Emergency imaging protocols US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Emergency imaging protocols. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Emergency imaging protocols US Medical PG Question 1: A 68-year-old woman is brought to the emergency department with intense abdominal pain for the past 2 hours. She has had 1 episode of bloody diarrhea recently. She has an 18-year history of diabetes mellitus. She was diagnosed with hypertension and ischemic heart disease 6 years ago. She is fully alert and oriented. Her temperature is 37.5°C (99.5°F), blood pressure is 145/90 mm Hg, pulse is 78/min, and respirations are 14/min. Abdominal examination shows mild generalized abdominal tenderness without guarding or rebound tenderness. An abdominal plain X-ray shows no abnormalities. Abdominal CT reveals colonic wall thickening and pericolonic fat stranding in the splenic curvature. Bowel rest, intravenous hydration, and IV antibiotics are initiated. Which of the following is the most important diagnostic evaluation at this time?
- A. Angiography
- B. Gastrografin-enhanced X-ray
- C. Laparotomy
- D. Inpatient observation
- E. Sigmoidoscopy (Correct Answer)
Emergency imaging protocols Explanation: ***Sigmoidoscopy***
- The patient's presentation with acute abdominal pain, bloody diarrhea, history of cardiovascular disease, and CT findings consistent with **colonic wall thickening** and **pericolonic fat stranding** strongly suggests **ischemic colitis**.
- **Flexible sigmoidoscopy** allows for direct visualization of the colonic mucosa to confirm the diagnosis, assess the extent and severity of ischemia, and rule out other causes of colitis, such as inflammatory bowel disease or infection.
*Angiography*
- While angiography can identify mesenteric arterial occlusion, it is generally reserved for cases of acute mesenteric ischemia involving the superior mesenteric artery, which typically presents with more severe pain out of proportion to physical exam findings and less clear CT findings of colitis.
- In cases of ischemic colitis, where the primary concern is mucosal ischemia rather than immediate large vessel occlusion, angiography is usually not the first-line diagnostic.
*Gastrografin-enhanced X-ray*
- This study (also known as a **Gastrografin swallow or enema**) is primarily used to evaluate for **perforations** or **obstructions**, or to assess lumen integrity.
- It does not provide the mucosal detail necessary to diagnose or assess the severity of **ischemic colitis**, and the contrast agent itself could potentially exacerbate an inflamed bowel.
*Laparotomy*
- **Laparotomy** (surgical exploration) is an invasive procedure reserved for cases with signs of peritonitis, bowel perforation, or severe, unresponsive ischemia requiring surgical intervention.
- Given the patient's stable vital signs, mild tenderness, and lack of guarding or rebound, immediate surgical exploration is not warranted without further diagnostic steps.
*Inpatient observation*
- While inpatient observation is part of the initial management (bowel rest, IV fluids, antibiotics), it is not a **diagnostic evaluation** itself.
- The question asks for the most important diagnostic evaluation to determine the underlying cause and guide further management.
Emergency imaging protocols US Medical PG Question 2: A 78-year-old man is brought in to the emergency department by ambulance after his wife noticed that he began slurring his speech and had developed facial asymmetry during dinner approximately 30 minutes ago. His past medical history is remarkable for hypertension and diabetes. His temperature is 99.1°F (37.3°C), blood pressure is 154/99 mmHg, pulse is 89/min, respirations are 12/min, and oxygen saturation is 98% on room air. Neurologic exam reveals right upper and lower extremity weakness and an asymmetric smile. Which of the following is the next best step in management?
- A. Alteplase
- B. MRI brain
- C. CT head (Correct Answer)
- D. Aspirin
- E. CTA head
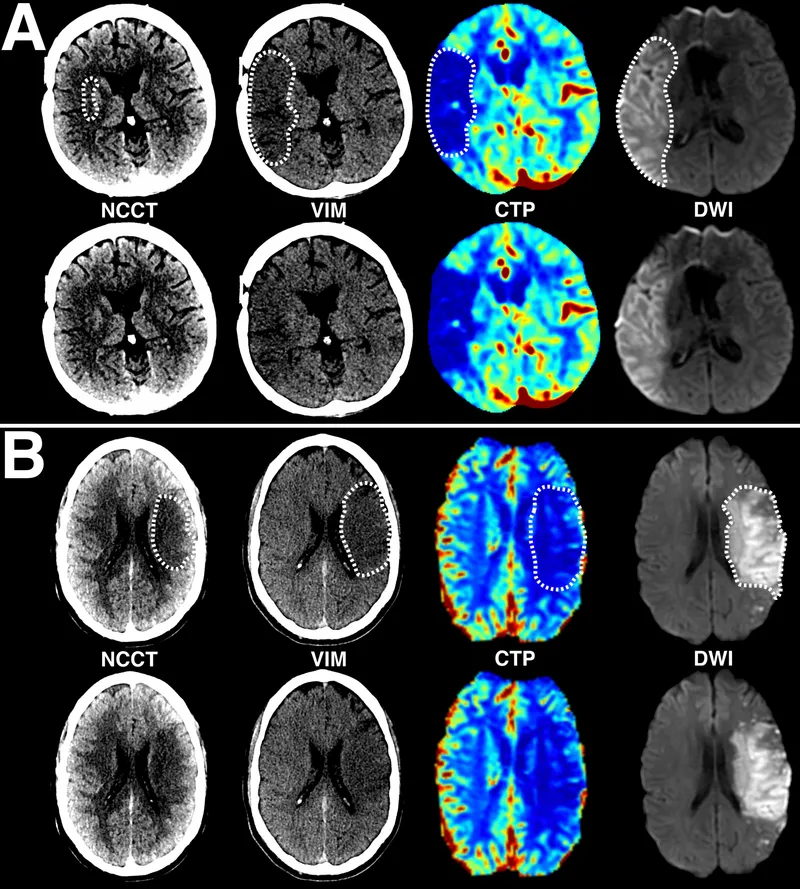
Emergency imaging protocols Explanation: ***CT head***
- A **non-contrast CT head** is the immediate priority to differentiate between ischemic and hemorrhagic stroke, which is critical for guiding subsequent treatment decisions.
- Given the patient's acute neurological deficits (slurred speech, facial asymmetry, weakness) and vascular risk factors (hypertension, diabetes), **stroke is highly suspected**, and identifying intracerebral hemorrhage is crucial before considering thrombolytic therapy.
*Alteplase*
- **Alteplase** (tPA) is a thrombolytic agent used for acute ischemic stroke, but its administration is **contraindicated in hemorrhagic stroke**.
- Initiating alteplase without first ruling out hemorrhage with a CT scan could lead to catastrophic bleeding.
*MRI brain*
- While an **MRI brain** can provide more detailed imaging of stroke, it is typically **not the initial imaging modality** in the emergency setting due to longer acquisition times and limited availability, especially when emergent differentiation between ischemic and hemorrhagic stroke is needed.
- Its use is usually reserved for cases where the CT is inconclusive or for later evaluation.
*Aspirin*
- **Aspirin** is an antiplatelet agent used in the management of ischemic stroke, but it should **not be given until a hemorrhagic stroke has been ruled out** via CT head.
- Administering aspirin in the context of an intracerebral hemorrhage could worsen bleeding.
*CTA head*
- A **CT angiography (CTA) head** is used to visualize the cerebral vasculature and identify large vessel occlusions, which can guide thrombectomy decisions in ischemic stroke.
- However, performing a **non-contrast CT head is a prerequisite** to rule out hemorrhage before proceeding with CTA or any other advanced imaging or therapeutic interventions.
Emergency imaging protocols US Medical PG Question 3: A 42-year-old man presents to the emergency department with abdominal pain. The patient was at home watching television when he experienced sudden and severe abdominal pain that prompted him to instantly call emergency medical services. The patient has a past medical history of obesity, smoking, alcoholism, hypertension, and osteoarthritis. His current medications include lisinopril and ibuprofen. His temperature is 98.5°F (36.9°C), blood pressure is 120/97 mmHg, pulse is 130/min, respirations are 22/min, and oxygen saturation is 97% on room air. The patient is in an antalgic position on the stretcher. His abdomen is rigid and demonstrates rebound tenderness and hypoactive bowel sounds. What is the next best step in management?
- A. CT of the abdomen
- B. Urgent laparoscopy
- C. NPO, IV fluids, and analgesics
- D. Urgent laparotomy (Correct Answer)
- E. Abdominal radiograph
Emergency imaging protocols Explanation: ***Urgent laparotomy***
- The patient's presentation with **sudden, severe abdominal pain**, a **rigid abdomen**, **rebound tenderness**, and **hypoactive bowel sounds** indicates **acute peritonitis**, most likely from a **perforated viscus**.
- In a patient with **frank peritonitis** and clinical signs of perforation, the diagnosis is **made clinically** based on physical examination findings.
- **Urgent laparotomy** (exploratory surgery) is the definitive management and should not be delayed for imaging when peritonitis is obvious.
- The patient's risk factors (NSAID use, alcoholism) further support peptic ulcer perforation as the likely etiology.
*CT of the abdomen*
- While CT scan is highly sensitive for identifying perforation and can provide anatomic detail, it is **not necessary when the diagnosis of peritonitis is clinically evident**.
- In a patient with **obvious peritonitis**, obtaining a CT scan would **delay definitive surgical treatment** without changing management.
- CT is more appropriate for stable patients with **uncertain diagnosis** or equivocal physical findings, not for those with frank peritonitis.
*Urgent laparoscopy*
- **Laparoscopy** can be used diagnostically and therapeutically in selected cases of abdominal emergencies.
- However, in a patient with diffuse peritonitis and suspected perforation, **laparotomy** is generally preferred over laparoscopy as it provides better exposure, faster source control, and easier peritoneal lavage.
- Laparoscopy may be considered in stable patients with localized findings, but this patient has signs of diffuse peritonitis.
*NPO, IV fluids, and analgesics*
- These are **essential supportive measures** and should be initiated immediately as part of resuscitation.
- However, they are **adjunctive** to definitive surgical management and do not constitute the "next best step" in a patient requiring emergency surgery.
- These measures should be initiated concurrently while preparing for urgent laparotomy.
*Abdominal radiograph*
- An **upright chest X-ray** or **abdominal radiograph** can show **free air under the diaphragm** (pneumoperitoneum) in cases of perforation.
- However, it is **only 50-70% sensitive**, meaning it misses many perforations.
- In a patient with **clinical peritonitis**, the absence of free air on X-ray does **not rule out perforation** and should not delay surgery.
- Imaging should not delay surgical intervention when peritonitis is clinically evident.
Emergency imaging protocols US Medical PG Question 4: An otherwise healthy 57-year-old man presents to the emergency department because of progressive shortness of breath and exercise intolerance for the past 5 days. He denies recent travel or illicit habits. His temperature is 36.7°C (98.1°F), the blood pressure is 88/57 mm Hg, and the pulse is 102/min. The radial pulse weakens with inspiration. Physical examination reveals bilateral 1+ pedal edema. There is jugular venous distention at 13 cm and muffled heart sounds. Transthoracic echocardiogram shows reciprocal respiratory ventricular inflow and ventricular diastolic collapse. Which of the following is the best next step in the management of this patient condition?
- A. Pericardiectomy
- B. Pericardial drainage (Correct Answer)
- C. Cardiac catheterization
- D. Cardiac MRI
- E. Chest X-ray
Emergency imaging protocols Explanation: ***Pericardial drainage***
- The clinical presentation, including progressive **shortness of breath**, **hypotension**, **tachycardia**, **pulsus paradoxus** (weak radial pulse with inspiration), **jugular venous distention**, **muffled heart sounds**, and **bilateral pedal edema**, strongly suggests **cardiac tamponade** due to a pericardial effusion.
- Prompt **pericardial drainage** (pericardiocentesis) is a life-saving intervention for cardiac tamponade, as it relieves the pressure on the heart and restores cardiac output.
*Pericardiectomy*
- This is a surgical procedure to remove part or all of the pericardium, typically performed in cases of **constrictive pericarditis** or recurrent effusions that fail conservative management.
- It is a more invasive procedure and not the immediate life-saving intervention required for acute cardiac tamponade.
*Cardiac catheterization*
- This procedure involves inserting a catheter into a blood vessel to measure pressures within the heart chambers and great vessels, often used for diagnosing **coronary artery disease** or valvular heart disease.
- While it can provide hemodynamic data, it is not the most immediate or direct therapeutic intervention for cardiac tamponade.
*Cardiac MRI*
- **Cardiac MRI** provides detailed anatomical imaging of the heart and pericardium, useful for characterizing pericardial effusions or detecting myocardial abnormalities.
- Although it could confirm the diagnosis, it takes time and is not the emergent therapeutic step needed for an unstable patient with cardiac tamponade.
*Chest X-ray*
- A **chest X-ray** might show an enlarged cardiac silhouette (water bottle sign) in cases of large pericardial effusions.
- However, it is not sufficiently sensitive or specific for diagnosing cardiac tamponade and does not provide detailed information about ventricular collapse or hemodynamic compromise.
Emergency imaging protocols US Medical PG Question 5: A 77-year-old man with a history of hypertension and a 46 pack-year smoking history presents to the emergency department from an extended care facility with acute onset of headache, nausea, vomiting, and neck pain which started 6 hours ago and has persisted since. He is alert, but his baseline level of consciousness is slightly diminished per the nursing home staff. His temperature is 99.0°F (37.2°C), blood pressure is 164/94 mmHg, pulse is 90/min, respirations are 16/min, and oxygen saturation is 98% on room air. The patient's neurological exam is unremarkable with cranial nerves II-XII grossly intact and with stable gait with a walker. He is immediately sent for a head CT which is normal. What is the most appropriate next step in management?
- A. Ultrasound
- B. Lumbar puncture (Correct Answer)
- C. Alteplase
- D. Ibuprofen, acetaminophen, metoclopramide, and diphenhydramine
- E. MRI
Emergency imaging protocols Explanation: ***Lumbar puncture***
- The patient's symptoms (acute severe headache, nausea, vomiting, neck pain) and risk factors (hypertension, smoking history) are highly suggestive of a **subarachnoid hemorrhage (SAH)**, even with a normal initial **non-contrast head CT**.
- A **lumbar puncture (LP)** is the next critical diagnostic step to detect **xanthochromia** (due to bilirubin degradation from red blood cells) or elevated red blood cell count in the cerebrospinal fluid (CSF), which would confirm SAH.
- CT has approximately **95% sensitivity in the first 6 hours**, but sensitivity decreases over time, making LP essential when clinical suspicion remains high.
*Ultrasound*
- **Ultrasound** is not a standard diagnostic tool for acute neurological symptoms like severe headache or suspected SAH.
- It is primarily used for evaluating soft tissues, abdominal organs, and vascular structures like carotid arteries, but offers limited utility for intracranial bleeding.
*Alteplase*
- **Alteplase** (tissue plasminogen activator, tPA) is a thrombolytic agent used in acute ischemic stroke, characterized by focal neurological deficits due to arterial occlusion.
- Administering alteplase in the setting of headache and neck pain without focal deficits, while SAH is suspected, could be fatal as it would worsen bleeding.
*Ibuprofen, acetaminophen, metoclopramide, and diphenhydramine*
- This combination of medications is used for **symptomatic relief** of headache and nausea but does not address the underlying potentially life-threatening cause.
- Treating symptoms without a definitive diagnosis in suspected SAH could lead to delayed intervention and worse outcomes.
*MRI*
- While **MRI with specific sequences (FLAIR, GRE, SWI)** has high sensitivity for detecting SAH and is increasingly used in clinical practice, **lumbar puncture remains the traditional and most widely recommended next step** after a negative CT in suspected SAH.
- LP directly detects **xanthochromia** (present 6-12 hours after bleeding) and RBCs in CSF, providing definitive evidence of SAH.
- MRI may not always be readily available in the emergency setting, takes longer to perform, and requires patient stability and cooperation.
- For standardized exams, **LP is the classic correct answer** when CT is negative but clinical suspicion for SAH remains high.
Emergency imaging protocols US Medical PG Question 6: A 27-year-old soldier is brought to the emergency department of a military hospital 20 minutes after being involved in a motor vehicle accident during a training exercise. He was an unrestrained passenger. On arrival, he has shortness of breath and chest pain. He appears pale and anxious. His temperature is 37°C (98.6°F), pulse is 110/min, respirations are 20/min, and blood pressure is 100/65 mm Hg. He is alert and oriented to person, place, and time. Examination shows pale conjunctivae and mucous membranes. There is bruising on the chest, extremities, and abdomen. The lungs are clear to auscultation. He has normal heart sounds and flat neck veins. The abdomen is flat, soft, and mildly tender. The remainder of the physical examination shows no abnormalities. High-flow oxygen is applied, and intravenous fluid resuscitation is begun. A chest x-ray is obtained. Which of the following is the most appropriate next step in management?
- A. Placement of a chest tube
- B. Pericardiocentesis
- C. Abdominal ultrasonography
- D. Intubation with positive pressure ventilation
- E. CT scan of the chest with contrast (Correct Answer)
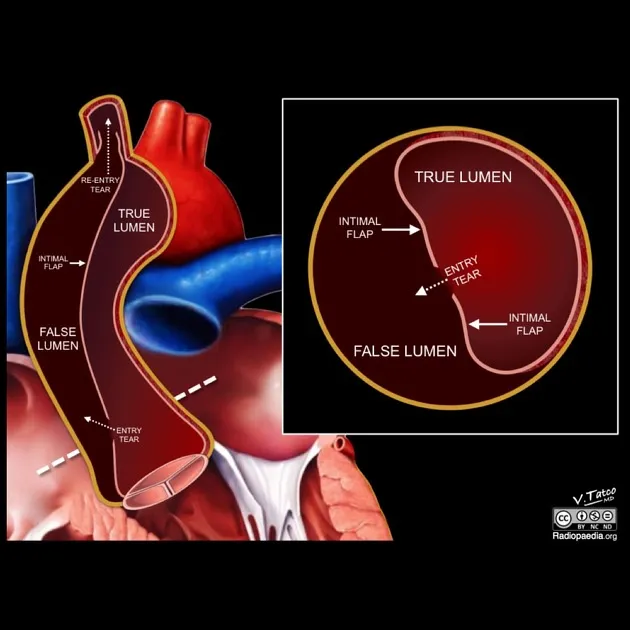
Emergency imaging protocols Explanation: ***CT scan of the chest with contrast***
- The patient has suffered a **blunt chest trauma** with symptoms including shortness of breath, chest pain, and signs of potential internal bleeding (pale, anxious, tachycardia, mild hypotension).
- A chest X-ray was performed; however, a **CT scan with contrast** is essential to further evaluate for **aortic injury**, **pulmonary contusions**, or other subtle thoracic injuries that may not be evident on plain radiographs, especially given the mechanism of injury (unrestrained passenger in a MVA).
*Placement of a chest tube*
- This intervention is indicated for conditions like **pneumothorax** or **hemothorax**, which would typically present with **diminished breath sounds** on the affected side or characteristic X-ray findings.
- The patient's lungs are described as **clear to auscultation**, and no specific X-ray findings are mentioned that would necessitate immediate chest tube placement.
*Pericardiocentesis*
- This procedure is performed for **cardiac tamponade**, which would manifest with muffled heart sounds, jugular venous distention, and pulsus paradoxus.
- The patient has **normal heart sounds** and **flat neck veins**, making cardiac tamponade less likely.
*Abdominal ultrasonography*
- While the patient has bruising and mild tenderness in the abdomen, suggesting potential **abdominal injury**, the primary life-threatening concerns based on his presentation (shortness of breath, chest pain, chest X-ray ordered) are thoracic.
- A **Focused Assessment with Sonography for Trauma (FAST) exam** would be appropriate if the abdominal tenderness was more pronounced or if there were signs of active intra-abdominal bleeding, but the immediate priority is to rule out life-threatening thoracic injuries.
*Intubation with positive pressure ventilation*
- This is indicated for patients with **respiratory failure** or an inability to protect their airway. The patient's respiratory rate is 20/min (within normal limits), and he is **alert and oriented**.
- While high-flow oxygen and fluid resuscitation have been initiated, there is no indication of impending respiratory collapse that would necessitate immediate intubation.
Emergency imaging protocols US Medical PG Question 7: A 43-year-old man presents with acute-onset left flank pain for the past 6 hours. He describes the pain as severe, intermittent, colicky, and “coming in waves”, and he points to the area of the left costovertebral angle (CVA). He says he recently has been restricting oral liquid intake to only 2 glasses of water per day based on the advice of his healer. He also reports nausea and vomiting. The patient has a history of hypertension, gout, and type 2 diabetes mellitus. He is afebrile, and his vital signs are within normal limits. On physical examination, he is writhing in pain and moaning. There is exquisite left CVA tenderness. A urinalysis shows gross hematuria. Which of the following is the next best step in the management of this patient?
- A. Non-contrast CT of the abdomen
- B. Contrast CT of the abdomen and pelvis
- C. Supine abdominal radiograph
- D. Renal ultrasound
- E. Non-contrast CT of the abdomen and pelvis (Correct Answer)
Emergency imaging protocols Explanation: **Non-contrast CT of the abdomen and pelvis**
- **Non-contrast CT of the abdomen and pelvis** is the gold standard for diagnosing urolithiasis, providing high sensitivity and specificity for detecting stones, identifying their size and location, and assessing for hydronephrosis.
- The patient's presentation with **acute-onset, severe, colicky flank pain**, nausea, vomiting, gross hematuria, and CVA tenderness is highly suggestive of **renal colic due to a kidney stone**.
*Non-contrast CT of the abdomen*
- This option is **insufficient** as kidney stones can be located in the ureters within the pelvis; a scan of the abdomen alone might miss stones in the distal ureter.
- While a non-contrast CT is appropriate, the scope of only the abdomen is **incomplete** for evaluating the entire urinary tract that might be affected by stones.
*Contrast CT of the abdomen and pelvis*
- **Contrast-enhanced CT is generally not indicated** for the initial evaluation of suspected renal colic due to urolithiasis because it can obscure the visualization of urinary stones.
- The use of contrast also carries risks such as **allergic reaction** and **contrast-induced nephropathy**, which are unnecessary in this acute, non-complicated setting.
*Supine abdominal radiograph*
- A supine abdominal radiograph (KUB) has **limited sensitivity** for detecting kidney stones, especially radiolucent stones (e.g., uric acid stones) or small stones.
- It also provides **poor anatomical detail** and cannot assess for hydronephrosis or other complications as effectively as CT.
*Renal ultrasound*
- Renal ultrasound can detect **hydronephrosis** and some kidney stones but is less sensitive than CT for visualizing smaller stones, especially in the ureters.
- Its diagnostic utility can be **limited by body habitus** and operator dependence, making it less reliable as a primary diagnostic tool for acute renal colic.
Emergency imaging protocols US Medical PG Question 8: A 70-year-old man with a history of chronic constipation presents to the emergency department with a two-day history of left lower quadrant abdominal pain. He is found to have a temperature of 100.8F, BP 140/90, HR 85, and RR 16. On physical examination, he is tender to light palpation in the left lower quadrant and exhibits voluntary guarding. Rectal examination reveals heme-positive stool. Laboratory values are unremarkable except for a WBC count of 12,500 with a left shift. Which of the following tests would be most useful in the diagnosis of this patient's disease?
- A. Abdominal x-ray
- B. Abdominal CT (Correct Answer)
- C. Emergent colonoscopy
- D. Left lower quadrant ultrasound
- E. Lipase
Emergency imaging protocols Explanation: ***Abdominal CT***
- **CT scan** is the most accurate imaging modality for diagnosing **diverticulitis**, identifying bowel wall thickening, inflammation, and complications such as abscess formation.
- It effectively differentiates diverticulitis from other causes of **left lower quadrant pain** and can guide intervention if necessary.
*Abdominal x-ray*
- An **abdominal x-ray** is generally not useful for diagnosing **diverticulitis** as it provides limited soft tissue detail.
- It may identify free air in cases of perforation, but it is not sensitive or specific for diverticular inflammation.
*Emergent colonoscopy*
- **Colonoscopy** is generally contraindicated in acute **diverticulitis** due to the risk of **perforation** of the inflamed colon.
- It is typically performed after recovery from an acute episode (usually 4-6 weeks later) to rule out underlying malignancy or other inflammatory bowel conditions.
*Left lower quadrant ultrasound*
- While **ultrasound** can identify diverticulitis, its diagnostic accuracy is highly **operator-dependent** and can be limited by bowel gas.
- It is often less sensitive than CT, particularly for deeper structures or in obese patients, making **CT** the preferred initial imaging study.
*Lipase*
- **Lipase** is a marker for **pancreatitis** and is not relevant for the diagnosis of **diverticulitis**.
- The patient's symptoms are localized to the left lower quadrant and are not suggestive of pancreatic inflammation.
Emergency imaging protocols US Medical PG Question 9: A 27-year-old man is witnessed falling off his bicycle. The patient rode his bicycle into a curb and hit his face against a rail. The patient did not lose consciousness and is ambulatory at the scene. There is blood in the patient's mouth and one of the patient's teeth is found on the sidewalk. The patient is transferred to the local emergency department. Which of the following is the best method to transport this patient's tooth?
- A. Wrapped in gauze soaked in normal saline
- B. Submerged in normal saline
- C. Submerged in milk (Correct Answer)
- D. Wrapped in sterile gauze
- E. Submerged in water
Emergency imaging protocols Explanation: ***Submerged in milk***
- **Milk** is the ideal solution for transporting an avulsed tooth because it has a pH and osmolality that is compatible with the **vitality of the periodontal ligament (PDL) cells**.
- Its nutrient content also helps to sustain these cells, increasing the likelihood of successful **replantation**.
*Wrapped in gauze soaked in normal saline*
- While **normal saline** can keep the tooth moist, its osmolality is not optimal for maintaining the **viability of PDL cells** for an extended period.
- Wrapping in gauze may also cause the tooth to dry out if not kept adequately saturated, which can damage the **periodontal ligament**.
*Submerged in normal saline*
- Submerging in **normal saline** is better than dry storage but is still **suboptimal** compared to milk.
- The tonicity and pH of normal saline are not as beneficial for the **long-term survival of PDL cells** as milk.
*Wrapped in sterile gauze*
- **Sterile gauze** alone does not provide moisture or nutrients, leading to **rapid desiccation and death of PDL cells**.
- A dry environment dramatically reduces the chances of successful **replantation** and increases the risk of **ankylosis** or **resorption**.
*Submerged in water*
- **Water** is a **hypotonic solution** that can cause **lysis of PDL cells** due to osmotic pressure differences.
- This significantly compromises the tooth's viability and success of **replantation**.
Emergency imaging protocols US Medical PG Question 10: A 40-year-old woman is brought to the emergency department by a paramedic team from the scene of a motor vehicle accident where she was the driver. The patient was restrained by a seat belt and was unconscious at the scene. On physical examination, the patient appears to have multiple injuries involving the trunk and extremities. There are no penetrating injuries to the chest. As part of her trauma workup, a CT scan of the chest is ordered. At what vertebral level of the thorax is this image from?
- A. T1
- B. T6
- C. T4
- D. T5
- E. T8 (Correct Answer)
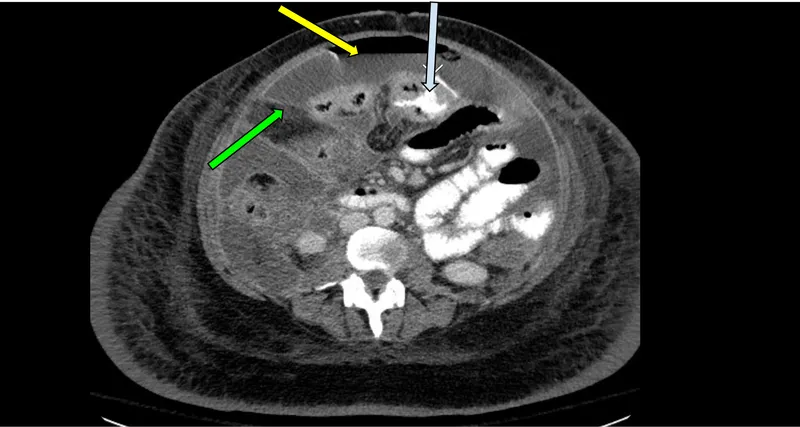
Emergency imaging protocols Explanation: ***T8***
- The CT image shows the **inferior vena cava (IVC)** located anterior and to the right of the aorta, and the **esophagus** located posterior to the aorta and slightly to the left. The **azygos vein** is seen to the right of the vertebral body and posterior to the esophagus.
- The **mainstem bronchi** are no longer visible, indicating a level below the carina. The presence of the IVC, aorta, esophagus, and azygos vein with the absence of mainstem bronchi is characteristic of the **T8 vertebral level**.
*T1*
- At the T1 level, the structures would primarily be the **trachea** anterior to the esophagus, with the main great vessels (e.g., brachiocephalic veins and arteries) visible, not the IVC.
- The mainstem bronchi would not yet be visualized at this higher level.
*T6*
- At the T6 level, the **trachea would have already bifurcated into the mainstem bronchi**, which would be prominent structures visible on the CT scan.
- While the aorta and esophagus would be present, the specific arrangement relative to the mainstem bronchi would differentiate it from T8.
*T4*
- The T4 level is typically associated with the **carina**, where the trachea bifurcates into the mainstem bronchi.
- The great vessels would be prominent, but the IVC in its more inferior course would not be as distinctly visualized in this configuration compared to T8.
*T5*
- At the T5 level, the **mainstem bronchi** would still be clearly visible, having just diverged from the trachea.
- While vessels like the aorta are present, the key differentiating factor from T8 is the presence of the mainstem bronchi.
More Emergency imaging protocols US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.