Primitive heart tube formation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Primitive heart tube formation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Primitive heart tube formation US Medical PG Question 1: A 19-year-old Caucasian male collapsed from sudden cardiac arrest while playing in a college basketball game. Attempts at resuscitation were unsuccessful. Post-mortem pathologic and histologic examination found asymmetric left ventricular hypertrophy and myocardial disarray. Assuming this was an inherited condition, the relevant gene most likely affects which of the following structures?
- A. Cardiac cell sarcomere proteins (Correct Answer)
- B. Membrane potassium channel proteins
- C. Membrane sodium channels
- D. Ryanodine receptors
- E. Autoimmune beta-cell antibodies
Primitive heart tube formation Explanation: ***Cardiac cell sarcomere proteins***
- The clinical presentation of **sudden cardiac arrest** in a young athlete, along with post-mortem findings of **asymmetric left ventricular hypertrophy** and **myocardial disarray**, are classic for **hypertrophic cardiomyopathy (HCM)**.
- HCM is most commonly caused by mutations in genes encoding **sarcomeric proteins**, leading to abnormal myocardial structure and function.
*Membrane potassium channel proteins*
- Mutations in voltage-gated **potassium channels** are typically associated with cardiac arrhythmias such as **long QT syndrome** and **short QT syndrome**.
- These conditions primarily affect cardiac electrical activity and do not directly cause asymmetric left ventricular hypertrophy or myocardial disarray.
*Membrane sodium channels*
- Defects in **sodium channels** are predominantly linked to conditions like **Brugada syndrome** and certain forms of **long QT syndrome**.
- These channelopathies are characterized by specific ECG abnormalities and increased risk of sudden cardiac death due to arrhythmias, but not structural heart disease like HCM.
*Ryanodine receptors*
- Mutations in the **ryanodine receptor 2 (RyR2) gene** are associated with **catecholaminergic polymorphic ventricular tachycardia (CPVT)**.
- CPVT causes life-threatening arrhythmias, particularly during exercise or emotional stress, but it does not typically present with the structural cardiac abnormalities of HCM.
*Autoimmune beta-cell antibodies*
- **Autoimmune beta-cell antibodies** are characteristic of **Type 1 diabetes mellitus**, an autoimmune disease affecting the pancreas.
- These antibodies are unrelated to cardiac structural or electrical abnormalities and would not explain sudden cardiac arrest with left ventricular hypertrophy and myocardial disarray.
Primitive heart tube formation US Medical PG Question 2: A newborn is rushed to the neonatal ICU after becoming cyanotic shortly after birth. An ultrasound is performed which shows the aorta coming off the right ventricle and lying anterior to the pulmonary artery. The newborn is given prostaglandin E1 and surgery is planned to correct the anatomic defect. Which of the following developmental processes failed to occur in the newborn?
- A. Failure of the membranous ventricular septum to fuse with the muscular interventricular septum
- B. Failure of the septum primum to fuse with the septum secundum
- C. Failure of the aorticopulmonary septum to spiral (Correct Answer)
- D. Failure of the ductus venosus to close
- E. Failure of the ductus arteriosus to close
Primitive heart tube formation Explanation: ***Failure of the aorticopulmonary septum to spiral***
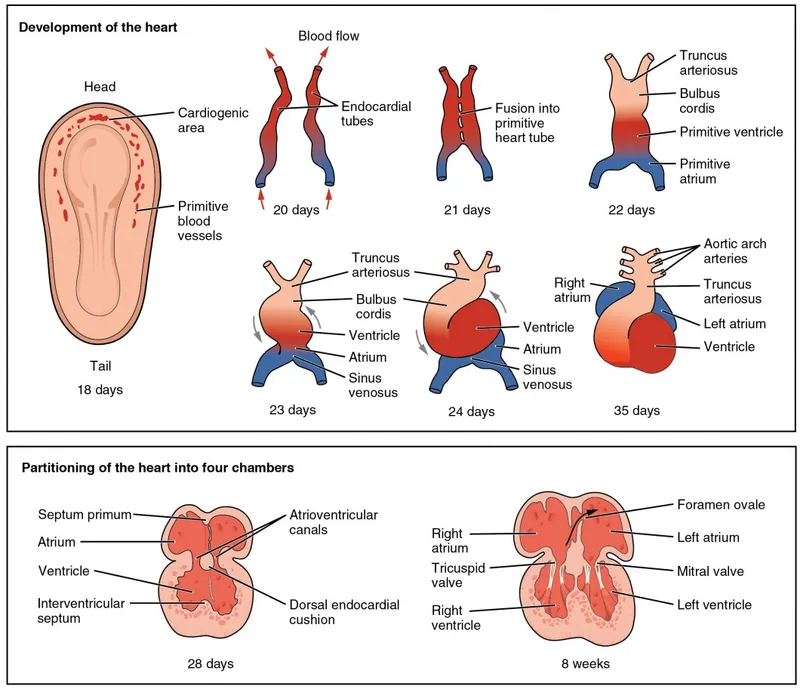
- **Transposition of the great arteries (TGA)**, characterized by the aorta originating from the right ventricle and the pulmonary artery from the left ventricle, results from the **aorticopulmonary septum** failing to spiral properly during embryological development.
- This defect leads to two separate circulatory systems, causing severe **cyanosis** shortly after birth and requiring **prostaglandin E1** to maintain a patent ductus arteriosus for mixing of oxygenated and deoxygenated blood.
- This is a ductal-dependent lesion requiring urgent intervention.
*Failure of the membranous ventricular septum to fuse with the muscular interventricular septum*
- This specific failure leads to a **ventricular septal defect (VSD)**, which allows blood to shunt between ventricles.
- While VSDs can cause cyanosis if large and associated with pulmonary hypertension (Eisenmenger syndrome), the description of **great artery transposition** is not caused by this developmental failure.
*Failure of the septum primum to fuse with the septum secundum*
- This developmental anomaly results in a **patent foramen ovale (PFO)** or an **atrial septal defect (ASD)**.
- These defects typically cause a left-to-right shunt and present with symptoms later in life, not with severe immediate cyanosis.
- In TGA, an ASD may actually be beneficial as it allows some mixing of blood.
*Failure of the ductus venosus to close*
- The **ductus venosus** shunts oxygenated blood from the umbilical vein directly to the inferior vena cava, bypassing the fetal liver during intrauterine life.
- Persistent patency of the ductus venosus after birth is rare and does not cause the severe cyanosis and specific great artery anatomy seen in TGA.
*Failure of the ductus arteriosus to close*
- A **patent ductus arteriosus (PDA)** allows blood to flow from the aorta to the pulmonary artery after birth, which can lead to pulmonary overcirculation.
- In **transposition of the great arteries**, a PDA is actually crucial for survival as it provides a pathway for mixing of oxygenated and deoxygenated blood; maintaining PDA patency with PGE1 is the initial management, not a cause of the condition.
Primitive heart tube formation US Medical PG Question 3: A 69-year-old smoker presents to physician after noticing that his face seems to be more swollen than usual. Upon further questioning, he reports increasing shortness of breath and cough over the past 6 months. On exam, his physician notices venous distention in his neck and distended veins in the upper chest and arms. Chest radiograph shows a right upper lobe mass. What is the embryologic origin of the vessel being compressed by this patient's tumor?
- A. Cardinal veins (Correct Answer)
- B. Primitive ventricle
- C. Left horn of sinus venosus
- D. Truncus arteriosus
- E. Bulbus cordis
Primitive heart tube formation Explanation: ***Cardinal veins***
- The symptoms of facial swelling, neck vein distention, and upper chest/arm vein distention, especially with a right upper lobe mass, are classic for **superior vena cava (SVC) syndrome**.
- The **SVC** is formed from the fusion of the anterior **cardinal veins**, which drain the upper body during embryonic development.
*Primitive ventricle*
- The **primitive ventricle** develops into parts of the left and right **ventricles** of the heart.
- It is not directly involved in the formation of major systemic veins like the SVC.
*Left horn of sinus venosus*
- The **left horn of the sinus venosus** mostly regresses and contributes to structures like the **coronary sinus** and the oblique vein of the left atrium.
- It does not form the SVC, which drains the upper body.
*Truncus arteriosus*
- The **truncus arteriosus** is an embryonic structure that separates to form the **aorta** and the **pulmonary artery**.
- It is an arterial structure, not a venous structure that would be compressed in SVC syndrome.
*Bulbus cordis*
- The **bulbus cordis** develops into the **conus arteriosus** (infundibulum) of the right ventricle and the **aortic vestibule** of the left ventricle.
- Like the truncus arteriosus, it is involved in arterial outflow tracts and not the formation of the SVC.
Primitive heart tube formation US Medical PG Question 4: A patient in the neonatal intensive care unit develops severe cyanosis. Cardiac exam reveals a single loud S2 with a right ventricular heave. Echocardiography reveals an aorta lying anterior and right of the pulmonary artery. Which of the following processes failed during fetal development?
- A. Aorticopulmonary septum to spiral (Correct Answer)
- B. Reentry of viscera from yolk sac
- C. Fusion of the membranous ventricular septum
- D. Fusion of septum primum and septum secondum
- E. Constriction by ductal tissue
Primitive heart tube formation Explanation: ***Aorticopulmonary septum to spiral***
- The clinical presentation describes **transposition of the great arteries (TGA)**, characterized by **severe cyanosis**, a **single loud S2**, and the **aorta lying anterior and right of the pulmonary artery**.
- TGA results from the failure of the **aorticopulmonary septum** to spiral correctly during development, causing the aorta to originate from the right ventricle and the pulmonary artery from the left ventricle.
*Reentry of viscera from yolk sac*
- Failure of this process leads to **omphalocele** or **gastroschisis**, which are abdominal wall defects with extrusion of visceral organs.
- These conditions do not cause severe neonatal cyanosis or specific cardiac malformations like TGA.
*Constriction by ductal tissue*
- This refers to the mechanism of **coarctation of the aorta**, where ectopic ductal tissue causes narrowing of the aortic arch.
- While coarctation can cause cyanosis in the lower body, it does not cause transposition of the great vessels and would not present with the echocardiographic findings described.
*Fusion of the membranous ventricular septum*
- Failure of fusion of the membranous ventricular septum results in a **ventricular septal defect (VSD)**.
- While a VSD can be associated with TGA, it is not the fundamental embryological defect that causes the transposition of the great arteries.
*Fusion of septum primum and septum secondum*
- Failure of fusion between the **septum primum** and **septum secundum** leads to an **atrial septal defect (ASD)**.
- An ASD allows for mixing of blood at the atrial level but is not the primary cause of the transposed great arteries.
Primitive heart tube formation US Medical PG Question 5: Research is being conducted on embryoblasts. The exact date of fertilization is unknown. There is the presence of a cytotrophoblast and syncytiotrophoblast, marking the time when implantation into the uterus would normally occur. Within the embryoblast, columnar and cuboidal cells are separated by a membrane. Which of these cell layers begins to line the yolk sac cavity?
- A. Hypoblast (Correct Answer)
- B. Epiblast
- C. Syncytiotrophoblast
- D. Inner cell mass
- E. Endoderm
Primitive heart tube formation Explanation: ***Hypoblast***
- The **hypoblast** is a layer of cuboidal cells that forms from the inner cell mass around day 8 post-fertilization.
- It plays a crucial role in forming the **primary yolk sac** by migrating to line the exocoelomic cavity.
*Epiblast*
- The **epiblast** is composed of columnar cells located dorsal to the hypoblast and forms the floor of the **amniotic cavity**.
- It is the source of the **three primary germ layers** during gastrulation (ectoderm, mesoderm, and endoderm), not the yolk sac lining itself.
*Syncytiotrophoblast*
- The **syncytiotrophoblast** is the outer, invasive layer of the trophoblast that facilitates implantation and forms the fetal component of the placenta.
- It is not involved in lining the yolk sac cavity but rather in **invading the uterine endometrium** and producing hCG.
*Inner cell mass*
- The **inner cell mass (ICM)** is the cluster of cells within the blastocyst that gives rise to the embryoblast (which further differentiates into epiblast and hypoblast).
- The ICM itself does not line the yolk sac; rather, its derivative, the hypoblast, does.
*Endoderm*
- The **endoderm** is one of the three primary germ layers that forms during gastrulation from the epiblast derivative.
- It ultimately forms the linings of the **gastrointestinal and respiratory tracts**, not the primary yolk sac lining.
Primitive heart tube formation US Medical PG Question 6: A 26-year-old woman comes to the physician because she has not had a menstrual period for 5 weeks. Menarche was at the age of 14 years and menses occurred at regular 30-day intervals. She reports having unprotected sexual intercourse 3 weeks ago. A urine pregnancy test is positive. Which of the following best describes the stage of development of the embryo at this time?
- A. Fetal heart is beating, but cardiac activity is not yet visible on ultrasound
- B. Limb buds have formed, but fetal movements have not begun
- C. Sexual differentiation has begun, but fetal movement has not started
- D. Neural crest has formed, but limb buds have not yet formed (Correct Answer)
- E. Implantation has occurred, but notochord has not yet formed
Primitive heart tube formation Explanation: ***Neural crest has formed, but limb buds have not yet formed***
- At **5 weeks gestational age (3 weeks post-fertilization)**, neurulation is completing or recently completed
- **Neural crest cells** migrate from the neural folds during weeks 3-4 post-fertilization and are definitely present by this time
- **Limb buds** appear later, around week 4-5 post-fertilization (week 6-7 gestational age), making this the most accurate description for the current developmental stage
*Fetal heart is beating, but cardiac activity is not yet visible on ultrasound*
- The primitive heart tube begins contracting around day 22-23 post-fertilization (early week 4)
- At 3 weeks post-fertilization (5 weeks gestational age), the heart may just be starting to beat, but this timing is less precise
- Cardiac activity becomes visible on transvaginal ultrasound around 5.5-6 weeks gestational age, so this option is close but less precise than the correct answer
*Limb buds have formed, but fetal movements have not begun*
- **Limb buds** typically appear around week 4-5 post-fertilization (week 6-7 gestational age)
- This is **too advanced** for 3 weeks post-fertilization
- While fetal movements aren't perceptible to the mother until 16-20 weeks, they begin much later than the current stage
*Sexual differentiation has begun, but fetal movement has not started*
- **Sexual differentiation** of the gonads begins around week 7 post-fertilization (week 9 gestational age)
- External genitalia differentiation occurs even later (weeks 9-12 post-fertilization)
- This stage is **far too advanced** for the current 3-week post-fertilization timeframe
*Implantation has occurred, but notochord has not yet formed*
- **Implantation** occurs 6-12 days after fertilization, which is approximately 2-3 weeks before a positive pregnancy test
- The **notochord** forms during gastrulation in the **3rd week post-fertilization** (5th week gestational age)
- By the time of this positive pregnancy test (5 weeks gestational age), the notochord has **already formed**, making this statement incorrect
Primitive heart tube formation US Medical PG Question 7: A 5-day-old boy is brought to the emergency department by his mother because of a 2-day history of difficulty feeding and multiple episodes of his lips turning blue. He was born at home via spontaneous vaginal delivery and Apgar scores were 7 and 8 at 1 and 5 minutes, respectively. Physical examination shows grunting and moderate intercostal and subcostal retractions. Echocardiography shows a single vessel exiting from the heart. Which of the following is the most likely underlying cause of this patient's condition?
- A. Abnormal placement of the infundibular septum
- B. Absent fusion of septum primum and septum secundum
- C. Failure of neural crest cell migration (Correct Answer)
- D. Insufficient growth of endocardial cushions
- E. Abnormal cardiac looping
Primitive heart tube formation Explanation: ***Failure of neural crest cell migration***
- The echocardiography finding of a **single vessel exiting the heart** is characteristic of **truncus arteriosus**, a congenital heart defect.
- This condition arises from the **failure of neural crest cells** to migrate properly and spiralize the **aortopulmonary septum**, which normally divides the truncus arteriosus into the aorta and pulmonary artery.
*Abnormal placement of the infundibular septum*
- Abnormal placement of the infundibular septum is typically associated with **Tetralogy of Fallot**, leading to an overriding aorta, pulmonary stenosis, ventricular septal defect, and right ventricular hypertrophy.
- While Tetralogy of Fallot is a cyanotic heart disease, it presents with a **bifurcated outflow tract** not a single great vessel.
*Absent fusion of septum primum and septum secundum*
- The absent fusion of the **septum primum** and **septum secundum** results in a **patent foramen ovale** or an **atrial septal defect**.
- These defects primarily cause left-to-right shunting, leading to volume overload in the right heart, but do not explain the presence of a single great vessel.
*Insufficient growth of endocardial cushions*
- Insufficient growth of the **endocardial cushions** can lead to **atrioventricular septal defects** and certain types of **ventricular septal defects**.
- These conditions involve issues with valve formation and septal development but do not directly cause a single great vessel to exit the heart.
*Abnormal cardiac looping*
- Abnormal cardiac looping is associated with conditions like **dextrocardia** or **transposition of the great arteries**.
- While **transposition of the great arteries** also causes cyanosis, it involves **two great vessels** that are improperly connected, not a single great vessel.
Primitive heart tube formation US Medical PG Question 8: A 29-year-old mother brings in her 2-week-old baby boy to a pediatrician because he has been having difficulty feeding. The mother reveals that she had no prenatal care during her pregnancy and gave birth at home without complications. She says that her son seems to be having difficulty sucking, and she occasionally sees breast milk coming out of the infant’s nose. Physical exam reveals that this patient has a gap between his oral and nasal cavities behind the incisive foramen. He is therefore prescribed specialized bottles and his mom is taught positional techniques to ensure better feeding. Failure to fuse which of the following structures is most likely responsible for this patient's disorder?
- A. Maxillary and medial nasal prominences
- B. Nasal septum with primary plates
- C. Maxillary and lateral nasal prominences
- D. Palatine shelves with primary plates
- E. Palatine shelves with nasal septum (Correct Answer)
Primitive heart tube formation Explanation: ***Palatine shelves with nasal septum***
- A **cleft palate** results from the **failure of fusion of the palatine shelves** with each other and/or with the **nasal septum**, creating an abnormal communication between the oral and nasal cavities.
- This anatomical defect explains the infant's **feeding difficulties** and the leakage of breast milk into the nose, as well as the observed **gap behind the incisive foramen**.
*Maxillary and medial nasal prominences*
- The failure of fusion between the maxillary and medial nasal prominences results in a **cleft lip**, which is an anterior defect and does not explain the posterior gap described.
- While cleft lip can coexist with cleft palate, the symptoms here specifically point to a palatal defect, not primarily a lip defect.
*Nasal septum with primary plates*
- The primary palate forms from the fusion of the medial nasal prominences, anterior to the incisive foramen.
- While crucial for normal development, the specific clinical presentation (gap *behind* the incisive foramen and feeding difficulties) is more characteristic of a secondary palate defect involving the palatine shelves.
*Maxillary and lateral nasal prominences*
- The fusion of these structures contributes to the formation of the **nasolacrimal groove** and parts of the cheek, not the palate.
- Deficiencies in this fusion would lead to defects in the lateral facial region, not an oro-nasal communication related to feeding.
*Palatine shelves with primary plates*
- The **primary palate** fuses with the anterior part of the secondary palate (formed by the palatine shelves) at the incisive foramen.
- However, the more common and clinically relevant defect leading to an open communication between the oral and nasal cavities, especially *behind* the incisive foramen, involves the failure of fusion of the **palatine shelves** with each other and the **nasal septum**.
Primitive heart tube formation US Medical PG Question 9: A 28-year-old woman with corrected transposition of the great arteries (L-TGA) who has been asymptomatic presents for preconception counseling. She has a systemic right ventricle supporting systemic circulation and asks about pregnancy risks. Her cardiologist notes mild tricuspid regurgitation. Evaluate the embryologic basis of her condition and synthesize recommendations regarding pregnancy.
- A. Simple transposition with late correction; pregnancy is safe with standard monitoring
- B. Both AV and ventriculoarterial discordance creating physiologically corrected circulation; pregnancy acceptable if systemic RV function normal, but requires high-risk obstetric and cardiology co-management (Correct Answer)
- C. Uncorrected transposition incompatible with pregnancy; recommend adoption
- D. Iatrogenic correction; pregnancy safe as anatomy is normalized
- E. Partial transposition; standard prenatal care is sufficient
Primitive heart tube formation Explanation: ***Both AV and ventriculoarterial discordance creating physiologically corrected circulation; pregnancy acceptable if systemic RV function normal, but requires high-risk obstetric and cardiology co-management***
- **L-TGA** involves **levo-looping** of the heart tube where the **morphologic right ventricle** (RV) supports the systemic circulation due to double discordance (atrioventricular and ventriculoarterial).
- Pregnancy is generally tolerated (maternal WHO class III) if **systemic RV function** is preserved, but requires multidisciplinary care to monitor for **heart failure**, **arrhythmias**, and worsening **tricuspid regurgitation**.
*Simple transposition with late correction; pregnancy is safe with standard monitoring*
- **D-TGA** (simple transposition) requires surgical correction (e.g., Arterial Switch) and has a distinct embryology involving failure of **conotruncal septation** spiral.
- Unlike L-TGA, corrected D-TGA carries different risks and would not be classified as having a "systemic right ventricle" if an **arterial switch** was performed.
*Uncorrected transposition incompatible with pregnancy; recommend adoption*
- **L-TGA** is "congenitally corrected," meaning blood flows in the correct physiological sequence; it is not inherently incompatible with pregnancy if the **systemic RV** is functional.
- Maternal mortality is not high enough to warrant absolute contraindication unless there is severe **RV dysfunction** or NYHA Class III/IV symptoms.
*Iatrogenic correction; pregnancy safe as anatomy is normalized*
- This condition is **congenitally corrected**, meaning the "correction" occurred during **embryogenesis** due to the double mismatch, not through surgery.
- The anatomy is never truly "normalized" because the **tricuspid valve** and **RV** are not designed for high-pressure systemic resistance, making pregnancy a high-risk event.
*Partial transposition; standard prenatal care is sufficient*
- There is no clinical entity termed "partial transposition" in this context; L-TGA is a complete, albeit **physiologically corrected**, malformation.
- Standard prenatal care is insufficient because the hemodynamic stress of pregnancy can trigger **systemic RV failure** or significant **heart block**.
Primitive heart tube formation US Medical PG Question 10: A newborn presents with severe cyanosis, hypoplastic right ventricle, pulmonary atresia, and an intact ventricular septum. The cardiologist notes this differs from tetralogy of Fallot despite both having pulmonary atresia. The neonatologist questions whether to maintain ductal patency or pursue immediate surgical intervention. Evaluate the embryologic differences and synthesize the optimal management strategy.
- A. Both result from infundibular deviation; maintain ductus with prostaglandins and perform staged repair
- B. Pulmonary atresia with intact septum results from primary valve failure; urgent surgical valvotomy or perforation
- C. Both are conotruncal defects; immediate complete repair is preferred
- D. Pulmonary atresia with intact septum results from primary valve failure; maintain ductus and evaluate RV-dependent coronary circulation before intervention (Correct Answer)
- E. Different embryologic timing but similar management; prostaglandin with elective repair at 6 months
Primitive heart tube formation Explanation: ***Pulmonary atresia with intact septum results from primary valve failure; maintain ductus and evaluate RV-dependent coronary circulation before intervention***
- Unlike Tetralogy of Fallot which is a **conotruncal defect**, Pulmonary Atresia with Intact Ventricular Septum (PA-IVS) is a primary **valvular failure** resulting in secondary right ventricular hypoplasia.
- It is critical to identify **RV-dependent coronary circulation** via sinusoids before any intervention, as decompressing the right ventricle in these patients can lead to fatal **myocardial ischemia**.
*Both result from infundibular deviation; maintain ductus with prostaglandins and perform staged repair*
- Only Tetralogy of Fallot results from the **anterior deviation** of the infundibular septum, whereas PA-IVS is characterized by a lack of communication between the RV and pulmonary artery without a VSD.
- While prostaglandins are used in both for **ductal patency**, the underlying embryologic mechanism and surgical risks differ significantly.
*Pulmonary atresia with intact septum results from primary valve failure; urgent surgical valvotomy or perforation*
- Although it is a primary valve failure, **urgent valvotomy** is contraindicated if there is **RV-dependent coronary circulation**.
- Releasing the high pressure in the RV can cause reversal of flow in **coronary sinusoids**, leading to sudden cardiac death.
*Both are conotruncal defects; immediate complete repair is preferred*
- PA-IVS is not a **conotruncal defect** because it lacks the malalignment of the outflow tract septum typically seen in Tetralogy or Transposition.
- **Complete repair** is often impossible in the neonatal period due to the **hypoplastic right ventricle** and anatomical constraints.
*Different embryologic timing but similar management; prostaglandin with elective repair at 6 months*
- Management is not similar because PA-IVS requires immediate mapping of the **coronary arteries** and high risk of **RV-dependent** flow.
- Elective repair at 6 months is often too late for stable management; these neonates require **prostaglandin (PGE1)** and early palliative or corrective intervention within the first weeks of life.
More Primitive heart tube formation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.