Lower limb lymphatic drainage US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lower limb lymphatic drainage. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lower limb lymphatic drainage US Medical PG Question 1: A 52-year-old man presents to the emergency department because of pain and swelling in his left leg over the past few hours. He traveled from Sydney to Los Angeles 2 days ago. He has had type 2 diabetes mellitus for 10 years and takes metformin for it. He has smoked a pack of cigarettes daily for 25 years. His temperature is 36.9°C (98.4°F), the blood pressure is 140/90 mm Hg, and the pulse is 90/min. On examination, the left calf is 5 cm greater in circumference than the right. The left leg appears more erythematous than the right with dilated superficial veins. Venous duplex ultrasound shows non-compressibility. Which of the following best represents the mechanism of this patient’s illness?
- A. Impaired venous blood flow (Correct Answer)
- B. Subcutaneous soft-tissue infection that may extend to the deep fascia
- C. Infection of the dermis and subcutaneous tissues
- D. Impaired arterial blood flow
- E. Impaired lymphatic flow
Lower limb lymphatic drainage Explanation: ***Impaired venous blood flow***
- The patient's symptoms (unilateral leg pain and swelling, erythema, dilated superficial veins, recent long-haul travel) and the **venous duplex ultrasound** finding of **non-compressibility** are highly indicative of **deep vein thrombosis (DVT)**, which results from impaired venous outflow.
- Risk factors such as **long-haul travel** (venous stasis), **smoking** (endothelial damage), and potentially **diabetes** contribute to a hypercoagulable state.
*Impaired lymphatic flow*
- This typically presents as **lymphedema**, characterized by chronic, often pitting edema, and skin changes like thickening (peau d'orange), but usually without acute erythema or dilated superficial veins in this context.
- **Venous duplex ultrasound** would not show non-compressibility in cases of impaired lymphatic flow, as veins themselves would be clear.
*Subcutaneous soft-tissue infection that may extend to the deep fascia*
- This describes **necrotizing fasciitis**, a severe infection often characterized by rapid progression, severe pain disproportionate to examination findings, blistering, and systemic toxicity, which are not clearly evident here.
- While there is erythema, the key diagnostic finding is the **non-compressible vein**, not signs of crepitus or rapidly spreading infection.
*Infection of the dermis and subcutaneous tissues*
- This describes **cellulitis**, which presents with localized redness, warmth, swelling, and tenderness, often with an entry point.
- While some symptoms overlap (erythema, swelling), the **venous duplex ultrasound finding of non-compressibility** definitively points away from a simple skin infection and towards a vascular obstruction.
*Impaired arterial blood flow*
- This presents as **acute limb ischemia**, characterized by the "6 Ps": pain, pallor, pulselessness, paresthesias, poikilothermia (coldness), and paralysis.
- The patient's leg is swollen and erythematous, not pale and cold, and the ultrasound directly implicates venous rather than arterial occlusion.
Lower limb lymphatic drainage US Medical PG Question 2: A 30-year-old woman who is 24-weeks pregnant presents to the emergency department with fever, painful urination, and headache. The patient's blood pressure is 111/67 mm Hg, the pulse is 95/min, the respiratory rate is 16/min, and the temperature is 38.3°C (101.1°F). Physical examination reveals bilateral tender inguinal lymphadenopathy and painful genital lesions. On closer inspection, the patient’s genital lesions contain clear fluid and measure 5–6 mm in diameter. What is the appropriate description of these lesions?
- A. Pustule
- B. Ulcer
- C. Papule
- D. Bulla
- E. Vesicle (Correct Answer)
Lower limb lymphatic drainage Explanation: ***Vesicle***
- A **vesicle** is defined as a **circumscribed, elevated lesion** (macule/papule) containing **clear fluid** and measuring less than 1 cm in diameter.
- The patient's lesions, which are 5-6 mm in diameter and contain clear fluid, perfectly fit the description of vesicles, characteristic of **herpes simplex virus (HSV)** infection.
*Pustule*
- A **pustule** is a small, elevated lesion similar to a vesicle but filled with **pus**, not clear fluid.
- Examples include acne or folliculitis, which are typically opaque and yellowish, unlike the described lesions.
*Ulcer*
- An **ulcer** is a defect or excavation of the skin past the **epidermis**, resulting in the loss of tissue.
- The patient's lesions are described as fluid-filled and elevated, not as an open wound with tissue loss.
*Papule*
- A **papule** is a **solid, elevated lesion** measuring less than 1 cm in diameter.
- While elevated and small, a papule does **not contain fluid**, which is a key characteristic of the described lesions.
*Bulla*
- A **bulla** is a **fluid-filled lesion** that is **larger than 1 cm** in diameter.
- The lesions described are 5-6 mm, making them smaller than the definition of a bulla.
Lower limb lymphatic drainage US Medical PG Question 3: A 59-year-old woman presents to her primary care provider with a 6-month history of progressive left-arm swelling. Two years ago she had a partial mastectomy and axillary lymph node dissection for left breast cancer. She was also treated with radiotherapy at the time. Upon further questioning, she denies fever, pain, or skin changes, but reports difficulty with daily tasks because her hand feels heavy and weak. She is bothered by the appearance of her enlarged extremity and has stopped playing tennis. On physical examination, nonpitting edema of the left arm is noted with hyperkeratosis, papillomatosis, and induration of the skin. Limb elevation, exercise, and static compression bandaging are started. If the patient has no improvement, which of the following will be the best next step?
- A. Diethylcarbamazine
- B. Low molecular weight heparin
- C. Endovascular stenting
- D. Vascularized lymph node transfer (Correct Answer)
- E. Antibiotics
Lower limb lymphatic drainage Explanation: ***Vascularized lymph node transfer***
- This patient presents with **secondary lymphedema** due to axillary dissection and radiotherapy, which has not responded to conservative management.
- **Vascularized lymph node transfer** is a surgical option that involves transplanting healthy lymph nodes to the affected area to re-establish lymphatic drainage pathways, offering a more definitive solution for refractory cases.
*Diethylcarbamazine*
- **Diethylcarbamazine** is an anti-filarial drug used to treat lymphedema caused by **parasitic infections**, specifically filariasis.
- The patient's lymphedema is secondary to breast cancer treatment, not parasitic infection, making this a **misdirected treatment**.
*Low molecular weight heparin*
- **Low molecular weight heparin** is an anticoagulant used to prevent or treat **venous thromboembolism (VTE)**.
- While patients with cancer are at increased risk for VTE, her symptoms are consistent with lymphedema and not thrombosis, which would typically present with more acute pain and swelling, making this an inappropriate treatment.
*Endovascular stenting*
- **Endovascular stenting** is a procedure used to open blocked or narrowed **blood vessels**, such as in peripheral artery disease or venous obstruction.
- Her condition is specifically lymphedema, a lymphatic circulation issue, not a vascular obstruction, so stenting would not address the underlying problem.
*Antibiotics*
- **Antibiotics** are used to treat **bacterial infections**, which can complicate lymphedema (e.g., cellulitis).
- While chronic lymphedema causes skin changes (hyperkeratosis, papillomatosis, induration), the patient shows no signs of **acute infection** such as fever, pain, erythema, or warmth, making empirical antibiotics unnecessary at this stage.
Lower limb lymphatic drainage US Medical PG Question 4: A 93-year-old woman is brought to the physician because of a purple area on her right arm that has been growing for one month. She has not had any pain or itching of the area. She has hyperlipidemia, a history of basal cell carcinoma treated with Mohs surgery 2 years ago, and a history of invasive ductal carcinoma of the right breast treated with radical mastectomy 57 years ago. She has had chronic lymphedema of the right upper extremity since the mastectomy. Her only medication is simvastatin. She lives in an assisted living facility. She is content with her living arrangement but feels guilty that she is dependent on others. Vital signs are within normal limits. Physical examination shows extensive edema of the right arm. Skin exam of the proximal upper right extremity shows three coalescing, 0.5–1.0 cm heterogeneous, purple-colored plaques with associated ulceration. Which of the following is the most likely diagnosis?
- A. Lymphangiosarcoma (Correct Answer)
- B. Cellulitis
- C. Thrombophlebitis
- D. Kaposi sarcoma
- E. Lichen planus
Lower limb lymphatic drainage Explanation: ***Lymphangiosarcoma***
- This patient presents with a **purple area** with **ulceration** on an arm affected by chronic **lymphedema** following a mastectomy. This constellation of findings is highly suggestive of **Stewart-Treves syndrome**, which is a rare but aggressive form of angiosarcoma (lymphangiosarcoma) arising in the setting of chronic lymphedema.
- The history of **radical mastectomy 57 years ago** with subsequent **chronic right upper extremity lymphedema** strongly predisposes to this condition, especially given the lack of pain or itching and the progressive nature of the lesion.
*Cellulitis*
- Characterized by **erythema**, **warmth**, **pain**, and **tenderness**, often with fever and systemic symptoms, none of which are described.
- While lymphedema is a risk factor for cellulitis, the description of a **purple, ulcerated plaque** with a duration of one month is inconsistent with acute bacterial infection.
*Thrombophlebitis*
- Typically presents with **pain**, **tenderness**, **erythema**, and a palpable cord-like vein along the course of a superficial vein, which is not described.
- The lesion described is a spreading, **ulcerated plaque**, not a discrete inflamed vein.
*Kaposi sarcoma*
- While it can present with **purple lesions**, Kaposi sarcoma is typically associated with **immunosuppression** (e.g., HIV infection) or certain endemic regions, neither of which is mentioned.
- The strong association with **chronic lymphedema** in this case makes lymphangiosarcoma a more specific diagnosis.
*Lichen planus*
- A chronic inflammatory condition characterized by **pruritic, purple, polygonal, planar papules and plaques (the 6 Ps)**, often with fine white lines (Wickham's striae).
- It does not typically present as a growing, **ulcerated purple plaque** in the setting of chronic lymphedema, and itching is a prominent symptom.
Lower limb lymphatic drainage US Medical PG Question 5: Two weeks after undergoing low anterior resection for rectal cancer, a 52-year-old man comes to the physician because of swelling in both feet. He has not had any fever, chills, or shortness of breath. His temperature is 36°C (96.8°F) and pulse is 88/min. Physical examination shows a normal thyroid and no jugular venous distention. Examination of the lower extremities shows bilateral non-pitting edema that extends from the feet to the lower thigh, with deep flexion creases. His skin is warm and dry, and there is no erythema or rash. Microscopic examination of the interstitial space in this patient's lower extremities would be most likely to show the presence of which of the following?
- A. Neutrophilic, protein-rich fluid
- B. Lymphocytic, hemosiderin-rich fluid
- C. Lipid-rich, protein-rich fluid (Correct Answer)
- D. Protein-rich, glycosaminoglycan-rich fluid
- E. Acellular, protein-poor fluid
Lower limb lymphatic drainage Explanation: ***Lipid-rich, protein-rich fluid***
- The presentation of bilateral non-pitting edema extending to the thigh, with deep flexion creases, in a patient post-**low anterior resection** for rectal cancer, strongly suggests **lymphedema**.
- Lymphedema results from impaired lymphatic drainage, leading to the accumulation of **protein-rich fluid**, **macromolecules**, and **adipose tissue** in the interstitial space, which eventually becomes lipid-rich due to chronic inflammation and fibroblasts stimulating adipogenesis.
*Neutrophilic, protein-rich fluid*
- This description is characteristic of **inflammatory edema** or **purulent exudate**, typically seen in infections.
- The patient's lack of fever, chills, erythema, or warmth makes an infectious or acute inflammatory process unlikely.
*Lymphocytic, hemosiderin-rich fluid*
- **Hemosiderin deposits** are indicative of chronic **venous insufficiency** or recurrent hemorrhages, leading to red blood cell extravasation and breakdown.
- While lymphocytes can be present in chronic inflammation, the primary issue here is lymphatic obstruction, not venous stasis or bleeding.
*Protein-rich, glycosaminoglycan-rich fluid*
- While lymphedema is indeed **protein-rich**, the primary accumulation in mature lymphedema involves **adipose tissue** and fibrosis.
- **Glycosaminoglycans** accumulate significantly in conditions like **myxedema** (hypothyroidism), which was ruled out by the normal thyroid examination.
*Acellular, protein-poor fluid*
- This describes a **transudate**, typically seen in conditions like **heart failure**, **liver cirrhosis**, or **nephrotic syndrome** where there's an imbalance of hydrostatic and oncotic pressures.
- The edema in this case is **non-pitting**, suggesting a higher protein content and tissue changes characteristic of lymphatic dysfunction, not systemic fluid overload leading to protein-poor fluid.
Lower limb lymphatic drainage US Medical PG Question 6: A 72-year-old woman presents with left lower limb swelling. She first noticed her left leg was swollen about 2 weeks ago. She denies any pain and initially thought the swelling would subside on its own. Past medical history is significant for hypertension and hyperlipidemia. She is a smoker with a 35 pack-year history and an occasional drinker. She takes chlorthalidone, lisinopril, atorvastatin and a multivitamin. On physical examination, her left leg appears larger than her right with 2+ pitting edema up to her knee. She also has a few distended superficial veins along the posterior aspect of her left leg. Lower extremities have 2+ pulses bilaterally. The ultrasound of her left lower thigh and leg shows an obstructing thrombosis of the distal portion of the femoral vein. Which of the following veins serve as collateral pathways to help mitigate the consequences of this patient's condition?
- A. Giacomini vein
- B. Fibular vein
- C. Accessory saphenous vein
- D. Perforator veins (Correct Answer)
- E. Deep femoral vein
Lower limb lymphatic drainage Explanation: ***Perforator veins***
- **Perforator veins** connect the **superficial venous system** to the **deep venous system**, normally allowing blood to flow from superficial to deep veins through one-way valves.
- In cases of **deep vein thrombosis (DVT)**, when the deep venous system is obstructed, these veins can serve as **important collateral pathways**, allowing blood to be rerouted from the obstructed deep system to the superficial system, thereby preventing excessive venous engorgement and helping to reduce severe edema.
- This explains the **distended superficial veins** seen on examination in this patient—blood is being diverted through perforators to the superficial system.
*Giacomini vein*
- The **Giacomini vein** is a **superficial vein** connecting the small saphenous vein to the great saphenous vein, typically in the popliteal fossa and posterior thigh.
- It primarily shunts blood within the **superficial system** and does not provide significant collateral drainage when the deep venous system is occluded.
*Fibular vein*
- The **fibular vein** (also known as the peroneal vein) is a **deep vein** of the lower leg, running alongside the fibula and draining into the posterior tibial veins.
- While it is part of the deep venous system, the thrombosis in this case is in the **femoral vein** (more proximal), so the fibular vein would drain into the same obstructed system rather than serving as a bypass collateral.
*Accessory saphenous vein*
- The **accessory saphenous vein** is a **superficial vein** that runs parallel to and is a tributary of the great saphenous vein in the thigh.
- It is part of the superficial system and does not provide a collateral pathway **from** the obstructed deep system, though it may carry increased flow if perforators are diverting blood to the superficial system.
*Deep femoral vein*
- The **deep femoral vein** (profunda femoris vein) is a **deep vein** that drains the deep compartments of the thigh and joins the common femoral vein.
- While it can provide some collateral drainage when the superficial femoral vein (femoral vein) is occluded, it ultimately drains into the **same deep venous system** proximally and is not the primary collateral mechanism connecting superficial and deep systems.
Lower limb lymphatic drainage US Medical PG Question 7: A 76-year-old woman comes to the physician for evaluation of a 3-month history of vulvar itching and pain. She was diagnosed with lichen sclerosus 4 years ago. She has smoked 1 pack of cigarettes daily for 35 years. Physical examination shows a 2.5-cm nodular, ulcerative lesion on the vaginal introitus and left labia minora with surrounding erythema. Punch biopsy shows squamous cell carcinoma. A CT scan of the chest, abdomen, and pelvis shows enlarged lymph nodes concerning for metastatic disease. Which of the following lymph node regions is the most likely primary site of metastasis?
- A. Superficial inguinal (Correct Answer)
- B. Internal iliac
- C. External iliac
- D. Inferior mesenteric
- E. Para-aortic
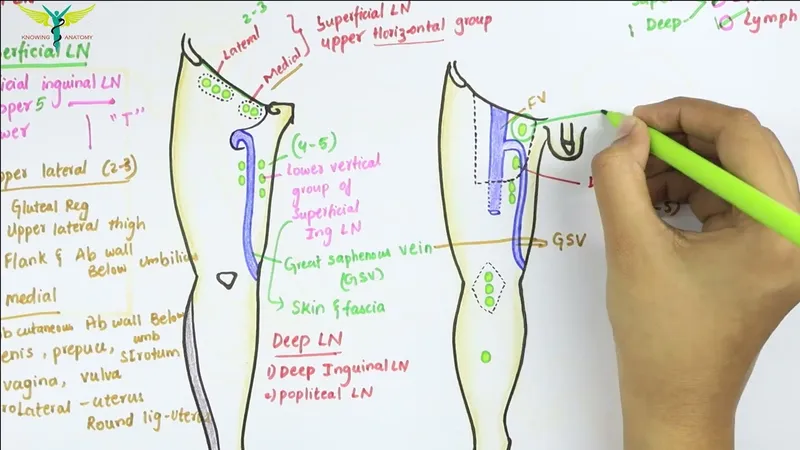
Lower limb lymphatic drainage Explanation: ***Superficial inguinal***
- The **vulva** drains primarily into the **superficial inguinal lymph nodes**, making them the most likely first site for metastatic spread from vulvar squamous cell carcinoma.
- The lesion's location on the **vaginal introitus** and **labia minora** directly correlates with this lymphatic drainage pathway.
*Internal iliac*
- **Internal iliac nodes** receive drainage mainly from deep pelvic structures like the cervix, upper vagina, and uterus, not directly from the vulva.
- Metastasis to these nodes usually occurs after involvement of more superficial nodes or in advanced disease with deeper invasion.
*External iliac*
- **External iliac nodes** generally drain the lower extremities and deeper pelvic structures (e.g., bladder, distal ureter), not the vulva as a primary site.
- Involvement here would typically indicate more advanced local spread or secondary metastasis from other pelvic nodes.
*Inferior mesenteric*
- **Inferior mesenteric nodes** drain the hindgut and its derivatives, including the distal colon and rectum, which are distant from the vulva.
- This region is not involved in the lymphatic drainage of the vulva.
*Para-aortic*
- **Para-aortic nodes** drain structures like the ovaries, fallopian tubes, and upper uterus; they are too superior for primary vulvar lymphatic drainage.
- Metastasis to these nodes from vulvar cancer would signify widespread, very advanced disease and not a primary site of spread.
Lower limb lymphatic drainage US Medical PG Question 8: A 34-year-old woman, gravida 4, para 3, comes to the physician because of left ankle swelling for 2 months. She notes that the swelling is present throughout the day and decreases when she goes to sleep. One year ago, she has had an episode of deep venous thrombosis after the delivery of her third child. Her prepregnancy BMI was 34 kg/m2. Examination shows distended, tortuous veins in the legs bilaterally and pitting edema of the left ankle. There are erythematous scaling patches on the medial side of the left ankle. Duplex ultrasonography is performed. Which of the following directions of blood flow would most likely confirm the diagnosis?
- A. Femoral vein to external iliac vein
- B. Anterior tibial vein to popliteal vein
- C. Femoral vein to great saphenous vein (Correct Answer)
- D. Popliteal vein to small saphenous vein
- E. Dorsal venous arch to great saphenous vein
Lower limb lymphatic drainage Explanation: ***Femoral vein to great saphenous vein***
- This represents **reflux at the saphenofemoral junction (SFJ)**, the most common cause of **chronic venous insufficiency (CVI)**.
- Incompetent valves allow retrograde blood flow from the deep venous system (femoral vein) into the superficial system (great saphenous vein), causing increased venous pressure.
- This leads to the patient's presenting features: **varicose veins** (distended, tortuous veins), **pitting edema**, and **venous stasis dermatitis** (erythematous scaling patches).
- **Duplex ultrasonography** demonstrating this reversed flow pattern confirms the diagnosis of CVI due to SFJ incompetence.
- Risk factors include obesity (BMI 34), previous DVT, and multiple pregnancies—all present in this patient.
*Dorsal venous arch to great saphenous vein*
- This describes **normal antegrade flow** from the superficial dorsal venous arch upward into the great saphenous vein.
- This is the physiological direction of blood flow, not reflux or pathological flow.
- Would not be diagnostic of venous insufficiency.
*Anterior tibial vein to popliteal vein*
- This represents **normal antegrade flow** from the anterior tibial vein (deep vein of the leg) proximally to the popliteal vein.
- This is the normal physiological direction for venous return from the lower leg.
- Not indicative of valvular incompetence or venous insufficiency.
*Femoral vein to external iliac vein*
- This describes **normal antegrade flow** from the femoral vein proximally to the external iliac vein.
- This is the correct physiological direction of venous return from the lower extremity toward the heart.
- Not reflux and would not confirm venous insufficiency.
*Popliteal vein to small saphenous vein*
- This represents reflux at the **saphenopopliteal junction (SPJ)**, a less common site of venous insufficiency.
- While this can cause varicosities in the small saphenous distribution (posterior calf), it is less common than SFJ incompetence.
- The medial ankle location of skin changes and the distribution of findings are more consistent with great saphenous vein involvement than small saphenous vein.
Lower limb lymphatic drainage US Medical PG Question 9: An otherwise healthy 39-year-old woman presents to her primary care provider because of right-leg swelling, which started 4 months ago following travel to Kenya. The swelling has been slowly progressive and interferes with daily tasks. She denies smoking or alcohol use. Family history is irrelevant. Vital signs include: temperature 38.1°C (100.5°F), blood pressure 115/72 mm Hg, and pulse 99/min. Physical examination reveals non-pitting edema of the entire right leg. The overlying skin is rough, thick and indurated. The left leg is normal in size and shape. Which of the following is the most likely cause of this patient condition?
- A. Obstruction of lymphatic channels (Correct Answer)
- B. Hypoalbuminemia
- C. Lymphatic hypoplasia
- D. Venous thromboembolism
- E. Persistent elevation of venous pressures
Lower limb lymphatic drainage Explanation: ***Obstruction of lymphatic channels***
- The patient's history of travel to **Kenya**, along with **progressive, non-pitting edema** of the entire right leg and **rough, thick, indurated skin**, strongly suggests **filariasis**, a parasitic infection that obstructs lymphatic channels.
- **Obstruction of lymphatic channels** leads to **lymphedema**, which characteristically presents with the described symptoms and skin changes (e.g., **elephantiasis**).
*Hypoalbuminemia*
- **Hypoalbuminemia** typically causes **generalized, pitting edema** due to decreased plasma oncotic pressure, not localized, non-pitting edema in a single limb.
- There are no clinical signs to suggest **hepatic** or **renal dysfunction** that would cause significant hypoalbuminemia.
*Lymphatic hypoplasia*
- **Lymphatic hypoplasia** (primary lymphedema) is usually congenital or develops in early life and would not typically manifest acutely after travel in a 39-year-old.
- While it causes lymphedema, the travel history points to an acquired cause rather than a congenital defect.
*Venous thromboembolism*
- **Venous thromboembolism** (DVT) typically presents with acute onset of **painful, edematous** limb, often with **pitting edema**, and can be associated with warmth and erythema.
- The **slowly progressive** nature of the swelling over 4 months and **non-pitting edema** are less consistent with acute DVT.
*Persistent elevation of venous pressures*
- **Persistent elevation of venous pressures** (e.g., chronic venous insufficiency) leads to **pitting edema**, skin discoloration (**hyperpigmentation**), and **ulcerations**, not the rough, thick, indurated skin seen in this case.
- This condition is also typically associated with factors like prolonged standing or obesity, which are not mentioned here.
Lower limb lymphatic drainage US Medical PG Question 10: A 72-year-old male presents to a cardiac surgeon for evaluation of severe aortic stenosis. He has experienced worsening dyspnea with exertion over the past year. The patient also has a history of poorly controlled hypertension, diabetes mellitus, and hyperlipidemia. An echocardiogram revealed a thickened calcified aortic valve. The surgeon is worried that the patient will be a poor candidate for open heart surgery and decides to perform a less invasive transcatheter aortic valve replacement. In order to perform this procedure, the surgeon must first identify the femoral pulse just inferior to the inguinal ligament and insert a catheter into the vessel in order to gain access to the arterial system. Which of the following structures is immediately lateral to this structure?
- A. Lymphatic vessels
- B. Femoral vein
- C. Sartorius muscle
- D. Pectineus muscle
- E. Femoral nerve (Correct Answer)
Lower limb lymphatic drainage Explanation: ***Femoral nerve***
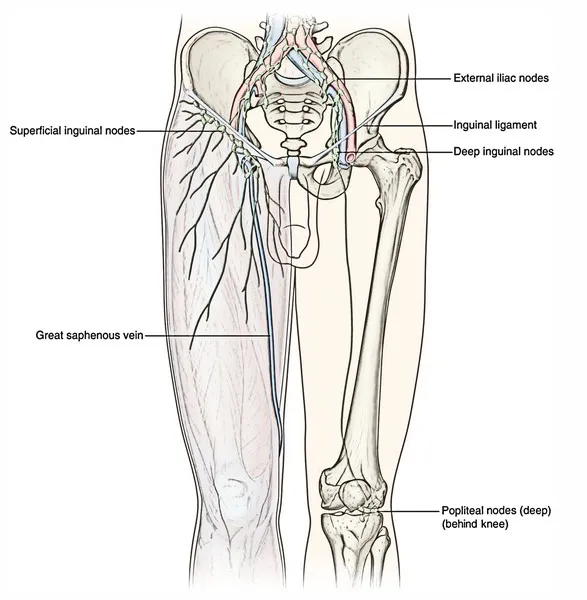
- The **femoral nerve** lies lateral to the **femoral artery** within the **femoral triangle**.
- The order of structures from **lateral to medial** under the inguinal ligament is remembered by the mnemonic **NAVEL**: **N**erve, **A**rtery, **V**ein, **E**mpty space, **L**ymphatics.
*Lymphatic vessels*
- **Lymphatic vessels** and nodes are located most medially within the femoral triangle, medial to the femoral vein.
- This position is not immediately lateral to the femoral artery.
*Femoral vein*
- The **femoral vein** is located immediately medial to the **femoral artery**.
- It would not be found immediately lateral to the femoral artery.
*Sartorius muscle*
- The **sartorius muscle** forms the lateral boundary of the **femoral triangle** but is not immediately adjacent and lateral to the femoral artery within the triangle itself.
- The femoral nerve is enclosed within the iliopsoas fascial compartment, which runs deep to the sartorius.
*Pectineus muscle*
- The **pectineus muscle** forms part of the floor of the **femoral triangle**, but it is deep to the neurovascular structures.
- It is not immediately lateral to the femoral artery.
More Lower limb lymphatic drainage US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.