Interventional radiology procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Interventional radiology procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Interventional radiology procedures US Medical PG Question 1: A 62-year-old man comes to the emergency department for severe, acute right leg pain. The patient's symptoms began suddenly 4 hours ago, while he was reading the newspaper. He has poorly-controlled hypertension and osteoarthritis. He has smoked one pack of cigarettes daily for 31 years. Current medications include lisinopril, metoprolol succinate, and ibuprofen. He appears to be in severe pain and is clutching his right leg. His temperature is 37.4°C (99.3°F), pulse is 102/min and irregularly irregular, respirations are 19/min, and blood pressure is 152/94 mm Hg. The right leg is cool to the touch, with decreased femoral, popliteal, posterior tibial, and dorsalis pedis pulses. There is moderate weakness and decreased sensation in the right leg. An ECG shows absent P waves and a variable R-R interval. Right leg Doppler study shows inaudible arterial signal and audible venous signal. Angiography shows 90% occlusion of the right common femoral artery. In addition to initiating heparin therapy, which of the following is the most appropriate next step in management?
- A. Surgical bypass of the affected vessel
- B. Percutaneous transluminal angioplasty
- C. Amputation of the affected limb
- D. Open embolectomy
- E. Balloon catheter embolectomy (Correct Answer)
Interventional radiology procedures Explanation: **Balloon catheter embolectomy**
- The patient presents with **acute limb ischemia** characterized by sudden onset of severe pain, cool extremity, absent pulses, motor weakness, and sensory deficits. The **irregularly irregular pulse** and **absent P waves on ECG** are highly suggestive of **atrial fibrillation**, a common source of arterial emboli.
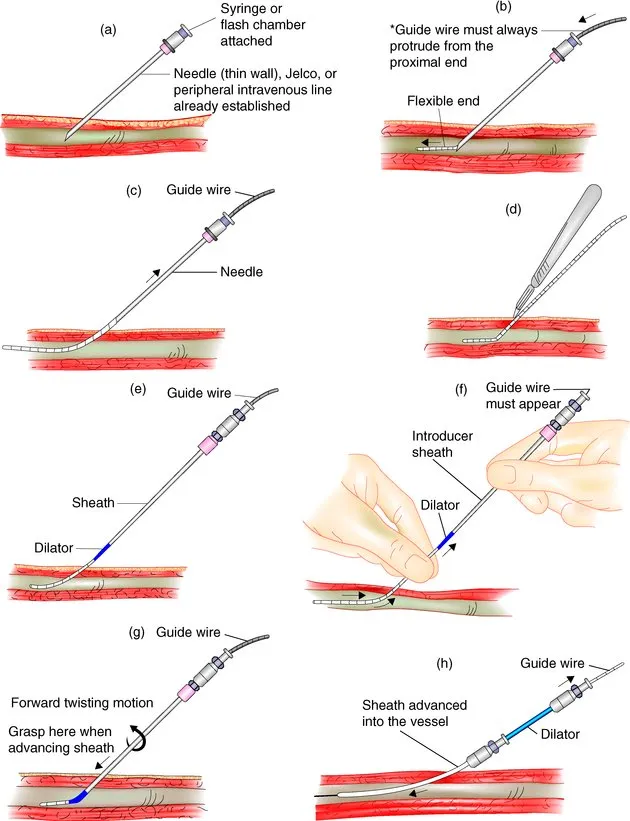
- Given the acute nature, the presence of a probable embolic source, and the Doppler findings of an **inaudible arterial signal**, **balloon catheter embolectomy** (e.g., using a Fogarty catheter) is the most appropriate and rapid intervention to restore blood flow and salvage the limb. This procedure directly retrieves the embolus.
*Surgical bypass of the affected vessel*
- **Surgical bypass** is typically indicated for **chronic limb ischemia** or extensive, complex occlusions that are not amenable to less invasive techniques.
- It is a more extensive procedure with a longer recovery time and is not the first-line treatment for acute embolic occlusion.
*Percutaneous transluminal angioplasty*
- **Percutaneous transluminal angioplasty** (PTA) is generally used for **atherosclerotic stenoses** or occlusions rather than acute arterial emboli.
- While it can be performed in some cases of acute limb ischemia, it is less effective than embolectomy for removing a fresh, mobile clot, especially in large vessels.
*Amputation of the affected limb*
- **Amputation** is considered only when the limb is **irreversibly ischemic** and non-viable, or when revascularization attempts have failed.
- In this case, the patient has moderate weakness and decreased sensation, indicating that the limb is still viable and potentially salvageable.
*Open embolectomy*
- **Open embolectomy** is a surgical procedure to remove an embolus, similar in goal to balloon catheter embolectomy but often performed with a larger incision.
- While effective, **balloon catheter embolectomy** is generally preferred due to its less invasive nature and ability to be performed rapidly, especially in emergent situations.
Interventional radiology procedures US Medical PG Question 2: A 57-year-old man is brought to the emergency department by his family because of several episodes of vomiting of blood in the past 24 hours. He has a history of alcoholic cirrhosis and is being treated for ascites with diuretics and for encephalopathy with lactulose. His vital signs include a temperature of 36.9°C (98.4°F), pulse of 85/min, and blood pressure of 80/52 mm Hg. On examination, he is confused and unable to give a complete history. He is noted to have jaundice, splenomegaly, and multiple spider angiomas over his chest. Which of the following is the best initial management of this patient?
- A. Endoscopic surveillance
- B. Non-selective beta-blockers
- C. Combined vasoactive and endoscopic therapy (Correct Answer)
- D. Balloon tamponade
- E. Transjugular intrahepatic portosystemic shunt (TIPS)
Interventional radiology procedures Explanation: ***Combined vasoactive and endoscopic therapy***
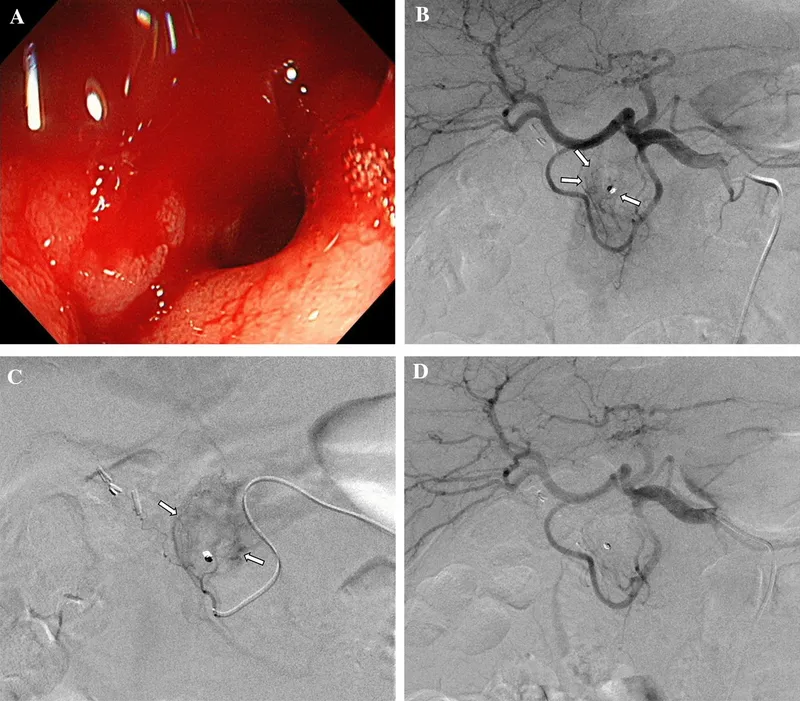
- The patient presents with **hematemesis**, **hypotension**, and signs of decompensated **alcoholic cirrhosis** (jaundice, splenomegaly, spider angiomas). This clinical picture is highly suggestive of **esophageal variceal bleeding**, a life-threatening emergency.
- **Combined vasoactive drug therapy** (e.g., octreotide to reduce splanchnic blood flow) and **endoscopic therapy** (e.g., variceal ligation or sclerotherapy) are the recommended initial management for **active variceal bleeding** to control hemorrhage and prevent rebleeding.
*Endoscopic surveillance*
- **Endoscopic surveillance** is performed for patients with known varices who are **not actively bleeding** to identify varices at high risk of rupture and to initiate primary prophylaxis.
- This patient is actively bleeding, making surveillance an inappropriate initial step.
*Non-selective beta-blockers*
- **Non-selective beta-blockers** (e.g., propranolol, carvedilol) are used for **primary and secondary prophylaxis** of variceal bleeding by reducing portal pressure.
- They are **not appropriate for acute bleeding management**, as their onset of action is too slow to control active hemorrhage.
*Balloon tamponade*
- **Balloon tamponade** (e.g., with a Sengstaken-Blakemore tube) is a **temporary measure** used to control massive, refractory variceal bleeding when endoscopic therapy is unsuccessful or immediately unavailable.
- It is a **bridge to definitive management** and carries significant risks, such as **esophageal rupture** or **aspiration**, so it is not the first-line initial treatment.
*Transjugular intrahepatic portosystemic shunt (TIPS)*
- **TIPS** is typically reserved for patients with **refractory variceal bleeding** that cannot be controlled by endoscopic and pharmacologic therapy, or for those with **recurrent bleeding despite optimal secondary prophylaxis**.
- It is an **invasive procedure** and not the immediate initial intervention for acute variceal hemorrhage.
Interventional radiology procedures US Medical PG Question 3: A researcher is trying to determine whether a newly discovered substance X can be useful in promoting wound healing after surgery. She conducts this study by enrolling the next 100 patients that will be undergoing this surgery and separating them into 2 groups. She decides which patient will be in which group by using a random number generator. Subsequently, she prepares 1 set of syringes with the novel substance X and 1 set of syringes with a saline control. Both of these sets of syringes are unlabeled and the substances inside cannot be distinguished. She gives the surgeon performing the surgery 1 of the syringes and does not inform him nor the patient which syringe was used. After the study is complete, she analyzes all the data that was collected and performs statistical analysis. This study most likely provides which level of evidence for use of substance X?
- A. Level 3
- B. Level 1 (Correct Answer)
- C. Level 4
- D. Level 5
- E. Level 2
Interventional radiology procedures Explanation: ***Level 1***
- The study design described is a **randomized controlled trial (RCT)**, which is considered the **highest level of evidence (Level 1)** in the hierarchy of medical evidence.
- Key features like **randomization**, **control group**, and **blinding (double-blind)** help minimize bias and strengthen the validity of the findings.
*Level 2*
- Level 2 evidence typically comprises **well-designed controlled trials without randomization** (non-randomized controlled trials) or **high-quality cohort studies**.
- While strong, they do not possess the same level of internal validity as randomized controlled trials.
*Level 3*
- Level 3 evidence typically includes **case-control studies** or **cohort studies**, which are observational designs and carry a higher risk of bias compared to RCTs.
- These studies generally do not involve randomization or intervention assignment by the researchers.
*Level 4*
- Level 4 evidence is usually derived from **case series** or **poor quality cohort and case-control studies**.
- These studies provide descriptive information or investigate associations without strong control for confounding factors.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, consisting of **expert opinion** or **animal research/bench research**.
- This level lacks human clinical data or systematic investigative rigor needed for higher evidence levels.
Interventional radiology procedures US Medical PG Question 4: A 62-year-old man comes to the physician because of a 5-day history of swelling in his left arm. Two months ago, he was diagnosed with a deep venous thrombosis in the left calf. He has had a 7-kg (15-lb) weight loss in the last 3 months. He has smoked 1 pack of cigarettes daily for the past 25 years. His only medication is warfarin. Physical examination shows warm edema of the left forearm with overlying erythema and a tender, palpable cord-like structure along the medial arm. His lungs are clear to auscultation bilaterally. Duplex sonography shows thrombosis of the left basilic and external jugular veins. Which of the following is the most appropriate next step to confirm the underlying diagnosis?
- A. CT scan of the chest
- B. X-ray of the chest (Correct Answer)
- C. Transesophageal echocardiography
- D. Serum antiphospholipid antibody level
- E. Serum D-dimer level
Interventional radiology procedures Explanation: **X-ray of the chest**
- The patient presents with **recurrent deep venous thrombosis (DVT)**, specifically in an unusual location (upper extremity), combined with **unexplained weight loss** and a **significant smoking history**. These are strong indicators of an underlying malignancy.
- A **chest x-ray** is a readily available and cost-effective initial screening tool to evaluate for **lung cancer**, which is common in smokers and can present with paraneoplastic phenomena like hypercoagulability (Trousseau phenomenon) leading to DVT.
*CT scan of the chest*
- While a **CT scan of the chest** is more sensitive than an X-ray for detecting lung masses, an **X-ray is the more appropriate initial step** for screening given the clinical context.
- A **CT scan** would typically be performed after an abnormal chest X-ray or if clinical suspicion remains high despite a normal X-ray.
*Transesophageal echocardiography*
- **Transesophageal echocardiography (TEE)** is primarily used to evaluate **cardiac structures**, valve function, and to detect intracardiac thrombi or vegetations.
- It is not indicated as a primary screening tool for an underlying malignancy or in the workup of a **venous thrombosis** not directly related to cardiac pathology.
*Serum antiphospholipid antibody level*
- **Antiphospholipid antibody syndrome** is a cause of recurrent thrombosis, but the patient's other symptoms (weight loss, smoking history, unusual DVT location) point more strongly towards an underlying malignancy.
- While it might be considered in a broader workup for hypercoagulability, it is not the most immediate next step given the constellation of findings strongly suggestive of cancer.
*Serum D-dimer level*
- A **serum D-dimer level** is a marker of fibrin degradation and is useful for **excluding DVT/PE** in low-probability patients.
- In this patient, a DVT has already been diagnosed by duplex sonography, so a D-dimer level would not provide additional diagnostic information regarding the presence of thrombosis, nor would it help in identifying the underlying cause of the recurrent thrombosis.
Interventional radiology procedures US Medical PG Question 5: A 29-year-old woman, gravida 1, para 1, comes to the physician for the evaluation of a painful mass in her left breast for several days. She has no fevers or chills. She has not noticed any changes in the right breast. She has no history of serious illness. Her last menstrual period was 3 weeks ago. She appears anxious. Her temperature is 37°C (98.6°F), pulse is 80/min, respirations are 13/min, and blood pressure is 130/75 mm Hg. Examination shows a palpable, mobile, tender mass in the left upper quadrant of the breast. Ultrasound shows a 1.75-cm, well-circumscribed anechoic mass with posterior acoustic enhancement. The patient says that she is very concerned that she may have breast cancer and wishes further diagnostic testing. Which of the following is the most appropriate next step in the management of this patient?
- A. Core needle biopsy
- B. MRI scan of the left breast
- C. Reassurance and clinical follow-up
- D. Fine needle aspiration (Correct Answer)
- E. Mammogram
Interventional radiology procedures Explanation: ***Fine needle aspiration***
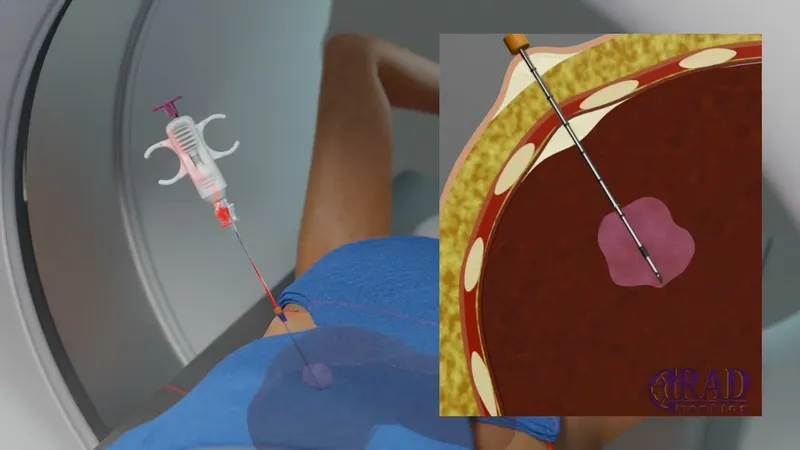
- This patient presents with a **palpable, mobile, tender mass** in the breast, and ultrasound reveals a **well-circumscribed anechoic mass with posterior acoustic enhancement**, which is highly suggestive of a **simple cyst**.
- **Fine needle aspiration** is the most appropriate next step for a symptomatic simple cyst; it can be both diagnostic and therapeutic, relieving patient anxiety and pain.
*Core needle biopsy*
- **Core needle biopsy** is typically reserved for lesions that are suspicious for malignancy, such as solid masses with **irregular margins** or **architectural distortion**, which are not present in this case.
- Performing a core needle biopsy on a likely simple cyst is excessively invasive and carries risks like bleeding and infection without clear indication.
*MRI scan of the left breast*
- An **MRI scan** is generally used for screening high-risk patients, evaluating the extent of known cancer, or further characterizing complex lesions not clearly defined by mammography and ultrasound.
- It is not indicated for a lesion that is highly characteristic of a **simple cyst** on ultrasound, as it would be an unnecessary and costly procedure.
*Reassurance and clinical follow-up*
- While the ultrasound findings are reassuring, her symptoms (painful mass) and anxiety warrant intervention. **Reassurance alone** is insufficient, as aspiration would confirm the diagnosis and relieve symptoms.
- Dismissing the patient's concerns without further action, especially with a symptomatic mass, is not the best practice and may cause undue stress.
*Mammogram*
- A **mammogram** would be less helpful in this young woman with dense breast tissue, and ultrasound has already characterized the lesion as a cyst.
- Furthermore, for a clearly cystic lesion, mammography provides little additional diagnostic information and exposes the patient to unnecessary radiation.
Interventional radiology procedures US Medical PG Question 6: A 27-year-old man is witnessed falling off his bicycle. The patient rode his bicycle into a curb and hit his face against a rail. The patient did not lose consciousness and is ambulatory at the scene. There is blood in the patient's mouth and one of the patient's teeth is found on the sidewalk. The patient is transferred to the local emergency department. Which of the following is the best method to transport this patient's tooth?
- A. Wrapped in gauze soaked in normal saline
- B. Submerged in normal saline
- C. Submerged in milk (Correct Answer)
- D. Wrapped in sterile gauze
- E. Submerged in water
Interventional radiology procedures Explanation: ***Submerged in milk***
- **Milk** is the ideal solution for transporting an avulsed tooth because it has a pH and osmolality that is compatible with the **vitality of the periodontal ligament (PDL) cells**.
- Its nutrient content also helps to sustain these cells, increasing the likelihood of successful **replantation**.
*Wrapped in gauze soaked in normal saline*
- While **normal saline** can keep the tooth moist, its osmolality is not optimal for maintaining the **viability of PDL cells** for an extended period.
- Wrapping in gauze may also cause the tooth to dry out if not kept adequately saturated, which can damage the **periodontal ligament**.
*Submerged in normal saline*
- Submerging in **normal saline** is better than dry storage but is still **suboptimal** compared to milk.
- The tonicity and pH of normal saline are not as beneficial for the **long-term survival of PDL cells** as milk.
*Wrapped in sterile gauze*
- **Sterile gauze** alone does not provide moisture or nutrients, leading to **rapid desiccation and death of PDL cells**.
- A dry environment dramatically reduces the chances of successful **replantation** and increases the risk of **ankylosis** or **resorption**.
*Submerged in water*
- **Water** is a **hypotonic solution** that can cause **lysis of PDL cells** due to osmotic pressure differences.
- This significantly compromises the tooth's viability and success of **replantation**.
Interventional radiology procedures US Medical PG Question 7: During the course of investigation of a suspected abdominal aortic aneurysm in a 57-year-old woman, a solid 6 × 5 cm mass is detected in the right kidney. The abdominal aorta reveals no abnormalities. The patient is feeling well and has no history of any serious illness or medication usage. She is a 25-pack-year smoker. Her vital signs are within normal limits. Physical examination reveals no abnormalities. Biopsy of the mass shows renal cell carcinoma. Contrast-enhanced CT scan indicates no abnormalities involving contralateral kidney, lymph nodes, lungs, liver, bone, or brain. Which of the following treatment options is the most appropriate next step in the management of this patient?
- A. Sunitinib
- B. Radiation
- C. Nephrectomy (Correct Answer)
- D. Interferon-ɑ (IFN-ɑ)
- E. Interleukin 2 (IL-2)
Interventional radiology procedures Explanation: ***Nephrectomy***
- The patient has a **localized renal cell carcinoma (RCC)** without evidence of metastasis, as indicated by the CT scan showing no abnormalities in the contralateral kidney, lymph nodes, lungs, liver, bone, or brain.
- **Surgical removal** of the affected kidney (**nephrectomy**) is the **gold standard** and curative treatment for localized RCC.
*Sunitinib*
- **Sunitinib** is a **tyrosine kinase inhibitor** used for advanced or metastatic RCC, not for localized disease.
- It would be considered if the disease had spread beyond the kidney or if surgical resection was not feasible.
*Radiation*
- **Renal cell carcinoma** is generally considered **radioresistant**, making external beam radiation therapy ineffective as a primary treatment.
- Radiation is sometimes used for **palliative care** in metastatic RCC, for example, to relieve bone pain or brain metastases.
*Interferon-ɑ (IFN-ɑ)*
- **Interferon-ɑ** is an **immunotherapy** agent. Its use in RCC has largely been replaced by newer, more effective agents.
- It was historically used for metastatic RCC but is not indicated for localized disease and has significant side effects.
*Interleukin 2 (IL-2)*
- **High-dose interleukin 2 (IL-2)** is another **immunotherapy** agent effective in a subset of patients with metastatic RCC.
- It is not used for localized RCC and carries a risk of serious toxicity, requiring administration in specialized centers.
Interventional radiology procedures US Medical PG Question 8: A 58-year-old man presents to the Emergency Department after 3 hours of intense suprapubic pain associated with inability to urinate for the past day or two. His medical history is relevant for benign prostatic hyperplasia (BPH) that has been under treatment with prazosin and tadalafil. Upon admission, he is found to have a blood pressure of 180/100 mm Hg, a pulse of 80/min, a respiratory rate of 23/min, and a temperature of 36.5°C (97.7°F). He weighs 84 kg (185.1 lb) and is 175 cm (5 ft 7 in) tall. Physical exam, he has suprapubic tenderness. A bladder scan reveals 700 ml of urine. A Foley catheter is inserted and the urine is drained. Initial laboratory tests and their follow up 8 hours after admission are shown below.
Admission 8 hours after admission
Serum potassium 4.2 mmol/L Serum potassium 4.0 mmol/L
Serum sodium 140 mmol/L Serum sodium 142 mmol/L
Serum chloride 102 mmol/L Serum chloride 110 mmol/L
Serum creatinine 1.4 mg/dL Serum creatinine 1.6 mg/dL
Serum blood urea nitrogen 64 mg/dL Serum blood urea nitrogen 62 mg/dL
Urine output 250 mL Urine output 260 mL
A senior attending suggests a consultation with Nephrology. Which of the following best justifies this suggestion?
- A. Estimated glomerular filtration rate (eGFR)
- B. Urine output (Correct Answer)
- C. Serum creatinine (SCr)
- D. Serum blood urea nitrogen (BUN)
- E. Serum potassium
Interventional radiology procedures Explanation: ***Urine output***
- The patient's **urine output is severely reduced** at 260 mL over 8 hours (approximately **32.5 mL/hour**), which constitutes **oliguria** (defined as <0.5 mL/kg/hr; this patient at 84 kg should produce ≥42 mL/hr).
- Despite **relief of the post-renal obstruction** via Foley catheterization, the persistent oliguria indicates **intrinsic kidney injury** rather than simple mechanical obstruction.
- The combination of **oliguria persisting after decompression** + **rising serum creatinine** (1.4→1.6 mg/dL) meets **KDIGO criteria for Stage 2 AKI** (urine output <0.5 mL/kg/hr for ≥12 hours).
- This requires **urgent nephrology consultation** to assess for acute tubular necrosis (ATN), guide fluid management during potential post-obstructive diuresis, and consider renal replacement therapy if oliguria worsens.
*Serum creatinine (SCr)*
- The serum creatinine **rose from 1.4 to 1.6 mg/dL** despite bladder decompression, which is concerning and suggests intrinsic renal injury.
- However, creatinine is a **lagging indicator** of kidney function - it takes 24-48 hours to reflect acute changes in GFR, whereas **urine output is a real-time indicator** of kidney function.
- While the rising creatinine supports the need for nephrology involvement, **urine output is the more immediate and actionable parameter** that prompted the attending's suggestion at this early time point.
*Estimated glomerular filtration rate (eGFR)*
- eGFR is **calculated from serum creatinine** using equations that assume steady-state conditions, which **do not apply in acute kidney injury**.
- In the **acute setting with rapidly changing kidney function**, eGFR calculations are unreliable and can significantly overestimate or underestimate true GFR.
- Clinicians rely more on **urine output and serial creatinine measurements** rather than eGFR when managing AKI.
*Serum blood urea nitrogen (BUN)*
- The BUN decreased slightly from 64 to 62 mg/dL, remaining elevated but showing minimal change after catheterization.
- Elevated BUN can reflect **pre-renal azotemia, dehydration, or upper GI bleeding** and is less specific for intrinsic kidney injury than oliguria.
- The **BUN:Cr ratio** is approximately 40:1 (64/1.6), suggesting a **pre-renal component**, but this alone doesn't justify urgent nephrology consultation as strongly as the persistent oliguria does.
*Serum potassium*
- Serum potassium levels remain **normal** (4.2→4.0 mmol/L) and do not indicate a metabolic emergency.
- While **hyperkalemia** is a common complication of AKI that would warrant nephrology involvement, this patient's potassium is well-controlled and not the driving concern at this time.
Interventional radiology procedures US Medical PG Question 9: A CT scan of the abdomen reveals a mass in the pancreatic uncinate process. Which of the following structures is most likely to be compressed by this mass?
- A. Common bile duct
- B. Portal vein
- C. Splenic vein
- D. Superior mesenteric vein (Correct Answer)
Interventional radiology procedures Explanation: ***Superior mesenteric vein***
- The **uncinate process** of the pancreas hooks around the **superior mesenteric vessels**. Therefore, a mass in this region would most directly compress the **superior mesenteric vein (SMV)** and artery (SMA).
- Compression of the SMV can lead to **venous outflow obstruction** from the small intestine, potentially causing **bowel ischemia** or edema.
*Common bile duct*
- The **common bile duct** passes through the **head of the pancreas**, not typically the uncinate process.
- Compression of the common bile duct would more commonly be associated with masses in the **head of the pancreas**, leading to **jaundice**.
*Portal vein*
- The **portal vein** is formed by the union of the **splenic vein** and the **superior mesenteric vein**, generally posterior to the neck of the pancreas.
- While pancreatic masses can affect the portal vein, a mass specifically in the uncinate process would more directly impinge on the SMV before significantly affecting the main portal vein, which is superior and posterior to the uncinate process.
*Splenic vein*
- The **splenic vein** runs along the **posterior aspect of the body and tail of the pancreas**.
- A mass in the uncinate process, located at the inferior margin of the head, is relatively distant from the splenic vein.
Interventional radiology procedures US Medical PG Question 10: A 48-year-old woman is brought to the emergency department because of a 1-hour history of sudden-onset headache associated with nausea and vomiting. The patient reports she was sitting at her desk when the headache began. The headache is global and radiates to her neck. She has hypertension. She has smoked one pack of cigarettes daily for the last 10 years. She drinks alcohol occasionally. Her father had a stroke at the age 58 years. Current medications include hydrochlorothiazide. She is in severe distress. She is alert and oriented to person, place, and time. Her temperature is 38.2°C (100.8°F), pulse is 89/min, respirations are 19/min, and blood pressure is 150/90 mm Hg. Cardiopulmonary examination shows no abnormalities. Cranial nerves II–XII are intact. She has no focal motor or sensory deficits. She flexes her hips and knees when her neck is flexed while lying in a supine position. A CT scan of the head is shown. Which of the following is the most appropriate intervention?
- A. Perform burr hole surgery
- B. Administer intravenous alteplase
- C. Administer intravenous vancomycin and ceftriaxone
- D. Perform surgical clipping (Correct Answer)
- E. Perform decompressive craniectomy
Interventional radiology procedures Explanation: ***Perform surgical clipping***
- The clinical presentation of **sudden-onset severe headache** ("thunderclap headache"), **nausea, vomiting, neck stiffness (positive Brudzinski's sign)**, and the CT scan showing **blood in the subarachnoid space** strongly indicate a **subarachnoid hemorrhage (SAH)** from a ruptured cerebral aneurysm.
- Definitive treatment requires **securing the aneurysm** to prevent **rebleeding**, which carries 40-50% mortality. Modern management includes **endovascular coiling** (first-line for most cases) or **surgical clipping**.
- **Surgical clipping** involves placing a metal clip across the aneurysm neck to exclude it from circulation. It remains the preferred approach for certain aneurysm locations (MCA), wide-necked aneurysms, or when accompanied by hematoma requiring evacuation.
- Among the options provided, surgical clipping is the only definitive intervention that secures the ruptured aneurysm.
*Perform burr hole surgery*
- **Burr hole surgery** is used for draining **subdural hematomas** or accessing the brain for procedures like biopsy or external ventricular drain placement.
- While burr holes may be needed for complications of SAH (e.g., hydrocephalus requiring EVD), this is not the primary intervention for securing the ruptured aneurysm itself.
*Administer intravenous alteplase*
- **Alteplase** (tPA) is a **thrombolytic agent** used for **acute ischemic stroke** within 4.5 hours of symptom onset.
- Administering thrombolytics in **hemorrhagic stroke** (like SAH) is **absolutely contraindicated** as it would worsen bleeding and cause catastrophic neurological deterioration or death.
*Administer intravenous vancomycin and ceftriaxone*
- **Vancomycin and ceftriaxone** treat **bacterial meningitis**, which can present with headache, fever, and meningeal signs.
- Although the patient has low-grade fever (likely from blood irritating meninges, not infection) and neck stiffness, the **sudden-onset thunderclap headache** and **CT findings of SAH** make ruptured aneurysm the diagnosis, not meningitis. The fever in SAH is typically from aseptic meningeal irritation.
*Perform decompressive craniectomy*
- **Decompressive craniectomy** removes skull bone to relieve **elevated intracranial pressure** from massive brain swelling (severe TBI, malignant MCA infarction).
- While SAH can cause elevated ICP, craniectomy does not secure the aneurysm. The immediate priority is preventing **rebleeding** by securing the aneurysm source, not managing secondary complications.
More Interventional radiology procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.