Ultrasound principles and interpretation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ultrasound principles and interpretation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ultrasound principles and interpretation US Medical PG Question 1: A 68-year-old man presents for a screening ultrasound scan. He has been feeling well and is in his usual state of good health. His medical history is notable for mild hypertension and a 100-pack-year tobacco history. He has a blood pressure of 128/86 and heart rate of 62/min. Physical examination is clear lung sounds and regular heart sounds. On ultrasound, an infrarenal aortic aneurysm of 4 cm in diameter is identified. Which of the following is the best initial step for this patient?
- A. Reassurance
- B. Beta-blockers
- C. Urgent repair
- D. Surveillance (Correct Answer)
- E. Elective repair
Ultrasound principles and interpretation Explanation: **Surveillance**
- An **infrarenal aortic aneurysm** of 4 cm in diameter in an asymptomatic patient is typically managed with **regular surveillance** to monitor for growth.
- Surgical intervention is generally reserved for aneurysms larger than 5.5 cm or those that are rapidly expanding or symptomatic.
*Reassurance*
- While it's important to provide reassurance, simply doing so without a concrete plan for follow-up would be inappropriate given the potential for **aneurysm expansion** and rupture.
- The patient's **tobacco history** is a significant risk factor for aneurysm progression and warrants monitoring.
*Beta-blockers*
- Beta-blockers may be part of the medical management for **hypertension** and could theoretically slow aneurysm growth by reducing pulsatile stress.
- However, they are not the primary **initial step** for an asymptomatic aneurysm of this size and do not replace the need for surveillance.
*Urgent repair*
- **Urgent repair** is indicated for symptomatic aneurysms, those that are rapidly expanding, or those showing signs of rupture or impending rupture, none of which are present here.
- A 4 cm aneurysm in an asymptomatic patient does not meet the criteria for **urgent intervention**.
*Elective repair*
- **Elective repair** is typically considered for aneurysms exceeding 5.5 cm in diameter or those that are symptomatic or rapidly growing.
- A 4 cm aneurysm is below the threshold for **elective repair** in an asymptomatic patient without other high-risk features.
Ultrasound principles and interpretation US Medical PG Question 2: A 67-year-old man with type 2 diabetes mellitus comes to the emergency department because of lightheadedness over the past 2 hours. He reports that he has had similar episodes of lightheadedness and palpitations over the past 3 days. His only medication is metformin. His pulse is 110/min and irregularly irregular. An ECG shows a variable R-R interval and absence of P waves. The patient undergoes transesophageal echocardiography. During the procedure, the tip of the ultrasound probe is angled posteriorly within the esophagus. This view is most helpful for evaluating which of the following conditions?
- A. Myxoma in the left atrium
- B. Thrombus in the left pulmonary artery
- C. Thrombus in the left ventricular apex
- D. Tumor in the right main bronchus
- E. Aneurysm of the descending aorta (Correct Answer)
Ultrasound principles and interpretation Explanation: ***Aneurysm of the descending aorta***
- When the TEE probe is angled **posteriorly within the esophagus**, it optimally visualizes structures directly posterior to the esophagus, particularly the **descending thoracic aorta**.
- The descending aorta runs parallel and immediately posterior to the esophagus, making this the ideal view for evaluating **aortic aneurysms, dissections, and atherosclerotic disease** of the descending aorta.
- Note: This patient's symptoms (lightheadedness, palpitations) are due to **atrial fibrillation** (irregularly irregular rhythm, absent P waves). The TEE is likely being performed for stroke risk evaluation, but this question tests knowledge of TEE probe positioning and anatomical visualization.
*Myxoma in the left atrium*
- The left atrium is best visualized using **mid-esophageal views** (especially the 4-chamber view at 0-20 degrees), not a posteriorly angled view.
- While TEE is excellent for detecting left atrial myxomas and is commonly performed in AFib patients to evaluate for left atrial appendage thrombus, the posterior angle is not optimal for this structure.
*Thrombus in the left pulmonary artery*
- The pulmonary arteries are located **anterior** to the esophagus, making them poorly visualized with a posteriorly angled probe.
- Pulmonary artery evaluation requires **anterior or superior angulation** of the TEE probe, or CT pulmonary angiography is preferred for pulmonary embolism diagnosis.
*Thrombus in the left ventricular apex*
- The left ventricular apex is best visualized using **transgastric views** (probe in stomach looking upward), not posterior esophageal views.
- LV apex thrombus evaluation requires short-axis and 2-chamber transgastric views at 0-90 degrees.
*Tumor in the right main bronchus*
- The bronchi are **anterior** to the esophagus and are not adequately visualized with TEE, regardless of probe angle.
- TEE is designed for cardiac and great vessel evaluation, not airway pathology; bronchoscopy or CT chest would be appropriate for bronchial tumors.
Ultrasound principles and interpretation US Medical PG Question 3: A 62-year-old woman comes to the physician because of a 2-month history of exertional shortness of breath and fatigue. She sometimes wakes up at night coughing and gasping for air. Cardiac examination shows a grade 3/6 holosystolic murmur best heard at the apex. Which of the following physical exam findings would be consistent with an exacerbation of this patient's condition?
- A. Head bobbing
- B. Early diastolic extra heart sound (Correct Answer)
- C. Prominent V wave
- D. Radiation of the murmur to the axilla
- E. Absence of A2 heart sound
Ultrasound principles and interpretation Explanation: ***Early diastolic extra heart sound***
- The patient's symptoms (dyspnea, orthopnea, paroxysmal nocturnal dyspnea) and holosystolic murmur at the apex are consistent with **mitral regurgitation**, leading to **left ventricular dysfunction** and elevated left atrial pressures.
- An early diastolic extra heart sound, or an **S3 gallop**, indicates increased left ventricular end-diastolic pressure and volume overload, a classic finding in **decompensated heart failure**.
- This is a key sign of **acute exacerbation** when heart failure worsens.
*Head bobbing*
- **Head bobbing** (De Musset's sign) is a peripheral sign of **severe aortic regurgitation**, not mitral regurgitation.
- This sign represents the rhythmic bobbing of the head with each heartbeat due to the large pulse pressure from AR.
*Prominent V wave*
- A prominent V wave in the jugular venous pressure waveform is associated with **tricuspid regurgitation**, reflecting increased right atrial pressure during ventricular systole.
- While jugular venous distention can occur in severe biventricular failure, this specific finding is characteristic of TR, not MR exacerbation.
*Radiation of the murmur to the axilla*
- **Radiation of the murmur to the axilla** is a characteristic finding of the **mitral regurgitation murmur itself**, present at baseline in this patient.
- This describes the location and transmission of the existing murmur, not a new finding indicating acute exacerbation or decompensation.
- The question asks for a sign of exacerbation, requiring evidence of worsening heart failure.
*Absence of A2 heart sound*
- **Absence of the A2 heart sound** suggests severe **aortic stenosis**, where the aortic valve leaflets are so rigid and immobile they do not produce an audible closing sound.
- This finding is unrelated to mitral regurgitation or its exacerbation.
Ultrasound principles and interpretation US Medical PG Question 4: A 65-year-old male with a history of coronary artery disease and myocardial infarction status post coronary artery bypass graft (CABG) surgery presents to his cardiologist for a routine appointment. On physical exam, the cardiologist appreciates a holosystolic, high-pitched blowing murmur heard loudest at the apex and radiating towards the axilla. Which of the following is the best predictor of the severity of this patient's murmur?
- A. Enhancement with expiration
- B. Presence of audible S3 (Correct Answer)
- C. Enhancement with hand grip maneuver
- D. Presence of audible S4
- E. Enhancement with inspiration
Ultrasound principles and interpretation Explanation: ***Presence of audible S3***
- An **S3 gallop** indicates rapid ventricular filling into a stiff or volume-overloaded ventricle, suggesting significant ventricular dysfunction due to severe regurgitation and increased preload.
- In the context of **mitral regurgitation (MR)**, an S3 is a strong predictor of **severe MR** and associated **left ventricular dysfunction**.
*Enhancement with expiration*
- This maneuver typically enhances **left-sided heart murmurs**, including mitral regurgitation, by increasing venous return to the left side of the heart.
- While it confirms the murmur's origin, it does not directly predict the **severity** of the regurgitation.
*Enhancement with hand grip maneuver*
- The **handgrip maneuver** increases afterload, which can enhance the intensity of murmurs associated with regurgitant lesions like mitral regurgitation.
- While helpful in identifying MR, it is not the best predictor of its **severity** compared to signs of ventricular dysfunction.
*Presence of audible S4*
- An **S4 heart sound** is associated with reduced ventricular compliance and atrial contraction against a stiff ventricle, often seen in conditions like **hypertension** or **aortic stenosis**.
- It does not directly indicate the **severity of mitral regurgitation** or current ventricular volume overload.
*Enhancement with inspiration*
- This maneuver typically enhances **right-sided heart murmurs** by increasing venous return to the right side of the heart.
- Since mitral regurgitation is a **left-sided murmur**, inspiration would likely have little to no effect or diminish its intensity.
Ultrasound principles and interpretation US Medical PG Question 5: A 17-year-old previously healthy, athletic male suddenly falls unconscious while playing soccer. His athletic trainer comes to his aid and notes that he is pulseless. He begins performing CPR on the patient until the ambulance arrives but the teenager is pronounced dead when the paramedics arrived. Upon investigation of his primary care physician's office notes, it was found that the child had a recognized murmur that was ruled to be "benign." Which of the following conditions would have increased the intensity of the murmur?
- A. Inspiration
- B. Placing the patient in a squatting position
- C. Valsalva (Correct Answer)
- D. Passive leg raise
- E. Handgrip
Ultrasound principles and interpretation Explanation: ***Valsalva***
- The patient's sudden death after collapsing during soccer, coupled with a previously noted "benign" murmur, strongly suggests **hypertrophic obstructive cardiomyopathy (HOCM)**, which is a common cause of sudden cardiac death in young athletes. The **Valsalva maneuver** decreases preload and left ventricular volume, thereby **increasing the left ventricular outflow tract (LVOT) obstruction** and hence the intensity of the HOCM murmur.
- This maneuver reduces venous return to the heart, leading to reduced ventricular filling and decreased stroke volume. This exacerbates the obstruction in HOCM, making the murmur louder.
*Inspiration*
- **Inspiration** typically **increases venous return to the right side of the heart**, which would generally intensify right-sided murmurs (e.g., tricuspid regurgitation).
- It would have **minimal effect or slightly decrease** the intensity of a left-sided obstructive murmur like that in HOCM, as it does not directly increase the LVOT obstruction.
*Placing the patient in a squatting position*
- Squatting increases both **preload** and **afterload** by increasing systemic vascular resistance and venous return.
- This increase in ventricular volume would **reduce the outflow tract obstruction** in HOCM, thereby **decreasing the intensity of the murmur**.
*Passive leg raise*
- A **passive leg raise** increases **venous return** and thus **preload**, leading to increased ventricular filling.
- Similar to squatting, this increased left ventricular volume would **reduce the left ventricular outflow tract obstruction** associated with HOCM, thereby **decreasing the murmur's intensity**.
*Handgrip*
- The **handgrip maneuver** primarily **increases afterload** and, to some extent, preload by increasing systemic vascular resistance.
- While it can increase the intensity of murmurs like mitral regurgitation and ventricular septal defect, it would generally **decrease or have no significant effect** on the murmur of HOCM due to the increased ventricular volume reducing the outflow obstruction.
Ultrasound principles and interpretation US Medical PG Question 6: A 60-year-old male engineer who complains of shortness of breath when walking a few blocks undergoes a cardiac stress test because of concern for coronary artery disease. During the test he asks his cardiologist about what variables are usually used to quantify the functioning of the heart. He learns that one of these variables is stroke volume. Which of the following scenarios would be most likely to lead to a decrease in stroke volume?
- A. Anxiety
- B. Heart failure (Correct Answer)
- C. Exercise
- D. Pregnancy
- E. Digitalis
Ultrasound principles and interpretation Explanation: ***Heart failure***
- In **heart failure**, the heart's pumping ability is impaired, leading to a reduced **ejection fraction** and thus a decreased **stroke volume**.
- The weakened myocardium cannot effectively contract to expel the normal volume of blood, resulting in lower blood output per beat.
*Anxiety*
- **Anxiety** typically causes an increase in **sympathetic nervous system** activity, leading to increased heart rate and myocardial contractility.
- This often results in a temporary **increase in stroke volume** due to enhanced cardiac performance, not a decrease.
*Exercise*
- During **exercise**, there is a significant **increase in venous return** and sympathetic stimulation, leading to increased **end-diastolic volume** and contractility.
- This physiological response causes a substantial **increase in stroke volume** to meet the body's higher oxygen demands.
*Pregnancy*
- **Pregnancy** leads to significant **physiological adaptations** to accommodate the growing fetus, including a substantial increase in **blood volume**.
- This increased blood volume and cardiac output result in an **increase in stroke volume** to maintain adequate perfusion for both mother and fetus.
*Digitalis*
- **Digitalis** is a cardiac glycoside that **increases intracellular calcium** in myocardial cells, enhancing the **force of contraction**.
- This positive inotropic effect leads to an **increased stroke volume** by improving the heart's pumping efficiency.
Ultrasound principles and interpretation US Medical PG Question 7: A 65-year-old man comes to the physician for a routine examination. He feels well. His pulse is 80/min and blood pressure is 140/85 mm Hg. Cardiac examination shows a holosystolic murmur in the 4th intercostal space along the left sternal border that gets louder during inspiration. The increase of this patient's murmur is best explained by which of the following hemodynamic changes?
- A. Increased systemic venous compliance
- B. Decreased pulmonary vessel capacity
- C. Decreased left ventricular preload
- D. Increased peripheral vascular resistance
- E. Increased right ventricular stroke volume (Correct Answer)
Ultrasound principles and interpretation Explanation: ***Increased right ventricular stroke volume***
- The murmur's location at the **left sternal border** in the 4th intercostal space, combined with its **holosystolic** nature and **inspiratory increase**, points to **tricuspid regurgitation**.
- During **inspiration**, intrathoracic pressure decreases, leading to **increased venous return** to the right side of the heart, thereby increasing the **right ventricular stroke volume** and the intensity of a right-sided murmur.
*Increased systemic venous compliance*
- An increase in systemic venous compliance would cause a **decrease in venous return** to the right heart due to venous pooling, which would **decrease** the intensity of right-sided murmurs.
- This condition would lead to a reduction in preload, not an increase needed to augment the murmur.
*Decreased pulmonary vessel capacity*
- A decrease in pulmonary vessel capacity would primarily affect **pulmonary hypertension** and right ventricular afterload, rather than directly increasing right ventricular stroke volume or the intensity of a tricuspid regurgitation murmur during inspiration.
- It would hinder blood flow from the right ventricle to the pulmonary artery, not enhance it.
*Decreased left ventricular preload*
- While deep inspiration can mildly decrease left ventricular preload due to pooling of blood in the pulmonary circulation, this effect is relevant for **left-sided murmurs** and would cause their intensity to **decrease**.
- This change would not explain the observed increase in a right-sided murmur.
*Increased peripheral vascular resistance*
- Increased peripheral vascular resistance would primarily affect the **left side of the heart** as the left ventricle would have to pump against a higher afterload.
- This would typically **increase** the intensity of **left-sided murmurs** like aortic stenosis or mitral regurgitation but would not directly explain the inspiratory increase of a right-sided murmur.
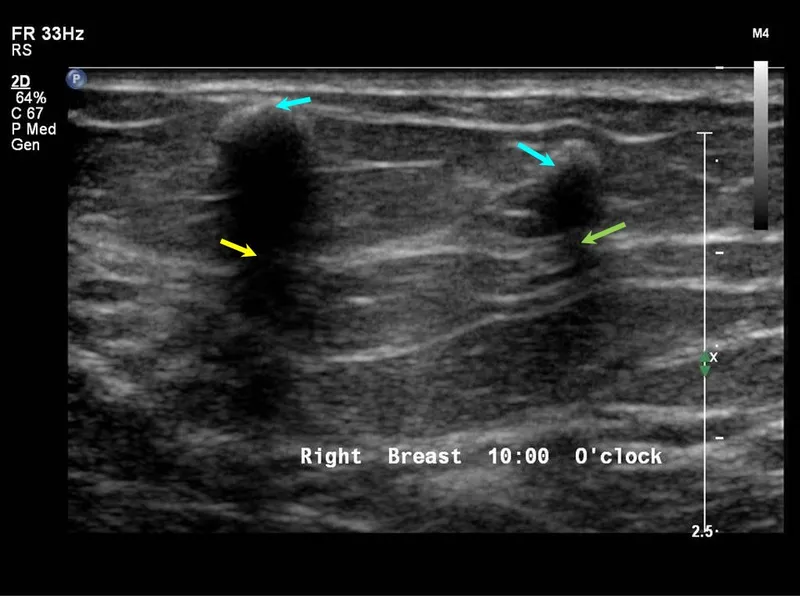
Ultrasound principles and interpretation US Medical PG Question 8: A 24-year-old woman comes to the physician for an annual routine examination. Menses occur at regular 28-day intervals and last for 4 days with normal flow. Her last menstrual period was 3 weeks ago. She is sexually active with one male partner and they use condoms consistently. The patient is 160 cm (5 ft 3 in) tall and weighs 72 kg (150 lb); BMI is 28.1 kg/m2. She feels well. Pelvic examination shows a smooth, mobile right adnexal mass. A subsequent ultrasound of the pelvis shows a single, 2-cm large, round, hypoechoic mass with a thin, smooth wall in the right ovary. The mass has posterior wall enhancement, and there are no signs of blood flow or septae within the mass. Which of the following is the most appropriate next step in management?
- A. Diagnostic laparoscopy
- B. CT scan of the pelvis
- C. Oral contraceptive
- D. CA-125 level
- E. Follow-up examination (Correct Answer)
Ultrasound principles and interpretation Explanation: ***Follow-up examination***
- The ultrasound findings of a **small (2-cm)**, **simple (hypoechoic, thin-walled, no septations, no blood flow)** adnexal cyst in a **premenopausal woman** are characteristic of a functional ovarian cyst.
- Functional cysts are typically benign and resolve spontaneously, making **expectant management with follow-up** the most appropriate initial step.
*Diagnostic laparoscopy*
- This is an **invasive surgical procedure** indicated for suspicious or persistent ovarian masses that require histological evaluation or removal.
- It is **not warranted for a small, simple cyst** with benign features found incidentally in an asymptomatic, premenopausal woman.
*CT scan of the pelvis*
- A CT scan provides additional imaging but exposes the patient to **radiation** and is generally reserved for masses with **complex features** or when evaluating for metastasis.
- It is **not necessary for a simple cyst** that has already been well-characterized by ultrasound.
*Oral contraceptive*
- While oral contraceptives can **suppress ovulation** and potentially prevent the formation of new functional cysts, they generally do **not hasten the resolution of existing cysts**.
- They are sometimes used in cases of recurrent functional cysts but are not the primary management for an initial, asymptomatic simple cyst.
*CA-125 level*
- **CA-125** is a tumor marker primarily used for monitoring ovarian cancer, especially in **postmenopausal women** or those with highly suspicious masses.
- Its levels can be elevated in various benign conditions, and it is **not indicated for a small, simple cyst** in a premenopausal woman, where the risk of malignancy is very low.
Ultrasound principles and interpretation US Medical PG Question 9: A 27-year-old man presents to the emergency department with back pain. The patient states that he has back pain that has been steadily worsening over the past month. He states that his pain is worse in the morning but feels better after he finishes at work for the day. He rates his current pain as a 7/10 and says that he feels short of breath. His temperature is 99.5°F (37.5°C), blood pressure is 130/85 mmHg, pulse is 80/min, respirations are 14/min, and oxygen saturation is 99% on room air. On physical exam, you note a young man who does not appear to be in any distress. Cardiac exam is within normal limits. Pulmonary exam is notable only for a minor decrease in air movement bilaterally at the lung bases. Musculoskeletal exam reveals a decrease in mobility of the back in all four directions. Which of the following is the best initial step in management of this patient?
- A. MRI of the sacroiliac joint (Correct Answer)
- B. CT scan of the chest
- C. Pulmonary function tests
- D. Ultrasound
- E. Radiography of the lumbosacral spine
Ultrasound principles and interpretation Explanation: ***MRI of the sacroiliac joint***
- The patient's symptoms of **worsening back pain**, morning stiffness that improves with activity, and decreased back mobility are highly suggestive of **ankylosing spondylitis**.
- **MRI** is the most sensitive imaging modality for detecting early inflammatory changes in the **sacroiliac joints** and spine, which are characteristic of ankylosing spondylitis, even before radiographic changes are visible.
*CT scan of the chest*
- While the patient reports feeling **short of breath**, his vital signs and oxygen saturation are normal, and he does not appear in acute distress.
- A CT scan of the chest would be a more appropriate step if there were clearer signs of acute pulmonary pathology, such as significant hypoxemia, fever, or adventitious lung sounds, which are not present here.
*Pulmonary function tests*
- **Shortness of breath** could eventually be a complication of severe ankylosing spondylitis due to restricted chest wall expansion.
- However, PFTs are generally not the *initial* diagnostic step given the primary presentation of back pain and the need to confirm the underlying rheumatologic condition first.
*Ultrasound*
- **Ultrasound** is not a primary imaging modality for evaluating the sacroiliac joints or the spine in the context of suspected ankylosing spondylitis.
- It could be useful for assessing peripheral joint inflammation in other arthropathies, but not for axial involvement.
*Radiography of the lumbosacral spine*
- **X-rays of the lumbosacral spine** might show changes in advanced ankylosing spondylitis (e.g., squaring of vertebrae, syndesmophytes), but they are often normal in the early stages of the disease.
- **MRI** is superior for detecting early inflammatory changes and is often used to diagnose the condition before radiographic damage is evident.
Ultrasound principles and interpretation US Medical PG Question 10: A 71-year-old man with type 2 diabetes mellitus comes to the physician because of a 9-month history of pain and stiffness in the right knee. He reports that the stiffness lasts approximately 10 minutes after waking up and that the pain is worse in the evening. There is no history of trauma. He is 175 cm (5 ft 9 in) tall and weighs 102 kg (225 lb); BMI is 33 kg/m2. Examination of the right knee shows tenderness in the anteromedial joint line and crepitus during knee movement. Laboratory studies show an erythrocyte sedimentation rate of 15 mm/h and a serum uric acid concentration of 6.9 mg/dL. Which of the following is the most likely finding on imaging of the right knee?
- A. Osteophytes and narrowing of the joint-space (Correct Answer)
- B. Loculated epiphyseal cyst with thinning of the overlying cortex
- C. Bony ankylosis and bone proliferation at the entheses
- D. Marginal bony erosions and opacification of periarticular soft tissue
- E. Periarticular osteopenia and pannus formation
Ultrasound principles and interpretation Explanation: ***Osteophytes and narrowing of the joint-space***
- The patient's symptoms (age, knee pain worse in evening, short morning stiffness, obesity, crepitus, anteromedial tenderness) are classic for **osteoarthritis (OA)**.
- **Osteoarthritis** is characterized by the breakdown of articular cartilage, leading to bone-on-bone friction, resulting in **joint space narrowing** and the formation of **osteophytes** (bone spurs) at the joint margins, which are readily visible on imaging.
*Loculated epiphyseal cyst with thinning of the overlying cortex*
- This finding is more characteristic of a **chondroblastoma** or an **aneurysmal bone cyst**, which are typically seen in younger individuals and present with localized pain, swelling, and sometimes pathologic fractures, rather than the chronic, activity-related pain of OA.
- While subchondral cysts can occur in severe OA, a large, loculated epiphyseal cyst with cortical thinning is not the primary or most characteristic radiographic finding and would suggest a different etiology.
*Bony ankylosis and bone proliferation at the entheses*
- **Bony ankylosis** (fusion of joints) and **enthesitis** (inflammation and ossification at tendon/ligament insertions) are hallmark features of **spondyloarthropathies** like ankylosing spondylitis, not osteoarthritis.
- The patient's symptoms do not suggest an inflammatory arthritis (e.g., morning stiffness is 10 minutes, not hours, and ESR is normal).
*Marginal bony erosions and opacification of periarticular soft tissue*
- **Marginal bony erosions** (rat-bite erosions) and **periarticular soft tissue opacification** (due to monosodium urate crystal deposition) are characteristic findings of **gout**.
- While the patient has an elevated serum uric acid (6.9 mg/dL), this level is within the normal range for some labs and not definitively diagnostic of gout, especially without acute inflammatory flares or tophi. The chronic, activity-related nature of the pain is inconsistent with acute gout.
*Periarticular osteopenia and pannus formation*
- **Periarticular osteopenia** (bone thinning around the joint) and **pannus formation** (granulation tissue that erodes cartilage and bone) are characteristic features of **rheumatoid arthritis**.
- The patient's presentation (older age, pain worse with activity, short morning stiffness, no systemic inflammatory signs) is inconsistent with rheumatoid arthritis.
More Ultrasound principles and interpretation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.