Lymph node groups and clinical significance US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lymph node groups and clinical significance. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lymph node groups and clinical significance US Medical PG Question 1: A 4-year-old girl is brought to the physician for a painless lump on her neck. She has no history of serious illness and her vital signs are within normal limits. On examination, there is a firm, 2-cm swelling at the midline just below the level of the hyoid bone. The mass moves cranially when she is asked to protrude her tongue. Which of the following is the most likely diagnosis?
- A. Cystic hygroma
- B. Thyroglossal cyst (Correct Answer)
- C. Ranula
- D. Dermoid cyst
Lymph node groups and clinical significance Explanation: Thyroglossal cyst
- A midline neck mass that moves cranially with tongue protrusion is the classic presentation of a thyroglossal duct cyst.
- These cysts arise from the remnant of the thyroglossal duct, the embryonic tract along which the thyroid gland descends from the foramen cecum to its final position [1].
Cystic hygroma
- This is a lymphatic malformation typically appearing as a soft, compressible, transilluminant mass, often in the posterior triangle of the neck.
- It does not move with tongue protrusion and is usually not midline.
Ranula
- A ranula is a mucocele that forms in the floor of the mouth, usually due to obstruction of a sublingual salivary gland.
- It presents as a swelling in the oral cavity, below the tongue, and not as an external neck mass.
Dermoid cyst
- A dermoid cyst in the neck is typically a painless, doughy, subcutaneous mass that is also usually midline but does not move with tongue protrusion.
- These cysts are often found above the hyoid bone, unlike the typical position of a thyroglossal cyst.
Lymph node groups and clinical significance US Medical PG Question 2: A 49-year-old woman presents to her physician with complaints of breast swelling and redness of the skin over her right breast for the past 1 month. She also mentions that the skin above her right breast appears to have thickened. She denies any pain or nipple discharge. The past medical history is significant for a total abdominal hysterectomy at 45 years of age. Her last mammogram 1 year ago was negative for any pathologic changes. On examination, the right breast was diffusely erythematous with gross edema and tenderness and appeared larger than the left breast. The right nipple was retracted and the right breast was warmer than the left breast. No localized mass was palpated. Which of the following statements best describes the patient’s most likely condition?
- A. It shows predominant lymphatic spread.
- B. The lesion expresses receptors for estrogen and progesterone.
- C. The lesion is due to Streptococcal infection.
- D. It is a benign lesion.
- E. The inflammation is due to obstruction of dermal lymphatic vessels. (Correct Answer)
Lymph node groups and clinical significance Explanation: ***The inflammation is due to obstruction of dermal lymphatic vessels.***
- The presentation of **rapid-onset breast swelling, redness, thickening of the skin, warmth, and nipple retraction** without a palpable mass is highly suggestive of **inflammatory breast cancer (IBC)**.
- IBC is characterized by the **obstruction of dermal lymphatic vessels by tumor cells**, leading to the classic inflammatory signs and **peau d'orange** appearance.
*It shows predominant lymphatic spread.*
- While IBC does involve **lymphatic spread**, this statement alone does not fully encompass the characteristic pathology of the condition causing the observed symptoms.
- The obstruction of the **dermal lymphatic vessels** is a more precise description of the immediate cause of the clinical presentation.
*The lesion expresses receptors for estrogen and progesterone.*
- Although some breast cancers are **hormone receptor-positive (ER/PR positive)**, there is no direct information in the vignette to suggest this specificity for the patient's condition.
- This statement refers to a **molecular characteristic** that is not a defining feature of the clinical presentation of IBC.
*The lesion is due to Streptococcal infection.*
- While a **bacterial infection** (like **streptococcal cellulitis**) can cause redness, swelling, and warmth, it typically presents with more acute symptoms, fever, and often a clearer response to antibiotics.
- The **thickening of the skin** and **nipple retraction** point away from a simple infection and towards a malignant process.
*It is a benign lesion.*
- The rapid progression of symptoms, pronounced skin changes, and nipple retraction are all **red flags for malignancy**, specifically inflammatory breast cancer.
- **Benign lesions** rarely cause such diffuse, severe, and rapidly progressing inflammatory signs.
Lymph node groups and clinical significance US Medical PG Question 3: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Lymph node groups and clinical significance Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
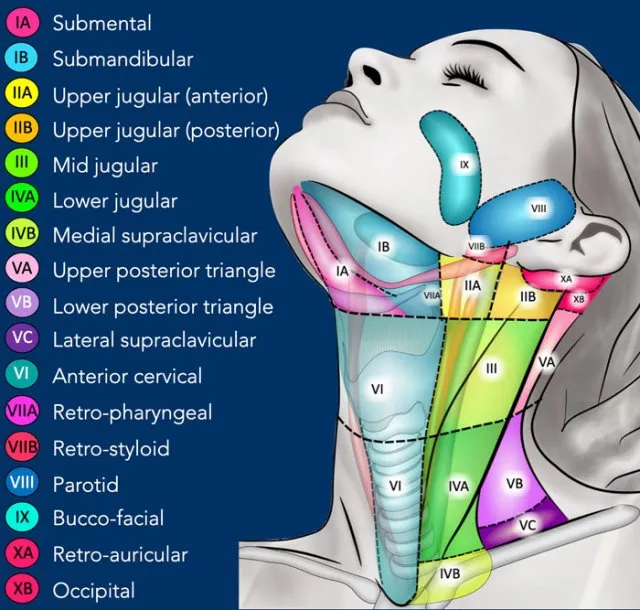
Lymph node groups and clinical significance US Medical PG Question 4: A 43-year-old man comes to the physician because of weight loss and swelling on the left side of his neck. Physical examination shows a firm, enlarged left upper cervical lymph node that is immobile. Immunohistochemical testing performed on a biopsy specimen from the lymph node stains positive for cytokeratin. Which of the following is the most likely site of the primary neoplasm in this patient?
- A. Nerve sheath
- B. Bone
- C. Muscle
- D. Skin
- E. Nasopharynx (Correct Answer)
Lymph node groups and clinical significance Explanation: ***Nasopharynx***
- A **firm, enlarged, immobile cervical lymph node** in the upper neck (Level II) with **cytokeratin positivity** indicates metastatic carcinoma of epithelial origin.
- **Nasopharyngeal carcinoma** classically presents with **cervical lymphadenopathy as the initial manifestation** in up to 90% of cases, often before other symptoms develop.
- The **left upper cervical location** is characteristic of nasopharyngeal primary tumors, which have a strong predilection for Level II nodal metastasis.
- **Weight loss** suggests systemic disease consistent with advanced carcinoma.
- Nasopharyngeal carcinoma is **cytokeratin-positive** (epithelial origin) and frequently presents with isolated neck mass **without nasal symptoms** in early stages.
*Skin*
- While cutaneous squamous cell carcinoma can metastasize to cervical nodes, it would require a **visible primary skin lesion** on the head, neck, or scalp, which would be evident on physical examination.
- Skin primaries more commonly metastasize to **posterior cervical nodes (Level V)** from scalp lesions, not upper anterior cervical nodes.
- This presentation is **far less common** than mucosal head and neck primaries for isolated cervical metastasis.
*Nerve sheath*
- Nerve sheath tumors such as **schwannomas** or **neurofibromas** are of mesenchymal origin and stain positive for **S-100 protein**, not cytokeratin.
- These tumors are typically **benign and mobile**, not firm and immobile like metastatic carcinoma.
*Bone*
- Primary bone tumors (e.g., osteosarcoma) do not express **cytokeratin** and would not present with isolated cervical lymphadenopathy.
- Bone tumors would show characteristic imaging findings and typically metastasize to lungs, not regional lymph nodes.
*Muscle*
- Muscle-derived tumors such as **rhabdomyosarcoma** or **leiomyosarcoma** are mesenchymal in origin.
- These tumors stain positive for **desmin** and **actin**, not cytokeratin, which is specific to epithelial cells.
Lymph node groups and clinical significance US Medical PG Question 5: A 32-year-old man comes to the physician because of a 3-week history of cough, weight loss, and night sweats. He migrated from Sri Lanka 6 months ago. He appears emaciated. His temperature is 38.1°C (100.5°F). Physical examination shows enlargement of the right supraclavicular lymph node. Chest and abdominal examination show no abnormalities. An interferon-gamma assay is positive. A biopsy specimen of the cervical lymph node is most likely to show the causal organism in which of the following locations?
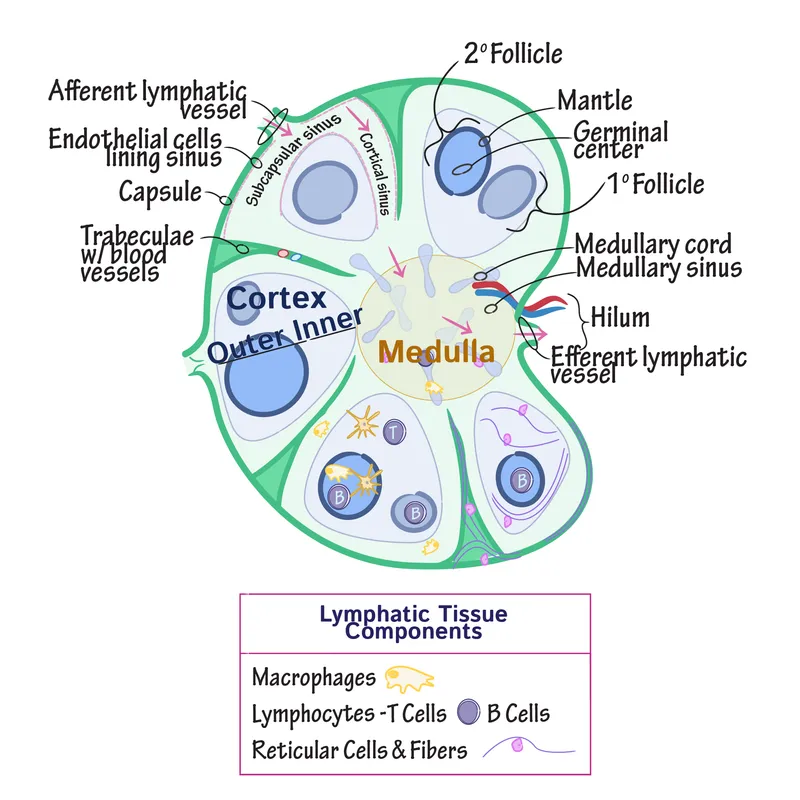
- A. Mantle zone
- B. Medullary sinus
- C. Germinal center
- D. Subcapsular sinus
- E. Paracortex (Correct Answer)
Lymph node groups and clinical significance Explanation: ***Paracortex***
- The patient's symptoms (cough, weight loss, night sweats, fever), recent migration from an endemic area (Sri Lanka), **supraclavicular lymphadenopathy**, and positive **interferon-gamma release assay (IGRA)** strongly suggest **tuberculosis**.
- In tuberculous lymphadenitis, **caseating granulomas** containing *Mycobacterium tuberculosis* organisms characteristically form in the **paracortex** (T-cell zone).
- The **paracortex** is where **cell-mediated immunity** occurs, with T cells interacting with infected macrophages and dendritic cells to form the **epithelioid granulomas** with **Langhans giant cells** that are pathognomonic for TB.
- The organisms are found within these **granulomas**, which predominantly occur in the paracortical (interfollicular) region.
*Mantle zone*
- The **mantle zone** primarily contains **naïve B cells** surrounding germinal centers.
- This is a B-cell area not typically involved in granuloma formation or mycobacterial infection.
*Germinal center*
- **Germinal centers** are sites of B cell proliferation, somatic hypermutation, and antibody class switching.
- TB is a disease of **cell-mediated immunity** (T cells and macrophages), not humoral immunity, so granulomas do not form in germinal centers.
*Medullary sinus*
- The **medullary sinuses** are channels in the medulla of the lymph node through which lymph flows toward the efferent lymphatic vessels.
- While macrophages line these sinuses and may contain some organisms in acute infections, the characteristic **caseating granulomas** of chronic tuberculous lymphadenitis form in the **paracortex**, not in the sinuses.
*Subcapsular sinus*
- The **subcapsular sinus** is the initial entry point for afferent lymph into the lymph node.
- While this is where pathogens first enter, chronic granulomatous infections like TB develop their characteristic pathology deeper in the node, specifically in the **paracortex** where T-cell-mediated granuloma formation occurs.
Lymph node groups and clinical significance US Medical PG Question 6: A 62-year-old woman presents to her physician with a painless breast mass on her left breast for the past 4 months. She mentions that she noticed the swelling suddenly one day and thought it would resolve by itself. Instead, it has been slowly increasing in size. On physical examination of the breasts, the physician notes a single non-tender, hard, and fixed nodule over left breast. An ultrasonogram of the breast shows a solid mass, and a fine-needle aspiration biopsy confirms the mass to be lobular carcinoma of the breast. When the patient asks about her prognosis, the physician says that the prognosis can be best determined after both grading and staging of the tumor. Based on the current diagnostic information, the physician says that they can only grade, but no stage, the neoplasm. Which of the following facts about the neoplasm is currently available to the physician?
- A. The tumor invades the pectoralis major.
- B. The tumor has spread via blood-borne metastasis.
- C. The tumor has not metastasized to the contralateral superior mediastinal lymph nodes.
- D. The tumor has metastasized to the axillary lymph nodes.
- E. The tumor cells exhibit marked nuclear atypia. (Correct Answer)
Lymph node groups and clinical significance Explanation: ***The tumor cells exhibit marked nuclear atypia.***
- **Grading** assesses the **histological appearance** of cancer cells and tissues, including features like nuclear atypia, mitotic rate, and architectural features, which are directly observable from the **fine-needle aspiration biopsy**.
- **Nuclear atypia** refers to abnormal changes in the size, shape, and chromatin pattern of cell nuclei, indicating a higher degree of anaplasia and aggressiveness.
*The tumor invades the pectoralis major.*
- **Invasion into surrounding tissues**, especially muscle, is a feature determined during **surgical staging** or comprehensive imaging, which is not described as being performed yet.
- This information relates to the **"T" (tumor size/extension)** component of TNM staging, which cannot be fully assessed with only a biopsy.
*The tumor has spread via blood-borne metastasis.*
- **Distant metastasis** is part of the **"M" (metastasis)** component of TNM staging, requiring imaging studies (e.g., PET scan, CT scan) or biopsies of suspected metastatic sites.
- The current diagnostic information (biopsy of the primary tumor) does not provide details about **blood-borne spread**.
*The tumor has not metastasized to the contralateral superior mediastinal lymph nodes.*
- Information about **lymph node involvement**, even in distant locations like the mediastinum, falls under the **"N" (nodes)** component of TNM staging, which requires thorough imaging or surgical dissection.
- The current biopsy focuses on the primary breast mass and cannot rule out distant lymph node metastasis.
*The tumor has metastasized to the axillary lymph nodes.*
- **Axillary lymph node metastasis** is also part of the **"N" component** of staging and is typically determined by sentinel lymph node biopsy or axillary dissection performed during surgery, or through imaging.
- A fine-needle aspiration of the primary breast mass does not provide information about regional lymph node involvement.
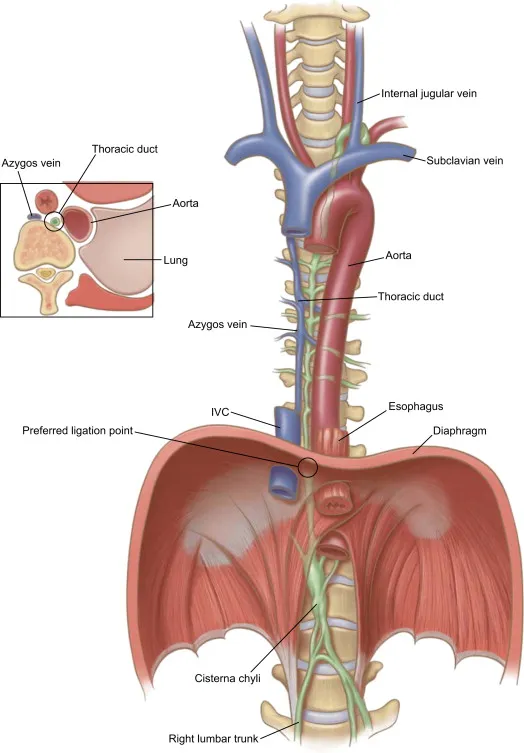
Lymph node groups and clinical significance US Medical PG Question 7: Two weeks after undergoing low anterior resection for rectal cancer, a 52-year-old man comes to the physician because of swelling in both feet. He has not had any fever, chills, or shortness of breath. His temperature is 36°C (96.8°F) and pulse is 88/min. Physical examination shows a normal thyroid and no jugular venous distention. Examination of the lower extremities shows bilateral non-pitting edema that extends from the feet to the lower thigh, with deep flexion creases. His skin is warm and dry, and there is no erythema or rash. Microscopic examination of the interstitial space in this patient's lower extremities would be most likely to show the presence of which of the following?
- A. Neutrophilic, protein-rich fluid
- B. Lymphocytic, hemosiderin-rich fluid
- C. Lipid-rich, protein-rich fluid (Correct Answer)
- D. Protein-rich, glycosaminoglycan-rich fluid
- E. Acellular, protein-poor fluid
Lymph node groups and clinical significance Explanation: ***Lipid-rich, protein-rich fluid***
- The presentation of bilateral non-pitting edema extending to the thigh, with deep flexion creases, in a patient post-**low anterior resection** for rectal cancer, strongly suggests **lymphedema**.
- Lymphedema results from impaired lymphatic drainage, leading to the accumulation of **protein-rich fluid**, **macromolecules**, and **adipose tissue** in the interstitial space, which eventually becomes lipid-rich due to chronic inflammation and fibroblasts stimulating adipogenesis.
*Neutrophilic, protein-rich fluid*
- This description is characteristic of **inflammatory edema** or **purulent exudate**, typically seen in infections.
- The patient's lack of fever, chills, erythema, or warmth makes an infectious or acute inflammatory process unlikely.
*Lymphocytic, hemosiderin-rich fluid*
- **Hemosiderin deposits** are indicative of chronic **venous insufficiency** or recurrent hemorrhages, leading to red blood cell extravasation and breakdown.
- While lymphocytes can be present in chronic inflammation, the primary issue here is lymphatic obstruction, not venous stasis or bleeding.
*Protein-rich, glycosaminoglycan-rich fluid*
- While lymphedema is indeed **protein-rich**, the primary accumulation in mature lymphedema involves **adipose tissue** and fibrosis.
- **Glycosaminoglycans** accumulate significantly in conditions like **myxedema** (hypothyroidism), which was ruled out by the normal thyroid examination.
*Acellular, protein-poor fluid*
- This describes a **transudate**, typically seen in conditions like **heart failure**, **liver cirrhosis**, or **nephrotic syndrome** where there's an imbalance of hydrostatic and oncotic pressures.
- The edema in this case is **non-pitting**, suggesting a higher protein content and tissue changes characteristic of lymphatic dysfunction, not systemic fluid overload leading to protein-poor fluid.
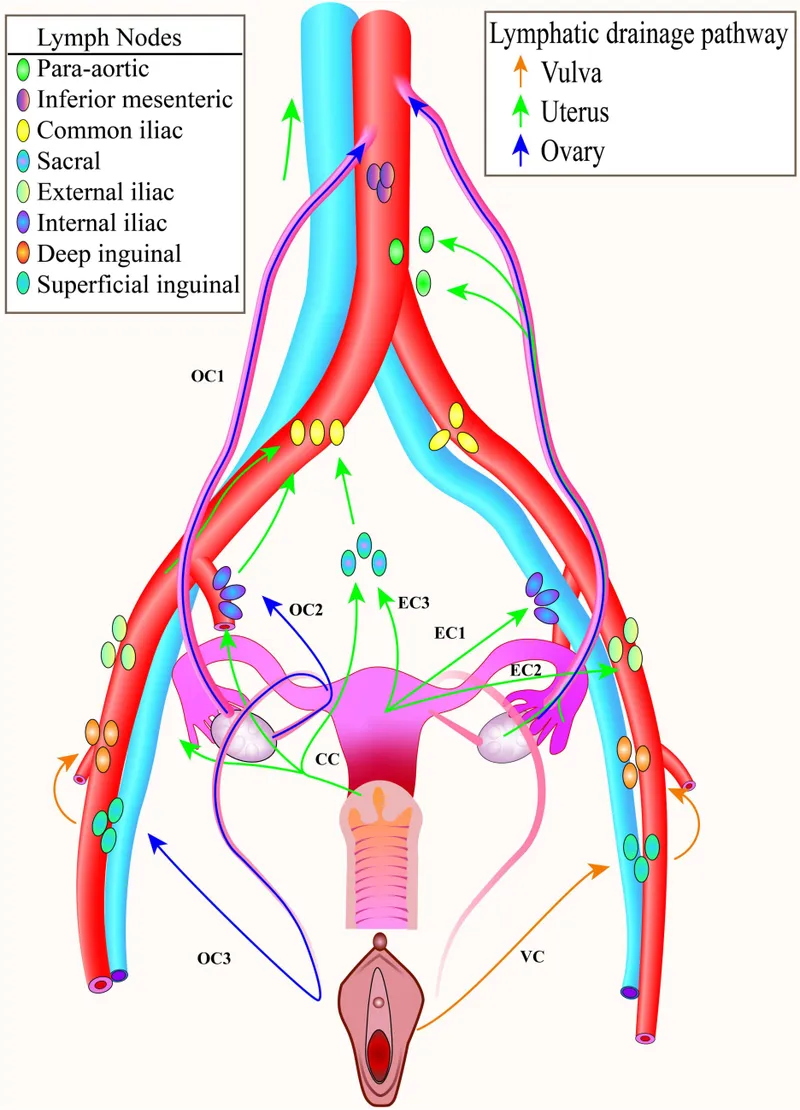
Lymph node groups and clinical significance US Medical PG Question 8: A 76-year-old woman comes to the physician for evaluation of a 3-month history of vulvar itching and pain. She was diagnosed with lichen sclerosus 4 years ago. She has smoked 1 pack of cigarettes daily for 35 years. Physical examination shows a 2.5-cm nodular, ulcerative lesion on the vaginal introitus and left labia minora with surrounding erythema. Punch biopsy shows squamous cell carcinoma. A CT scan of the chest, abdomen, and pelvis shows enlarged lymph nodes concerning for metastatic disease. Which of the following lymph node regions is the most likely primary site of metastasis?
- A. Superficial inguinal (Correct Answer)
- B. Internal iliac
- C. External iliac
- D. Inferior mesenteric
- E. Para-aortic
Lymph node groups and clinical significance Explanation: ***Superficial inguinal***
- The **vulva** drains primarily into the **superficial inguinal lymph nodes**, making them the most likely first site for metastatic spread from vulvar squamous cell carcinoma.
- The lesion's location on the **vaginal introitus** and **labia minora** directly correlates with this lymphatic drainage pathway.
*Internal iliac*
- **Internal iliac nodes** receive drainage mainly from deep pelvic structures like the cervix, upper vagina, and uterus, not directly from the vulva.
- Metastasis to these nodes usually occurs after involvement of more superficial nodes or in advanced disease with deeper invasion.
*External iliac*
- **External iliac nodes** generally drain the lower extremities and deeper pelvic structures (e.g., bladder, distal ureter), not the vulva as a primary site.
- Involvement here would typically indicate more advanced local spread or secondary metastasis from other pelvic nodes.
*Inferior mesenteric*
- **Inferior mesenteric nodes** drain the hindgut and its derivatives, including the distal colon and rectum, which are distant from the vulva.
- This region is not involved in the lymphatic drainage of the vulva.
*Para-aortic*
- **Para-aortic nodes** drain structures like the ovaries, fallopian tubes, and upper uterus; they are too superior for primary vulvar lymphatic drainage.
- Metastasis to these nodes from vulvar cancer would signify widespread, very advanced disease and not a primary site of spread.
Lymph node groups and clinical significance US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Lymph node groups and clinical significance Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Lymph node groups and clinical significance US Medical PG Question 10: A 59-year-old woman presents to her primary care provider with a 6-month history of progressive left-arm swelling. Two years ago she had a partial mastectomy and axillary lymph node dissection for left breast cancer. She was also treated with radiotherapy at the time. Upon further questioning, she denies fever, pain, or skin changes, but reports difficulty with daily tasks because her hand feels heavy and weak. She is bothered by the appearance of her enlarged extremity and has stopped playing tennis. On physical examination, nonpitting edema of the left arm is noted with hyperkeratosis, papillomatosis, and induration of the skin. Limb elevation, exercise, and static compression bandaging are started. If the patient has no improvement, which of the following will be the best next step?
- A. Diethylcarbamazine
- B. Low molecular weight heparin
- C. Endovascular stenting
- D. Vascularized lymph node transfer (Correct Answer)
- E. Antibiotics
Lymph node groups and clinical significance Explanation: ***Vascularized lymph node transfer***
- This patient presents with **secondary lymphedema** due to axillary dissection and radiotherapy, which has not responded to conservative management.
- **Vascularized lymph node transfer** is a surgical option that involves transplanting healthy lymph nodes to the affected area to re-establish lymphatic drainage pathways, offering a more definitive solution for refractory cases.
*Diethylcarbamazine*
- **Diethylcarbamazine** is an anti-filarial drug used to treat lymphedema caused by **parasitic infections**, specifically filariasis.
- The patient's lymphedema is secondary to breast cancer treatment, not parasitic infection, making this a **misdirected treatment**.
*Low molecular weight heparin*
- **Low molecular weight heparin** is an anticoagulant used to prevent or treat **venous thromboembolism (VTE)**.
- While patients with cancer are at increased risk for VTE, her symptoms are consistent with lymphedema and not thrombosis, which would typically present with more acute pain and swelling, making this an inappropriate treatment.
*Endovascular stenting*
- **Endovascular stenting** is a procedure used to open blocked or narrowed **blood vessels**, such as in peripheral artery disease or venous obstruction.
- Her condition is specifically lymphedema, a lymphatic circulation issue, not a vascular obstruction, so stenting would not address the underlying problem.
*Antibiotics*
- **Antibiotics** are used to treat **bacterial infections**, which can complicate lymphedema (e.g., cellulitis).
- While chronic lymphedema causes skin changes (hyperkeratosis, papillomatosis, induration), the patient shows no signs of **acute infection** such as fever, pain, erythema, or warmth, making empirical antibiotics unnecessary at this stage.
More Lymph node groups and clinical significance US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.