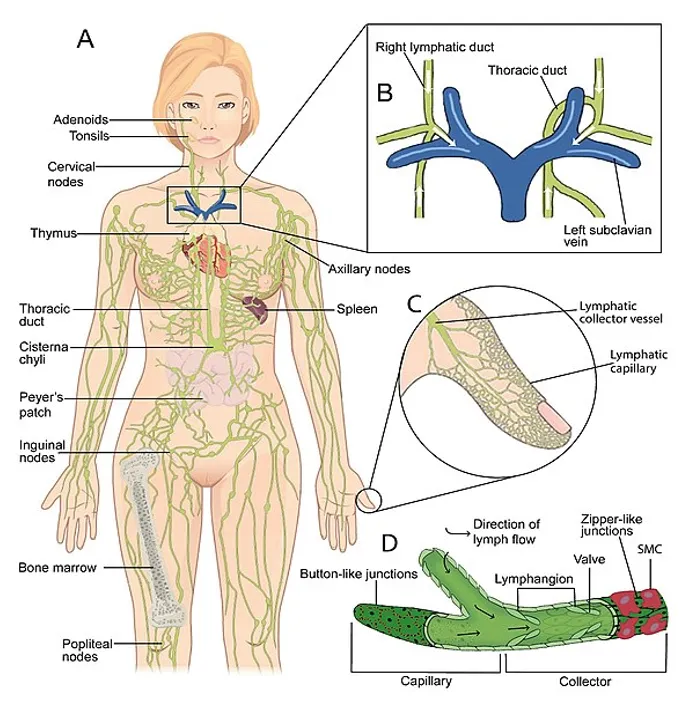
- The presentation of bilateral non-pitting edema extending to the thigh, with deep flexion creases, in a patient post-**low anterior resection** for rectal cancer, strongly suggests **lymphedema**.
- Lymphedema results from impaired lymphatic drainage, leading to the accumulation of **protein-rich fluid**, **macromolecules**, and **adipose tissue** in the interstitial space, which eventually becomes lipid-rich due to chronic inflammation and fibroblasts stimulating adipogenesis.
*Neutrophilic, protein-rich fluid*
- This description is characteristic of **inflammatory edema** or **purulent exudate**, typically seen in infections.
- The patient's lack of fever, chills, erythema, or warmth makes an infectious or acute inflammatory process unlikely.
*Lymphocytic, hemosiderin-rich fluid*
- **Hemosiderin deposits** are indicative of chronic **venous insufficiency** or recurrent hemorrhages, leading to red blood cell extravasation and breakdown.
- While lymphocytes can be present in chronic inflammation, the primary issue here is lymphatic obstruction, not venous stasis or bleeding.
*Protein-rich, glycosaminoglycan-rich fluid*
- While lymphedema is indeed **protein-rich**, the primary accumulation in mature lymphedema involves **adipose tissue** and fibrosis.
- **Glycosaminoglycans** accumulate significantly in conditions like **myxedema** (hypothyroidism), which was ruled out by the normal thyroid examination.
*Acellular, protein-poor fluid*
- This describes a **transudate**, typically seen in conditions like **heart failure**, **liver cirrhosis**, or **nephrotic syndrome** where there's an imbalance of hydrostatic and oncotic pressures.
- The edema in this case is **non-pitting**, suggesting a higher protein content and tissue changes characteristic of lymphatic dysfunction, not systemic fluid overload leading to protein-poor fluid.
Principles of lymphatic circulation US Medical PG Question 4: A 50-year-old man undergoes parathyroidectomy for treatment-resistant hyperparathyroidism. The procedure is complicated by brisk bleeding from the superior thyroid artery near the external branch of the superior laryngeal nerve. To stop the bleeding, the artery is ligated at its origin. Which of the following is most likely the origin of the artery that was injured in this patient?
- A. Thyrocervical trunk
- B. Ascending pharyngeal artery
- C. Internal carotid artery
- D. Subclavian artery
- E. External carotid artery (Correct Answer)
Principles of lymphatic circulation Explanation: ***External carotid artery***
- The **superior thyroid artery** is the first branch to arise from the **external carotid artery** in the neck.
- Ligation of this artery at its origin is a common surgical maneuver to control bleeding during thyroid or parathyroid surgery.
*Thyrocervical trunk*
- The **thyrocervical trunk** is a branch of the **subclavian artery** and gives rise to the inferior thyroid artery, not the superior thyroid artery.
- Injury to the superior thyroid artery would not necessitate ligation of a vessel originating from the thyrocervical trunk.
*Ascending pharyngeal artery*
- The **ascending pharyngeal artery** is a small artery that branches from the **external carotid artery** but supplies the pharynx, not the thyroid gland.
- It is not typically implicated in bleeding during parathyroidectomy or in relation to the superior laryngeal nerve.
*Internal carotid artery*
- The **internal carotid artery** primarily supplies the brain and does not have branches in the neck that supply the thyroid or parathyroid glands.
- It arises from the common carotid artery but does not give off the superior thyroid artery.
*Subclavian artery*
- The **subclavian artery** gives rise to the **thyrocervical trunk**, which then supplies the inferior thyroid artery, but not directly the superior thyroid artery.
- The superior thyroid artery originates higher up from the external carotid artery.
Principles of lymphatic circulation US Medical PG Question 5: A 35-year-old woman volunteers for a study on respiratory physiology. Pressure probes A and B are placed as follows:
Probe A: between the parietal and visceral pleura
Probe B: within the cavity of an alveolus
The probes provide a pressure reading relative to atmospheric pressure. To obtain a baseline reading, she is asked to sit comfortably and breathe normally. Which of the following sets of values will most likely be seen at the end of inspiration?
- A. Probe A: -6 mm Hg; Probe B: 0 mm Hg (Correct Answer)
- B. Probe A: 0 mm Hg; Probe B: -1 mm Hg
- C. Probe A: -4 mm Hg; Probe B: 0 mm Hg
- D. Probe A: -4 mm Hg; Probe B: -1 mm Hg
- E. Probe A: -6 mm Hg; Probe B: -1 mm Hg
Principles of lymphatic circulation Explanation: ***Probe A: -6 mm Hg; Probe B: 0 mm Hg***
- At the **end of inspiration**, the **intrapleural pressure (Probe A)** is at its most negative, typically around -6 to -8 cm H2O (equivalent to -4 to -6 mmHg), reflecting the maximum expansion of the thoracic cavity.
- At the **end of inspiration**, just before exhalation begins, there is **no airflow**, so the **intrapulmonary pressure (Probe B)** equalizes with atmospheric pressure, resulting in a 0 mm Hg reading.
*Probe A: 0 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of 0 mm Hg** would indicate a **pneumothorax** since it should always be negative to prevent lung collapse.
- An **intrapulmonary pressure of -1 mm Hg** would indicate that **inspiration is still ongoing**, as air would be flowing into the lungs.
*Probe A: -4 mm Hg; Probe B: 0 mm Hg*
- While an **intrapulmonary pressure of 0 mm Hg** is correct at the end of inspiration, an **intrapleural pressure of -4 mm Hg** is typical for the **end of expiration (Functional Residual Capacity)** during quiet breathing, not the end of inspiration.
- The **intrapleural pressure becomes more negative** during inspiration due to increased thoracic volume, so -4 mm Hg would be insufficient.
*Probe A: -4 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of -4 mm Hg** is the normal pressure at the **end of expiration**, not the end of inspiration, where it becomes more negative.
- An **intrapulmonary pressure of -1 mm Hg** indicates that **inspiration is still in progress**, not at its end, as air would still be flowing into the lungs.
*Probe A: -6 mm Hg; Probe B: -1 mm Hg*
- While an **intrapleural pressure of -6 mm Hg** is consistent with the end of inspiration, an **intrapulmonary pressure of -1 mm Hg** means that **airflow is still occurring into the lungs**.
- At the **very end of inspiration**, just before the start of exhalation, airflow momentarily ceases, and intrapulmonary pressure becomes zero relative to the atmosphere.
Principles of lymphatic circulation US Medical PG Question 6: A 65-year-old man presents with painless swelling of the neck over the past week. He also has noted severe night sweats, which require a change of clothes and bed linens the next day. His medical history is significant for long-standing hypertension. He received a kidney transplant 6 years ago. His current medications include amlodipine, metoprolol, furosemide, aspirin, tacrolimus, and mycophenolate. His family history is significant for his sister, who died last year from lymphoma. A review of systems is positive for a 6-kg (13.2-lb) unintentional weight loss over the past 2 months. His vital signs include: temperature 37.8°C (100.0°F) and blood pressure 120/75 mm Hg. On physical examination, there are multiple painless lymph nodes, averaging 2 cm in diameter, palpable in the anterior and posterior triangles of the neck bilaterally. Axillary and inguinal lymphadenopathy is palpated on the right side. Abdominal examination is significant for a spleen of 16 cm below the costal margin on percussion. Laboratory studies are significant for the following:
Hemoglobin 9 g/dL
Mean corpuscular volume 88 μm3
Leukocyte count 12,000/mm3
Platelet count 130,000/mm3
Creatinine 1.1 mg/dL
Lactate dehydrogenase (LDH) 1,000 U/L
A peripheral blood smear is unremarkable. Which of the following is the most likely diagnosis in this patient?
- A. Multiple myeloma
- B. Non-Hodgkin’s lymphoma (NHL) (Correct Answer)
- C. Drug-induced lymphadenopathy
- D. Chronic lymphocytic leukemia (CLL)
- E. Cytomegalovirus infection
Principles of lymphatic circulation Explanation: ***Non-Hodgkin’s lymphoma (NHL)***
- This patient presents with **B symptoms** (**unintentional weight loss**, **night sweats**, fever), diffuse **lymphadenopathy**, and **splenomegaly**, which are classic signs of lymphoma. Elevated **LDH** and a history of kidney transplant requiring immunosuppression (tacrolimus, mycophenolate) significantly increase the risk of **post-transplant lymphoproliferative disorder (PTLD)**, a type of NHL.
- The **anemia**, **thrombocytopenia**, and **leukocytosis** (with an otherwise unremarkable peripheral smear) are consistent with bone marrow involvement or chronic disease in lymphoma.
*Multiple myeloma*
- Multiple myeloma is a plasma cell dyscrasia characterized by **bone pain**, **renal failure**, **hypercalcemia**, and **anemia**. While anemia and potential renal impairment are present, the widespread lymphadenopathy and splenomegaly are not typical features.
- The elevated LDH and presence of B symptoms are more indicative of lymphoma than multiple myeloma.
*Drug-induced lymphadenopathy*
- While some medications can cause lymphadenopathy, it is typically less severe, often without systemic B symptoms, and usually resolves upon discontinuation of the causative drug.
- The combination of severe B symptoms, impressive splenomegaly, and significantly elevated LDH points to a more aggressive underlying malignancy rather than a drug reaction.
*Chronic lymphocytic leukemia (CLL)*
- CLL is characterized by a persistent **lymphocytosis** (often >5,000 mature lymphocytes/µL) on peripheral smear, which is not described here ("unremarkable").
- While CLL can cause lymphadenopathy and splenomegaly, the rapid onset of severe B symptoms and the extremely high LDH are more suggestive of an aggressive lymphoma rather than indolent CLL.
*Cytomegalovirus infection*
- CMV infection can cause lymphadenopathy, fever, and fatigue, particularly in immunocompromised patients. However, the degree of **weight loss**, **splenomegaly**, and elevated **LDH** seen here are uncharacteristic of CMV infection and point towards a more serious underlying malignancy.
- CMV typically presents with a more acute, mononucleosis-like illness and often lymphocytosis with atypical lymphocytes on peripheral smear.
Principles of lymphatic circulation US Medical PG Question 7: A 34-year-old man comes to the physician because of progressive swelling of the left lower leg for 4 months. One year ago, he had an episode of intermittent fever and tender lymphadenopathy that occurred shortly after he returned from a trip to India and resolved spontaneously. Physical examination shows 4+ nonpitting edema of the left lower leg. His leukocyte count is 8,000/mm3 with 25% eosinophils. A blood smear obtained at night confirms the diagnosis. Treatment with diethylcarbamazine is initiated. Which of the following is the most likely route of transmission of the causal pathogen?
- A. Penetration of the skin by hookworms in feces
- B. Penetration of the skin by cercariae from contaminated fresh water
- C. Deposition of larvae into the skin by a female black fly
- D. Ingestion of encysted larvae in undercooked pork
- E. Deposition of thread-like larvae into the skin by a female mosquito (Correct Answer)
Principles of lymphatic circulation Explanation: ***Deposition of thread-like larvae into the skin by a female mosquito***
- The symptoms described, including progressive **nonpitting edema** (lymphedema), a history of **fever** and **lymphadenopathy** after travel to an endemic area (India), and significant **eosinophilia**, are classic for **lymphatic filariasis**.
- Lymphatic filariasis, caused by filarial worms like *Wuchereria bancrofti* or *Brugia malayi*, is transmitted by **mosquitoes** that deposit infectious larvae onto the skin during a blood meal.
*Penetration of the skin by hookworms in feces*
- This describes the transmission of **hookworm infection**, which causes **iron deficiency anemia** and gastrointestinal symptoms, not lymphedema or high eosinophilia with nocturnal microfilaremia.
- While hookworms can cause eosinophilia, the clinical presentation of chronic lymphedema and the need for a nocturnal blood smear point away from hookworm infection.
*Penetration of the skin by cercariae from contaminated fresh water*
- This is the transmission method for **schistosomiasis**, which can cause symptoms depending on the species and affected organs, such as **urinary tract disease**, **hepatic fibrosis**, or **intestinal inflammation**.
- Schistosomiasis does not typically present with the progressive lymphedema and episodic lymphadenitis characteristic of filariasis.
*Deposition of larvae into the skin by a female black fly*
- This describes the transmission of **onchocerciasis** (river blindness), caused by *Onchocerca volvulus*.
- Onchocerciasis primarily causes skin disease (intense **pruritus**, dermatitis) and **ocular lesions** leading to blindness, not extensive lymphedema of the limbs.
*Ingestion of encysted larvae in undercooked pork*
- This is the route of transmission for **trichinellosis**, caused by *Trichinella spiralis*.
- Trichinellosis involves **muscle pain**, fever, and periorbital edema, but not chronic lymphedema of the extremities or the specific nocturnal periodicity for diagnosis.
Principles of lymphatic circulation US Medical PG Question 8: A 76-year-old woman comes to the physician for evaluation of a 3-month history of vulvar itching and pain. She was diagnosed with lichen sclerosus 4 years ago. She has smoked 1 pack of cigarettes daily for 35 years. Physical examination shows a 2.5-cm nodular, ulcerative lesion on the vaginal introitus and left labia minora with surrounding erythema. Punch biopsy shows squamous cell carcinoma. A CT scan of the chest, abdomen, and pelvis shows enlarged lymph nodes concerning for metastatic disease. Which of the following lymph node regions is the most likely primary site of metastasis?
- A. Superficial inguinal (Correct Answer)
- B. Internal iliac
- C. External iliac
- D. Inferior mesenteric
- E. Para-aortic
Principles of lymphatic circulation Explanation: ***Superficial inguinal***
- The **vulva** drains primarily into the **superficial inguinal lymph nodes**, making them the most likely first site for metastatic spread from vulvar squamous cell carcinoma.
- The lesion's location on the **vaginal introitus** and **labia minora** directly correlates with this lymphatic drainage pathway.
*Internal iliac*
- **Internal iliac nodes** receive drainage mainly from deep pelvic structures like the cervix, upper vagina, and uterus, not directly from the vulva.
- Metastasis to these nodes usually occurs after involvement of more superficial nodes or in advanced disease with deeper invasion.
*External iliac*
- **External iliac nodes** generally drain the lower extremities and deeper pelvic structures (e.g., bladder, distal ureter), not the vulva as a primary site.
- Involvement here would typically indicate more advanced local spread or secondary metastasis from other pelvic nodes.
*Inferior mesenteric*
- **Inferior mesenteric nodes** drain the hindgut and its derivatives, including the distal colon and rectum, which are distant from the vulva.
- This region is not involved in the lymphatic drainage of the vulva.
*Para-aortic*
- **Para-aortic nodes** drain structures like the ovaries, fallopian tubes, and upper uterus; they are too superior for primary vulvar lymphatic drainage.
- Metastasis to these nodes from vulvar cancer would signify widespread, very advanced disease and not a primary site of spread.
Principles of lymphatic circulation US Medical PG Question 9: A 44-year-old woman undergoes radical hysterectomy for stage IB2 cervical cancer. During surgery, the gynecologic oncologist notes aberrant lymphatic drainage patterns possibly related to the patient's history of pelvic inflammatory disease and previous cesarean section. Frozen section of a lymph node from the obturator fossa shows metastatic disease. Synthesizing knowledge of primary and collateral cervical lymphatic drainage, which nodal group represents the most critical next level of drainage that would impact surgical decision-making?
- A. Presacral nodes via uterosacral ligament pathway
- B. Common iliac and para-aortic nodes via external iliac pathway (Correct Answer)
- C. Internal iliac nodes only
- D. Inguinal nodes via deep femoral pathway
- E. Superficial inguinal nodes via round ligament pathway
Principles of lymphatic circulation Explanation: ***Common iliac and para-aortic nodes via external iliac pathway***
- The **common iliac nodes** serve as the primary drainage destination from both the **external iliac** and **obturator nodes**, making them the critical next level when **obturator metastasis** is confirmed.
- Lymphatic spread in cervical cancer typically follows a regular pattern: primary pelvic nodes (obturator, external/internal iliacs) move toward the **common iliac** and then **para-aortic** regions.
*Superficial inguinal nodes via round ligament pathway*
- Drainage to these nodes occurs primarily from the **uterine horns** or the **vulva**, not typically the cervix unless the tumor involves the lower vagina.
- These nodes are not part of the standard cephalad **retroperitoneal spread** pathway for stage IB2 cervical cancer.
*Presacral nodes via uterosacral ligament pathway*
- These nodes provide a minor primary drainage route via the **uterosacral ligaments**, but they are anatomically distinct from the lateral **obturator fossa** chain.
- They do not represent the "next level" of drainage that would indicate **systemic progression** beyond the pelvic basin.
*Internal iliac nodes only*
- The **internal iliac nodes** are primary pelvic nodes and are considered on the **same drainage tier** as the obturator nodes already found to be positive.
- Assessing these nodes only would not provide enough information regarding the **cephalad extent** of the disease required for surgical modification.
*Inguinal nodes via deep femoral pathway*
- The **deep femoral pathway** primarily drains the lower limb and vulva rather than the **cervical stroma** and parametrium.
- Involvement of these nodes would be an exception and would not help in determining the transition to **extended-field radiation** for retroperitoneal disease.
Principles of lymphatic circulation US Medical PG Question 10: A 67-year-old man with squamous cell carcinoma of the anal canal presents for staging. Physical examination reveals a 3 cm tumor at the dentate line extending both above and below it. Inguinal lymphadenopathy is palpable bilaterally. CT shows both inguinal and pelvic lymph node enlargement. Evaluating the lymphatic drainage of the anal canal, which treatment approach best addresses the dual drainage patterns of this tumor location?
- A. Chemoradiation targeting both inguinal and pelvic nodal basins (Correct Answer)
- B. Pelvic lymph node dissection only, following inferior mesenteric pathways
- C. Sequential surgery: abdominoperineal resection then inguinal dissection
- D. Radiation to inguinal nodes only with surgical resection of pelvic nodes
- E. Inguinal lymph node dissection only, as anal tumors drain superficially
Principles of lymphatic circulation Explanation: ***Chemoradiation targeting both inguinal and pelvic nodal basins***
- Tumors at the **dentate line** exhibit dual lymphatic drainage: the area above drains to **internal iliac** and **perirectal nodes**, while the area below drains to **superficial inguinal nodes**.
- The standard of care for anal **squamous cell carcinoma** (SCC) is the **Nigro protocol**, which uses **definitive chemoradiotherapy** to treat both the primary tumor and all involved regional nodal basins.
*Inguinal lymph node dissection only, as anal tumors drain superficially*
- While the area below the dentate line drains to **inguinal nodes**, the area above drains into the **pelvis**, meaning a dissection limited to the groin would miss half of the drainage pathway.
- Surgical dissection is not the primary treatment for anal SCC, as **chemoradiation** offers high rates of cure while preserving anal sphincter function.
*Pelvic lymph node dissection only, following inferior mesenteric pathways*
- This approach neglects the **superficial inguinal nodes**, which are already palpably enlarged in this patient and are the primary drainage route for the inferior anal canal.
- **Pelvic lymph node dissection** is technically difficult and carries high morbidity; it has been largely superseded by targeted **radiotherapy** in the management of this malignancy.
*Sequential surgery: abdominoperineal resection then inguinal dissection*
- **Abdominoperineal resection (APR)** is now considered **salvage therapy** for persistent or recurrent disease after definitive chemoradiotherapy rather than a first-line treatment.
- Sequential surgeries increase the risk of **wound complications** and **lymphedema** without offering a survival benefit over conservative chemoradiation in SCC.
*Radiation to inguinal nodes only with surgical resection of pelvic nodes*
- Splitting treatment between radiation for one basin and surgery for another increases **treatment toxicity** and delays the start of systemic chemotherapy.
- Both **inguinal and pelvic nodal basins** are exquisitely **radiosensitive** in anal SCC, so the entire region is standardly managed with integrated radiation fields.
More Principles of lymphatic circulation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.