Aging-related histological changes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Aging-related histological changes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Aging-related histological changes US Medical PG Question 1: A 78-year-old man dies suddenly from complications of acute kidney failure. An autopsy is performed and microscopic evaluation of the kidneys shows pale, swollen cells in the proximal convoluted tubules. Microscopic evaluation of the liver shows similar findings. Which of the following is the most likely underlying mechanism of these findings?
- A. Double-stranded DNA breakage
- B. Impaired Na+/K+-ATPase pump activity (Correct Answer)
- C. Free radical formation
- D. Cytochrome C release
- E. Cytoplasmic triglyceride accumulation
Aging-related histological changes Explanation: ***Impaired Na+/K+-ATPase pump activity***
- **Acute kidney failure** leads to **hypoxia** and ATP depletion, which impairs the function of the **Na+/K+-ATPase pump** on the cell membrane.
- Failure of this pump results in **intracellular accumulation of sodium** and water, causing **cellular swelling** and pallor as seen in the kidneys and liver.
*Double-stranded DNA breakage*
- This is primarily associated with **apoptosis** or **radiation injury**, which would lead to nuclear fragmentation and cellular death rather than simple cellular swelling.
- While cell death can occur in acute kidney failure, the initial changes described (pale, swollen cells) are characteristic of **reversible cell injury** before extensive DNA damage.
*Free radical formation*
- **Free radical formation** (oxidative stress) can cause cellular injury, but it primarily leads to **lipid peroxidation of membranes** and damage to proteins and DNA, not directly to the widespread intracellular water accumulation described.
- While part of the injury cascade, it's not the most direct mechanism for the initial gross and microscopic findings of swelling.
*Cytochrome C release*
- **Cytochrome C release** from mitochondria is a critical step in the **intrinsic pathway of apoptosis**, leading to programmed cell death.
- The findings described (pale, swollen cells) are more indicative of **reversible cellular injury** or early necrosis, prior to the widespread activation of apoptosis.
*Cytoplasmic triglyceride accumulation*
- **Cytoplasmic triglyceride accumulation** (steatosis or fatty change) is often seen in conditions like **alcoholic liver disease** or **metabolic syndrome**.
- While it can be a sign of cellular injury, it does not directly explain the generalized "pale, swollen cells" observed in both the kidneys and liver following acute kidney failure, which points to water influx.
Aging-related histological changes US Medical PG Question 2: A surgeon is interested in studying how different surgical techniques impact the healing of tendon injuries. In particular, he will compare 3 different types of suture repairs biomechanically in order to determine the maximum load before failure of the tendon 2 weeks after repair. He collects data on maximum load for 90 different repaired tendons from an animal model. Thirty tendons were repaired using each of the different suture techniques. Which of the following statistical measures is most appropriate for analyzing the results of this study?
- A. Chi-squared
- B. Wilcoxon rank sum
- C. Pearson r coefficient
- D. Student t-test
- E. ANOVA (Correct Answer)
Aging-related histological changes Explanation: ***ANOVA***
- **ANOVA (Analysis of Variance)** is appropriate here because it compares the means of **three or more independent groups** (the three different suture techniques) on a continuous dependent variable (maximum load before failure).
- The study has three distinct repair techniques, each with 30 tendons, making ANOVA suitable for determining if there are statistically significant differences among their mean failure loads.
*Chi-squared*
- The **Chi-squared test** is used for analyzing **categorical data** (frequencies or proportions) to determine if there is an association between two nominal variables.
- This study involves quantitative measurement (maximum load), not categorical data, making Chi-squared inappropriate.
*Wilcoxon rank sum*
- The **Wilcoxon rank sum test** (also known as Mann-Whitney U test) is a **non-parametric test** used to compare two independent groups when the data is not normally distributed or is ordinal.
- While the study has independent groups, it involves three groups, and the dependent variable is continuous, making ANOVA a more powerful and appropriate choice assuming normal distribution.
*Pearson r coefficient*
- The **Pearson r coefficient** measures the **strength and direction of a linear relationship between two continuous variables**.
- This study aims to compare means across different groups, not to determine the correlation between two continuous variables.
*Student t-test*
- The **Student t-test** is used to compare the means of **exactly two groups** (either independent or paired) on a continuous dependent variable.
- This study involves comparing three different suture techniques, not just two, making the t-test unsuitable.
Aging-related histological changes US Medical PG Question 3: A 71-year-old man with colorectal cancer comes to the physician for follow-up examination after undergoing a sigmoid colectomy. The physician recommends adjuvant chemotherapy with an agent that results in single-stranded DNA breaks. This chemotherapeutic agent most likely has an effect on which of the following enzymes?
- A. DNA polymerase III
- B. Topoisomerase I (Correct Answer)
- C. Helicase
- D. Telomerase
- E. Topoisomerase II
Aging-related histological changes Explanation: ***Topoisomerase I***
- **Topoisomerase I** creates **single-stranded DNA (ssDNA) breaks** to relieve torsional stress during DNA replication and transcription.
- Many chemotherapeutic agents, such as camptothecin and its derivatives (e.g., irinotecan, topotecan), target topoisomerase I, leading to DNA damage and apoptosis in cancer cells.
*DNA polymerase III*
- **DNA polymerase III** is primarily involved in bacterial DNA replication, synthesizing new DNA strands in a 5' to 3' direction.
- While essential for bacterial survival, it is not the target of chemotherapeutic agents that induce single-stranded DNA breaks in human cells.
*Helicase*
- **Helicase** is responsible for unwinding the DNA double helix during replication and transcription, separating the two strands.
- While its function is critical for DNA processes, it does not directly create DNA breaks as its primary mechanism of action.
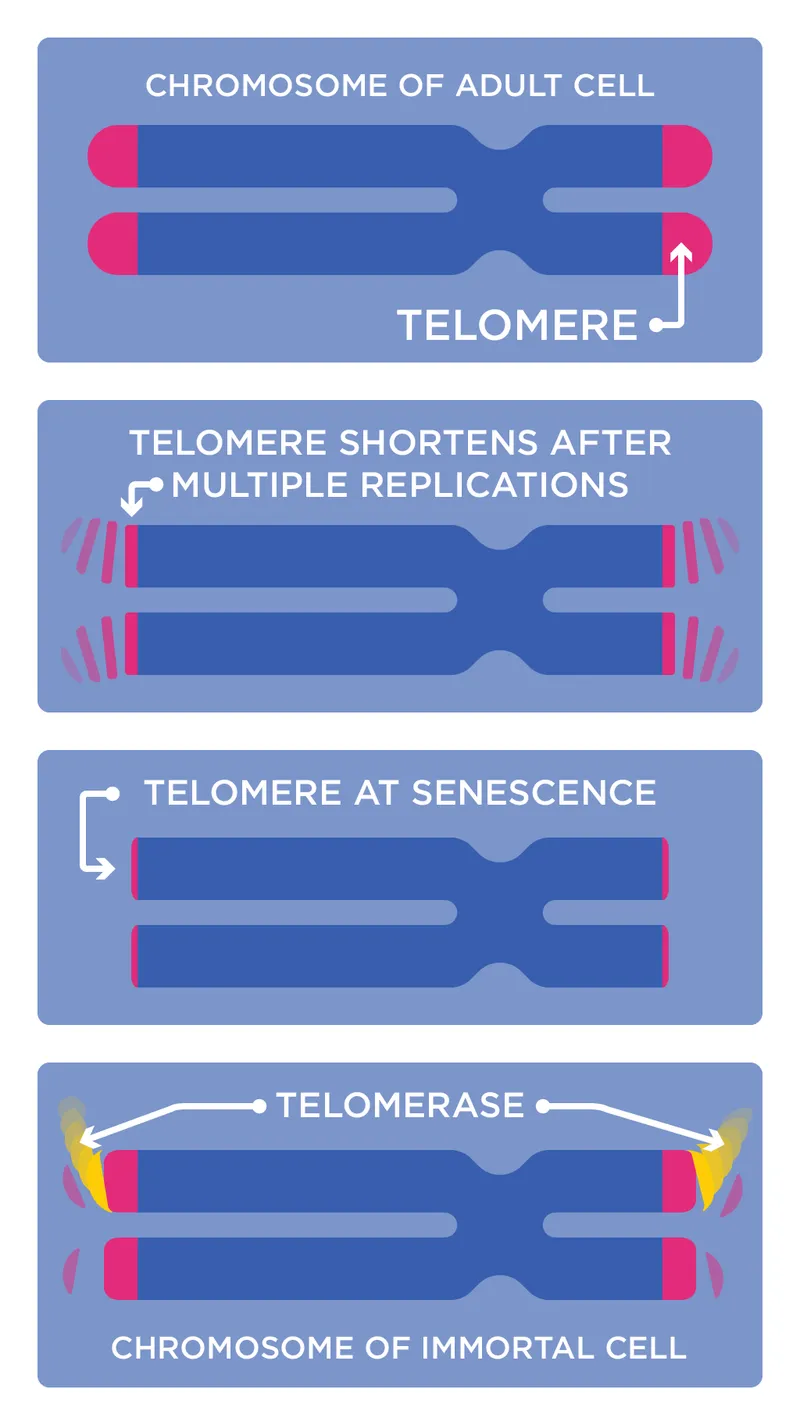
*Telomerase*
- **Telomerase** is an enzyme that maintains telomere length at the ends of chromosomes, particularly active in cancer cells.
- Inhibitors of telomerase aim to shorten telomeres, leading to cellular senescence or apoptosis, but they do not primarily cause single-stranded DNA breaks.
*Topoisomerase II*
- **Topoisomerase II** creates **double-stranded DNA (dsDNA) breaks** to untangle and decatenate DNA.
- Though also a target for chemotherapy (e.g., etoposide, doxorubicin), its mechanism involves double-stranded breaks, not single-stranded breaks as specified in the question.
Aging-related histological changes US Medical PG Question 4: A 30-year-old man comes to the physician for a follow-up examination 1 month after sustaining a chemical burn over the dorsum of his right hand and forearm. Physical examination shows hyperextension of the hand at the wrist. The skin over the dorsum of the wrist is tense and there is a thick, epithelialized scar. Range of motion of the right wrist is restricted. This patient's contracture is most likely due to activity of which of the following cells?
- A. Fibroblasts
- B. Myofibroblasts (Correct Answer)
- C. Neutrophils
- D. Macrophages
- E. Endothelial cells
Aging-related histological changes Explanation: ***Myofibroblasts***
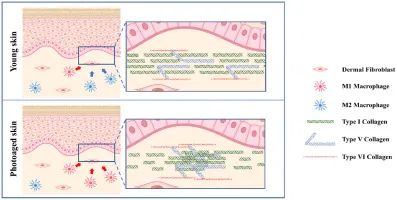
- The patient presents with a **contracture** (restricted range of motion and hyperextension of the hand due to a thick scar) after a burn, which is characteristic of the action of **myofibroblasts**.
- Myofibroblasts are specialized cells that possess features of both fibroblasts (synthesizing **collagen** and extracellular matrix) and smooth muscle cells (containing **actin microfilaments**), allowing them to exert contractile force which leads to scar contraction.
*Fibroblasts*
- While fibroblasts are crucial for **wound healing** by producing collagen and other extracellular matrix components, they primarily lay down the foundation for scar tissue.
- They lack the strong contractile capabilities that lead to significant **tissue retraction** and contracture.
*Neutrophils*
- Neutrophils are **acute inflammatory cells** that primarily function in the early stages of wound healing to phagocytose debris and pathogens.
- They do not play a direct role in the formation of **scar tissue** or **contractures**.
*Macrophages*
- Macrophages are important **immune cells** involved in clearing debris, presenting antigens, and releasing growth factors during the later stages of wound healing.
- They also influence fibroblast activity, but they do not directly cause **tissue contraction** or scar formation.
*Endothelial cells*
- Endothelial cells line **blood vessels** and are essential for **angiogenesis** (formation of new blood vessels) during wound healing.
- They are not involved in the **contractile process** that leads to scar contracture.
Aging-related histological changes US Medical PG Question 5: An investigator is studying the biology of human sperm cells. She isolates spermatogonia obtained on a testicular biopsy from a group of healthy male volunteers. She finds that the DNA of spermatogonia obtained from these men show a large number of TTAGGG sequence repeats. This finding can best be explained by increased activity of an enzyme with which of the following functions?
- A. Ligation of Okazaki fragments
- B. Proofreading of synthesized daughter strands
- C. RNA-dependent synthesis of DNA (Correct Answer)
- D. Production of short RNA sequences
- E. Hemimethylation of DNA strand
Aging-related histological changes Explanation: ***RNA-dependent synthesis of DNA***
- The TTAGGG sequence repeats are **telomeric sequences**, which are maintained by **telomerase**, an enzyme that synthesizes DNA from an RNA template.
- **Spermatogonia** are germline stem cells that express high levels of telomerase to maintain telomere length across generations.
*Ligation of Okazaki fragments*
- This function is carried out by **DNA ligase**, which joins discontinuous DNA fragments during replication on the lagging strand.
- This process is essential for general DNA replication but is not specific to the formation or maintenance of telomeric repeats.
*Proofreading of synthesized daughter strands*
- This is a function of **DNA polymerase exonuclease activity**, which corrects errors during DNA replication.
- While important for genetic fidelity, it does not explain the presence or increase of specific TTAGGG repeat sequences at telomeres.
*Production of short RNA sequences*
- This function is performed by **primase**, which synthesizes RNA primers necessary to initiate DNA synthesis during replication.
- These RNA primers are later removed and replaced with DNA, and this process is not directly responsible for generating or extending telomeric repeats.
*Hemimethylation of DNA strand*
- Hemimethylation occurs during **DNA replication** when new DNA strands are unmethylated while parental strands are methylated.
- This phenomenon is involved in DNA repair and gene regulation but is unrelated to the synthesis or regulation of telomeric sequences.
Aging-related histological changes US Medical PG Question 6: A 48-year-old man has smoked approximately 3 packs of cigarettes per day for the past 12 years. Which of the following pathologic changes is most likely to occur in his bronchial epithelium?
- A. Metaplasia (Correct Answer)
- B. Hyperplasia
- C. Hypertrophy
- D. Dysplasia
- E. Atrophy
Aging-related histological changes Explanation: ***Metaplasia***
- Chronic irritation from **cigarette smoking** can cause the **bronchial epithelium** to change from ciliated columnar to stratified squamous, a process known as **metaplasia**.
- This adaptation makes the tissue more resistant to injury but results in the loss of important protective functions like **mucociliary clearance**.
*Hyperplasia*
- **Hyperplasia** involves an increase in the number of cells in a tissue or organ, often in response to increased demand or chronic stimulation.
- While smoking can cause hyperplasia of goblet cells and mucous glands in the bronchi, the direct epithelial change in response to chronic irritation is more specifically **metaplasia**.
*Hypertrophy*
- **Hypertrophy** is an increase in the size of individual cells, leading to an increase in the size of the organ or tissue.
- This is not the primary adaptive change seen in the bronchial epithelium in response to chronic smoking; instead, cells change their type.
*Dysplasia*
- **Dysplasia** refers to disorderly cell growth, often characterized by variations in cell size, shape, and organization; it is considered a precursor to cancer.
- While chronic smoking can eventually lead to dysplasia and then carcinoma, the initial and most common adaptive change in the bronchial epithelium is **metaplasia**.
*Atrophy*
- **Atrophy** is a decrease in cell size or number, leading to a reduction in the size of an organ or tissue, usually due to decreased workload, nutrition, or blood supply.
- This is not a typical response of the bronchial epithelium to chronic irritation from smoking, which tends to induce proliferative or adaptive changes.
Aging-related histological changes US Medical PG Question 7: A 42-year-old man with systolic heart failure secondary to amyloidosis undergoes heart transplantation. The donor heart is obtained from a 17-year-old boy who died in a motor vehicle collision. Examination of the donor heart during the procedure shows a flat, yellow-white discoloration with an irregular border on the luminal surface of the aorta. A biopsy of this lesion is most likely to show which of the following?
- A. Apoptotic smooth muscle cells
- B. Necrotic cell debris
- C. Proteoglycan accumulation
- D. Collagen deposition
- E. Lipoprotein-laden macrophages (Correct Answer)
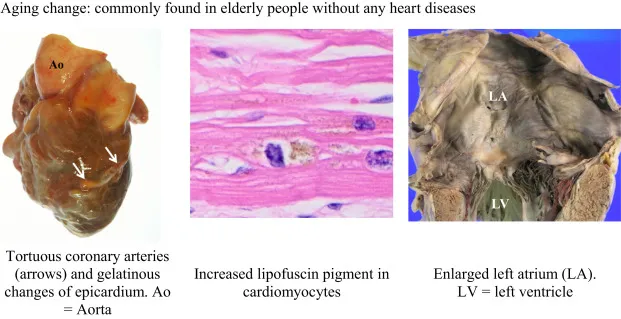
Aging-related histological changes Explanation: ***Lipoprotein-laden macrophages***
- The description of a flat, yellow-white discolored lesion with an irregular border on the luminal surface of the aorta in a 17-year-old is classic for a **fatty streak**, the earliest lesion of **atherosclerosis**.
- Fatty streaks are histologically characterized by the accumulation of **macrophages that have ingested oxidized lipoproteins**, appearing as foam cells within the intima.
*Apoptotic smooth muscle cells*
- While apoptosis of various cell types, including smooth muscle cells, can occur in advanced atherosclerotic lesions, it is not the primary or defining feature of an early **fatty streak**.
- **Apoptosis** contributes to the necrotic core formation in later stages of plaque development, not the initial yellow-white discoloration of a fatty streak.
*Necrotic cell debris*
- **Necrotic cell debris** is a prominent feature of more advanced, **complicated atherosclerotic plaques**, forming the necrotic core.
- In a **fatty streak**, the cells are primarily viable foam cells, and significant necrosis is not yet present.
*Proteoglycan accumulation*
- **Proteoglycan accumulation** occurs in the arterial intima and is involved in the retention of lipoproteins, contributing to the development of atherosclerosis.
- However, the immediate and most characteristic histological finding of the **yellow-white discoloration** in a fatty streak is the lipid-laden macrophage.
*Collagen deposition*
- **Collagen deposition** is a key feature of the fibrous cap in **advanced atherosclerotic plaques**, laid down by migrating smooth muscle cells.
- It is not the primary histological characteristic of an early, flat, yellow-white **fatty streak**.
Aging-related histological changes US Medical PG Question 8: A 72-year-old man presents to his primary care physician for his annual exam. He has a very stoic personality and says that he is generally very healthy and has "the normal aches and pains of old age." On further probing, you learn that he does have pretty significant back and hip pain that worsens throughout the day. On physical exam you note bony enlargement of the distal interphalangeal joints bilaterally. Which of the following is the likely cause of his symptoms?
- A. Rheumatoid arthritis
- B. Osteoarthritis (Correct Answer)
- C. Gout
- D. Pseudogout
- E. Osteopenia
Aging-related histological changes Explanation: ***Osteoarthritis***
- The patient's age (72 years), back and hip pain that **worsens throughout the day** (classic for *wear-and-tear*), and **bony enlargement of the distal interphalangeal (DIP) joints** (Heberden's nodes) are highly characteristic of osteoarthritis.
- This condition involves the progressive **degeneration of articular cartilage**, leading to bone-on-bone friction and osteophyte formation.
*Osteopenia*
- **Osteopenia** is a precursor to osteoporosis, characterized by **reduced bone mineral density**, making bones weaker.
- It typically presents with **no symptoms** until it progresses to osteoporosis and causes fractures; it does not cause pain that worsens throughout the day or bony enlargements of joints.
*Rheumatoid arthritis*
- **Rheumatoid arthritis** typically affects the **small joints of the hands and feet symmetrically**, but it predominantly involves the **proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints**, sparing the distal interphalangeal (DIP) joints.
- Pain and stiffness associated with rheumatoid arthritis are usually **worse in the morning** and *improve with activity*, in contrast to the patient's symptoms.
*Gout*
- **Gout** is an inflammatory arthritis caused by the deposition of **urate crystals**, typically presenting as *acute, severe attacks* of pain, swelling, and redness in a single joint, most commonly the **big toe**.
- While it can affect other joints over time, it does not typically cause gradual onset, activity-related pain, or bony enlargement of DIP joints as described.
*Pseudogout*
- **Pseudogout**, or **calcium pyrophosphate deposition disease (CPPD)**, is caused by the deposition of **calcium pyrophosphate crystals** in joints.
- Similar to gout, it causes *acute inflammatory arthritis*, often affecting larger joints like the knee or wrist, and is not characterized by the chronic, activity-related pain and DIP joint bony changes seen in this patient.
Aging-related histological changes US Medical PG Question 9: A 55-year-old man presents to his primary care physician with a complaint of fatigue for a couple of months. He was feeling well during his last visit 6 months ago. He has a history of hypertension for the past 8 years, diabetes mellitus for the past 5 years, and chronic kidney disease (CKD) for a year. The vital signs include: blood pressure 138/84 mm Hg, pulse 81/min, temperature 36.8°C (98.2°F), and respiratory rate 9/min. On physical examination, moderate pallor is noted on the palpebral conjunctiva and nail bed.
Complete blood count results are as follows:
Hemoglobin 8.5 g/dL
RBC 4.2 million cells/µL
Hematocrit 39%
Total leukocyte count 6,500 cells/µL
Neutrophils 61%
Lymphocytes 34%
Monocytes 4%
Eosinophils 1%
Basophils 0%
Platelets 240,000 cells/µL
A basic metabolic panel shows:
Sodium 133 mEq/L
Potassium 5.8 mEq/L
Chloride 101 mEq/L
Bicarbonate 21 mEq/L
Albumin 3.1 mg/dL
Urea nitrogen 31 mg/dL
Creatinine 2.8 mg/dL
Uric acid 6.4 mg/dL
Calcium 8.1 mg/dL
Glucose 111 mg/dL
Which of the following explanations best explains the mechanism for his decreased hemoglobin?
- A. Progressive metabolic acidosis
- B. Side effect of his medication
- C. Failure of adequate erythropoietin production (Correct Answer)
- D. Failure of 1-alpha-hydroxylation of 25-hydroxycholecalciferol
- E. Increased retention of uremic products
Aging-related histological changes Explanation: ***Failure of adequate erythropoietin production***
- The patient's history of **chronic kidney disease (CKD)** is the key factor. As kidney function declines, the peritubular interstitial cells in the renal cortex, which produce **erythropoietin (EPO)**, are damaged, leading to inadequate EPO synthesis.
- **Erythropoietin** is essential for stimulating red blood cell production in the bone marrow, so its deficiency directly causes **normocytic, normochromic anemia**, consistent with the patient's low hemoglobin (8.5 g/dL) and pallor.
*Progressive metabolic acidosis*
- While metabolic acidosis can occur in CKD, it primarily impacts overall metabolic function and can mildly suppress bone marrow, but it is not the **primary mechanism** for severe anemia in CKD.
- The patient's bicarbonate of 21 mEq/L indicates mild acidosis, not severe enough to be the dominant cause of his profound anemia.
*Side effect of his medication*
- Although some medications can cause anemia (e.g., ACE inhibitors or angiotensin receptor blockers can rarely worsen renal anemia), there is no information provided about specific medications that would directly cause this degree of **hemoglobin reduction** as their primary side effect in this context.
- His complex medical history and lab findings point more directly to a CKD-related etiology for anemia rather than an unmentioned medication side effect.
*Failure of 1-alpha-hydroxylation of 25-hydroxycholecalciferol*
- This process is crucial for the production of **calcitriol (active vitamin D)** in the kidneys, and its failure primarily leads to **hypocalcemia** and **renal osteodystrophy**.
- While related to CKD, impairment of vitamin D activation does not directly explain **decreased hemoglobin production** or significant anemia.
*Increased retention of uremic products*
- The accumulation of **uremic toxins** in CKD can indeed suppress bone marrow, shorten red blood cell survival, and impair iron utilization, contributing to anemia.
- However, the most significant and direct mechanism for anemia in CKD, especially at this stage, is the **lack of erythropoietin production**, which is a hormonal deficiency rather than a toxic effect.
Aging-related histological changes US Medical PG Question 10: As part of a clinical research study, the characteristics of neoplastic and normal cells are being analyzed in culture. It is observed that neoplastic cell division is aided by an enzyme which repairs progressive chromosomal shortening, which is not the case in normal cells. Due to the lack of chromosomal shortening, these neoplastic cells divide more rapidly than the normal cells. Which of the following enzymes is most likely involved?
- A. Topoisomerase
- B. DNA polymerase
- C. Reverse transcriptase
- D. Protein kinase
- E. Telomerase (Correct Answer)
Aging-related histological changes Explanation: ***Telomerase***
- **Telomerase** is an enzyme that adds repetitive nucleotide sequences (telomeres) to the ends of chromosomes, counteracting their progressive shortening during DNA replication. This activity is crucial for the continuous division of neoplastic cells.
- In normal somatic cells, **telomerase activity is typically low or absent**, leading to telomere shortening with each division, eventually triggering cellular senescence or apoptosis. The presence of telomerase in neoplastic cells allows them to bypass these natural limits on proliferation.
*Topoisomerase*
- **Topoisomerases** are enzymes that regulate the supercoiling of DNA by breaking and rejoining DNA strands, which is essential during replication and transcription to relieve torsional stress.
- They do not directly repair chromosomal shortening but rather manage the topological state of DNA.
*DNA polymerase*
- **DNA polymerase** is primarily responsible for synthesizing new DNA strands by adding nucleotides, thereby elongating the DNA molecule during replication and DNA repair processes.
- While essential for DNA replication, it cannot fully replicate the very ends of linear chromosomes, leading to the **end-replication problem** and telomere shortening.
*Reverse transcriptase*
- **Reverse transcriptase** is an enzyme that synthesizes DNA from an RNA template, a process central to retroviruses and some eukaryotic elements like retrotransposons.
- Although telomerase itself is a specialized reverse transcriptase (using an RNA template to synthesize DNA telomeres), the general term "reverse transcriptase" does not specifically refer to the enzyme that repairs chromosomal shortening in the context of cell division.
*Protein kinase*
- **Protein kinases** are enzymes that add phosphate groups to proteins, a process known as phosphorylation. This modification can alter protein activity, localization, or stability, playing a critical role in signal transduction pathways.
- They are involved in regulating various cellular processes, including cell growth and division, but do not directly repair chromosomal shortening.
More Aging-related histological changes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.