MRI principles and interpretation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for MRI principles and interpretation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
MRI principles and interpretation US Medical PG Question 1: A 72-year-old man is brought to the physician by his wife for memory issues over the last 7 months. The patient's wife feels that he has gradually become more forgetful. He commonly misplaces his car keys and forgets his children's names. He seems to have forgotten how to make dinner and sometimes serves uncooked noodles or raw meat. One night he parked his car in a neighbor's bushes and was found wandering the street. He has a history of hypertension, hyperlipidemia, and COPD. Current medications include atorvastatin, metoprolol, ipratropium, and fluticasone. Vital signs are within normal limits. He is alert and oriented to person and place only. Neurologic examination shows no focal findings. His Mini-Mental State Examination score is 19/30. A complete blood count and serum concentrations of electrolytes, urea nitrogen, creatinine, thyroid-stimulating hormone, liver function tests, vitamin B12 (cobalamin), and folate are within the reference range. Which of the following is the most appropriate next step in diagnosis?
- A. Electroencephalography
- B. PET scan
- C. MRI of the brain (Correct Answer)
- D. Lumbar puncture
- E. Neuropsychologic testing
MRI principles and interpretation Explanation: ***MRI of the brain***
- An **MRI of the brain** is crucial for evaluating **structural causes of cognitive impairment**, such as tumors, strokes, hydrocephalus, or significant atrophy that might explain the patient's rapidly progressing memory loss and functional decline.
- Given the patient's age, rapidly worsening dementia symptoms, and normal initial lab work, imaging is essential to rule out **reversible or treatable causes** and to characterize the extent of neurodegeneration.
*Electroencephalography*
- **EEG** is primarily used to detect **seizure activity** or to evaluate for rapidly progressive encephalopathies like Creutzfeldt-Jakob disease, which is not indicated by the patient's presentation.
- The patient's symptoms are consistent with a dementia syndrome, not acute encephalopathy or seizures.
*PET scan*
- A **PET scan** (e.g., FDG-PET or amyloid-PET) can provide information about metabolic activity or amyloid plaques, useful for **differentiating types of dementia** (e.g., Alzheimer's disease).
- However, it is an advanced test typically considered after structural imaging has ruled out other causes and when the diagnosis remains unclear.
*Lumbar puncture*
- **Lumbar puncture** is performed to analyze **cerebrospinal fluid (CSF)** for biomarkers (e.g., tau, Aβ42 levels) to help diagnose specific neurodegenerative diseases like Alzheimer's or to rule out infectious/inflammatory causes.
- It's usually reserved for cases where other investigations are inconclusive or specific conditions are strongly suspected, and structural imaging has been performed.
*Neuropsychologic testing*
- **Neuropsychologic testing** provides a detailed assessment of various cognitive domains and can help to **characterize the pattern and severity of cognitive impairment**.
- While valuable, it is usually performed after initial medical workup and structural imaging to understand the functional impact of any identified brain changes or to further delineate the type of cognitive disorder.
MRI principles and interpretation US Medical PG Question 2: A 36-year-old male is taken to the emergency room after jumping from a building. Bilateral fractures to the femur were stabilized at the scene by emergency medical technicians. The patient is lucid upon questioning and his vitals are stable. Pain only at his hips was elicited. Cervical exam was not performed. What is the best imaging study for this patient?
- A. AP and lateral radiographs of hips
- B. Lateral radiograph (x-ray) of hips
- C. Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area
- D. Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area
- E. Computed tomography (CT) scan of cervical spine, hips, and lumbar area (Correct Answer)
MRI principles and interpretation Explanation: ***Computed tomography (CT) scan of cervical spine, hips, and lumbar area***
- In **high-energy trauma** (fall from height), a CT scan is the **gold standard** for evaluating the **spine and pelvis**, providing detailed cross-sectional images superior to plain radiographs.
- Since the **cervical exam was not performed**, cervical spine imaging is **mandatory** per ATLS (Advanced Trauma Life Support) protocols. High-energy falls carry significant risk of **cervical spine injury** even without obvious neurological symptoms.
- CT allows comprehensive assessment of **hip fractures, pelvic injuries, and the entire spine** (cervical, thoracic, lumbar), identifying both obvious and **subtle fractures** that may be missed on plain films.
- This approach provides the most **efficient and thorough evaluation** in the acute trauma setting, allowing for appropriate surgical planning and ruling out life-threatening spinal instability.
*AP and lateral radiographs of hips*
- Plain radiographs provide **limited detail** and may **miss subtle fractures**, particularly in complex areas like the pelvis and acetabulum.
- This option **fails to address cervical spine clearance**, which is essential in all high-energy trauma patients, especially when cervical exam has not been performed.
- Radiographs are insufficient for **comprehensive trauma evaluation** after a fall from height.
*Lateral radiograph (x-ray) of hips*
- A single lateral view is **grossly insufficient** for evaluating hip and pelvic fractures, providing only a **two-dimensional perspective** that can miss significant injuries.
- This option **completely neglects spinal evaluation**, which is dangerous in an uncleared trauma patient with a high-energy mechanism.
*Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area*
- While MRI excels at evaluating **soft tissues, ligaments, and bone marrow**, it is **not the initial imaging modality** for acute bony trauma due to longer scan times and lower sensitivity for acute fractures compared to CT.
- MRI is **time-consuming and impractical** in the emergency setting for initial fracture assessment, potentially delaying definitive treatment.
- CT is superior for evaluating **acute skeletal injuries** in the trauma bay.
*Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area*
- Multiple plain radiographs have **limited sensitivity** for complex or non-displaced fractures, particularly in the **spine and pelvis**, making them inadequate for high-energy trauma evaluation.
- Obtaining multiple radiographic views requires **numerous patient repositionings**, which risks further injury if **spinal instability** is present.
- Plain films provide significantly **less diagnostic information** than CT scanning for trauma assessment.
MRI principles and interpretation US Medical PG Question 3: A 65-year-old man is referred by his primary care provider to a neurologist for leg pain. He reports a 6-month history of progressive bilateral lower extremity pain that is worse in his left leg. The pain is 5/10 in severity at its worst and is described as a "burning" pain. He has noticed that the pain is acutely worse when he walks downhill. He has started riding his stationary bike more often as it relieves his pain. His past medical history is notable for hypertension, diabetes mellitus, and a prior myocardial infarction. He also sustained a distal radius fracture the previous year after falling on his outstretched hand. He takes aspirin, atorvastatin, metformin, glyburide, enalapril, and metoprolol. He has a 30-pack-year smoking history and drinks 2-3 glasses of wine with dinner every night. His temperature is 99°F (37.2°C), blood pressure is 145/85 mmHg, pulse is 91/min, and respirations are 18/min. On exam, he is well-appearing and in no acute distress. A straight leg raise is negative. A valsalva maneuver does not worsen his pain. Which of the following is the most appropriate test to confirm this patient's diagnosis?
- A. Electromyography
- B. Ankle-brachial index
- C. Computerized tomography myelography
- D. Magnetic resonance imaging (Correct Answer)
- E. Radiography
MRI principles and interpretation Explanation: **Magnetic resonance imaging**
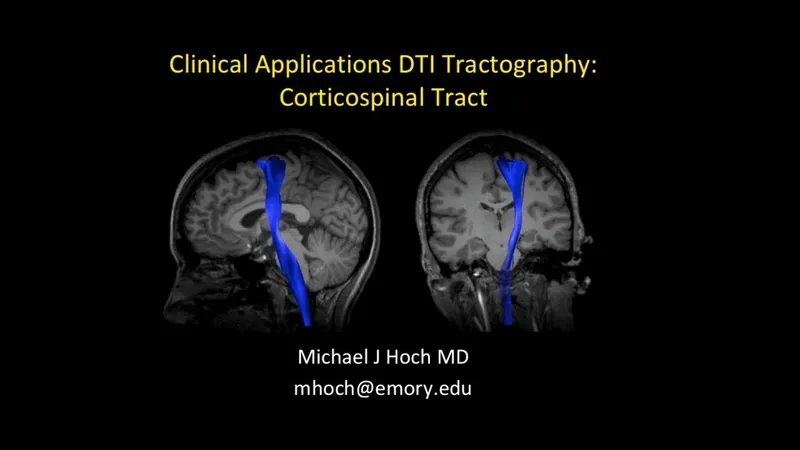
- **Magnetic resonance imaging (MRI)** is the most appropriate test for diagnosing **lumbar spinal stenosis** because it provides detailed imaging of soft tissues, including the **spinal cord, nerve roots, and intervertebral discs**.
- The patient's symptoms of bilateral lower extremity pain, worse with downhill walking and relieved by stationary biking (which typically involves a flexed spine), are classic for **neurogenic claudication** caused by spinal stenosis.
*Electromyography*
- **Electromyography (EMG)** measures electrical activity of muscles and can identify **radiculopathy** or **neuropathy** but does not directly visualize the spinal canal or its contents to diagnose the cause of nerve compression.
- While it could show nerve root involvement, it wouldn't be the primary diagnostic test to confirm **spinal stenosis** itself.
*Ankle-brachial index*
- The **ankle-brachial index (ABI)** is used to diagnose **peripheral artery disease (PAD)**, which can also cause leg pain with activity (**vascular claudication**).
- However, the patient's pain being worse with downhill walking and relieved by spine flexion (like on a stationary bike) is more consistent with **neurogenic claudication** than vascular claudication.
*Computerized tomography myelography*
- **CT myelography** involves injecting contrast into the spinal canal and then performing a CT scan. While it can visualize the spinal canal, it is more invasive than MRI and exposes the patient to **ionizing radiation**.
- It is typically reserved for cases where MRI is contraindicated (e.g., pacemakers) or when MRI findings are inconclusive.
*Radiography*
- **Radiography (X-rays)** can show bony changes such as **spondylosis** and **degenerative disc disease**, which are often associated with spinal stenosis.
- However, X-rays do not directly visualize the **spinal cord, nerve roots, or soft tissue compression**, making them inadequate for confirming spinal stenosis as the cause of neurogenic claudication.
MRI principles and interpretation US Medical PG Question 4: An investigator studying epigenetic mechanisms isolates histone proteins, the structural motifs involved in DNA binding and regulation of transcription. The peptide bonds of histone proteins are hydrolyzed and one type of amino acid is isolated. At normal body pH, this amino acid has a net charge of +1 . The investigator performs titration of this amino acid and obtains the graph shown. The isolated amino acid is most likely which of the following?
- A. Proline
- B. Lysine (Correct Answer)
- C. Aspartate
- D. Serine
- E. Histidine
MRI principles and interpretation Explanation: ***Lysine***
- Histones are **positively charged** proteins rich in **basic amino acids** like lysine and arginine, which allows them to bind tightly to the negatively charged DNA.
- The titration curve shown with three distinct pKa values and a net charge of +1 at normal body pH (around 7.4) is characteristic of **lysine**, which has both an alpha-amino group (pKa ~9-10) and a basic side chain (pKa ~10.5).
*Proline*
- **Proline is a nonpolar** amino acid that does not contribute significantly to the positive charge of histones required for DNA binding.
- Furthermore, its unique cyclic structure incorporates its amino group into the ring, impacting its pKa relative to other primary amino acids but not making it a primary basic residue in the histone context.
*Aspartate*
- **Aspartate is an acidic amino acid** with a negatively charged side chain at physiological pH, which would repel DNA rather than bind to it.
- Its titration curve would show a net negative charge at normal body pH, not a positive one.
*Serine*
- **Serine is a polar, uncharged** amino acid and would not contribute the necessary positive charge for histone-DNA interaction.
- Its side chain lacks an ionizable group within the physiological pH range, so its titration curve would only show two pKa values (for the carboxyl and amino groups) and a net charge of 0 at neutral pH.
*Histidine*
- While **histidine is a basic amino acid**, its side chain pKa is around 6.0, meaning it is only partially protonated and positively charged at physiological pH.
- A protein rich in **histidine** would not consistently carry a strong positive charge across the typical physiological pH range as effectively as one rich in lysine or arginine.
MRI principles and interpretation US Medical PG Question 5: A 40-year-old man comes to the physician because of weight gain over the past 3 months. During this period, he has gained 10 kg (22 lb) unintentionally. He also reports decreased sexual desire, oily skin, and sleeping difficulties. There is no personal or family history of serious illness. He has smoked one pack of cigarettes daily for the past 10 years. The patient appears lethargic. His temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 150/90 mm Hg. Physical examination shows central obesity, acne, and thin, easily bruisable skin with stretch marks on the abdomen. There is darkening of the mucous membranes and the skin creases. Examination of the muscles shows atrophy and weakness of proximal muscle groups. His serum glucose concentration is 240 mg/dL. Which of the following findings would most likely be present on imaging?
- A. Pituitary microadenoma (Correct Answer)
- B. Decreased thyroid size
- C. Multiple kidney cysts
- D. Kidney tumor
- E. Adrenal carcinoma
MRI principles and interpretation Explanation: ***Pituitary microadenoma***
* The patient's symptoms, including **weight gain, central obesity, oily skin, acne, thin and easily bruisable skin with stretch marks, proximal muscle weakness, hypertension, and hyperglycemia**, are classic for **Cushing's syndrome**.
* A common cause of Cushing's syndrome is **Cushing's disease**, which is caused by an **ACTH-secreting pituitary adenoma** (often a microadenoma).
*Decreased thyroid size*
* **Decreased thyroid size** would be associated with conditions like **atrophic thyroiditis** or **iodine deficiency**, typically leading to **hypothyroidism**.
* **Hypothyroidism** would present with **weight gain** and **fatigue**, but not with **hypertension, hyperglycemia, central obesity, skin bruising, or proximal muscle weakness** as seen in this patient.
*Multiple kidney cysts*
* **Multiple kidney cysts** are characteristic of **polycystic kidney disease**, which can cause **hypertension** and sometimes **renal failure**.
* However, polycystic kidney disease does not typically cause **central obesity, skin changes (bruising, stretch marks, acne), proximal muscle weakness, or hyperglycemia** seen in this patient.
*Kidney tumor*
* A **kidney tumor** (e.g., **renal cell carcinoma**) can cause **hypertension** and **weight loss** but is not associated with the full spectrum of symptoms presented here like **central obesity, skin fragility, stretch marks, muscle atrophy, or hyperglycemia**.
* Some kidney tumors can produce **erythropoietin** leading to **polycythemia**, but not the endocrine features of Cushing's syndrome.
*Adrenal carcinoma*
* While an **adrenal carcinoma** can cause Cushing's syndrome by directly producing **cortisol**, it is typically a **large tumor** visible on imaging and often presents with more rapid and severe symptom onset.
* The presence of **skin darkening (hyperpigmentation)** in this patient, due to increased ACTH stimulation of melanocytes, suggests an **ACTH-dependent Cushing's syndrome**, making a pituitary adenoma more likely than a primary adrenal tumor which would suppress ACTH.
MRI principles and interpretation US Medical PG Question 6: A 60-year-old male is admitted to the ICU for severe hypertension complicated by a headache. The patient has a past medical history of insulin-controlled diabetes, hypertension, and hyperlipidemia. He smokes 2 packs of cigarettes per day. He states that he forgot to take his medications yesterday and started getting a headache about one hour ago. His vitals on admission are the following: blood pressure of 160/110 mmHg, pulse 95/min, temperature 98.6 deg F (37.2 deg C), and respirations 20/min. On exam, the patient has an audible abdominal bruit. After administration of antihypertensive medications, the patient has a blood pressure of 178/120 mmHg. The patient reports his headache has increased to a 10/10 pain level, that he has trouble seeing, and he can't move his extremities. After stabilizing the patient, what is the best next step to diagnose the patient's condition?
- A. Doppler ultrasound of the carotids
- B. CT head with intravenous contrast
- C. MRI head without intravenous contrast
- D. CT head without intravenous contrast (Correct Answer)
- E. MRI head with intravenous contrast
MRI principles and interpretation Explanation: ***CT head without intravenous contrast***
- The sudden onset of severe headache, visual disturbances, and neurological deficits (inability to move extremities), coupled with uncontrolled severe hypertension despite initial treatment, is highly suggestive of an **intracranial pathology**, most likely a **hemorrhagic stroke**.
- A **non-contrast CT scan of the head** is the **gold standard** for rapidly identifying acute intracranial hemorrhage, as it can be performed quickly and is readily available in emergency settings.
*Doppler ultrasound of the carotids*
- This test is primarily used to evaluate **carotid artery stenosis** due to atherosclerosis, which can lead to ischemic stroke.
- While the patient has risk factors for atherosclerosis, his acute presentation with severe central neurological symptoms points more towards an acute intracranial event rather than carotid disease.
*CT head with intravenous contrast*
- While a contrast CT can be useful for identifying tumors, abscesses, or vascular malformations, it is **contraindicated in the initial assessment of acute stroke** if an intracranial hemorrhage is suspected.
- Contrast can sometimes obscure subtle bleeds or complicate the interpretation of acute hemorrhage, and it also carries a risk of **contrast-induced nephropathy**, especially in a patient with diabetes.
*MRI head without intravenous contrast*
- An MRI provides superior soft tissue resolution compared to CT and is excellent for detecting ischemic strokes in later stages, as well as subtle hemorrhages, tumors, and other conditions.
- However, it is **less available, takes longer to perform**, and is often not the first choice in an acute neurological emergency where time is critical, particularly when differentiating between ischemic and hemorrhagic stroke.
*MRI head with intravenous contrast*
- Similar to a contrast CT, an MRI with contrast is generally **not the initial imaging choice for acute stroke** due to time constraints and the need to quickly rule out hemorrhage before considering contrast administration.
- Contrast agents for MRI, such as gadolinium, have their own risks, including **nephrogenic systemic fibrosis** in patients with renal impairment, which is a concern in a diabetic patient.
MRI principles and interpretation US Medical PG Question 7: A new drug X is being tested for its effect on renal function. During the experiments, the researchers found that in patients taking substance X, the urinary concentration of sodium decreases while urine potassium concentration increase. Which of the following affects the kidneys in the same way as does substance X?
- A. Aldosterone (Correct Answer)
- B. Furosemide
- C. Spironolactone
- D. Atrial natriuretic peptide
- E. Hydrochlorothiazide
MRI principles and interpretation Explanation: ***Aldosterone***
- **Aldosterone** acts on the **principal cells** of the **collecting duct** to increase sodium reabsorption and potassium secretion.
- This action leads to a decrease in urinary sodium concentration and an increase in urinary potassium concentration, matching the effects of drug X.
*Furosemide*
- **Furosemide** is a **loop diuretic** that inhibits the **Na-K-2Cl cotransporter** in the **thick ascending limb** of the loop of Henle.
- This inhibition leads to increased excretion of sodium, potassium, and water, resulting in higher urinary sodium concentration.
*Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that blocks aldosterone's effects on the collecting duct.
- This leads to increased sodium excretion and decreased potassium excretion (potassium-sparing effect), which is the opposite of drug X.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** is released in response to atrial stretch and causes **natriuresis** (increased sodium excretion) and **diuresis**.
- It works by dilating afferent arterioles and constricting efferent arterioles, increasing GFR, and inhibiting sodium reabsorption, thus increasing urinary sodium concentration.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** that inhibits the **Na-Cl cotransporter** in the **distal convoluted tubule**.
- This leads to increased sodium and chloride excretion but typically causes potassium wasting (hypokalemia), which differs from the increased urinary potassium concentration seen with drug X.
MRI principles and interpretation US Medical PG Question 8: During the course of investigation of a suspected abdominal aortic aneurysm in a 57-year-old woman, a solid 6 × 5 cm mass is detected in the right kidney. The abdominal aorta reveals no abnormalities. The patient is feeling well and has no history of any serious illness or medication usage. She is a 25-pack-year smoker. Her vital signs are within normal limits. Physical examination reveals no abnormalities. Biopsy of the mass shows renal cell carcinoma. Contrast-enhanced CT scan indicates no abnormalities involving contralateral kidney, lymph nodes, lungs, liver, bone, or brain. Which of the following treatment options is the most appropriate next step in the management of this patient?
- A. Sunitinib
- B. Radiation
- C. Nephrectomy (Correct Answer)
- D. Interferon-ɑ (IFN-ɑ)
- E. Interleukin 2 (IL-2)
MRI principles and interpretation Explanation: ***Nephrectomy***
- The patient has a **localized renal cell carcinoma (RCC)** without evidence of metastasis, as indicated by the CT scan showing no abnormalities in the contralateral kidney, lymph nodes, lungs, liver, bone, or brain.
- **Surgical removal** of the affected kidney (**nephrectomy**) is the **gold standard** and curative treatment for localized RCC.
*Sunitinib*
- **Sunitinib** is a **tyrosine kinase inhibitor** used for advanced or metastatic RCC, not for localized disease.
- It would be considered if the disease had spread beyond the kidney or if surgical resection was not feasible.
*Radiation*
- **Renal cell carcinoma** is generally considered **radioresistant**, making external beam radiation therapy ineffective as a primary treatment.
- Radiation is sometimes used for **palliative care** in metastatic RCC, for example, to relieve bone pain or brain metastases.
*Interferon-ɑ (IFN-ɑ)*
- **Interferon-ɑ** is an **immunotherapy** agent. Its use in RCC has largely been replaced by newer, more effective agents.
- It was historically used for metastatic RCC but is not indicated for localized disease and has significant side effects.
*Interleukin 2 (IL-2)*
- **High-dose interleukin 2 (IL-2)** is another **immunotherapy** agent effective in a subset of patients with metastatic RCC.
- It is not used for localized RCC and carries a risk of serious toxicity, requiring administration in specialized centers.
MRI principles and interpretation US Medical PG Question 9: A 67-year-old man presents to his primary care provider with bloody urine. He first noticed the blood 1 week ago. He otherwise feels healthy. His past medical history is significant for type 2 diabetes mellitus for 18 years, for which he takes insulin injections. He has smoked 30–40 cigarettes per day for the past 29 years and drinks alcohol socially. Today his vital signs include: temperature 36.6°C (97.8°F), blood pressure 135/82 mm Hg, and heart rate 105/min. There are no findings on physical examination. Urinalysis shows 15–20 red cells/high power field. Which of the following is the next best test to evaluate this patient’s condition?
- A. Prostate-specific antigen
- B. Urine cytology
- C. Urinary markers
- D. Biopsy
- E. Contrast-enhanced CT (Correct Answer)
MRI principles and interpretation Explanation: ***Contrast-enhanced CT***
- This patient presents with **painless gross hematuria** and significant risk factors, including a 29-year history of **heavy smoking** and age, which raise suspicion for **urothelial carcinoma** (e.g., bladder cancer, renal cell carcinoma).
- A **contrast-enhanced CT** of the abdomen and pelvis is the most appropriate initial imaging study to evaluate the entire urinary tract for masses, stones, or other structural abnormalities causing the hematuria.
*Prostate-specific antigen*
- This test is primarily used for **prostate cancer screening** and monitoring, and while prostate issues can cause hematuria, the absence of urinary obstruction symptoms and the patient's age and smoking history make other causes more likely.
- An elevated **PSA** would not explain gross, painless hematuria in this context and would not be the initial diagnostic step for evaluating the urinary tract in general.
*Urine cytology*
- While urine cytology can detect **malignant cells**, its sensitivity for urothelial carcinoma is variable and often low, especially for low-grade tumors.
- A negative cytology does not rule out cancer, and an imaging study is still necessary to **localize the source** of bleeding and assess for structural abnormalities.
*Urinary markers*
- Various **urinary markers** (e.g., BTA stat, NMP22) are available for bladder cancer detection, but they are generally less sensitive and specific than imaging or cystoscopy.
- These markers are often used in conjunction with other tests or for surveillance, but not as the initial definitive test for **gross hematuria** in a high-risk patient.
*Biopsy*
- A biopsy is a **definitive diagnostic step** for confirming cancer but requires an identified lesion to target.
- Before a biopsy can be performed, imaging (like CT) is needed to **locate any potential tumors** in the kidneys, ureters, or bladder that would then be amenable to biopsy (e.g., via cystoscopy with biopsy or renal biopsy).
MRI principles and interpretation US Medical PG Question 10: A 65-year-old man presents to the emergency department for sudden weakness. He was doing mechanical work on his car where he acutely developed right-leg weakness and fell to the ground. He is accompanied by his wife, who said that this has never happened before. He was last seen neurologically normal approximately 2 hours prior to presentation. His past medical history is significant for hypertension and type II diabetes. His temperature is 98.8°F (37.1°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. Neurological exam reveals that he is having trouble speaking and has profound weakness of his right upper and lower extremity. Which of the following is the best next step in management?
- A. Thrombolytics
- B. Noncontrast head CT (Correct Answer)
- C. CT angiogram
- D. MRI of the head
- E. Aspirin
MRI principles and interpretation Explanation: ***Noncontrast head CT***
- A **noncontrast head CT** is the most crucial initial step in managing acute stroke symptoms because it can rapidly rule out an **intracranial hemorrhage**.
- Distinguishing between ischemic stroke and hemorrhagic stroke is critical, as the management strategies are vastly different and administering thrombolytics in the presence of hemorrhage can be fatal.
*Thrombolytics*
- **Thrombolytics** can only be administered after an **intracranial hemorrhage** has been excluded via noncontrast head CT.
- Administering thrombolytics without imaging could worsen a hemorrhagic stroke, causing significant harm or death.
*CT angiogram*
- A **CT angiogram** is used to identify large vessel occlusions in ischemic stroke and is typically performed after a noncontrast CT rules out hemorrhage.
- This imaging is crucial for determining eligibility for **endovascular thrombectomy** but is not the very first diagnostic step.
*MRI of the head*
- An **MRI of the head** is more sensitive for detecting acute ischemic changes but takes longer to perform and is often not readily available in the acute emergency setting.
- It is not the initial imaging of choice for ruling out hemorrhage due to its longer acquisition time compared to CT.
*Aspirin*
- **Aspirin** is indicated for acute ischemic stroke but should only be given after an **intracranial hemorrhage** has been ruled out.
- Like thrombolytics, aspirin could exacerbate a hemorrhagic stroke and is thus deferred until initial imaging is complete.
More MRI principles and interpretation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.