Electron microscopy in histology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Electron microscopy in histology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Electron microscopy in histology US Medical PG Question 1: A scientist is studying the anatomy and function of bone growth. He is able to create a cell line of osteocytes with a mutation that prevents the osteocytes from exchanging nutrients and waste products within neighboring lamellae. This mutation most likely affected which of the following cell structures?
- A. Dynein
- B. Gap junctions (Correct Answer)
- C. Endoplasmic reticulum
- D. Plasma membrane
- E. Kinesin
Electron microscopy in histology Explanation: ***Gap junctions***
- **Gap junctions** are specialized intercellular connections that permit direct communication and exchange of small molecules and ions between adjacent cells.
- In osteocytes, **gap junctions** located in the **canaliculi** are crucial for the exchange of nutrients, waste, and signaling molecules within and between lamellae, allowing for synchronous activity and maintaining bone health.
- These connexin-based channels physically connect the cytoplasm of neighboring osteocytes embedded in bone matrix.
*Dynein*
- **Dynein** is a motor protein involved in intracellular transport towards the minus end of **microtubules**, playing a role in moving organelles and vesicles.
- It is not directly responsible for the intercellular exchange of nutrients and waste products between cells.
*Endoplasmic reticulum*
- The **endoplasmic reticulum** is an organelle involved in protein synthesis and lipid metabolism, playing a critical role in cellular function.
- It does not directly mediate the exchange of nutrients and waste products between adjacent cells.
*Plasma membrane*
- While **gap junctions** are embedded within the **plasma membrane**, the membrane itself does not facilitate direct cytoplasmic continuity between cells.
- The question specifically refers to structures that enable direct cell-to-cell exchange; the mutation affects the gap junction channels themselves (connexins), not the general plasma membrane structure.
- Without functional gap junctions, the plasma membrane alone cannot support the intercellular communication required for osteocyte networks.
*Kinesin*
- **Kinesin** is a motor protein that moves cargo along **microtubules** towards the plus end, involved in fundamental cellular processes like cell division and organelle transport.
- It is not involved in direct intercellular communication for nutrient and waste exchange but rather internal cellular trafficking.
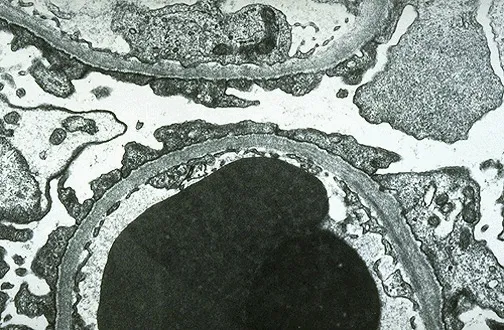
Electron microscopy in histology US Medical PG Question 2: A 42-year-old man presents to his primary care provider complaining of foamy urine for the last 2 weeks. He has also begun to notice swelling in his hands and feet, and he says that his shoes have not been fitting normally. On exam, the patient has a temperature of 98.8°F (37.1°C), blood pressure is 132/84 mmHg, pulse is 64/min, and respirations are 12/min. The patient has 2+ pitting edema bilaterally up to his shins. A 24-hour urine study is found to contain 9.0 g of protein. The patient is referred to a specialist and undergoes a renal biopsy. On light microscopy, the glomeruli demonstrate basement membrane thickening. On electron microscopy, subepithelial deposits are seen. Which of the following is a characteristic of this patient’s disease?
- A. X-linked condition
- B. Antibodies to alveolar basement membrane
- C. Loss of podocyte foot processes
- D. Antibodies to phospholipase A2 receptor (Correct Answer)
- E. IgA immune complex deposition
Electron microscopy in histology Explanation: ***Antibodies to phospholipase A2 receptor***
- The patient's presentation with **foamy urine**, **edema**, and **9.0 g of protein** in a 24-hour urine study indicates **nephrotic syndrome**. Renal biopsy findings of **glomerular basement membrane thickening** on light microscopy and **subepithelial deposits** on electron microscopy are characteristic of **membranous nephropathy**.
- Approximately 70-80% of primary membranous nephropathy cases are associated with **autoantibodies to the M-type phospholipase A2 receptor (PLA2R)**, a protein expressed on podocytes.
*X-linked condition*
- This description is characteristic of **Alport syndrome**, a genetic disorder leading to progressive kidney disease, hearing loss, and eye abnormalities.
- Alport syndrome presents with **hematuria** rather than significant proteinuria, and biopsy would show **laminar splitting of the glomerular basement membrane**.
*Antibodies to alveolar basement membrane*
- This describes **Goodpasture syndrome**, which is characterized by the presence of anti-glomerular basement membrane (anti-GBM) antibodies that target both the kidney and the lung.
- Patients typically present with rapidly progressive glomerulonephritis and pulmonary hemorrhage, and biopsy would show **linear IgG deposition** along the glomerular basement membrane on immunofluorescence.
*Loss of podocyte foot processes*
- This is a characteristic finding in **minimal change disease** and **focal segmental glomerulosclerosis (FSGS)**, two other causes of nephrotic syndrome.
- Minimal change disease typically shows normal glomeruli on light microscopy, while FSGS shows segmental sclerosis. Neither shows subepithelial deposits.
*IgA immune complex deposition*
- This is the hallmark of **IgA nephropathy (Berger's disease)** or **Henoch-Schönlein purpura** in children.
- Patients typically present with **hematuria**, often macroscopic, following an upper respiratory or gastrointestinal infection. Biopsy would show IgA deposits in the mesangium, not subepithelial deposits.
Electron microscopy in histology US Medical PG Question 3: An investigator is studying the interaction between epithelial cells and calcium ion concentration. When the calcium ion concentration available to a sample of epithelial tissue is decreased, an increased gap between adjacent epithelial cells is seen on electron microscopy. This observed decrease in cell adhesion is most likely due to an effect on which of the following proteins?
- A. Actin
- B. Integrin
- C. Cadherin (Correct Answer)
- D. Claudin
- E. Cytokeratin
Electron microscopy in histology Explanation: ***Cadherin***
- **Cadherins** are calcium-dependent adhesion proteins that mediate cell-to-cell adhesion, particularly in epithelial tissues.
- A decrease in calcium concentration would directly impair cadherin function, leading to reduced cell adhesion and increased intercellular gaps.
*Actin*
- **Actin** is a component of the cell's cytoskeleton, involved in cell shape, motility, and intracellular transport, but not directly responsible for calcium-dependent cell adhesion between epithelial cells.
- While actin filaments interact with adhesion junctions, their primary role is structural and dynamic rather than adhesive.
*Integrin*
- **Integrins** are primarily involved in cell-to-extracellular matrix adhesion, connecting the cell to the surrounding matrix, not directly mediating calcium-dependent cell-to-cell adhesion between epithelial cells.
- They can be affected by intracellular calcium signaling but do not directly bind calcium to mediate their adhesive function in the same way cadherins do.
*Claudin*
- **Claudins** are key components of **tight junctions**, which regulate paracellular permeability and form a barrier between cells, but they are not directly responsible for calcium-dependent cell-to-cell adhesion, which is characteristic of adherens junctions.
- While tight junctions contribute to overall cell-cell contact, the observation of an *increased gap* suggests an issue with adhesive complexes like adherens junctions, where cadherins are prominent.
*Cytokeratin*
- **Cytokeratins** are intermediate filaments found in epithelial cells, providing structural support and mechanical strength.
- They are linked to desmosomes and hemidesmosomes but are not directly involved in calcium-dependent cell-to-cell adhesion.
Electron microscopy in histology US Medical PG Question 4: A 59-year-old woman with a history of chronic kidney disease comes to the physician for a 3-month history of easy fatiguability. Physical examination shows subconjunctival pallor. Her hemoglobin concentration is 8.9 g/dL, mean corpuscular volume is 86 μm3, and serum ferritin is 225 ng/mL. Treatment with erythropoietin is begun. A peripheral blood smear is obtained one week after treatment. A photomicrograph of the smear after specialized staining is shown. The prominent color of the intracellular structure in some of the cells is most likely the result of staining which of the following?
- A. Golgi apparatus
- B. Ribosomal RNA (Correct Answer)
- C. Remnants of the nucleus
- D. Denatured globin chains
- E. Mitochondria
Electron microscopy in histology Explanation: ***Ribosomal RNA***
- The patient's presentation of **anemia** in the setting of chronic kidney disease and subsequent treatment with erythropoietin points to a likely increase in **reticulocytes** in the peripheral smear.
- The described prominent intracellular structures are characteristic of **reticulofilamentous material**, which is composed primarily of **RNA (ribosomal RNA)** that precipitates out with supravital stains like **new methylene blue**.
*Golgi apparatus*
- The **Golgi apparatus** is an organelle involved in modifying, sorting, and packaging proteins and lipids.
- It is not visible as prominent intracellular structures with **supravital stains** on a peripheral blood smear and does not contribute to reticulocyte staining.
*Remnants of the nucleus*
- While red blood cell precursors have a nucleus, mature erythrocytes and reticulocytes are **anucleated**.
- **Nuclear remnants** (e.g., Howell-Jolly bodies) are typically **DNA-containing fragments** appearing as dense, basophilic inclusions, which are distinctly different from the reticulofilamentous network.
*Denatured globin chains*
- **Denatured globin chains** (e.g., **Heinz bodies**) are associated with oxidative stress and appear as small, irregular inclusions that require **crystal violet stain** for visualization.
- These are not the prominent basophilic reticulations seen in reticulocytes.
*Mitochondria*
- **Mitochondria** are organelles responsible for cellular respiration and are present in many cell types, including immature red blood cells.
- However, they do not stain in the characteristic reticular pattern observed in reticulocytes using **supravital stains** for RNA.
Electron microscopy in histology US Medical PG Question 5: A 36-year-old man undergoes ileocecal resection after a gunshot injury. The resected ileocecal segment is sent for histological evaluation. One of the slides derived from the specimen is shown in the image. Which of the following statements regarding the structure marked within the red circle is correct?
- A. This structure can be only found in the colon.
- B. These structures mostly contain M-cells.
- C. This structure can become a site of entry of certain microorganisms including S. typhi. (Correct Answer)
- D. This structure only appears in case of bacterial infection.
- E. Infants have the largest amount of these structures within their intestinal wall.
Electron microscopy in histology Explanation: ***This structure can become a site of entry of certain microorganisms including S. typhi.***
- The image illustrates **Peyer's patches**, which are lymphoid follicles found primarily in the ileum. These structures are rich in **M-cells**, which sample antigens from the intestinal lumen.
- While M-cells are crucial for initiating immune responses, some pathogens like *Salmonella typhi* exploit them to **translocate across the intestinal barrier** and disseminate, leading to systemic infection.
*This structure can be only found in the colon.*
- The structure shown is a **Peyer's patch**, which is predominantly found in the **ileum** of the small intestine, not exclusively in the colon.
- While lymphoid tissue is present throughout the GI tract, these large aggregated lymphoid nodules are characteristic of the ileum.
*These structures mostly contain M-cells.*
- While **M-cells (microfold cells)** are indeed present in the dome epithelium overlying Peyer's patches and are critical for antigen sampling, they constitute a minority of the cells within the entire structure.
- The bulk of Peyer's patches consists of **lymphocytes** (B cells, T cells), macrophages, and dendritic cells, forming lymphoid follicles and interfollicular areas.
*This structure only appears in case of bacterial infection.*
- **Peyer's patches** are a normal and permanent component of the gut-associated lymphoid tissue (GALT) and are present in healthy individuals.
- They serve as crucial sites for **immune surveillance** and the induction of adaptive immune responses to both commensal bacteria and pathogens, even in the absence of an active infection.
*Infants have the largest amount of these structures within their intestinal wall.*
- Peyer's patches are **well-developed at birth** and continue to increase in size and number during childhood and adolescence.
- They tend to **atrophy with age**, meaning that young adults and adolescents typically have the most prominent and numerous Peyer's patches, not infants.
Electron microscopy in histology US Medical PG Question 6: A 45-year-old man presents to the office with complaints of facial puffiness and mild swelling in his lower back. He denies chest pain, blood in the urine, or fever. He was recently diagnosed with colon cancer. The vital signs include a blood pressure of 122/78 mm Hg, a pulse of 76/min, a temperature of 36.9°C (98.4°F), and a respiratory rate of 10/min. On physical examination, there is mild facial puffiness that is pitting in nature and presacral edema. His other systemic findings are within normal limits.
Urinalysis shows:
pH 6.2
Color light yellow
RBC none
WBC 3–4/HPF
Protein 4+
Cast oval fat bodies
Glucose absent
Crystal none
Ketone absent
Nitrite absent
24 hours urine protein excretion 4.8 g
A renal biopsy is ordered and diffuse capillary and basement membrane thickening is noted. Which of the following findings is expected to be present if an electron microscopy of the biopsy sample is performed?
- A. Subepithelial humps
- B. Effacement of foot process
- C. Basket-weave appearance of GBM
- D. Massive amyloid deposition and spicular aggregates
- E. Spike and dome appearance (Correct Answer)
Electron microscopy in histology Explanation: ***Spike and dome appearance***
- The patient's presentation with **facial puffiness**, **presacral edema**, **4+ proteinuria**, **oval fat bodies**, and **4.8 g/24hr protein excretion** with **diffuse capillary and basement membrane thickening** on renal biopsy, in the setting of **colon cancer**, is highly suggestive of **membranous nephropathy**.
- **Membranous nephropathy** is characterized on electron microscopy by **subepithelial immune complex deposits**, which often manifest as a **"spike and dome" appearance** due to new basement membrane material laid down between the immune deposits.
*Subepithelial humps*
- **Subepithelial humps** are characteristic of **post-streptococcal glomerulonephritis** and other forms of **acute post-infectious glomerulonephritis**.
- This patient's presentation with **nephrotic syndrome** features and chronic disease does not align with acute glomerulonephritis.
*Effacement of foot process*
- **Effacement of foot processes** (podocyte effacement) is a finding seen in almost all causes of **heavy proteinuria** and **nephrotic syndrome**, including **minimal change disease**, **focal segmental glomerulosclerosis**, and **membranous nephropathy**.
- While it would be present in this case, it is a non-specific finding of proteinuria itself, not a defining characteristic of **membranous nephropathy** itself, which is what "spike and dome" is.
*Basket-weave appearance of GBM*
- The **"basket-weave" appearance** refers to the irregular thickening and lamellation of the **glomerular basement membrane (GBM)**, typically seen in **Alport syndrome**.
- This is a genetic disorder of type IV collagen and does not fit the clinical picture of an adult with recent colon cancer and acquired nephrotic syndrome.
*Massive amyloid deposition and spicular aggregates*
- **Massive amyloid deposition** with **spicular aggregates** is characteristic of **amyloidosis**.
- While amyloidosis can cause nephrotic syndrome and be associated with chronic diseases, the light microscopy finding of **diffuse capillary and basement membrane thickening** without specific mention of congophilic deposits or apple-green birefringence makes membranous nephropathy a more direct fit with the "spike and dome" EM finding.
Electron microscopy in histology US Medical PG Question 7: An investigator is studying the effects of zinc deprivation on cancer cell proliferation. It is hypothesized that because zinc is known to be a component of transcription factor motifs, zinc deprivation will result in slower tumor growth. To test this hypothesis, tumor cells are cultured on media containing low and high concentrations of zinc. During the experiment, a labeled oligonucleotide probe is used to identify the presence of a known transcription factor. The investigator most likely used which of the following laboratory techniques?
- A. ELISA
- B. PCR
- C. Western blot
- D. Northern blot
- E. Southwestern blot (Correct Answer)
Electron microscopy in histology Explanation: ***Southwestern blot***
- A **Southwestern blot** specifically identifies **DNA-binding proteins** (such as transcription factors) by detecting their ability to bind to specific **labeled DNA oligonucleotide probes**
- The technique involves: protein separation by gel electrophoresis → transfer to membrane → probing with **labeled double-stranded DNA oligonucleotide**
- This directly answers the question: using a labeled oligonucleotide probe to identify a transcription factor
*ELISA*
- **ELISA** detects and quantifies proteins using **antibody-antigen interactions**, not DNA-binding activity
- While it could detect the presence of a transcription factor protein, it cannot assess the protein's ability to bind to specific DNA sequences
- Does not utilize oligonucleotide probes for detection
*PCR*
- **PCR** amplifies specific **DNA sequences** but does not detect or characterize proteins
- This technique would amplify DNA, not identify DNA-binding proteins
- Not applicable for detecting transcription factor presence or function
*Western blot*
- **Western blot** detects specific proteins using **antibodies**, not oligonucleotide probes
- While it could confirm transcription factor protein presence, it cannot assess DNA-binding capability
- Uses antibody-based detection, not nucleotide probe-based detection
*Northern blot*
- **Northern blot** detects specific **RNA molecules**, not DNA-binding proteins
- Uses labeled DNA or RNA probes to detect RNA, not to detect proteins that bind DNA
- Wrong target molecule (RNA vs. proteins)
Electron microscopy in histology US Medical PG Question 8: A 4-year-old male is accompanied by his mother to the pediatrician. His mother reports that over the past two weeks, the child has had intermittent low grade fevers and has been more lethargic than usual. The child’s past medical history is notable for myelomeningocele complicated by lower extremity weakness as well as bowel and bladder dysfunction. He has been hospitalized multiple times at an outside facility for recurrent urinary tract infections. The child is in the 15th percentile for both height and weight. His temperature is 100.7°F (38.2°C), blood pressure is 115/70 mmHg, pulse is 115/min, and respirations are 20/min. Physical examination is notable for costovertebral angle tenderness that is worse on the right. Which of the following would most likely be found on biopsy of this patient’s kidney?
- A. Replacement of renal parenchyma with foamy histiocytes
- B. Tubular colloid casts with diffuse lymphoplasmacytic infiltrate (Correct Answer)
- C. Diffusely necrotic papillae with dystrophic calcification
- D. Mononuclear and eosinophilic infiltrate
- E. Destruction of the proximal tubule and medullary thick ascending limb
Electron microscopy in histology Explanation: ***Tubular colloid casts with diffuse lymphoplasmacytic infiltrate***
- The patient's history of **myelomeningocele**, recurrent **urinary tract infections (UTIs)**, and current symptoms (fever, lethargy, CVA tenderness) strongly suggest **chronic pyelonephritis**.
- **Chronic pyelonephritis** is characterized histologically by **tubular atrophy**, interstitial fibrosis, and a **lymphoplasmacytic infiltrate**, often with "thyroidization" of the tubules where they are dilated and filled with colloid casts.
*Replacement of renal parenchyma with foamy histiocytes*
- This description is characteristic of **xanthogranulomatous pyelonephritis**, a severe and rare form of chronic pyelonephritis.
- While possible given chronic UTIs, the more general and common finding in chronic pyelonephritis is a diffuse lymphoplasmacytic infiltrate, not necessarily dominant foamy histiocytes.
*Diffusely necrotic papillae with dystrophic calcification*
- This finding is most consistent with **renal papillary necrosis**.
- Renal papillary necrosis is typically associated with conditions like **analgesic nephropathy**, **sickle cell disease**, or severe acute pyelonephritis, but not the primary histological change in chronic pyelonephritis as described.
*Mononuclear and eosinophilic infiltrate*
- A prominent **eosinophilic infiltrate** in the kidney is often seen in **acute interstitial nephritis**, which can be drug-induced.
- While chronic inflammation involves mononuclear cells, the specific mention of eosinophils makes this less likely to be the primary finding in chronic pyelonephritis from recurrent UTIs.
*Destruction of the proximal tubule and medullary thick ascending limb*
- Destruction of specific tubular segments, particularly the **proximal tubule**, is characteristic of acute tubular necrosis (ATN).
- While chronic pyelonephritis leads to tubular atrophy and damage, the primary description here points to an acute injury rather than the chronic inflammatory changes expected.
Electron microscopy in histology US Medical PG Question 9: This type of epithelium is most commonly seen in which of the following organs?
- A. Ureter
- B. Trachea (Correct Answer)
- C. Duodenum
- D. Gall bladder
- E. Esophagus
Electron microscopy in histology Explanation: ***Trachea***
- The image displays **pseudostratified columnar epithelium with cilia and goblet cells**, which is characteristic of the respiratory tract, including the trachea.
- This specialized epithelium functions to trap and expel foreign particles from the airways, ensuring respiratory health.
*Ureter*
- The ureter is lined by **transitional epithelium** (urothelium), which is characterized by its ability to stretch.
- This epithelium would show a cuboidal to columnar appearance when relaxed and a flattened appearance when stretched, and the cells on the surface are typically dome-shaped, unlike the image.
*Duodenum*
- The duodenum is lined by **simple columnar epithelium** with a brush border and numerous goblet cells for absorption and mucus secretion.
- It also features **villi and crypts of Lieberkühn**, which are not seen in the provided image.
*Gall bladder*
- The gallbladder is lined by **simple columnar epithelium** with microvilli, specialized for water absorption.
- It lacks the cilia and pseudostratified arrangement evident in the given histopathology slide.
*Esophagus*
- The esophagus is lined by **non-keratinized stratified squamous epithelium**, designed to protect against abrasion from food passage.
- This epithelium appears as multiple layers of flattened cells, completely different from the tall, columnar, ciliated cells shown in the image.
Electron microscopy in histology US Medical PG Question 10: An investigator is conducting a study to document the histological changes in the respiratory tree of a chronic smoker. He obtains multiple biopsy samples from the respiratory system of a previously healthy 28-year-old man. Histopathological examination of one sample shows simple cuboidal cells with a surrounding layer of smooth muscle. Chondrocytes and goblet cells are absent. This specimen was most likely obtained from which of the following parts of the respiratory system?
- A. Terminal bronchiole (Correct Answer)
- B. Alveolar sac
- C. Main stem bronchus
- D. Bronchiole
- E. Respiratory bronchiole
Electron microscopy in histology Explanation: ***Terminal bronchiole***
- Terminal bronchioles are lined by **simple cuboidal epithelium** and contain surrounding **smooth muscle** but lack cartilage (chondrocytes) and goblet cells, matching the histological description.
- They represent the most distal purely conducting airways before respiratory bronchioles, where gas exchange begins.
*Alveolar sac*
- Alveolar sacs are primarily composed of **Type I and Type II pneumocytes** for gas exchange, and would not have a prominent smooth muscle layer or cuboidal cells in this described pattern.
- They are the terminal structures of the respiratory tree where gas exchange occurs, defined by very thin walls lacking cartilage and goblet cells.
*Main stem bronchus*
- The main stem bronchi are characterized by **pseudostratified ciliated columnar epithelium** with abundant **goblet cells** and contain **hyaline cartilage** (chondrocytes) in their walls.
- The presence of goblet cells and cartilage (chondrocytes) makes this option inconsistent with the given histological findings.
*Bronchiole*
- Bronchioles are generally lined by **ciliated columnar to cuboidal epithelium** with scattered goblet cells in larger ones, and they possess smooth muscle but lack cartilage.
- While they share some features with terminal bronchioles, the presence of goblet cells (even if sparse) distinguishes bronchioles from terminal bronchioles.
*Respiratory bronchiole*
- Respiratory bronchioles are distinguished by their walls having occasional **alveoli**, indicating the beginning of gas exchange. Their epithelium is cuboidal.
- They would not be described as having a "surrounding layer of smooth muscle" in isolation as clearly as a terminal bronchiole, and the presence of alveoli would be a key distinguishing feature.
More Electron microscopy in histology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.