Histopathological changes in common diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Histopathological changes in common diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Histopathological changes in common diseases US Medical PG Question 1: A 78-year-old man dies suddenly from complications of acute kidney failure. An autopsy is performed and microscopic evaluation of the kidneys shows pale, swollen cells in the proximal convoluted tubules. Microscopic evaluation of the liver shows similar findings. Which of the following is the most likely underlying mechanism of these findings?
- A. Double-stranded DNA breakage
- B. Impaired Na+/K+-ATPase pump activity (Correct Answer)
- C. Free radical formation
- D. Cytochrome C release
- E. Cytoplasmic triglyceride accumulation
Histopathological changes in common diseases Explanation: ***Impaired Na+/K+-ATPase pump activity***
- **Acute kidney failure** leads to **hypoxia** and ATP depletion, which impairs the function of the **Na+/K+-ATPase pump** on the cell membrane.
- Failure of this pump results in **intracellular accumulation of sodium** and water, causing **cellular swelling** and pallor as seen in the kidneys and liver.
*Double-stranded DNA breakage*
- This is primarily associated with **apoptosis** or **radiation injury**, which would lead to nuclear fragmentation and cellular death rather than simple cellular swelling.
- While cell death can occur in acute kidney failure, the initial changes described (pale, swollen cells) are characteristic of **reversible cell injury** before extensive DNA damage.
*Free radical formation*
- **Free radical formation** (oxidative stress) can cause cellular injury, but it primarily leads to **lipid peroxidation of membranes** and damage to proteins and DNA, not directly to the widespread intracellular water accumulation described.
- While part of the injury cascade, it's not the most direct mechanism for the initial gross and microscopic findings of swelling.
*Cytochrome C release*
- **Cytochrome C release** from mitochondria is a critical step in the **intrinsic pathway of apoptosis**, leading to programmed cell death.
- The findings described (pale, swollen cells) are more indicative of **reversible cellular injury** or early necrosis, prior to the widespread activation of apoptosis.
*Cytoplasmic triglyceride accumulation*
- **Cytoplasmic triglyceride accumulation** (steatosis or fatty change) is often seen in conditions like **alcoholic liver disease** or **metabolic syndrome**.
- While it can be a sign of cellular injury, it does not directly explain the generalized "pale, swollen cells" observed in both the kidneys and liver following acute kidney failure, which points to water influx.
Histopathological changes in common diseases US Medical PG Question 2: A previously healthy 82-year-old man dies in a motor vehicle collision. At autopsy, the heart shows slight ventricular thickening. There are abnormal, insoluble aggregations of protein filaments in beta-pleated linear sheets in the ventricular walls and, to a lesser degree, in the atria and lungs. No other organs show this abnormality. Bone marrow examination shows no plasma cell dyscrasia. The abnormal protein aggregations are most likely composed of which of the following?
- A. Immunoglobulin light chain
- B. Normal transthyretin (Correct Answer)
- C. β-amyloid peptide
- D. Natriuretic peptide
- E. Serum amyloid A
Histopathological changes in common diseases Explanation: ***Normal transthyretin***
- The patient's age and the localization of the amyloid deposits primarily in the **heart (ventricular walls and atria)**, along with normal bone marrow and the absence of systemic involvement, are highly characteristic of **senile systemic amyloidosis** which is caused by wild-type (normal) transthyretin.
- **Transthyretin** is a transport protein for thyroid hormones and retinol; with aging, it can misfold and deposit as amyloid fibrils, particularly in the heart.
*Immunoglobulin light chain*
- This typically causes **primary amyloidosis (AL amyloidosis)**, which is associated with a **plasma cell dyscrasia** and multiorgan involvement, neither of which are present in this case.
- AL amyloidosis often affects the kidneys, liver, and nerves, in addition to the heart, which is not described here.
*β-amyloid peptide*
- This protein forms plaques primarily in the **brain** in **Alzheimer's disease** and cerebral amyloid angiopathy, not typically causing significant cardiac amyloidosis.
- While it can be found in some vascular structures, its primary association is with neurodegenerative disease.
*Natriuretic peptide*
- **Natriuretic peptides (ANP, BNP)** are hormones involved in cardiovascular homeostasis and do not form amyloid deposits.
- They are markers of heart failure, not the causative agents of amyloidosis.
*Serum amyloid A*
- This protein is associated with **secondary amyloidosis (AA amyloidosis)**, which develops as a complication of chronic inflammatory diseases or infections.
- The patient's history does not mention any such underlying conditions, and the deposition pattern is not typical for AA amyloidosis.
Histopathological changes in common diseases US Medical PG Question 3: A 74-year-old man presents with complaints of sudden severe crushing retrosternal pain. The pain radiated to his left arm shortly after it began, and he was subsequently rushed to the emergency department for evaluation. His troponins and creatine kinase-MB (CK-MB) were elevated. Unfortunately, the patient died within the next 2 hours and an autopsy was performed immediately. The gross examination of the heart will show?
- A. White, patchy, non-contractile scar
- B. Normal heart tissue (Correct Answer)
- C. Pallor of the infarcted tissue
- D. Abundant neutrophils
- E. Red granulation tissue surrounding the infarction
Histopathological changes in common diseases Explanation: ***Normal heart tissue***
- At **0-4 hours** following a myocardial infarction, the heart muscle shows **no gross changes** on autopsy examination.
- Although **coagulative necrosis** begins at the cellular level within minutes, these microscopic changes are **not visible** to the naked eye during gross examination.
- The patient died within **2 hours** of symptom onset, which falls within this early window where the heart appears **grossly normal** despite the acute infarction.
- Elevated **cardiac enzymes** (troponins, CK-MB) confirm myocardial injury has occurred, but gross pathological changes lag behind biochemical and microscopic changes.
*Pallor of the infarcted tissue*
- **Pallor** (pale discoloration) of infarcted myocardium typically becomes visible on gross examination at **4-12 hours** post-infarction.
- At 2 hours, this change has not yet developed sufficiently to be visible on gross inspection.
- Pallor results from **edema** and the accumulation of dead cells, which takes several hours to manifest grossly.
*White, patchy, non-contractile scar*
- A **white fibrotic scar** is characteristic of a **healed myocardial infarction**, which takes **several weeks to months** to form.
- This represents complete replacement of necrotic tissue by **collagenous scar tissue** (fibrosis).
- This is a chronic finding, not an acute one.
*Abundant neutrophils*
- **Neutrophil infiltration** is a microscopic finding that typically begins around **12-24 hours** after infarction, becoming abundant over the following days.
- Even when present, neutrophils are not visible on **gross examination**—they require microscopic evaluation.
- At 2 hours post-infarction, neutrophils have not yet migrated to the infarcted area.
*Red granulation tissue surrounding the infarction*
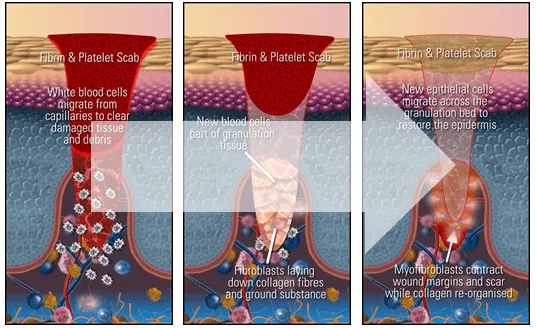
- **Granulation tissue** formation begins around **3-7 days** after infarction and involves proliferation of **capillaries** and **fibroblasts**.
- Grossly, this appears as a **hyperemic border** with central yellow softening.
- This represents the healing phase and would not be present within 2 hours of symptom onset.
Histopathological changes in common diseases US Medical PG Question 4: An 80-year-old woman is brought to the physician by her 2 daughters for worsening memory loss. They report that their mother is increasingly forgetful about recent conversations and events. She is unable to remember her appointments and commitments she has made. 3 years ago, the patient was moved into an elder care facility because she was often getting lost on her way home and forgetting to take her medications. The patient reports that she is very socially active at her new home and has long conversations with the other residents about her adventures as an air hostess during her youth. Which of the following cerebral pathologies is most likely present in this patient?
- A. Lewy bodies
- B. Lacunar infarcts
- C. Intracytoplasmic vacuoles
- D. Neurofibrillary tangles (Correct Answer)
- E. Demyelination
Histopathological changes in common diseases Explanation: ***Neurofibrillary tangles***
- The patient's presentation with **progressive memory loss** affecting recent events, getting lost, and forgetting medications, while largely preserving long-term memory (recalling youth as an air hostess and engaging in conversations), is highly characteristic of **Alzheimer's disease**.
- **Neurofibrillary tangles**, composed of hyperphosphorylated tau protein, along with **amyloid plaques**, are the hallmark pathological findings in Alzheimer's disease.
*Lewy bodies*
- **Lewy bodies** are characteristic of **Lewy body dementia** or Parkinson's disease with dementia, which typically present with prominent **fluctuations in cognition**, recurrent **visual hallucinations**, and parkinsonism.
- While memory loss can occur, the dominant features in this case point away from Lewy body pathology.
*Lacunar infarcts*
- **Lacunar infarcts** are associated with **vascular dementia**, which often presents with a more **step-wise decline** in cognitive function, focal neurological deficits, and evidence of cerebrovascular disease on imaging.
- The patient's gradual and progressive memory loss is less typical of lacunar infarcts as the primary cause.
*Intracytoplasmic vacuoles*
- **Intracytoplasmic vacuoles** are characteristic of **Creutzfeldt-Jakob disease** (spongiform encephalopathy), which is a rapidly progressive and fatal neurodegenerative disorder with distinct neurological symptoms such as myoclonus and ataxia, not fitting this patient's profile.
- The disease course is typically much faster than the 3-year progression described.
*Demyelination*
- **Demyelination** is the hallmark of conditions like **multiple sclerosis**, which primarily affects younger individuals and typically presents with a range of neurological deficits, including motor, sensory, and visual disturbances, that often relapse and remit.
- It does not typically present as a primary, progressive memory disorder in an 80-year-old in this manner.
Histopathological changes in common diseases US Medical PG Question 5: A 72-year-old female is brought to the emergency department by ambulance because she was unable to walk. She says that she cut her leg while falling about a week ago. Since then, the wound has started draining fluid and become progressively more painful. She is found to have necrotizing fasciitis and is taken emergently to the operating room. Histological examination of cells along the fascial planes reveal cells undergoing necrosis. Which of the following represents the earliest sign that a cell has progressed to irreversible damage in this patient?
- A. Fragmentation of the nucleus
- B. Membrane blebbing from organelles
- C. Chromatin dissolution and disappearance
- D. Ribosomal detachment from the endoplasmic reticulum
- E. Condensation of DNA into a basophilic mass (Correct Answer)
Histopathological changes in common diseases Explanation: ***Condensation of DNA into a basophilic mass***
- **Karyopyknosis**, or the **condensation of nuclear chromatin into a dense, shrunken mass**, is an early microscopic sign of irreversible cell injury leading to necrosis. It indicates the cell has committed to a death pathway.
- This nuclear change is characterized by the nucleus appearing as a **small, dense, and deeply basophilic structure** due to chromatin clumping.
*Fragmentation of the nucleus*
- **Karyorrhexis**, the fragmentation of the pyknotic nucleus, occurs *after* karyopyknosis, indicating a later stage of irreversible injury.
- This process involves the breakdown of the condensed nuclear fragments, leading to their subsequent disappearance.
*Membrane blebbing from organelles*
- **Membrane blebbing** can occur in both reversible and irreversible injury, but its presence on *organelles* specifically doesn't necessarily represent the *earliest* sign of irreversible damage compared to nuclear changes.
- While significant blebbing points towards severe damage, **nuclear changes** are often considered more definitive early markers of irreversible commitment.
*Chromatin dissolution and disappearance*
- **Karyolysis**, the dissolution and fading of the nucleus due to enzymatic degradation, represents a *later* stage of irreversible injury, occurring after karyopyknosis and karyorrhexis.
- In this stage, the nucleus eventually completely disappears, leaving only an anucleated ghost cell.
*Ribosomal detachment from the endoplasmic reticulum*
- **Ribosomal detachment** from the endoplasmic reticulum is an early sign of **reversible cell injury**, leading to decreased protein synthesis.
- It indicates initial cellular stress but not necessarily a commitment to irreversible damage or necrosis.
Histopathological changes in common diseases US Medical PG Question 6: A 78-year-old man with a history of myocardial infarction status post coronary artery bypass grafting and a 60-pack-year history of smoking is found deceased in his apartment after not returning calls to his family for the last 2 days. The man was last known to be alive 3 days ago, when his neighbor saw him getting his mail. The family requests an autopsy. On autopsy, the man is found to have a 100% blockage of his left anterior descending artery of his heart and likely passed from sudden cardiac death 2 days prior. Which of the following findings is expected to be found on histologic examination of his damaged myocardium?
- A. Fat saponification
- B. Cellular debris and lymphocytes
- C. Cystic cavitation
- D. Cellular debris and macrophages
- E. Uniform binding of acidophilic dyes (Correct Answer)
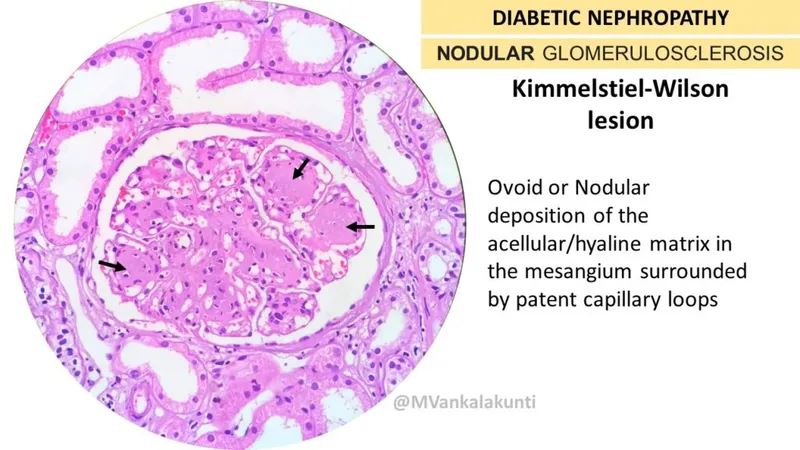
Histopathological changes in common diseases Explanation: ***Uniform binding of acidophilic dyes***
- This finding, often described as **coagulative necrosis**, is characteristic of myocardial infarction 1-3 days after onset, as enzymes denature and bind to eosin more uniformly.
- The patient was found deceased 2 days after his suspected death, placing the myocardial changes within this timeframe.
*Fat saponification*
- **Fat saponification** is a type of fat necrosis, typically seen in the pancreas or breast, resulting from the enzymatic destruction of fat cells.
- It does not occur in the myocardium following an ischemic event.
*Cellular debris and lymphocytes*
- **Lymphocytes** are generally not the predominant inflammatory cells in the initial stages of a myocardial infarction.
- While cellular debris would be present, the primary inflammatory infiltrate in the first 3 days after an MI is typically **neutrophils**, not lymphocytes.
*Cystic cavitation*
- **Cystic cavitation** is a characteristic feature of liquefactive necrosis, which occurs in the brain following an ischemic stroke, but not in the heart.
- The heart undergoes **coagulative necrosis** after an MI.
*Cellular debris and macrophages*
- **Macrophages** become prominent later in the healing process of a myocardial infarction, typically starting around **3-7 days** after the event.
- At the 2-day mark, the dominant cells would still be neutrophils and necrotic myocytes.
Histopathological changes in common diseases US Medical PG Question 7: A 31-year-old woman scrapes her finger on an exposed nail and sustains a minor laceration. Five minutes later, her finger is red, swollen, and painful. She has no past medical history and does not take any medications. She drinks socially with her friends and does not smoke. The inflammatory cell type most likely to be prominent in this patient's finger has which of the following characteristics?
- A. Segmented nuclei (Correct Answer)
- B. Dramatically expanded endoplasmic reticulum
- C. Large cell with amoeboid movement
- D. Multiple peripheral processes
- E. Dark histamine containing granules
Histopathological changes in common diseases Explanation: ***Segmented nuclei***
- This scenario describes **acute inflammation** following a minor injury, with classic signs of **redness, swelling, and pain** within minutes.
- **Neutrophils** are the primary inflammatory cells in acute inflammation and are characterized by their **segmented (multi-lobed) nuclei.**
*Dramatically expanded endoplasmic reticulum*
- An expanded endoplasmic reticulum is characteristic of cells highly active in protein synthesis and secretion, such as **plasma cells** producing antibodies.
- Plasma cells are typically involved in **chronic inflammation** and adaptive immune responses, not rapid acute inflammation.
*Large cell with amoeboid movement*
- This describes **macrophages**, which are phagocytic cells important in both acute and chronic inflammation, and in cleaning up debris.
- While macrophages are present, **neutrophils** are the predominant early responders in acute bacterial infections and tissue injury.
*Multiple peripheral processes*
- This description is characteristic of **dendritic cells**, which are antigen-presenting cells that initiate adaptive immune responses.
- Dendritic cells play a role in linking innate and adaptive immunity but are not the primary inflammatory cell type in the immediate acute response.
*Dark histamine containing granules*
- This description applies to **mast cells** and **basophils**, which release histamine and other mediators in allergic reactions and acute inflammation.
- While mast cells are involved in the immediate response by releasing mediators, **neutrophils** are the main cellular players migrating to the site of injury.
Histopathological changes in common diseases US Medical PG Question 8: A 48-year-old man has smoked approximately 3 packs of cigarettes per day for the past 12 years. Which of the following pathologic changes is most likely to occur in his bronchial epithelium?
- A. Metaplasia (Correct Answer)
- B. Hyperplasia
- C. Hypertrophy
- D. Dysplasia
- E. Atrophy
Histopathological changes in common diseases Explanation: ***Metaplasia***
- Chronic irritation from **cigarette smoking** can cause the **bronchial epithelium** to change from ciliated columnar to stratified squamous, a process known as **metaplasia**.
- This adaptation makes the tissue more resistant to injury but results in the loss of important protective functions like **mucociliary clearance**.
*Hyperplasia*
- **Hyperplasia** involves an increase in the number of cells in a tissue or organ, often in response to increased demand or chronic stimulation.
- While smoking can cause hyperplasia of goblet cells and mucous glands in the bronchi, the direct epithelial change in response to chronic irritation is more specifically **metaplasia**.
*Hypertrophy*
- **Hypertrophy** is an increase in the size of individual cells, leading to an increase in the size of the organ or tissue.
- This is not the primary adaptive change seen in the bronchial epithelium in response to chronic smoking; instead, cells change their type.
*Dysplasia*
- **Dysplasia** refers to disorderly cell growth, often characterized by variations in cell size, shape, and organization; it is considered a precursor to cancer.
- While chronic smoking can eventually lead to dysplasia and then carcinoma, the initial and most common adaptive change in the bronchial epithelium is **metaplasia**.
*Atrophy*
- **Atrophy** is a decrease in cell size or number, leading to a reduction in the size of an organ or tissue, usually due to decreased workload, nutrition, or blood supply.
- This is not a typical response of the bronchial epithelium to chronic irritation from smoking, which tends to induce proliferative or adaptive changes.
Histopathological changes in common diseases US Medical PG Question 9: A 45-year-old man comes to his primary care provider for a routine visit. The patient mentions that while he was cooking 5 days ago, he accidentally cut himself with a meat cleaver and lost the skin at the tip of his finger. After applying pressure and ice, the bleeding stopped and he did not seek treatment. The patient is otherwise healthy and does not take any daily medications. The patient’s temperature is 98.2°F (36.8°C), blood pressure is 114/72 mmHg, pulse is 60/min, and respirations are 12/min. On exam, the patient demonstrates a 0.5 x 0.3 cm wound on the tip of his left third finger. No bone is involved, and the wound is red, soft, and painless. There are no signs of infection. Which of the following can be expected on histopathological examination of the wounded area?
- A. Platelet aggregates
- B. Epithelial cell migration from the wound borders
- C. Neutrophil migration into the wound
- D. Deposition of type III collagen (Correct Answer)
- E. Deposition of type I collagen
Histopathological changes in common diseases Explanation: ***Deposition of type III collagen***
- Five days post-injury, the **proliferative phase of wound healing** is active, characterized by the formation of an initial **granulation tissue** matrix primarily composed of **Type III collagen**.
- This type of collagen forms thinner, more flexible fibers that provide a temporary scaffold for tissue regeneration before being gradually replaced by stronger Type I collagen.
*Platelet aggregates*
- **Platelet aggregation** occurs immediately after injury as part of **hemostasis**, forming a plug to stop bleeding.
- By five days, this initial phase would have concluded, and the primary focus would be on tissue repair and regeneration.
*Epithelial cell migration from the wound borders*
- **Epithelial cell migration** for re-epithelialization typically occurs within the first 24-48 hours after injury, forming a new epidermal layer over the wound.
- While it continues, the dominant histological feature at day 5 in an open wound of this size would be **granulation tissue formation** in the dermis.
*Neutrophil migration into the wound*
- **Neutrophil migration** is a hallmark of the **inflammatory phase**, peaking within 24-48 hours post-injury to clear debris and microbes.
- By day 5, the inflammatory phase would be subsiding, and macrophages would be more prevalent, signaling the transition to the proliferative phase.
*Deposition of type I collagen*
- **Type I collagen** is the predominant collagen found in mature scar tissue and is deposited during the later **remodeling phase** of wound healing.
- While some Type I collagen may be present, **Type III collagen** is characteristic of the early granulation tissue prominent at day 5.
Histopathological changes in common diseases US Medical PG Question 10: A 10-year-old boy presents to your office with puffy eyes. The patient's mother states that his eyes seem abnormally puffy and thinks he may have an eye infection. Additionally, he had a sore throat a week ago which resolved with over the counter medications. The mother also thought that his urine was darker than usual and is concerned that blood may be present. His temperature is 99.5°F (37.5°C), blood pressure is 107/62 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for bilateral periorbital edema. Cranial nerves are grossly intact bilaterally. Which of the following is the most likely finding on renal biopsy for this patient?
- A. Sub-epithelial electron dense deposits on electron microscopy (Correct Answer)
- B. Linear Ig deposits along the basement membrane
- C. Podocyte fusion on electron microscopy
- D. Alternating thickening and thinning of basement membrane with splitting of the lamina densa
- E. No abnormalities
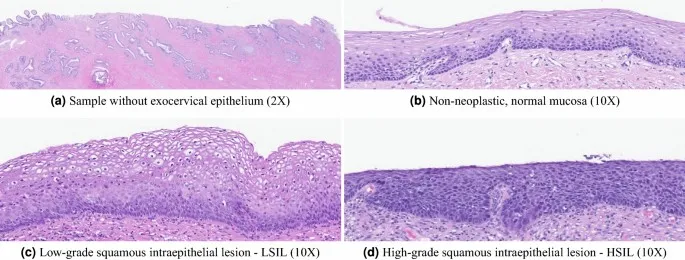
Histopathological changes in common diseases Explanation: ***Sub-epithelial electron dense deposits on electron microscopy***
- The patient's presentation with periorbital edema, dark urine (suggesting hematuria), and a recent history of pharyngitis strongly points towards **post-streptococcal glomerulonephritis (PSGN)**.
- Renal biopsy in PSGN characteristically shows **sub-epithelial humps** (electron-dense deposits) primarily composed of IgG and C3, which are best visualized on electron microscopy.
*Linear Ig deposits along the basement membrane*
- **Linear immunoglobulin G (IgG) deposits** along the glomerular basement membrane (GBM) are characteristic of **Goodpasture syndrome (anti-GBM disease)**.
- This condition presents with rapidly progressive glomerulonephritis and often pulmonary hemorrhage, which is not suggested by this patient's symptoms.
*Podocyte fusion on electron microscopy*
- **Podocyte effacement** (fusion of foot processes) is the hallmark finding in **minimal change disease**.
- Minimal change disease typically presents with **nephrotic syndrome** (heavy proteinuria, hypoalbuminemia, severe edema) without significant hematuria or a history of recent infection.
*Alternating thickening and thinning of basement membrane with splitting of the lamina densa*
- This description is characteristic of **Alport syndrome**, an inherited disorder affecting collagen IV.
- Alport syndrome presents with progressive hematuria, sensorineural hearing loss, and ocular abnormalities, which are not mentioned in this acute presentation.
*No abnormalities*
- Given the patient's clear symptoms of **nephritic syndrome** (edema, hematuria following infection), it is highly unlikely that a renal biopsy would show no abnormalities.
- A significant pathological process is indicated by the clinical picture.
More Histopathological changes in common diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.