Immunohistochemistry US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Immunohistochemistry. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Immunohistochemistry US Medical PG Question 1: A 43-year-old man comes to the physician because of weight loss and swelling on the left side of his neck. Physical examination shows a firm, enlarged left upper cervical lymph node that is immobile. Immunohistochemical testing performed on a biopsy specimen from the lymph node stains positive for cytokeratin. Which of the following is the most likely site of the primary neoplasm in this patient?
- A. Nerve sheath
- B. Bone
- C. Muscle
- D. Skin
- E. Nasopharynx (Correct Answer)
Immunohistochemistry Explanation: ***Nasopharynx***
- A **firm, enlarged, immobile cervical lymph node** in the upper neck (Level II) with **cytokeratin positivity** indicates metastatic carcinoma of epithelial origin.
- **Nasopharyngeal carcinoma** classically presents with **cervical lymphadenopathy as the initial manifestation** in up to 90% of cases, often before other symptoms develop.
- The **left upper cervical location** is characteristic of nasopharyngeal primary tumors, which have a strong predilection for Level II nodal metastasis.
- **Weight loss** suggests systemic disease consistent with advanced carcinoma.
- Nasopharyngeal carcinoma is **cytokeratin-positive** (epithelial origin) and frequently presents with isolated neck mass **without nasal symptoms** in early stages.
*Skin*
- While cutaneous squamous cell carcinoma can metastasize to cervical nodes, it would require a **visible primary skin lesion** on the head, neck, or scalp, which would be evident on physical examination.
- Skin primaries more commonly metastasize to **posterior cervical nodes (Level V)** from scalp lesions, not upper anterior cervical nodes.
- This presentation is **far less common** than mucosal head and neck primaries for isolated cervical metastasis.
*Nerve sheath*
- Nerve sheath tumors such as **schwannomas** or **neurofibromas** are of mesenchymal origin and stain positive for **S-100 protein**, not cytokeratin.
- These tumors are typically **benign and mobile**, not firm and immobile like metastatic carcinoma.
*Bone*
- Primary bone tumors (e.g., osteosarcoma) do not express **cytokeratin** and would not present with isolated cervical lymphadenopathy.
- Bone tumors would show characteristic imaging findings and typically metastasize to lungs, not regional lymph nodes.
*Muscle*
- Muscle-derived tumors such as **rhabdomyosarcoma** or **leiomyosarcoma** are mesenchymal in origin.
- These tumors stain positive for **desmin** and **actin**, not cytokeratin, which is specific to epithelial cells.
Immunohistochemistry US Medical PG Question 2: An investigator is studying the effect of different cytokines on the growth and differentiation of B cells. The investigator isolates a population of B cells from the germinal center of a lymph node. After exposure to a particular cytokine, these B cells begin to produce an antibody that prevents attachment of pathogens to mucous membranes but does not fix complement. Which of the following cytokines is most likely responsible for the observed changes in B-cell function?
- A. Interleukin-5 (Correct Answer)
- B. Interleukin-6
- C. Interleukin-8
- D. Interleukin-2
- E. Interleukin-4
Immunohistochemistry Explanation: ***Interleukin-5***
- The antibody described (prevents pathogen attachment to mucous membranes, does not fix complement) is characteristic of **IgA**.
- **IL-5** plays a crucial role in promoting **IgA secretion** by differentiated B cells and supports B cell growth and differentiation in mucosal immunity.
- IL-5 works synergistically with **TGF-β** (the primary cytokine for IgA class switching) to enhance IgA production, particularly in mucosal-associated lymphoid tissue.
- Among the options provided, **IL-5 has the strongest association with IgA production**.
*Interleukin-4*
- **IL-4** is the primary cytokine driving class switching to **IgE** (and IgG4), not IgA.
- IL-4 is central to **allergic responses** and type 2 immunity, promoting B cells to produce IgE antibodies against allergens and parasites.
- It does not play a significant role in IgA production or mucosal immunity.
*Interleukin-6*
- **IL-6** is a pleiotropic cytokine involved in acute phase reactions, inflammation, and promoting B cell **differentiation into plasma cells**.
- While it supports general B cell maturation and antibody secretion, it is not specifically associated with **IgA production** or class switching.
*Interleukin-8*
- **IL-8** (CXCL8) is a **chemokine** that primarily recruits and activates neutrophils during inflammation.
- It has no direct role in B cell class switching or antibody production.
*Interleukin-2*
- **IL-2** is essential for T cell proliferation and differentiation, enhancing **cell-mediated immunity**.
- While it can indirectly affect B cell responses through T cell help, it is not directly responsible for promoting **IgA production** or class switching.
Immunohistochemistry US Medical PG Question 3: Fluorescein is an artificial dark orange colored organic molecule used in the diagnosis of corneal ulcers and herpetic corneal infections. It is observed that, in experimental animals, the fluorescein binds to receptors on certain B cells, but it does not stimulate them to produce fluorescein specific antibodies unless it is first attached to a larger molecule such as albumin. Which of the following terms best describes fluorescein?
- A. Tolerogen
- B. Hapten (Correct Answer)
- C. Immunogen
- D. Carrier
- E. Adjuvant
Immunohistochemistry Explanation: ***Hapten***
- A **hapten** is a small molecule that can bind to B cell receptors and be recognized by antibodies but **cannot by itself induce an immune response**.
- For a hapten to become immunogenic (stimulate antibody production), it must be **covalently linked to a larger carrier molecule**, such as a protein like albumin, which provides the necessary T cell help.
*Tolerogen*
- A **tolerogen** is an antigen that, under specific circumstances, **induces immune unresponsiveness (tolerance)** rather than an immune response.
- This typically involves rendering lymphocytes anergic or causing their deletion, preventing future responses to that specific antigen.
*Immunogen*
- An **immunogen** is any substance that is capable of **eliciting a humoral or cell-mediated immune response** on its own.
- These molecules are typically large and complex enough to be recognized by the immune system and drive antibody production or T cell activation without requiring a carrier molecule.
*Carrier*
- A **carrier protein** is a large molecule to which a hapten is conjugated to make it **immunogenic**.
- In this scenario, albumin serves as the carrier molecule, but fluorescein itself is not the carrier; it is the molecule requiring the carrier for immunogenicity.
*Adjuvant*
- An **adjuvant** is a substance that **enhances the immune response to an antigen** when administered together, but it is not itself specifically targeted by the immune response.
- Adjuvants work by mechanisms such as prolonging antigen presentation, enhancing co-stimulatory signals, or inducing local inflammation, rather than being the immunogenic component itself.
Immunohistochemistry US Medical PG Question 4: A 45-year-old immigrant presents with unintentional weight loss, sleep hyperhidrosis, and a persistent cough. He says these symptoms have been present for quite some time. Upon imaging, many granulomas in the upper lobes are present. It is noted that these apical granulomas have centers of necrosis that appear cheese-like in appearance. Encircling the area of necrosis are large cells with cytoplasms pale in color. Of the following surface markers, which one is most closely associated with these cells?
- A. CD20
- B. CD3
- C. CD4
- D. CD14 (Correct Answer)
- E. CD8
Immunohistochemistry Explanation: ***CD14***
- The description of **caseating granulomas** in the upper lobes with large cells having pale cytoplasm points towards **tuberculosis** and the presence of **epithelioid macrophages**.
- **CD14** is a surface marker commonly found on **monocytes** and **macrophages**, making it the most appropriate choice among the given options.
- Note: While epithelioid macrophages (the activated form seen in granulomas) may downregulate CD14 compared to circulating monocytes, CD14 remains the most closely associated macrophage marker among these choices. **CD68** would be the ideal marker for tissue macrophages, but it is not listed.
*CD20*
- **CD20** is a surface marker characteristic of **B lymphocytes**.
- While B cells might be present in inflammatory lesions, they are not the predominant cell type described as "large cells with pale cytoplasm" forming the granuloma.
*CD3*
- **CD3** is a pan T-cell marker, indicating the presence of all types of **T lymphocytes**.
- While T cells (specifically CD4+ T helper cells) are crucial in granuloma formation, the "large cells with pale cytoplasm" encasing the necrosis specifically refer to epithelioid macrophages, not T cells.
*CD4*
- **CD4** is a surface marker for **helper T lymphocytes**.
- **CD4+ T cells** play a critical role in orchestrating the immune response and granuloma formation in tuberculosis through IFN-γ secretion, but the description of the large cells with pale cytoplasm refers to macrophages, not lymphocytes.
*CD8*
- **CD8** is a surface marker for **cytotoxic T lymphocytes**.
- **CD8+ T cells** are also involved in the immune response to mycobacterial infection but are not the primary cell type described as forming the bulk of the granuloma's characteristic "large cells with pale cytoplasm."
Immunohistochemistry US Medical PG Question 5: What is the primary stimulus for erythropoietin production?
- A. Increased temperature
- B. Decreased blood pressure
- C. Decreased plasma proteins
- D. Tissue hypoxia (Correct Answer)
Immunohistochemistry Explanation: ***Tissue hypoxia***
- Erythropoietin (EPO) production is primarily stimulated by sensing **low oxygen levels** in the kidneys.
- This response is crucial for maintaining adequate oxygen delivery to tissues by increasing **red blood cell mass**.
*Increased temperature*
- An increase in body temperature is a stimulus for processes like **sweating** and **vasodilation**, to regulate body temperature.
- It does not directly affect erythropoietin production or red blood cell synthesis.
*Decreased blood pressure*
- A decrease in blood pressure primarily stimulates the **renin-angiotensin-aldosterone system** and the release of **ADH** to regulate blood volume and pressure.
- It does not directly cause an increase in erythropoietin release as its primary function is not related to oxygen sensing.
*Decreased plasma proteins*
- A decrease in plasma proteins primarily affects **oncotic pressure** and can lead to edema.
- It is not a direct stimulus for erythropoietin production.
Immunohistochemistry US Medical PG Question 6: During an experiment, the immunophenotypes of different cells in a sample are determined. The cells are labeled with fluorescent antibodies specific to surface proteins, and a laser is then focused on the samples. The intensity of fluorescence created by the laser beam is then plotted on a scatter plot. The result shows most of the cells in the sample to be positive for CD8 surface protein. Which of the following cell types is most likely represented in this sample?
- A. Mature cytotoxic T lymphocytes (Correct Answer)
- B. Activated regulatory T lymphocytes
- C. Inactive B lymphocytes
- D. Dendritic cells
- E. Mature helper T lymphocytes
Immunohistochemistry Explanation: ***Mature cytotoxic T lymphocytes***
- **CD8** is a characteristic surface marker for **cytotoxic T lymphocytes**, indicating their immune function in directly killing infected or cancerous cells.
- The "mature" designation implies they have fully developed and are ready to exert their effector functions.
*Activated regulatory T lymphocytes*
- **Regulatory T lymphocytes** are typically identified by the expression of **CD4** and **CD25**, along with the intracellular transcription factor **FOXP3**, not CD8.
- Their primary role is immune suppression, not direct cytotoxicity.
*Inactive B lymphocytes*
- **B lymphocytes** are characterized by the expression of **CD19**, **CD20**, and surface immunoglobulins, which are distinct from the CD8 marker.
- Their main function is antibody production.
*Dendritic cells*
- **Dendritic cells** are primarily **antigen-presenting cells** and are identified by markers such as **CD11c** and **MHC class II molecules**, not CD8.
- While some rare subsets of dendritic cells can express CD8α, it is not their predominant or defining marker.
*Mature helper T lymphocytes*
- **Helper T lymphocytes** are defined by the expression of **CD4** and play a crucial role in coordinating the immune response.
- They do not express CD8, which is characteristic of cytotoxic T cells.
Immunohistochemistry US Medical PG Question 7: An investigator studying targeted therapy in patients with gastrointestinal stromal tumors requires a reliable test to determine the spatial distribution of CD117-positive cells in biopsy specimens. Which of the following is the most appropriate test?
- A. Northern blot
- B. Immunohistochemistry (Correct Answer)
- C. Flow cytometry
- D. Fluorescence in-situ hybridization
- E. Western blot
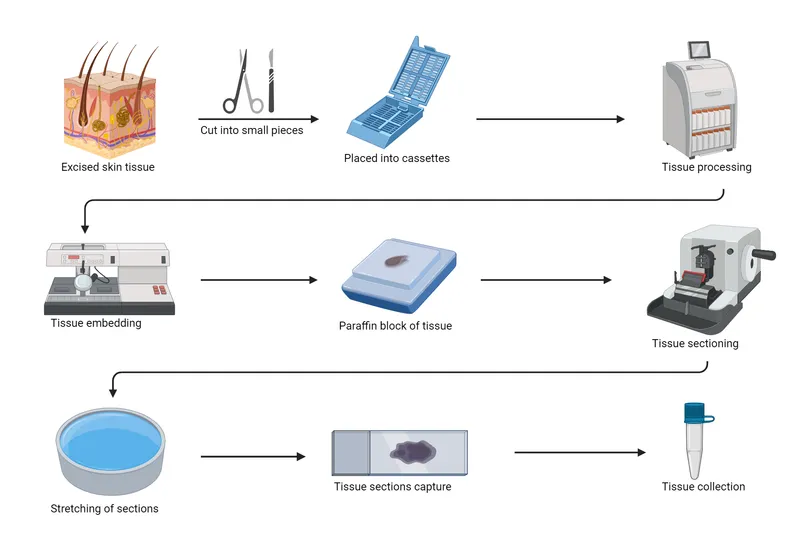
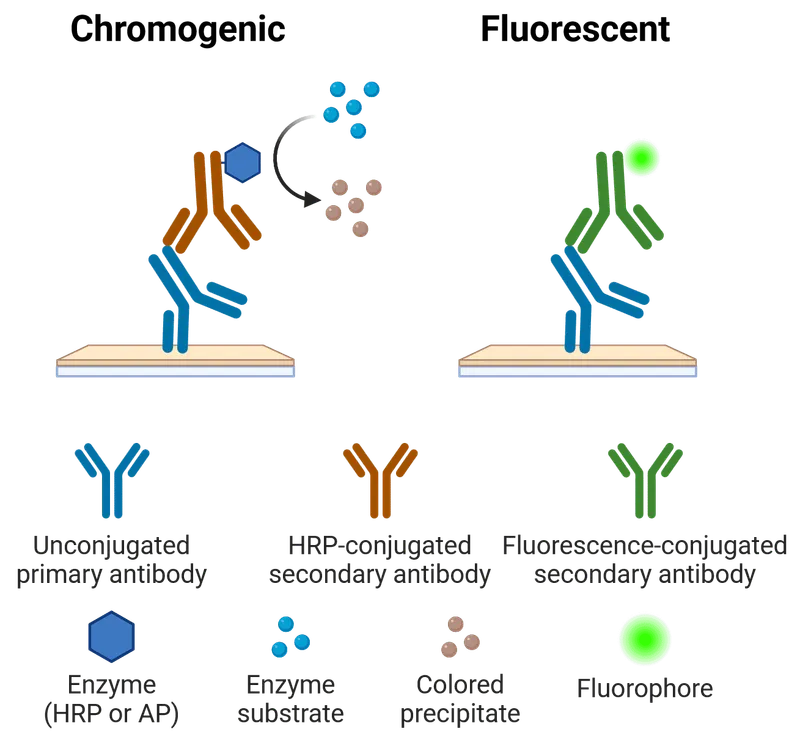
Immunohistochemistry Explanation: ***Immunohistochemistry***
- **Immunohistochemistry (IHC)** uses **antibodies** to target specific antigens (like **CD117**) within tissue sections, allowing for **visualization of their spatial distribution** under a microscope.
- This technique is ideal for identifying the precise location and quantity of **CD117-positive cells** within a biopsy, which is crucial for assessing targeted therapy in gastrointestinal stromal tumors.
*Northern blot*
- **Northern blot** is used to detect and quantify specific **RNA** sequences in a sample.
- It does not provide information about **protein expression** or the **spatial distribution of cells** within tissue.
*Flow cytometry*
- **Flow cytometry** is used for analyzing and sorting cells based on their **surface or intracellular markers** by passing them in a fluid stream through laser light.
- While it can quantify **CD117-positive cells**, it requires cells to be in suspension and thus **destroys the tissue architecture**, preventing analysis of spatial distribution.
*Fluorescence in-situ hybridization*
- **Fluorescence in-situ hybridization (FISH)** uses **fluorescent probes** to detect and locate specific **DNA or RNA sequences** on chromosomes or in cells.
- FISH is primarily used for genetic analysis and **does not directly assess protein expression** or cellular distribution in the context of targeted therapy.
*Western blot*
- **Western blot** is used to detect and quantify specific **proteins** from a sample by separating them by size, but it is performed on **tissue homogenates**.
- This technique provides information on the **total protein content** but **does not preserve the spatial arrangement** of cells within the original tissue.
Immunohistochemistry US Medical PG Question 8: A 7-month old boy, born to immigrant parents from Greece, presents to the hospital with pallor and abdominal distention. His parents note that they recently moved into an old apartment building and have been concerned about their son's exposure to chipped paint from the walls. On physical exam, the patient is found to have hepatosplenomegaly and frontal skull bossing. Hemoglobin electrophoresis reveals markedly increased HbF and HbA2 levels. What would be the most likely findings on a peripheral blood smear?
- A. Microcytosis and hypochromasia of erythrocytes (Correct Answer)
- B. Sickling of erythrocytes
- C. Basophilic stippling of erythrocytes
- D. Macrocytosis of erythrocytes with hypersegmented neutrophils
- E. Schistocytes and normocytic erythrocytes
Immunohistochemistry Explanation: ### ***Microcytosis and hypochromasia of erythrocytes***
- This patient presents with **β-thalassemia major**, as evidenced by **Greek ancestry** (Mediterranean population at high risk), **markedly elevated HbF and HbA2 levels** on hemoglobin electrophoresis, **frontal skull bossing** from bone marrow expansion, and **hepatosplenomegaly** from extramedullary hematopoiesis.
- The peripheral blood smear in β-thalassemia major characteristically shows **severe microcytic, hypochromic anemia** with target cells, nucleated RBCs, and marked anisocytosis and poikilocytosis.
- The inadequate β-globin chain production leads to ineffective erythropoiesis and severe hemolysis, resulting in the microcytic, hypochromic pattern.
### *Basophilic stippling of erythrocytes*
- While **basophilic stippling** can be seen in β-thalassemia, it is not the **most characteristic** finding and is more commonly associated with **lead poisoning**.
- The chipped paint exposure in this case is a distractor; **lead poisoning does NOT cause elevated HbF/HbA2, frontal bossing, or this degree of organomegaly** in a 7-month-old.
- The hemoglobin electrophoresis findings definitively point to thalassemia, not lead toxicity.
### *Sickling of erythrocytes*
- **Sickling** is pathognomonic for **sickle cell disease**, which presents with elevated HbS (not HbF and HbA2) on electrophoresis.
- While both are hemoglobinopathies affecting Mediterranean populations, the electrophoresis pattern and clinical features clearly indicate thalassemia, not sickle cell disease.
### *Schistocytes and normocytic erythrocytes*
- **Schistocytes** indicate **microangiopathic hemolytic anemia** (e.g., TTP, HUS, DIC), which involves mechanical RBC fragmentation in damaged microvasculature.
- The patient's chronic presentation, organomegaly, skeletal changes, and hemoglobin electrophoresis findings are inconsistent with microangiopathic hemolysis.
### *Macrocytosis of erythrocytes with hypersegmented neutrophils*
- **Macrocytic anemia with hypersegmented neutrophils** is characteristic of **megaloblastic anemia** from vitamin B12 or folate deficiency.
- β-thalassemia causes **microcytic** anemia due to deficient hemoglobin synthesis, not macrocytic anemia from impaired DNA synthesis.
Immunohistochemistry US Medical PG Question 9: A 52-year-old woman sees you in your office with a complaint of new-onset headaches over the past few weeks. On exam, you find a 2 x 2 cm dark, irregularly shaped, pigmented lesion on her back. She is concerned because her father recently passed away from skin cancer. What tissue type most directly gives rise to the lesion this patient is experiencing?
- A. Neural crest cells (Correct Answer)
- B. Endoderm
- C. Mesoderm
- D. Ectoderm
- E. Neuroectoderm
Immunohistochemistry Explanation: ***Neural crest cells***
- The suspected lesion, given its description and the patient's family history of skin cancer, is likely a **melanoma**.
- Melanoma originates from **melanocytes**, which are derived from **neural crest cells** during embryonic development.
*Endoderm*
- The endoderm gives rise to the **lining of the gastrointestinal and respiratory tracts**, as well as organs such as the liver and pancreas.
- It is not involved in the formation of melanocytes or skin lesions like melanoma.
*Mesoderm*
- The mesoderm forms tissues such as **muscle, bone, cartilage, connective tissue**, and the circulatory system.
- It does not directly give rise to melanocytes, which are the cells of origin for melanoma.
*Ectoderm*
- The ectoderm gives rise to the **epidermis, nervous system**, and sensory organs.
- While melanocytes are found in the epidermis, they are specifically derived from the **neural crest (a sub-population of ectoderm)**, not the general ectoderm.
*Neuroectoderm*
- Neuroectoderm specifically refers to the ectoderm that develops into the **nervous system**.
- While neural crest cells originate from the neuroectoderm, "neural crest cells" is a more precise answer for the origin of melanocytes.
Immunohistochemistry US Medical PG Question 10: This type of epithelium is most commonly seen in which of the following organs?
- A. Ureter
- B. Trachea (Correct Answer)
- C. Duodenum
- D. Gall bladder
- E. Esophagus
Immunohistochemistry Explanation: ***Trachea***
- The image displays **pseudostratified columnar epithelium with cilia and goblet cells**, which is characteristic of the respiratory tract, including the trachea.
- This specialized epithelium functions to trap and expel foreign particles from the airways, ensuring respiratory health.
*Ureter*
- The ureter is lined by **transitional epithelium** (urothelium), which is characterized by its ability to stretch.
- This epithelium would show a cuboidal to columnar appearance when relaxed and a flattened appearance when stretched, and the cells on the surface are typically dome-shaped, unlike the image.
*Duodenum*
- The duodenum is lined by **simple columnar epithelium** with a brush border and numerous goblet cells for absorption and mucus secretion.
- It also features **villi and crypts of Lieberkühn**, which are not seen in the provided image.
*Gall bladder*
- The gallbladder is lined by **simple columnar epithelium** with microvilli, specialized for water absorption.
- It lacks the cilia and pseudostratified arrangement evident in the given histopathology slide.
*Esophagus*
- The esophagus is lined by **non-keratinized stratified squamous epithelium**, designed to protect against abrasion from food passage.
- This epithelium appears as multiple layers of flattened cells, completely different from the tall, columnar, ciliated cells shown in the image.
More Immunohistochemistry US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.