Abdominal lymphatic drainage US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Abdominal lymphatic drainage. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Abdominal lymphatic drainage US Medical PG Question 1: A 34-year-old patient presents with severe pain in the right upper quadrant that radiates to the right shoulder. During laparoscopic cholecystectomy, which of the following anatomical spaces must be carefully identified to prevent bile duct injury?
- A. Foramen of Winslow
- B. Lesser sac
- C. Calot's triangle (Correct Answer)
- D. Morrison's pouch
Abdominal lymphatic drainage Explanation: ***Calot's triangle***
- **Calot's triangle** is the critical anatomical landmark containing the **cystic artery** and **cystic duct**, whose proper identification is essential to prevent injury to the hepatic artery or bile ducts during cholecystectomy.
- Its boundaries are the **cystic duct** (lateral), the **common hepatic duct** (medial), and the **inferior border of the liver** (superior, sometimes described as the cystic artery).
*Foramen of Winslow*
- The **Foramen of Winslow** (epiploic foramen) is an opening connecting the **greater and lesser sacs** of the peritoneal cavity.
- It is not directly relevant to identifying structures during cholecystectomy, but rather to accessing the lesser sac or for surgical procedures involving structures like the portal triad.
*Lesser sac*
- The **lesser sac** (omental bursa) is a peritoneal cavity posterior to the stomach and lesser omentum.
- It is explored in procedures involving the pancreas, posterior gastric wall, or for assessing fluid collections, but not for direct identification of cystic structures during standard cholecystectomy.
*Morrison's pouch*
- **Morrison's pouch** is the **hepatorenal recess**, a potential space between the posterior aspect of the liver and the right kidney and adrenal gland.
- It is a common site for **fluid accumulation** (e.g., ascites, blood) but is not directly incised or dissected for preventing bile duct injury during cholecystectomy.
Abdominal lymphatic drainage US Medical PG Question 2: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Abdominal lymphatic drainage Explanation: ***Left renal artery***
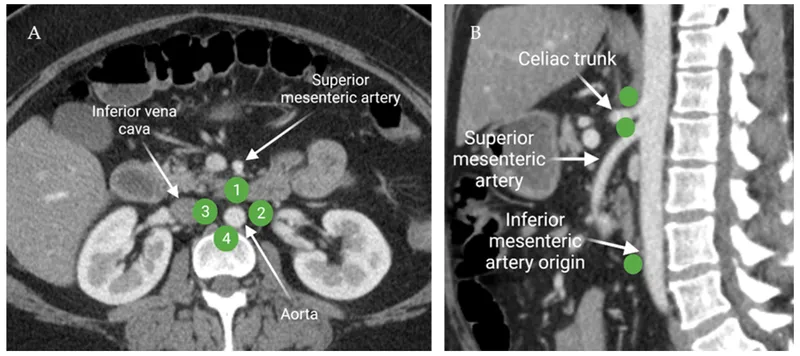
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
Abdominal lymphatic drainage US Medical PG Question 3: A 29-year-old man presents to his primary care provider complaining of testicular pain. He reports a four-day history of dull chronic pain in his left testicle that is worse with standing. His past medical history is notable for asthma and major depressive disorder. He takes inhaled albuterol as needed and sertraline. He is sexually active with a single female partner and always uses barrier protection. His temperature is 99.2°F (37.3°C), blood pressure is 125/75 mmHg, pulse is 85/min, and respirations are 17/min. Physical examination reveals a non-tender twisted mass along the left spermatic cord that disappears when the patient lies supine. This patient’s condition most likely stems from decreased laminar flow at which of the following vascular junctions?
- A. Descending aorta – Left testicular artery
- B. Left testicular vein – Left suprarenal vein
- C. Left testicular vein – Inferior vena cava
- D. Left testicular vein – Left renal vein (Correct Answer)
- E. Left testicular vein – Left internal iliac vein
Abdominal lymphatic drainage Explanation: ***Left testicular vein – Left renal vein***
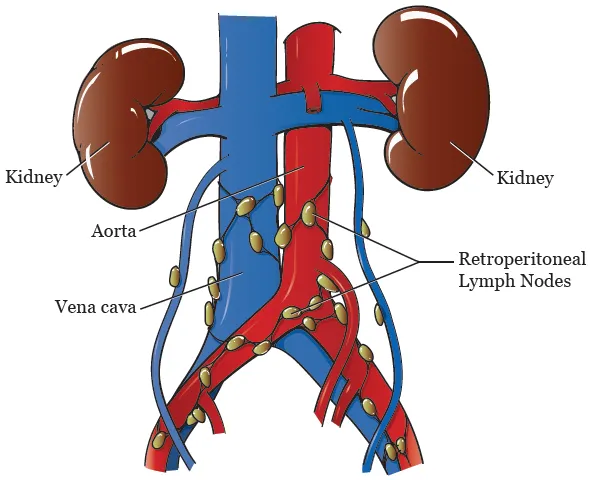
- This clinical presentation of a **nontender, twisted mass along the spermatic cord** that disappears when supine is classic for a **varicocele**. Varicoceles are more common on the left side due to the **anatomic drainage of the left testicular vein** into the left renal vein at a **perpendicular angle**.
- This perpendicular angle, along with the **increased length of the left testicular vein** and its drainage into the higher-pressure left renal vein, creates conditions for **increased hydrostatic pressure** and **decreased laminar flow**, leading to venous engorgement and varicocele formation.
*Descending aorta – Left testicular artery*
- This junction involves an **artery**, not a vein. Varicoceles are caused by **venous insufficiency and dilatation**, not arterial issues.
- The left testicular artery branches directly from the aorta and supplies blood to the testicle; problems with this junction would typically manifest as **ischemia or arterial insufficiency**, not venous congestion.
*Left testicular vein – Left suprarenal vein*
- While the left suprarenal vein also drains into the left renal vein, the **left testicular vein does not directly connect to the left suprarenal vein**.
- This junction is not anatomically relevant to the direct drainage pathway causing a varicocele.
*Left testicular vein – Inferior vena cava*
- The **right testicular vein drains directly into the inferior vena cava**, explaining why varicoceles are less common on the right side.
- The left testicular vein typically drains into the left renal vein, not directly into the inferior vena cava.
*Left testicular vein – Left internal iliac vein*
- The **left internal iliac vein primarily drains pelvic structures** and has no direct anatomical connection or primary drainage role for the left testicular vein.
- The testicular veins follow a retroperitoneal course and do not typically involve the internal iliac venous system in their main drainage.
Abdominal lymphatic drainage US Medical PG Question 4: A 32-year-old man comes to the emergency department because of a wound in his foot. Four days ago, he stepped on a nail while barefoot at the beach. Examination of the plantar surface of his right foot shows a purulent puncture wound at the base of his second toe with erythema and tenderness of the surrounding skin. The afferent lymphatic vessels from the site of the lesion drain directly into which of the following groups of regional lymph nodes?
- A. Popliteal
- B. Deep inguinal
- C. Anterior tibial
- D. Superficial inguinal (Correct Answer)
- E. External iliac
Abdominal lymphatic drainage Explanation: ***Superficial inguinal***
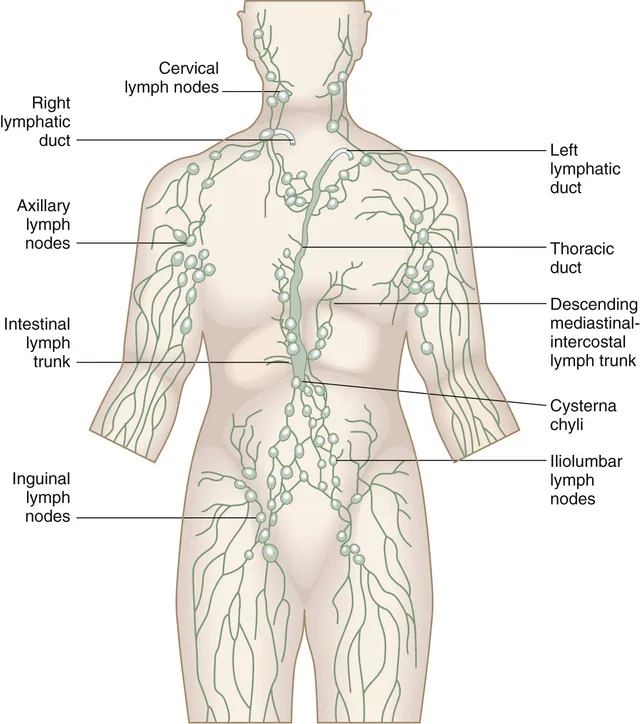
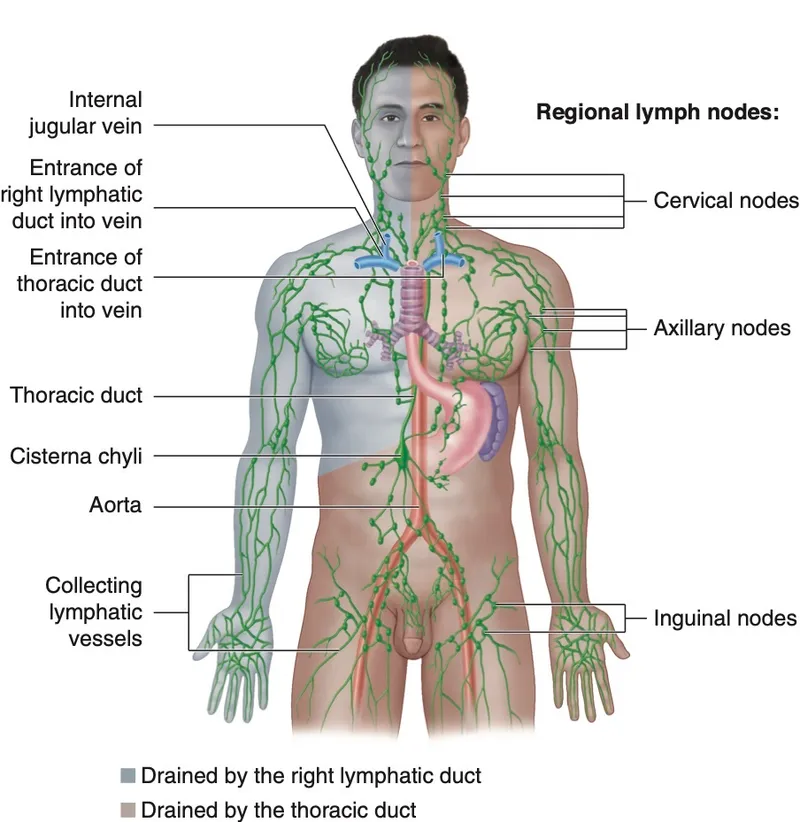
- Lymph from the **plantar surface of the foot** (including the base of the toes) drains into the **superficial inguinal lymph nodes**.
- The **medial and central plantar surfaces** specifically follow the medial superficial lymphatic vessels that accompany the great saphenous vein system to reach these nodes.
- These nodes are the **primary drainage site** and crucial in the initial immune response to infections of the lower limb.
*Popliteal*
- The **popliteal lymph nodes** primarily drain lymph from the **lateral foot and heel**, posterior leg, and knee.
- They are located within the popliteal fossa and would not be the direct drainage site for a wound on the plantar surface of the second toe.
*Deep inguinal*
- **Deep inguinal lymph nodes** receive lymph from the superficial inguinal nodes, as well as from deeper structures of the thigh and glans penis/clitoris.
- They are considered a **secondary drainage site** and not the primary destination for superficial foot infections.
*Anterior tibial*
- There are no well-defined major lymph nodes specifically termed "anterior tibial" that serve as a primary drainage site for the foot.
- Lymphatics generally follow venous drainage patterns, and the anterior tibial vessels drain superiorly, not to a specific nodal group at this level.
*External iliac*
- **External iliac lymph nodes** receive lymph primarily from the deep inguinal nodes and pelvic organs.
- They are a more **proximal group** in the lymphatic chain and not the direct initial drainage site for a foot infection.
Abdominal lymphatic drainage US Medical PG Question 5: A 76-year-old woman comes to the physician for evaluation of a 3-month history of vulvar itching and pain. She was diagnosed with lichen sclerosus 4 years ago. She has smoked 1 pack of cigarettes daily for 35 years. Physical examination shows a 2.5-cm nodular, ulcerative lesion on the vaginal introitus and left labia minora with surrounding erythema. Punch biopsy shows squamous cell carcinoma. A CT scan of the chest, abdomen, and pelvis shows enlarged lymph nodes concerning for metastatic disease. Which of the following lymph node regions is the most likely primary site of metastasis?
- A. Superficial inguinal (Correct Answer)
- B. Internal iliac
- C. External iliac
- D. Inferior mesenteric
- E. Para-aortic
Abdominal lymphatic drainage Explanation: ***Superficial inguinal***
- The **vulva** drains primarily into the **superficial inguinal lymph nodes**, making them the most likely first site for metastatic spread from vulvar squamous cell carcinoma.
- The lesion's location on the **vaginal introitus** and **labia minora** directly correlates with this lymphatic drainage pathway.
*Internal iliac*
- **Internal iliac nodes** receive drainage mainly from deep pelvic structures like the cervix, upper vagina, and uterus, not directly from the vulva.
- Metastasis to these nodes usually occurs after involvement of more superficial nodes or in advanced disease with deeper invasion.
*External iliac*
- **External iliac nodes** generally drain the lower extremities and deeper pelvic structures (e.g., bladder, distal ureter), not the vulva as a primary site.
- Involvement here would typically indicate more advanced local spread or secondary metastasis from other pelvic nodes.
*Inferior mesenteric*
- **Inferior mesenteric nodes** drain the hindgut and its derivatives, including the distal colon and rectum, which are distant from the vulva.
- This region is not involved in the lymphatic drainage of the vulva.
*Para-aortic*
- **Para-aortic nodes** drain structures like the ovaries, fallopian tubes, and upper uterus; they are too superior for primary vulvar lymphatic drainage.
- Metastasis to these nodes from vulvar cancer would signify widespread, very advanced disease and not a primary site of spread.
Abdominal lymphatic drainage US Medical PG Question 6: A 62-year-old female presents to her primary care physician complaining of bloody stool. She reports several episodes of bloody stools over the past two months as well as a feeling of a mass near her anus. She has one to two non-painful bowel movements per day. She has a history of alcohol abuse and hypertension. Anoscopy reveals engorged vessels. Which of the following vessels most likely drains blood from the affected region?
- A. Internal pudendal vein
- B. Left colic vein
- C. Inferior rectal vein (Correct Answer)
- D. Middle rectal vein
- E. Superior rectal vein
Abdominal lymphatic drainage Explanation: ***Inferior rectal vein***
- The patient's symptoms (bloody stool, anal mass, engorged vessels on anoscopy) are classic for **external hemorrhoids**.
- **External hemorrhoids** are distended veins located **below the dentate line** in the anal canal, which are drained by the **inferior rectal veins**.
- The inferior rectal veins drain into the **internal pudendal vein**, then to the **internal iliac vein** (part of the **systemic venous circulation**).
*Internal pudendal vein*
- The **internal pudendal vein** drains structures in the perineum and external genitalia, but it is not the **primary/direct drainage** for hemorrhoids.
- It receives blood from the inferior rectal veins but is one step removed from the hemorrhoidal plexus itself.
*Left colic vein*
- The **left colic vein** typically drains the distal transverse colon and descending colon.
- It is part of the **inferior mesenteric venous system** and is anatomically distant from the anorectal region, not involved in draining hemorrhoids.
*Middle rectal vein*
- The **middle rectal vein** drains the middle part of the rectum and connects both portal and systemic circulations.
- It drains the **muscularis layer** of the rectum but is not the primary drainage for the external hemorrhoidal plexus below the dentate line.
*Superior rectal vein*
- The **superior rectal vein** drains the upper part of the rectum and anal canal **above the dentate line**.
- Distention of these veins leads to **internal hemorrhoids**, which are typically painless unless prolapsed or thrombosed.
- It drains into the **inferior mesenteric vein** (part of the **portal venous circulation**).
Abdominal lymphatic drainage US Medical PG Question 7: A 59-year-old woman presents to her primary care provider with a 6-month history of progressive left-arm swelling. Two years ago she had a partial mastectomy and axillary lymph node dissection for left breast cancer. She was also treated with radiotherapy at the time. Upon further questioning, she denies fever, pain, or skin changes, but reports difficulty with daily tasks because her hand feels heavy and weak. She is bothered by the appearance of her enlarged extremity and has stopped playing tennis. On physical examination, nonpitting edema of the left arm is noted with hyperkeratosis, papillomatosis, and induration of the skin. Limb elevation, exercise, and static compression bandaging are started. If the patient has no improvement, which of the following will be the best next step?
- A. Diethylcarbamazine
- B. Low molecular weight heparin
- C. Endovascular stenting
- D. Vascularized lymph node transfer (Correct Answer)
- E. Antibiotics
Abdominal lymphatic drainage Explanation: ***Vascularized lymph node transfer***
- This patient presents with **secondary lymphedema** due to axillary dissection and radiotherapy, which has not responded to conservative management.
- **Vascularized lymph node transfer** is a surgical option that involves transplanting healthy lymph nodes to the affected area to re-establish lymphatic drainage pathways, offering a more definitive solution for refractory cases.
*Diethylcarbamazine*
- **Diethylcarbamazine** is an anti-filarial drug used to treat lymphedema caused by **parasitic infections**, specifically filariasis.
- The patient's lymphedema is secondary to breast cancer treatment, not parasitic infection, making this a **misdirected treatment**.
*Low molecular weight heparin*
- **Low molecular weight heparin** is an anticoagulant used to prevent or treat **venous thromboembolism (VTE)**.
- While patients with cancer are at increased risk for VTE, her symptoms are consistent with lymphedema and not thrombosis, which would typically present with more acute pain and swelling, making this an inappropriate treatment.
*Endovascular stenting*
- **Endovascular stenting** is a procedure used to open blocked or narrowed **blood vessels**, such as in peripheral artery disease or venous obstruction.
- Her condition is specifically lymphedema, a lymphatic circulation issue, not a vascular obstruction, so stenting would not address the underlying problem.
*Antibiotics*
- **Antibiotics** are used to treat **bacterial infections**, which can complicate lymphedema (e.g., cellulitis).
- While chronic lymphedema causes skin changes (hyperkeratosis, papillomatosis, induration), the patient shows no signs of **acute infection** such as fever, pain, erythema, or warmth, making empirical antibiotics unnecessary at this stage.
Abdominal lymphatic drainage US Medical PG Question 8: A 39-year-old woman presents to her primary care physician because she has been experiencing intermittent abdominal pain for the last 2 weeks. She says that the pain is squeezing in nature, is located in the right upper quadrant, and is particularly severe after eating a meal. After a diagnosis is made, the patient asks why the pain gets worse after eating. The physician explains that food is detected by the gastrointestinal tract through numerous receptors and that this information is transmitted to other parts of the body to cause compensatory changes. The neurons responsible for transmitting this information are most likely located in a layer of the intestine that has which of the following characteristics?
- A. Contracts to generate local movement in mucosa
- B. Contains cells that primarily absorb nutrients
- C. Connective tissue that envelops the other layers
- D. Contracts to generate peristaltic waves (Correct Answer)
- E. Contains large blood vessels and large lymphatic vessels
Abdominal lymphatic drainage Explanation: ***Contracts to generate peristaltic waves***
- This describes the **muscularis propria** (external muscle layer), which contains the **myenteric plexus (Auerbach's plexus)** between its inner circular and outer longitudinal smooth muscle layers.
- The **myenteric plexus is the primary neural network** responsible for detecting food through mechanoreceptors and chemoreceptors, transmitting sensory information, and coordinating both local reflexes and systemic compensatory responses throughout the gastrointestinal tract.
- These neurons communicate with the **autonomic nervous system** and coordinate the release of hormones like **cholecystokinin (CCK)** after eating, which causes gallbladder contraction (relevant to this patient's postprandial pain from cholecystitis).
- While this layer's most obvious function is generating peristalsis, it contains the most extensive enteric nervous system network for sensory integration and motor coordination.
*Contains large blood vessels and large lymphatic vessels*
- This describes the **submucosa**, which contains the **submucosal plexus (Meissner's plexus)**.
- While the submucosal plexus does contain sensory neurons, it primarily regulates **local functions** such as mucosal secretion, absorption, and blood flow rather than the broader systemic compensatory responses described in the question.
- The submucosa's neural network is more limited compared to the myenteric plexus.
*Contracts to generate local movement in mucosa*
- This describes the **muscularis mucosae**, a thin layer of smooth muscle within the mucosa that causes local folding and movement of the mucosal surface.
- This layer lacks significant neural plexuses and is not involved in transmitting sensory information for systemic responses.
*Contains cells that primarily absorb nutrients*
- This refers to the **mucosa**, specifically the epithelial cells lining the intestinal surface.
- While the mucosa contains chemoreceptors and mechanoreceptors, the question asks about the neurons that **transmit** this information, which are located in the deeper neural plexuses (primarily myenteric), not in the absorptive epithelium itself.
*Connective tissue that envelops the other layers*
- This describes the **serosa** (or adventitia), the outermost protective layer.
- The serosa contains minimal neural tissue and is not involved in sensory detection or transmission of gastrointestinal information.
Abdominal lymphatic drainage US Medical PG Question 9: A 23-year-old man comes to the physician because of a whistling sound during respiration for the past 3 weeks. He reports that the whistling is becoming louder, and is especially loud when he exercises. He says the noise is frustrating for him. Six months ago, the patient underwent outpatient treatment for an uncomplicated nasal fracture after being hit in the nose by a high-velocity stray baseball. Since the accident, the patient has been taking aspirin for pain. He has a history of asymptomatic nasal polyps. His temperature is 37°C (98.6°F), pulse is 70/min, respirations are 12/min, and blood pressure is 110/70 mm Hg. Physical examination shows no abnormalities. Which of the following, if performed immediately after the initial nasal fracture, would have prevented the whistling during respiration?
- A. Nasal polyp removal
- B. Nasal septal hematoma drainage (Correct Answer)
- C. Septoplasty
- D. Antibiotic therapy
- E. Rhinoplasty
Abdominal lymphatic drainage Explanation: ***Nasal septal hematoma drainage***
- The whistling sound is indicative of a **nasal septal perforation**, likely caused by pressure necrosis from an undrained septal hematoma after the nasal fracture.
- Prompt drainage of a **nasal septal hematoma** would relieve pressure on the septum and prevent necrosis, thus averting a perforation and the subsequent whistling.
*Nasal polyp removal*
- While the patient has asymptomatic nasal polyps, they are generally not the cause of a whistling sound during respiration unless they are obstructing the airway completely, which typically manifests as difficulty breathing rather than isolated whistling.
- Uncomplicated nasal polyps are **unlikely to cause septal perforation** or the specific symptom of a whistling noise when other potential causes are present.
*Septoplasty*
- Septoplasty is a surgical procedure to correct a **deviated nasal septum**, improving airflow and resolving issues like difficulty breathing or recurrent sinusitis.
- It is performed for a deviated septum but would not have prevented a **septal hematoma-induced perforation** if the hematoma itself was not addressed.
*Antibiotic therapy*
- Antibiotic therapy would primarily be indicated for **bacterial infections**, such as those that might arise from an infected hematoma or a complicated fracture.
- While an infected hematoma could worsen the outcome, antibiotics alone would not prevent the **mechanical damage and pressure necrosis** that leads to perforation from an undrained hematoma.
*Rhinoplasty*
- Rhinoplasty is a cosmetic surgical procedure to **reshape the nose**, primarily focusing on its external appearance.
- It is not indicated for preventing or treating complications like **septal hematomas** or perforations after an acute nasal fracture.
Abdominal lymphatic drainage US Medical PG Question 10: A 7-year-old girl comes in to the emergency department with her mother for swelling of her left periorbital region. Yesterday morning she woke up with a painful, warm, soft lump on her left eyelid. Eye movement does not worsen the pain. Physical examination shows redness and swelling of the upper left eyelid, involving the hair follicles. Upon palpation, the swelling drains purulent fluid. Which of the following is the most likely diagnosis?
- A. Xanthelasma
- B. Chalazion
- C. Dacryocystitis
- D. Blepharitis
- E. Hordeolum (Correct Answer)
Abdominal lymphatic drainage Explanation: ***Hordeolum***
- A hordeolum (stye) is an **acute bacterial infection** of the sebaceous glands of the eyelid, often involving a hair follicle, presenting as a **painful, warm, soft lump with purulent drainage**.
- The swelling of the eyelid **involving hair follicles** and the presence of **purulent fluid** are classic signs of a hordeolum.
*Xanthelasma*
- **Xanthelasma** consists of **yellowish plaques** on the eyelids, typically caused by cholesterol deposits, and is painless and not inflammatory.
- It is a **chronic condition** and does not present with acute pain, warmth, or purulent discharge.
*Chalazion*
- A **chalazion** is a **painless, firm, non-tender nodule** resulting from a blocked meibomian gland, which is usually not painful or associated with acute inflammation and purulence.
- Unlike a hordeolum, it is a **granulomatous reaction** and typically presents as a non-infectious, chronic lesion.
*Dacryocystitis*
- **Dacryocystitis** is an infection of the **lacrimal sac**, located at the inner corner of the eye, presenting with swelling, redness, and pain in that specific area.
- This condition would not typically involve the eyelid's hair follicles or present with general eyelid purulence.
*Blepharitis*
- **Blepharitis** is a **chronic inflammation of the eyelid margins**, characterized by redness, flaking, and crusting of the eyelashes, often with itching or burning.
- It causes **generalized eyelid discomfort and irritation**, but not a localized warm, painful, purulent lump like described in the scenario.
More Abdominal lymphatic drainage US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.