Lymphedema pathophysiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lymphedema pathophysiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lymphedema pathophysiology US Medical PG Question 1: A 52-year-old man presents to the emergency department because of pain and swelling in his left leg over the past few hours. He traveled from Sydney to Los Angeles 2 days ago. He has had type 2 diabetes mellitus for 10 years and takes metformin for it. He has smoked a pack of cigarettes daily for 25 years. His temperature is 36.9°C (98.4°F), the blood pressure is 140/90 mm Hg, and the pulse is 90/min. On examination, the left calf is 5 cm greater in circumference than the right. The left leg appears more erythematous than the right with dilated superficial veins. Venous duplex ultrasound shows non-compressibility. Which of the following best represents the mechanism of this patient’s illness?
- A. Impaired venous blood flow (Correct Answer)
- B. Subcutaneous soft-tissue infection that may extend to the deep fascia
- C. Infection of the dermis and subcutaneous tissues
- D. Impaired arterial blood flow
- E. Impaired lymphatic flow
Lymphedema pathophysiology Explanation: ***Impaired venous blood flow***
- The patient's symptoms (unilateral leg pain and swelling, erythema, dilated superficial veins, recent long-haul travel) and the **venous duplex ultrasound** finding of **non-compressibility** are highly indicative of **deep vein thrombosis (DVT)**, which results from impaired venous outflow.
- Risk factors such as **long-haul travel** (venous stasis), **smoking** (endothelial damage), and potentially **diabetes** contribute to a hypercoagulable state.
*Impaired lymphatic flow*
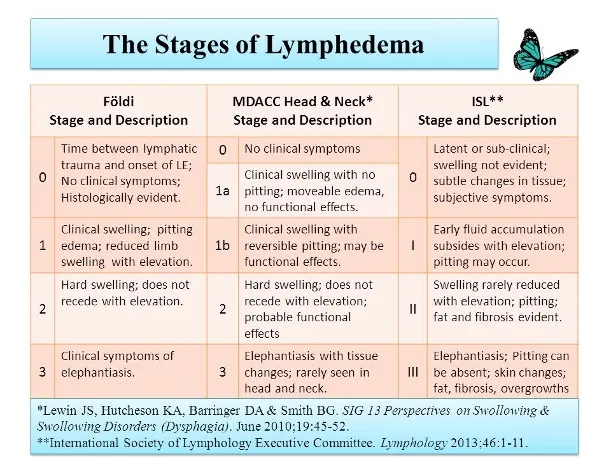
- This typically presents as **lymphedema**, characterized by chronic, often pitting edema, and skin changes like thickening (peau d'orange), but usually without acute erythema or dilated superficial veins in this context.
- **Venous duplex ultrasound** would not show non-compressibility in cases of impaired lymphatic flow, as veins themselves would be clear.
*Subcutaneous soft-tissue infection that may extend to the deep fascia*
- This describes **necrotizing fasciitis**, a severe infection often characterized by rapid progression, severe pain disproportionate to examination findings, blistering, and systemic toxicity, which are not clearly evident here.
- While there is erythema, the key diagnostic finding is the **non-compressible vein**, not signs of crepitus or rapidly spreading infection.
*Infection of the dermis and subcutaneous tissues*
- This describes **cellulitis**, which presents with localized redness, warmth, swelling, and tenderness, often with an entry point.
- While some symptoms overlap (erythema, swelling), the **venous duplex ultrasound finding of non-compressibility** definitively points away from a simple skin infection and towards a vascular obstruction.
*Impaired arterial blood flow*
- This presents as **acute limb ischemia**, characterized by the "6 Ps": pain, pallor, pulselessness, paresthesias, poikilothermia (coldness), and paralysis.
- The patient's leg is swollen and erythematous, not pale and cold, and the ultrasound directly implicates venous rather than arterial occlusion.
Lymphedema pathophysiology US Medical PG Question 2: A 76-year-old woman is brought to the physician because of lesions on her left arm. She first noticed them 3 months ago and they have grown larger since that time. She has not had any pain or pruritus in the area. She has a history of invasive ductal carcinoma of the left breast, which was treated with mastectomy and radiation therapy 27 years ago. Since that time, she has had lymphedema of the left arm. Physical examination shows extensive edema of the left arm. There are four coalescing, firm, purple-blue nodules on the left lateral axillary region and swelling of the surrounding skin. Which of the following is the most likely diagnosis?
- A. Thrombophlebitis
- B. Cellulitis
- C. Melanoma
- D. Angiosarcoma (Correct Answer)
- E. Kaposi sarcoma
Lymphedema pathophysiology Explanation: ***Angiosarcoma***
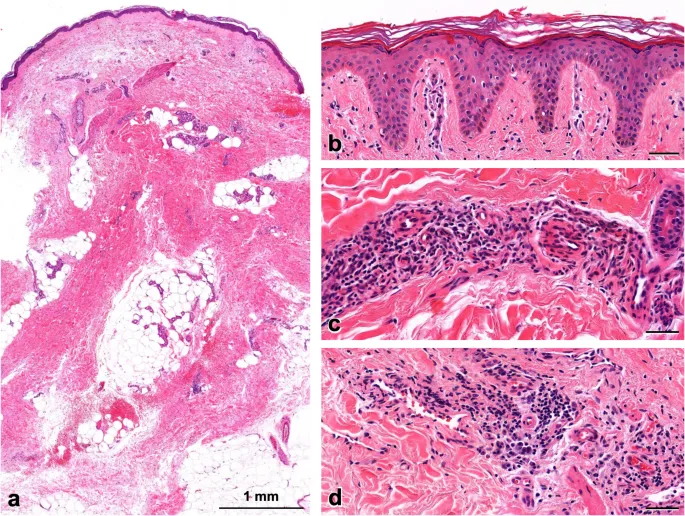
- The presence of **firm, purple-blue nodules** in a patient with **chronic lymphedema** following **mastectomy and radiation** for breast cancer is highly suggestive of **angiosarcoma (Stewart-Treves syndrome)**.
- This rare but aggressive vascular malignancy often presents as skin lesions in the setting of long-standing lymphedema, particularly in the upper extremity after breast cancer treatment.
*Thrombophlebitis*
- Typically presents with **erythema**, **tenderness**, and **pain** along the course of a superficial vein, which is not described here.
- The lesions would likely blanch with pressure and feel more like a cord or streak, rather than firm, discrete nodules.
*Cellulitis*
- Would present with **warmth**, **tenderness**, **erythema with ill-defined borders**, and often **fever**, none of which are mentioned.
- While lymphedema is a risk factor for cellulitis, the description of discrete, firm, purple-blue nodules growing over time is not characteristic.
*Melanoma*
- Although melanoma can present as a dark lesion, it often has **irregular borders**, **asymmetry**, and **color variegation**, and is typically associated with UV exposure.
- While it can be nodular, the specific context of chronic lymphedema and the description of purple-blue lesions are more indicative of a vascular tumor.
*Kaposi sarcoma*
- Characterized by **purple-brown skin lesions** and is primarily associated with **HIV infection** or **immunosuppression**, neither of which is indicated in this patient.
- While it is a vascular tumor, the unique presentation in the context of chronic lymphedema post-breast cancer therapy makes angiosarcoma a more fitting diagnosis.
Lymphedema pathophysiology US Medical PG Question 3: A 93-year-old woman is brought to the physician because of a purple area on her right arm that has been growing for one month. She has not had any pain or itching of the area. She has hyperlipidemia, a history of basal cell carcinoma treated with Mohs surgery 2 years ago, and a history of invasive ductal carcinoma of the right breast treated with radical mastectomy 57 years ago. She has had chronic lymphedema of the right upper extremity since the mastectomy. Her only medication is simvastatin. She lives in an assisted living facility. She is content with her living arrangement but feels guilty that she is dependent on others. Vital signs are within normal limits. Physical examination shows extensive edema of the right arm. Skin exam of the proximal upper right extremity shows three coalescing, 0.5–1.0 cm heterogeneous, purple-colored plaques with associated ulceration. Which of the following is the most likely diagnosis?
- A. Lymphangiosarcoma (Correct Answer)
- B. Cellulitis
- C. Thrombophlebitis
- D. Kaposi sarcoma
- E. Lichen planus
Lymphedema pathophysiology Explanation: ***Lymphangiosarcoma***
- This patient presents with a **purple area** with **ulceration** on an arm affected by chronic **lymphedema** following a mastectomy. This constellation of findings is highly suggestive of **Stewart-Treves syndrome**, which is a rare but aggressive form of angiosarcoma (lymphangiosarcoma) arising in the setting of chronic lymphedema.
- The history of **radical mastectomy 57 years ago** with subsequent **chronic right upper extremity lymphedema** strongly predisposes to this condition, especially given the lack of pain or itching and the progressive nature of the lesion.
*Cellulitis*
- Characterized by **erythema**, **warmth**, **pain**, and **tenderness**, often with fever and systemic symptoms, none of which are described.
- While lymphedema is a risk factor for cellulitis, the description of a **purple, ulcerated plaque** with a duration of one month is inconsistent with acute bacterial infection.
*Thrombophlebitis*
- Typically presents with **pain**, **tenderness**, **erythema**, and a palpable cord-like vein along the course of a superficial vein, which is not described.
- The lesion described is a spreading, **ulcerated plaque**, not a discrete inflamed vein.
*Kaposi sarcoma*
- While it can present with **purple lesions**, Kaposi sarcoma is typically associated with **immunosuppression** (e.g., HIV infection) or certain endemic regions, neither of which is mentioned.
- The strong association with **chronic lymphedema** in this case makes lymphangiosarcoma a more specific diagnosis.
*Lichen planus*
- A chronic inflammatory condition characterized by **pruritic, purple, polygonal, planar papules and plaques (the 6 Ps)**, often with fine white lines (Wickham's striae).
- It does not typically present as a growing, **ulcerated purple plaque** in the setting of chronic lymphedema, and itching is a prominent symptom.
Lymphedema pathophysiology US Medical PG Question 4: Two weeks after undergoing low anterior resection for rectal cancer, a 52-year-old man comes to the physician because of swelling in both feet. He has not had any fever, chills, or shortness of breath. His temperature is 36°C (96.8°F) and pulse is 88/min. Physical examination shows a normal thyroid and no jugular venous distention. Examination of the lower extremities shows bilateral non-pitting edema that extends from the feet to the lower thigh, with deep flexion creases. His skin is warm and dry, and there is no erythema or rash. Microscopic examination of the interstitial space in this patient's lower extremities would be most likely to show the presence of which of the following?
- A. Neutrophilic, protein-rich fluid
- B. Lymphocytic, hemosiderin-rich fluid
- C. Lipid-rich, protein-rich fluid (Correct Answer)
- D. Protein-rich, glycosaminoglycan-rich fluid
- E. Acellular, protein-poor fluid
Lymphedema pathophysiology Explanation: ***Lipid-rich, protein-rich fluid***
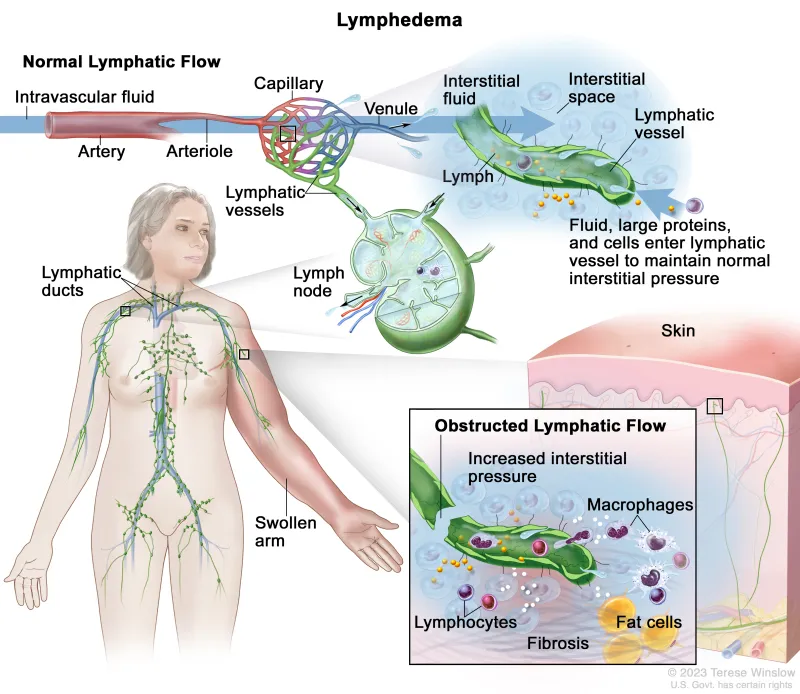
- The presentation of bilateral non-pitting edema extending to the thigh, with deep flexion creases, in a patient post-**low anterior resection** for rectal cancer, strongly suggests **lymphedema**.
- Lymphedema results from impaired lymphatic drainage, leading to the accumulation of **protein-rich fluid**, **macromolecules**, and **adipose tissue** in the interstitial space, which eventually becomes lipid-rich due to chronic inflammation and fibroblasts stimulating adipogenesis.
*Neutrophilic, protein-rich fluid*
- This description is characteristic of **inflammatory edema** or **purulent exudate**, typically seen in infections.
- The patient's lack of fever, chills, erythema, or warmth makes an infectious or acute inflammatory process unlikely.
*Lymphocytic, hemosiderin-rich fluid*
- **Hemosiderin deposits** are indicative of chronic **venous insufficiency** or recurrent hemorrhages, leading to red blood cell extravasation and breakdown.
- While lymphocytes can be present in chronic inflammation, the primary issue here is lymphatic obstruction, not venous stasis or bleeding.
*Protein-rich, glycosaminoglycan-rich fluid*
- While lymphedema is indeed **protein-rich**, the primary accumulation in mature lymphedema involves **adipose tissue** and fibrosis.
- **Glycosaminoglycans** accumulate significantly in conditions like **myxedema** (hypothyroidism), which was ruled out by the normal thyroid examination.
*Acellular, protein-poor fluid*
- This describes a **transudate**, typically seen in conditions like **heart failure**, **liver cirrhosis**, or **nephrotic syndrome** where there's an imbalance of hydrostatic and oncotic pressures.
- The edema in this case is **non-pitting**, suggesting a higher protein content and tissue changes characteristic of lymphatic dysfunction, not systemic fluid overload leading to protein-poor fluid.
Lymphedema pathophysiology US Medical PG Question 5: A 54-year-old man comes to the emergency department because of a 3-week history of intermittent swelling of his left arm and feeling of fullness in his head that is exacerbated by lying down and bending over to tie his shoes. Physical examination shows left-sided facial edema and distention of superficial veins in the neck and left chest wall. Which of the following is the most likely cause of this patient's symptoms?
- A. Cervical rib
- B. Mediastinal lymphoma
- C. Subclavian steal syndrome
- D. Apical lung tumor (Correct Answer)
- E. Right heart failure
Lymphedema pathophysiology Explanation: ***Apical lung tumor***
- The symptoms of **facial edema**, **neck vein distention**, and **swelling of the left arm**, particularly when exacerbated by positional changes such as lying down or bending over, are classic signs of **superior vena cava (SVC) syndrome**.
- An **apical lung tumor (Pancoast tumor)** is a common cause of SVC syndrome due to its proximity to the SVC and surrounding structures, leading to compression.
- The **left-sided predominance** (left arm swelling, left facial edema, left chest wall venous distention) specifically points to a left apical mass compressing the left brachiocephalic vein and/or SVC.
*Cervical rib*
- A cervical rib can cause **thoracic outlet syndrome**, leading to neurovascular compression, but it typically presents with neurological symptoms (pain, numbness, weakness in the arm/hand) or arterial insufficiency rather than widespread facial and neck edema.
- While it can cause *venous compression*, resulting in arm swelling, the **facial edema and neck vein distention** suggest a more central venous obstruction like SVC syndrome rather than peripheral thoracic outlet compression.
*Mediastinal lymphoma*
- Malignancies in the mediastinum, such as lymphoma, can indeed cause SVC syndrome by compressing the SVC.
- However, mediastinal lymphomas typically cause **bilateral** symptoms due to their central location, whereas this patient has **predominant left-sided findings** (left arm swelling, left facial edema, left chest wall veins), which more specifically suggests a left apical lung mass.
- Additionally, lymphoma commonly presents with systemic "B symptoms" (fever, night sweats, weight loss) and generalized lymphadenopathy, which are not mentioned here.
*Subclavian steal syndrome*
- This syndrome results from **subclavian artery stenosis** proximal to the vertebral artery origin, causing **retrograde blood flow** in the vertebral artery to supply the arm.
- It presents with **arm claudication**, dizziness, and syncope, especially with arm exercise, rather than venous congestion and swelling of the face, neck, and arm.
- This is an **arterial** syndrome, not a **venous** syndrome.
*Right heart failure*
- **Right heart failure** causes systemic venous congestion, leading to symptoms like **peripheral edema** (especially in the lower extremities), **jugular venous distention**, and **hepatomegaly**.
- While it can cause jugular venous distension, it typically presents with **bilateral lower extremity edema** and *rarely* causes unilateral arm swelling or predominant facial edema, as seen here.
- The **positional exacerbation** and **unilateral left-sided findings** are not characteristic of right heart failure.
Lymphedema pathophysiology US Medical PG Question 6: A 65-year-old man presents with painless swelling of the neck over the past week. He also has noted severe night sweats, which require a change of clothes and bed linens the next day. His medical history is significant for long-standing hypertension. He received a kidney transplant 6 years ago. His current medications include amlodipine, metoprolol, furosemide, aspirin, tacrolimus, and mycophenolate. His family history is significant for his sister, who died last year from lymphoma. A review of systems is positive for a 6-kg (13.2-lb) unintentional weight loss over the past 2 months. His vital signs include: temperature 37.8°C (100.0°F) and blood pressure 120/75 mm Hg. On physical examination, there are multiple painless lymph nodes, averaging 2 cm in diameter, palpable in the anterior and posterior triangles of the neck bilaterally. Axillary and inguinal lymphadenopathy is palpated on the right side. Abdominal examination is significant for a spleen of 16 cm below the costal margin on percussion. Laboratory studies are significant for the following:
Hemoglobin 9 g/dL
Mean corpuscular volume 88 μm3
Leukocyte count 12,000/mm3
Platelet count 130,000/mm3
Creatinine 1.1 mg/dL
Lactate dehydrogenase (LDH) 1,000 U/L
A peripheral blood smear is unremarkable. Which of the following is the most likely diagnosis in this patient?
- A. Multiple myeloma
- B. Non-Hodgkin’s lymphoma (NHL) (Correct Answer)
- C. Drug-induced lymphadenopathy
- D. Chronic lymphocytic leukemia (CLL)
- E. Cytomegalovirus infection
Lymphedema pathophysiology Explanation: ***Non-Hodgkin’s lymphoma (NHL)***
- This patient presents with **B symptoms** (**unintentional weight loss**, **night sweats**, fever), diffuse **lymphadenopathy**, and **splenomegaly**, which are classic signs of lymphoma. Elevated **LDH** and a history of kidney transplant requiring immunosuppression (tacrolimus, mycophenolate) significantly increase the risk of **post-transplant lymphoproliferative disorder (PTLD)**, a type of NHL.
- The **anemia**, **thrombocytopenia**, and **leukocytosis** (with an otherwise unremarkable peripheral smear) are consistent with bone marrow involvement or chronic disease in lymphoma.
*Multiple myeloma*
- Multiple myeloma is a plasma cell dyscrasia characterized by **bone pain**, **renal failure**, **hypercalcemia**, and **anemia**. While anemia and potential renal impairment are present, the widespread lymphadenopathy and splenomegaly are not typical features.
- The elevated LDH and presence of B symptoms are more indicative of lymphoma than multiple myeloma.
*Drug-induced lymphadenopathy*
- While some medications can cause lymphadenopathy, it is typically less severe, often without systemic B symptoms, and usually resolves upon discontinuation of the causative drug.
- The combination of severe B symptoms, impressive splenomegaly, and significantly elevated LDH points to a more aggressive underlying malignancy rather than a drug reaction.
*Chronic lymphocytic leukemia (CLL)*
- CLL is characterized by a persistent **lymphocytosis** (often >5,000 mature lymphocytes/µL) on peripheral smear, which is not described here ("unremarkable").
- While CLL can cause lymphadenopathy and splenomegaly, the rapid onset of severe B symptoms and the extremely high LDH are more suggestive of an aggressive lymphoma rather than indolent CLL.
*Cytomegalovirus infection*
- CMV infection can cause lymphadenopathy, fever, and fatigue, particularly in immunocompromised patients. However, the degree of **weight loss**, **splenomegaly**, and elevated **LDH** seen here are uncharacteristic of CMV infection and point towards a more serious underlying malignancy.
- CMV typically presents with a more acute, mononucleosis-like illness and often lymphocytosis with atypical lymphocytes on peripheral smear.
Lymphedema pathophysiology US Medical PG Question 7: A 67-year-old woman comes to the physician with a 6-month history of pain and swelling of both legs. The symptoms are worst at the end of the day and are associated with itching of the overlying skin. Physical examination shows bilateral pitting ankle edema. An image of one of the ankles is shown. This patient is at greatest risk for which of the following complications?
- A. Osmotic injury to the peripheral nerves
- B. Thrombosis of a deep vein
- C. Malignant transformation of lymphatic endothelium
- D. Biliverdin accumulation in the epidermis
- E. Ulceration of the cutis (Correct Answer)
Lymphedema pathophysiology Explanation: ***Ulceration of the cutis (skin)***
- This patient has **chronic venous insufficiency** with signs of **venous stasis dermatitis** (bilateral pitting edema, end-of-day worsening, pruritus)
- Chronic venous hypertension leads to skin breakdown and **venous stasis ulcers**, typically at the medial malleolus
- The 6-month duration, itching, and skin changes indicate progression toward ulceration - the **most common serious complication** of chronic venous insufficiency
- Venous ulcers develop in 3-5% of patients with chronic venous disease
*Osmotic injury to the peripheral nerves*
- Not a recognized complication of venous insufficiency
- Osmotic nerve injury occurs in conditions like **diabetes** with glucose-induced osmotic stress, unrelated to the venous pathology presented
*Thrombosis of a deep vein*
- While **venous stasis** is a risk factor for DVT (Virchow's triad), this patient has **chronic bilateral** findings suggesting longstanding venous insufficiency rather than acute thrombosis
- DVT typically presents with **unilateral**, acute-onset pain, warmth, and swelling
- Given the chronic presentation with skin changes, **ulceration is the greatest risk**
*Malignant transformation of lymphatic endothelium*
- Refers to **lymphangiosarcoma (Stewart-Treves syndrome)**, an extremely rare complication of **chronic lymphedema**, not venous insufficiency
- Would present with purple nodules and typically occurs after years of severe lymphatic obstruction
*Biliverdin accumulation in the epidermis*
- **Hemosiderin** (not biliverdin) deposition occurs in chronic venous insufficiency, causing brown hyperpigmentation (hemosiderin staining)
- However, this is a cosmetic finding, not a serious complication like ulceration
- Biliverdin is associated with bruising/hematoma resolution, not chronic venous disease
Lymphedema pathophysiology US Medical PG Question 8: A 23-year-old woman presents to her primary care physician with 3 days of fatigue and back pain after she started a drug for malaria prophylaxis. She says that her urine has also been darker over the same time period. Her past medical history is significant for allergies as well as a broken elbow that was treated in a cast 10 years ago. She does not take any medications, does not smoke, and drinks socially. Peripheral blood smear reveals both red blood cells with dark intracellular inclusions as well as abnormally shaped red blood cells. The immune cells responsible for the shape of these red blood cells are located in which of the following places?
- A. Lymph nodes
- B. Red pulp of the spleen (Correct Answer)
- C. Bone marrow
- D. White pulp of the spleen
- E. Blood vessels
Lymphedema pathophysiology Explanation: ***Red pulp of the spleen***
- The patient's symptoms (fatigue, back pain, dark urine after malaria prophylaxis) and lab findings (**dark intracellular inclusions** and abnormally shaped red blood cells) suggest **G6PD deficiency**, leading to **hemolytic anemia**.
- The **red pulp of the spleen** is where old or damaged red blood cells, including those with Heinz bodies (intracellular inclusions) or abnormal shapes, are **phagocytosed** by macrophages, thus "shaping" them or removing severely affected cells.
*Lymph nodes*
- **Lymph nodes** are primarily involved in filtering lymph and are major sites for adaptive immune responses, housing B and T lymphocytes.
- They are not the primary sites for the destruction or "shaping" of red blood cells.
*Bone marrow*
- The **bone marrow** is the primary site of **hematopoiesis**, where red blood cells are produced, not where they are destroyed or undergo physical shaping due to immune cell action in hemolysis.
- While macrophages are present, their main role in marrow is related to erythropoiesis (e.g., central macrophage in erythroblastic islands) and debris clearance, not erythrocyte shaping in peripheral circulation.
*White pulp of the spleen*
- The **white pulp of the spleen** is rich in lymphocytes and is the site of immune responses, similar to lymph nodes.
- It is involved in adaptive immunity and not directly engaged in the physical destruction or "shaping" of red blood cells during hemolysis.
*Blood vessels*
- **Blood vessels** are conduits for blood transport and are not primary sites for the physical destruction or shaping of red blood cells by immune cells.
- While some hemolysis can occur intravascularly, the immune cells responsible for removing and "shaping" damaged red blood cells (like macrophages) are predominantly organ-resident.
Lymphedema pathophysiology US Medical PG Question 9: A 44-year-old woman undergoes radical hysterectomy for stage IB2 cervical cancer. During surgery, the gynecologic oncologist notes aberrant lymphatic drainage patterns possibly related to the patient's history of pelvic inflammatory disease and previous cesarean section. Frozen section of a lymph node from the obturator fossa shows metastatic disease. Synthesizing knowledge of primary and collateral cervical lymphatic drainage, which nodal group represents the most critical next level of drainage that would impact surgical decision-making?
- A. Presacral nodes via uterosacral ligament pathway
- B. Common iliac and para-aortic nodes via external iliac pathway (Correct Answer)
- C. Internal iliac nodes only
- D. Inguinal nodes via deep femoral pathway
- E. Superficial inguinal nodes via round ligament pathway
Lymphedema pathophysiology Explanation: ***Common iliac and para-aortic nodes via external iliac pathway***
- The **common iliac nodes** serve as the primary drainage destination from both the **external iliac** and **obturator nodes**, making them the critical next level when **obturator metastasis** is confirmed.
- Lymphatic spread in cervical cancer typically follows a regular pattern: primary pelvic nodes (obturator, external/internal iliacs) move toward the **common iliac** and then **para-aortic** regions.
*Superficial inguinal nodes via round ligament pathway*
- Drainage to these nodes occurs primarily from the **uterine horns** or the **vulva**, not typically the cervix unless the tumor involves the lower vagina.
- These nodes are not part of the standard cephalad **retroperitoneal spread** pathway for stage IB2 cervical cancer.
*Presacral nodes via uterosacral ligament pathway*
- These nodes provide a minor primary drainage route via the **uterosacral ligaments**, but they are anatomically distinct from the lateral **obturator fossa** chain.
- They do not represent the "next level" of drainage that would indicate **systemic progression** beyond the pelvic basin.
*Internal iliac nodes only*
- The **internal iliac nodes** are primary pelvic nodes and are considered on the **same drainage tier** as the obturator nodes already found to be positive.
- Assessing these nodes only would not provide enough information regarding the **cephalad extent** of the disease required for surgical modification.
*Inguinal nodes via deep femoral pathway*
- The **deep femoral pathway** primarily drains the lower limb and vulva rather than the **cervical stroma** and parametrium.
- Involvement of these nodes would be an exception and would not help in determining the transition to **extended-field radiation** for retroperitoneal disease.
Lymphedema pathophysiology US Medical PG Question 10: A 67-year-old man with squamous cell carcinoma of the anal canal presents for staging. Physical examination reveals a 3 cm tumor at the dentate line extending both above and below it. Inguinal lymphadenopathy is palpable bilaterally. CT shows both inguinal and pelvic lymph node enlargement. Evaluating the lymphatic drainage of the anal canal, which treatment approach best addresses the dual drainage patterns of this tumor location?
- A. Chemoradiation targeting both inguinal and pelvic nodal basins (Correct Answer)
- B. Pelvic lymph node dissection only, following inferior mesenteric pathways
- C. Sequential surgery: abdominoperineal resection then inguinal dissection
- D. Radiation to inguinal nodes only with surgical resection of pelvic nodes
- E. Inguinal lymph node dissection only, as anal tumors drain superficially
Lymphedema pathophysiology Explanation: ***Chemoradiation targeting both inguinal and pelvic nodal basins***
- Tumors at the **dentate line** exhibit dual lymphatic drainage: the area above drains to **internal iliac** and **perirectal nodes**, while the area below drains to **superficial inguinal nodes**.
- The standard of care for anal **squamous cell carcinoma** (SCC) is the **Nigro protocol**, which uses **definitive chemoradiotherapy** to treat both the primary tumor and all involved regional nodal basins.
*Inguinal lymph node dissection only, as anal tumors drain superficially*
- While the area below the dentate line drains to **inguinal nodes**, the area above drains into the **pelvis**, meaning a dissection limited to the groin would miss half of the drainage pathway.
- Surgical dissection is not the primary treatment for anal SCC, as **chemoradiation** offers high rates of cure while preserving anal sphincter function.
*Pelvic lymph node dissection only, following inferior mesenteric pathways*
- This approach neglects the **superficial inguinal nodes**, which are already palpably enlarged in this patient and are the primary drainage route for the inferior anal canal.
- **Pelvic lymph node dissection** is technically difficult and carries high morbidity; it has been largely superseded by targeted **radiotherapy** in the management of this malignancy.
*Sequential surgery: abdominoperineal resection then inguinal dissection*
- **Abdominoperineal resection (APR)** is now considered **salvage therapy** for persistent or recurrent disease after definitive chemoradiotherapy rather than a first-line treatment.
- Sequential surgeries increase the risk of **wound complications** and **lymphedema** without offering a survival benefit over conservative chemoradiation in SCC.
*Radiation to inguinal nodes only with surgical resection of pelvic nodes*
- Splitting treatment between radiation for one basin and surgery for another increases **treatment toxicity** and delays the start of systemic chemotherapy.
- Both **inguinal and pelvic nodal basins** are exquisitely **radiosensitive** in anal SCC, so the entire region is standardly managed with integrated radiation fields.
More Lymphedema pathophysiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.