Contrast studies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Contrast studies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Contrast studies US Medical PG Question 1: A 72-year-old female presents to the emergency department complaining of severe abdominal pain and several days of bloody diarrhea. Her symptoms began with intermittent bloody diarrhea five days ago and have worsened steadily. For the last 24 hours, she has complained of fevers, chills, and abdominal pain. She has a history of ulcerative colitis, idiopathic hypertension, and hypothyroidism. Her medications include hydrochlorothiazide, levothyroxine, and sulfasalazine.
In the ED, her temperature is 39.1°C (102.4°F), pulse is 120/min, blood pressure is 90/60 mmHg, and respirations are 20/min. On exam, the patient is alert and oriented to person and place, but does not know the day. Her mucus membranes are dry. Heart and lung exam are not revealing. Her abdomen is distended with marked rebound tenderness. Bowel sounds are hyperactive.
Serum:
Na+: 142 mEq/L
Cl-: 107 mEq/L
K+: 3.3 mEq/L
HCO3-: 20 mEq/L
BUN: 15 mg/dL
Glucose: 92 mg/dL
Creatinine: 1.2 mg/dL
Calcium: 10.1 mg/dL
Hemoglobin: 11.2 g/dL
Hematocrit: 30%
Leukocyte count: 14,600/mm^3 with normal differential
Platelet count: 405,000/mm^3
What is the next best step in management?
- A. Emergent colonoscopy
- B. Contrast enema
- C. Colectomy
- D. Plain abdominal radiograph
- E. Abdominal CT with IV contrast (Correct Answer)
Contrast studies Explanation: ***Abdominal CT with IV contrast***
- The patient presents with **severe abdominal pain, bloody diarrhea, fever, hypotension, tachycardia, abdominal distension, rebound tenderness, and leukocytosis**, all suggestive of **toxic megacolon** complicating her ulcerative colitis.
- An **abdominal CT with IV contrast** is the most appropriate next step to confirm the diagnosis, assess the extent of colonic dilation and inflammation, and rule out complications like perforation.
*Emergent colonoscopy*
- **Colonoscopy** is generally **contraindicated** in suspected toxic megacolon due to the high risk of **perforation** of the severely inflamed and dilated colon.
- While it can diagnose ulcerative colitis, the current acute, severe presentation makes it too risky.
*Contrast enema*
- A **contrast enema** is also **contraindicated** in setting of potential **toxic megacolon** or suspected colonic perforation.
- The pressure from the contrast agent could worsen dilation or cause perforation in an already compromised colon.
*Colectomy*
- **Colectomy** is a surgical intervention reserved for cases of **toxic megacolon** that **fail medical management** or when there is evidence of **perforation** or **ischemia**.
- It is not the *immediate* next step in management without further imaging and attempts at medical stabilization.
*Plain abdominal radiograph*
- A plain abdominal radiograph can show colonic dilation and air-fluid levels, which are indicative of toxic megacolon; however, it has **limited ability to assess the extent of inflammation**, detect complications like **perforation**, or rule out other intra-abdominal pathologies.
- It might be a useful initial screen but is not as comprehensive as a CT scan, especially when a definitive diagnosis and management plan is needed.
Contrast studies US Medical PG Question 2: A 81-year-old man presents to his cardiologist for ongoing management of mild heart failure. He has not had any changes in his cardiac function status and says that he is tolerating lisinopril without any major side effects. During the course of the visit, the patient says that he is unhappy with his urologist because he has been experiencing episodes of dizziness after starting prazosin for benign prostatic hyperplasia. He says that he feels these episodes were caused by malpractice on his urologist's behalf and is considering a lawsuit against his urologist. Which of the following is the most appropriate course of action for the cardiologist?
- A. Call the urologist and warn him of an impending lawsuit
- B. Encourage the patient to speak with his urologist directly (Correct Answer)
- C. Call the urologist to convey the patient's dissatisfaction
- D. Contact his insurance agent to discuss possible risks
- E. Sympathize with the patient's desire for a lawsuit
Contrast studies Explanation: ***Encourage the patient to speak with his urologist directly***
- It is crucial to promote **direct patient-physician communication** to resolve concerns, as this often de-escalates potential conflicts and fosters a better therapeutic relationship.
- The cardiologist's role is to facilitate this communication, empowering the patient to voice concerns directly to the treating physician, rather than acting as an intermediary or advisor on legal matters.
*Call the urologist and warn him of an impending lawsuit*
- This action is **unprofessional** and violates the patient's right to privacy and confidentiality, as the patient has not given consent for such disclosure.
- It can also establish an antagonistic dynamic between the physicians and may not be based on established facts of a lawsuit.
*Call the urologist to convey the patient's dissatisfaction*
- This is an **indirect approach** that bypasses the patient's responsibility to communicate his concerns directly and denies the urologist the opportunity to address the patient's specific grievances firsthand.
- The cardiologist should not act as a messenger between the patient and another physician without the patient's explicit request or consent, especially when the concern involves the other physician's care.
*Contact his insurance agent to discuss possible risks*
- This action is **premature** and assumes the lawsuit is imminent, which is speculative and based solely on the patient's expressed intent.
- The cardiologist's primary concern should be the patient's well-being and facilitating communication, not preemptively engaging in defensive measures for another doctor.
*Sympathize with the patient's desire for a lawsuit*
- While it's important to empathize with the patient's feelings of dissatisfaction, actively sympathizing with the desire for a lawsuit could be interpreted as **endorsing legal action**, which is beyond the cardiologist's medical scope.
- The cardiologist should remain neutral regarding legal proceedings and focus on medical care and facilitating appropriate communication channels for conflict resolution.
Contrast studies US Medical PG Question 3: A drug research team has synthesized a novel oral drug that acts as an agonist at multiple adrenergic receptors. When administered in animals, it has been shown to produce urinary retention at therapeutic doses with the absence of other manifestations of adrenergic stimulation. The researchers are interested in understanding signal transduction and molecular mechanisms behind the action of the novel drug. Which of the following receptors would most likely transduce signals across the plasma membrane following the administration of this novel drug?
- A. GoPCRs (Go protein-coupled receptors)
- B. GsPCRs (Gs protein-coupled receptors)
- C. GqPCRs (Gq protein-coupled receptors) (Correct Answer)
- D. GtPCRs (Gt protein-coupled receptors)
- E. GiPCRs (Gi protein-coupled receptors)
Contrast studies Explanation: ***GqPCRs (Gq protein-coupled receptors)***
- **Urinary retention** is primarily mediated by the activation of **alpha-1 adrenergic receptors** in the bladder neck and prostate, which are classically Gq-protein coupled receptors.
- Activation of **GqPCRs** leads to the activation of **phospholipase C**, increased **IP3 (inositol trisphosphate)** and **DAG (diacylglycerol)**, and subsequently, a rise in intracellular **calcium**, causing smooth muscle contraction.
*GoPCRs (Go protein-coupled receptors)*
- While Go proteins are a subtype of Gi/Go family, their direct primary role in mediating **urinary retention** via **adrenergic agonism** is not as well-established as Gq.
- Go signaling often involves modulation of **ion channels** and can be involved in neuronal signaling, not directly causing smooth muscle contraction in the bladder.
*GsPCRs (Gs protein-coupled receptors)*
- **GsPCRs** (e.g., beta-adrenergic receptors) activate **adenylate cyclase**, leading to increased **cAMP** levels, which typically causes smooth muscle relaxation.
- This effect would promote **urinary relaxation** and flow, not retention, and hence is contrary to the observed drug effect.
*GtPCRs (Gt protein-coupled receptors)*
- **GtPCRs** (transducin) are primarily involved in the **phototransduction** cascade in the retina, mediating vision.
- They have no known central role in mediating adrenergic effects on the **urinary tract smooth muscle**.
*GiPCRs (Gi protein-coupled receptors)*
- **GiPCRs** (e.g., alpha-2 adrenergic receptors) inhibit **adenylate cyclase**, leading to decreased **cAMP** levels, which generally causes smooth muscle contraction in some tissues, but also presynaptic inhibition.
- While Gi activation can lead to contraction in some contexts, the primary mechanism of **urinary retention** via bladder neck contraction is through alpha-1 receptors linked to Gq.
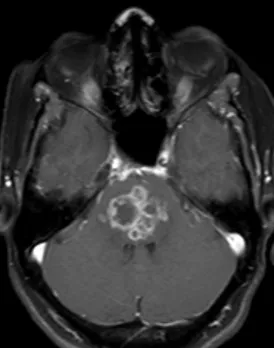
Contrast studies US Medical PG Question 4: A 30-year-old obese female presents with new-onset headaches, ringing in her ears, and blurry vision. Ibuprofen and avoidance of light has not relieved her symptoms. She denies a history of recent trauma, fever, chills, and fatigue. Past medical history is significant for type 2 diabetes mellitus managed with metformin. She has had 20/20 vision her whole life and wonders if she might need to get eyeglasses. She has 2 healthy school-age children. Her temperature is 36.8°C (98.2°F), heart rate is 90/min, respiratory rate is 15/min, and blood pressure is 135/80 mm Hg. Physical exam is notable for decreased lateral eye movement, and the funduscopic findings are shown in the picture. Laboratory findings are within normal limits and brain imaging is normal. Lumbar puncture demonstrates an elevated opening pressure and normal CSF composition. Which of the following is a side effect of the medication used to treat this condition?
- A. Elevated liver function tests
- B. Rhabdomyolysis
- C. Kidney stones (Correct Answer)
- D. Pancreatitis
- E. Decreased white blood cell count
Contrast studies Explanation: ***Kidney stones***
- The patient's symptoms (headaches, tinnitus, blurry vision), **obesity**, normal brain imaging, and **elevated CSF opening pressure with normal CSF composition** are classic for **idiopathic intracranial hypertension (IIH)**, also known as pseudotumor cerebri.
- The first-line medical treatment for IIH is **acetazolamide**, a carbonic anhydrase inhibitor, which commonly causes **kidney stones** due to altered urine pH and reduced citrate excretion.
*Elevated liver function tests*
- While some medications can cause elevated liver function tests, this is not a typical or common side effect of **acetazolamide**.
- **Acetaminophen** overdose or certain antibiotics are more frequently associated with this side effect.
*Rhabdomyolysis*
- **Rhabdomyolysis** is characterized by muscle breakdown and is often associated with statin use, significant trauma, or certain illicit drugs.
- It is not a known side effect of **acetazolamide**.
*Pancreatitis*
- **Pancreatitis** can be a side effect of various medications (e.g., thiopurines, certain diuretics), but it is not commonly associated with **acetazolamide**.
- The patient's history of Type 2 Diabetes is a risk factor for pancreatitis, but not directly linked to the treatment of IIH.
*Decreased white blood cell count*
- A decrease in white blood cell count (leukopenia or agranulocytosis) is a serious but rare side effect of certain medications, such as **clozapine** or **methimazole**.
- It is not a typical side effect of **acetazolamide**.
Contrast studies US Medical PG Question 5: A new drug X is being tested for its effect on renal function. During the experiments, the researchers found that in patients taking substance X, the urinary concentration of sodium decreases while urine potassium concentration increase. Which of the following affects the kidneys in the same way as does substance X?
- A. Aldosterone (Correct Answer)
- B. Furosemide
- C. Spironolactone
- D. Atrial natriuretic peptide
- E. Hydrochlorothiazide
Contrast studies Explanation: ***Aldosterone***
- **Aldosterone** acts on the **principal cells** of the **collecting duct** to increase sodium reabsorption and potassium secretion.
- This action leads to a decrease in urinary sodium concentration and an increase in urinary potassium concentration, matching the effects of drug X.
*Furosemide*
- **Furosemide** is a **loop diuretic** that inhibits the **Na-K-2Cl cotransporter** in the **thick ascending limb** of the loop of Henle.
- This inhibition leads to increased excretion of sodium, potassium, and water, resulting in higher urinary sodium concentration.
*Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that blocks aldosterone's effects on the collecting duct.
- This leads to increased sodium excretion and decreased potassium excretion (potassium-sparing effect), which is the opposite of drug X.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** is released in response to atrial stretch and causes **natriuresis** (increased sodium excretion) and **diuresis**.
- It works by dilating afferent arterioles and constricting efferent arterioles, increasing GFR, and inhibiting sodium reabsorption, thus increasing urinary sodium concentration.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** that inhibits the **Na-Cl cotransporter** in the **distal convoluted tubule**.
- This leads to increased sodium and chloride excretion but typically causes potassium wasting (hypokalemia), which differs from the increased urinary potassium concentration seen with drug X.
Contrast studies US Medical PG Question 6: A 37-year-old woman presents to the Emergency Department after 8 hours of left sided flank pain that radiates to her groin and pelvic pain while urinating. Her medical history is relevant for multiple episodes of urinary tract infections, some requiring hospitalization, and intravenous antibiotics. In the hospital, her blood pressure is 125/83 mm Hg, pulse of 88/min, a respiratory rate of 28/min, and a body temperature of 36.5°C (97.7°F). On physical examination, she has left costovertebral tenderness and lower abdominal pain. Laboratory studies include a negative pregnancy test, mild azotemia, and a urinary dipstick that is positive for blood. Which of the following initial tests would be most useful in the diagnosis of this case?
- A. Urine osmolality
- B. Fractional excretion of sodium (FeNa+)
- C. Renal ultrasonography (Correct Answer)
- D. Contrast abdominal computed tomography
- E. Blood urea nitrogen (BUN): serum creatinine (SCr) ratio
Contrast studies Explanation: ***Renal ultrasonography***
- This is the most appropriate initial imaging test to evaluate for **kidney stones** (given the flank pain radiating to groin and hematuria) and **hydronephrosis** (which can indicate obstruction) and assess for signs of **pyelonephritis** (given the history of recurrent UTIs and CVA tenderness).
- It is **non-invasive**, readily available, and avoids radiation exposure, making it suitable as a first-line diagnostic tool in this setting.
*Urine osmolality*
- This test primarily assesses the kidney's ability to **concentrate urine**, which is more relevant for evaluating fluid balance, diabetes insipidus, or other renal tubular disorders.
- It would not directly diagnose the cause of acute flank pain or urinary tract obstruction.
*Fractional excretion of sodium (FeNa+)*
- FeNa+ is used to differentiate between **prerenal azotemia** and **acute tubular necrosis**, indicating the kidney's response to hypoperfusion.
- While the patient has mild azotemia, FeNa+ would not identify the underlying cause of the flank pain, hematuria, or potential obstruction.
*Contrast abdominal computed tomography*
- While highly sensitive for diagnosing kidney stones and other renal pathologies, **contrast CT** exposes the patient to **ionizing radiation** and risks associated with contrast agents (e.g., contrast-induced nephropathy), especially with pre-existing azotemia.
- It is often reserved for cases where ultrasound is inconclusive or more detailed anatomical information is needed.
*Blood urea nitrogen (BUN): serum creatinine (SCr) ratio*
- This ratio is primarily used to differentiate between **prerenal** causes of acute kidney injury (high ratio, e.g., >20:1) and **intrinsic renal** causes (lower ratio, e.g., <15:1).
- While it can provide insight into the etiology of azotemia, it does not directly identify the cause of the patient's acute flank pain or potential urinary tract obstruction.
Contrast studies US Medical PG Question 7: A 23-year-old woman comes to the emergency department for the evaluation of mild retrosternal pain for the last 7 hours after several episodes of self-induced vomiting. The patient was diagnosed with bulimia nervosa 9 months ago. Her only medication is citalopram. She is 170 cm (5 ft 7 in) tall and weighs 62 kg (136.6 lb); BMI is 21.5 kg/m2. She appears pale. Her temperature is 37°C (98.6°F), pulse is 75/min, respirations are 21/min, and blood pressure is 110/75 mm Hg. The lungs are clear to auscultation. Cardiac examinations shows no murmurs, rubs, or gallops. The abdomen is soft and nontender with no organomegaly. The remainder of the physical examination shows swelling of the salivary glands, dry skin, and brittle nails. An ECG and an x-ray of the chest show no abnormalities. Contrast esophagram with gastrografin shows mild leakage of contrast from the lower esophagus into the mediastinum without contrast extravasation into the pleural and peritoneal cavities. Which of the following is the most appropriate next step in the management?
- A. Diagnostic endoscopy
- B. CT scan with contrast
- C. Intravenous labetalol therapy
- D. Intravenous ampicillin and sulbactam therapy (Correct Answer)
- E. Intravenous octreotide therapy
Contrast studies Explanation: **Intravenous ampicillin and sulbactam therapy**
- The patient presents with a **mild esophageal leak** into the mediastinum following self-induced vomiting, strongly suggesting **Boerhaave syndrome** or esophageal perforation. This condition is prone to rapid infection due to contamination from esophageal contents.
- **Broad-spectrum antibiotics**, such as ampicillin and sulbactam, are crucial to prevent or treat **mediastinitis** and sepsis, which are life-threatening complications of esophageal perforation.
*Diagnostic endoscopy*
- **Endoscopy is contraindicated** in suspected esophageal perforation as insufflation of air can worsen the mediastinal contamination and increase the size of the perforation.
- It is generally reserved for stable patients with upper gastrointestinal bleeding or foreign body removal when perforation is not suspected.
*CT scan with contrast*
- A **CT scan with oral and intravenous contrast** would be the *next diagnostic step* to better delineate the extent of the esophageal injury and mediastinal involvement. However, it is not the *most appropriate initial management step*, which should prioritize stabilizing the patient and preventing infection.
- The question asks for the **most appropriate *next step in management*** after a diagnosis of a mild leak has been made by gastrografin esophagram, not the next diagnostic test.
*Intravenous labetalol therapy*
- **Labetalol is a beta-blocker** used to reduce blood pressure and heart rate, typically in conditions like hypertensive urgency/emergency or aortic dissection.
- There is no indication for labetalol in this patient, as her blood pressure and pulse are stable, and the primary issue is esophageal perforation.
*Intravenous octreotide therapy*
- **Octreotide** is a somatostatin analog primarily used to reduce portal pressure in **variceal bleeding** or to manage neuroendocrine tumors.
- It has no role in the management of esophageal perforation or mediastinal leak.
Contrast studies US Medical PG Question 8: A 27-year-old woman comes to the emergency department because of progressive numbness and weakness in her left arm and left leg for 2 days. During this period, she has also had urinary urgency and incontinence. Three months ago, she had blurry vision, difficulty distinguishing colors, and headache for one week, all of which have resolved. The patient has smoked a half pack of cigarettes daily for 10 years and drinks four glasses of wine each week. Her temperature is 37°C (98.6°F), pulse is 78/min, respirations are 14/min, and blood pressure is 110/68 mm Hg. Examination shows 3/5 strength in the left arm and leg, and 5/5 strength on the right side. Upon flexion of the neck, the patient experiences a shooting electric sensation that travels down the spine. MRI of the brain shows gadolinium-enhancing lesions in the right central sulcus, cervical spinal cord, and optic nerve. Which of the following is the most appropriate next step in the management of this patient?
- A. Administer lorazepam
- B. Plasmapheresis
- C. Administer IV methylprednisolone (Correct Answer)
- D. Glatiramer acetate therapy
- E. Administer tissue plasminogen activator
Contrast studies Explanation: ***Administer IV methylprednisolone***
- This patient presents with an acute exacerbation of **multiple sclerosis (MS)**, characterized by new neurological deficits (numbness, weakness, urinary urgency) and resolving symptoms that point to prior demyelination (blurry vision).
- High-dose **intravenous corticosteroids** like methylprednisolone are the first-line treatment for acute MS relapses to reduce inflammation and shorten the duration of the attack.
*Administer lorazepam*
- **Lorazepam** is a benzodiazepine primarily used for anxiety, seizures, or agitation and does not address the underlying inflammatory process of an acute MS exacerbation.
- While some MS patients may experience anxiety, it is not the indicated treatment for acute neurological deficits.
*Plasmapheresis*
- **Plasmapheresis** is considered for severe MS exacerbations that are refractory to high-dose corticosteroids.
- It is not typically the first-line treatment in an acute relapse unless corticosteroids have failed.
*Glatiramer acetate therapy*
- **Glatiramer acetate** is a disease-modifying therapy (DMT) for MS, used to reduce the frequency of relapses and prevent disease progression.
- It is administered long-term but is not an appropriate treatment for an acute MS exacerbation.
*Administer tissue plasminogen activator*
- **Tissue plasminogen activator (tPA)** is a thrombolytic agent used to treat acute ischemic stroke by dissolving blood clots.
- This patient's symptoms are neurological but are consistent with demyelination rather than an ischemic event, making tPA inappropriate.
Contrast studies US Medical PG Question 9: A researcher is investigating the effects of a new antihypertensive medication on renal physiology. She gives a subject a dose of the new medication, and she then collects plasma and urine samples. She finds the following: Hematocrit: 40%; Serum creatinine: 0.0125 mg/mL; Urine creatinine: 1.25 mg/mL. Urinary output is 1 mL/min. Renal blood flow is 1 L/min. Based on the above information and approximating that the creatinine clearance is equal to the GFR, what answer best approximates filtration fraction in this case?
- A. 10%
- B. 17% (Correct Answer)
- C. 33%
- D. 50%
- E. 25%
Contrast studies Explanation: ***17%***
- First, calculate **GFR** using the creatinine clearance formula: GFR = (Urine creatinine × Urinary output) / Serum creatinine = (1.25 mg/mL × 1 mL/min) / 0.0125 mg/mL = **100 mL/min**.
- Next, calculate **Renal Plasma Flow (RPF)** from Renal Blood Flow (RBF) and Hematocrit: RPF = RBF × (1 - Hematocrit) = 1000 mL/min × (1 - 0.40) = **600 mL/min**.
- Finally, calculate **Filtration Fraction (FF)** = GFR / RPF = 100 mL/min / 600 mL/min = 0.1667 = **16.7%, which approximates to 17%**.
- This is the correct answer based on the physiological calculations and represents a normal filtration fraction.
*10%*
- This would correspond to a filtration fraction of 0.10, which would require either a GFR of 60 mL/min (lower than calculated) or an RPF of 1000 mL/min (higher than calculated).
- This value is too low given the provided parameters and doesn't match the calculation from the given data.
*25%*
- This value would suggest FF = 0.25, requiring a GFR of 150 mL/min with the calculated RPF of 600 mL/min.
- This is higher than the calculated GFR of 100 mL/min and doesn't match the given creatinine values.
*33%*
- This would imply FF = 0.33, requiring a GFR of approximately 200 mL/min with RPF of 600 mL/min.
- This is significantly higher than the calculated GFR and would represent an abnormally elevated filtration fraction.
*50%*
- A filtration fraction of 50% is unphysiologically high and would indicate severe pathology.
- This would require a GFR of 300 mL/min with the calculated RPF, which is impossible given the provided creatinine clearance data.
Contrast studies US Medical PG Question 10: A 74-year-old male is brought to the emergency department 1 hour after he fell from the top of the staircase at home. He reports pain in his neck as well as weakness of his upper extremities. He is alert and immobilized in a cervical collar. He has hypertension treated with hydrochlorothiazide. His pulse is 90/min and regular, respirations are 18/min, and blood pressure is 140/70 mmHg. Examination shows bruising and midline cervical tenderness. Neurologic examination shows diminished strength and sensation to pain and temperature in the upper extremities, particularly in the hands. Upper extremity deep tendon reflexes are absent. Strength, sensation, and reflexes in the lower extremities are intact. Anal sensation and tone are present. Babinski's sign is absent bilaterally. Which of the following is most likely to confirm the cause of this patient's neurologic examination findings?
- A. CT angiography of the neck
- B. MRI of the cervical spine without contrast (Correct Answer)
- C. X-ray of the cervical spine
- D. CT of the cervical spine with contrast
- E. Cervical myelography
Contrast studies Explanation: ***MRI of the cervical spine without contrast***
- This patient presents with symptoms consistent with **central cord syndrome**, characterized by greater weakness in the upper extremities than the lower extremities, often following a hyperextension injury in older adults with pre-existing cervical spondylosis. **MRI is the gold standard for visualizing soft tissue injuries**, including spinal cord compression, edema, or hemorrhage, which are typical causes of central cord syndrome.
- Given the primary concern for spinal cord injury and the detailed neurological deficits indicating specific cord involvement, **MRI** offers the best resolution for evaluating the extent of cord damage, disc herniation, ligamentous injury, and pre-existing degenerative changes.
*CT angiography of the neck*
- **CT angiography** primarily evaluates the **vascular structures** of the neck (e.g., carotid and vertebral arteries) for dissection, stenosis, or occlusion.
- While vascular injury could occur in trauma, the patient's neurological findings (disproportionate upper extremity weakness, pain and temperature sensation loss) point more directly to **spinal cord pathology** rather than isolated vascular compromise as the primary cause.
*X-ray of the cervical spine*
- **X-rays** are useful for initial screening of **bony fractures** and significant dislocations but offer limited information about soft tissues, such as the spinal cord, ligaments, or intervertebral discs.
- They cannot adequately visualize the spinal cord damage responsible for the patient's specific neurological deficits, making it insufficient for confirming the cause of central cord syndrome.
*CT of the cervical spine with contrast*
- **CT scans** excel at visualizing **bony structures** and acute fractures, but even with contrast, they provide less detail of the **spinal cord parenchyma** and soft tissue ligaments compared to MRI.
- **Contrast** is typically used to highlight vascular structures, inflammatory processes, or tumors, which are not the primary diagnostic concerns suggested by this patient's acute post-traumatic presentation of central cord syndrome.
*Cervical myelography*
- **Myelography** involves injecting contrast into the subarachnoid space, followed by X-ray or CT imaging, to outline the spinal cord and nerve roots.
- While it can identify **spinal cord compression**, it is an **invasive procedure** with risks (e.g., headache, seizures) and has largely been replaced by the non-invasive and superior soft tissue imaging capabilities of MRI, especially in acute trauma.
More Contrast studies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.