Congenital heart defects US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Congenital heart defects. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Congenital heart defects US Medical PG Question 1: A 43-year-old woman presents to her primary care provider with shortness of breath. She reports a 4-month history of progressively worsening difficulty breathing with associated occasional chest pain. She is a long-distance runner but has had trouble running recently due to her breathing difficulties. Her past medical history is notable for well-controlled hypertension for which she takes hydrochlorothiazide. She had a tibial osteosarcoma lesion with pulmonary metastases as a child and successfully underwent chemotherapy and surgical resection. She has a 10 pack-year smoking history but quit 15 years ago. She drinks a glass of wine 3 times per week. Her temperature is 98.6°F (37°C), blood pressure is 140/85 mmHg, pulse is 82/min, and respirations are 18/min. On exam, she has increased work of breathing with a normal S1 and loud P2. An echocardiogram in this patient would most likely reveal which of the following?
- A. Biventricular dilatation with a decreased ejection fraction
- B. Left ventricular dilatation with an incompetent aortic valve
- C. Left atrial dilatation with mitral valve stenosis
- D. Right ventricular hypertrophy with a dilated pulmonary artery (Correct Answer)
- E. Left ventricular hypertrophy with a bicuspid aortic valve
Congenital heart defects Explanation: The patient's history of **pulmonary metastases** (even successfully treated) and a **loud P2 heart sound** suggest **pulmonary hypertension**, which leads to increased afterload on the right ventricle. [1] **Pulmonary hypertension** causes the **right ventricle to hypertrophy** to overcome the elevated pulmonary arterial pressure, and the **pulmonary artery itself often dilates** due to the sustained high pressure. [1] [2] This describes **dilated cardiomyopathy**, which typically presents with **symptoms of heart failure** but doesn't specifically explain the **loud P2**, which points to pulmonary hypertension. [2]
Congenital heart defects US Medical PG Question 2: A male neonate is being examined by a pediatrician. His mother informs the doctor that she had a mild fever with rash, muscle pain, and swollen and tender lymph nodes during the second month of gestation. The boy was born at 39 weeks gestation via spontaneous vaginal delivery with no prenatal care. On physical examination, the neonate has normal vital signs. Retinal examination reveals the findings shown in the image. Which of the following congenital heart defects is most likely to be present in this neonate?
- A. Double outlet right ventricle
- B. Atrial septal defect
- C. Patent ductus arteriosus (Correct Answer)
- D. Ventricular septal defect
- E. Tetralogy of Fallot
Congenital heart defects Explanation: ***Patent ductus arteriosus***
- This neonate has **congenital rubella syndrome (CRS)** based on maternal symptoms during the first trimester (fever, rash, lymphadenopathy) and the characteristic **"salt and pepper" retinopathy** shown on retinal examination
- **PDA is the most common cardiac defect** associated with CRS, occurring in approximately 50-85% of affected infants
- Other cardiac manifestations of CRS include peripheral pulmonary artery stenosis, but PDA predominates
- The classic triad of CRS includes cardiac defects, ocular abnormalities (cataracts, glaucoma, retinopathy), and sensorineural deafness
*Double outlet right ventricle*
- This is a **conotruncal anomaly** typically presenting with cyanosis in the neonatal period
- Not associated with maternal rubella infection or congenital rubella syndrome
- Would present with abnormal ventricular anatomy and significant hemodynamic compromise
*Atrial septal defect*
- While ASD is a common congenital heart defect, it is **not characteristically associated with CRS**
- Much less frequently linked to maternal viral infections compared to PDA
- Often asymptomatic in the neonatal period and detected later in childhood
*Ventricular septal defect*
- VSD is less commonly associated with **congenital rubella syndrome** compared to PDA
- When present, typically manifests with a holosystolic murmur at the left lower sternal border
- Can occur with maternal infections but is not the predominant cardiac finding in CRS
*Tetralogy of Fallot*
- Consists of four anatomic abnormalities: VSD, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy
- Presents with **cyanosis** ("tet spells") and is not specifically linked to maternal rubella infection
- Not part of the congenital rubella syndrome spectrum
Congenital heart defects US Medical PG Question 3: A 2-year-old boy is presented to the pediatrician due to poor weight gain and easy fatigability. His mother states that the patient barely engages in any physical activity as he becomes short of breath easily. The prenatal and birth histories are insignificant. Past medical history includes a few episodes of upper respiratory tract infection that were treated successfully. The patient is in the 10th percentile for weight and 40th percentile for height. The vital signs include: heart rate 122/min and respirations 32/min. Cardiac auscultation reveals clear lungs and a grade 2/6 holosystolic murmur loudest at the left lower sternal border. The remainder of the physical examination is negative for clubbing, cyanosis, and peripheral edema. Which of the following is the most likely diagnosis in this patient?
- A. Tetralogy of Fallot (TOF)
- B. Atrial septal defect (ASD)
- C. Coarctation of aorta
- D. Ventricular septal defect (VSD) (Correct Answer)
- E. Patent ductus arteriosus (PDA)
Congenital heart defects Explanation: ***Ventricular septal defect (VSD)***
- A **holosystolic murmur** loudest at the **left lower sternal border**, poor weight gain, and easy fatigability in a 2-year-old are classic signs of a **VSD**.
- The symptoms arise from significant **left-to-right shunting**, leading to pulmonary overcirculation and heart failure symptoms.
*Tetralogy of Fallot (TOF)*
- TOF typically presents with **cyanosis** and **TET spells**, which are absent in this patient.
- The murmur in TOF is usually an **ejection systolic murmur**, not holosystolic, and often associated with a single loud S2.
*Atrial septal defect (ASD)*
- An ASD typically presents with a **fixed, split S2** and an **ejection systolic murmur** at the upper left sternal border due to increased flow across the pulmonic valve.
- Symptoms like poor weight gain and easy fatigability are less common in early childhood unless the shunt is very large.
*Coarctation of aorta*
- This condition is characterized by **femoral-radial delay** and **differential blood pressures** between the upper and lower extremities.
- The murmur is typically heard in the **back** or subclavicular region, and symptoms usually include poor feeding, lethargy, and sometimes heart failure.
*Patent ductus arteriosus (PDA)*
- PDA is classically associated with a **continuous "machinery-like" murmur** loudest below the left clavicle.
- While it can cause poor weight gain and fatigability, the type of murmur described is not consistent with a PDA.
Congenital heart defects US Medical PG Question 4: A 15-month-old boy is brought to the pediatrician for immunizations and assessment. His parents report that he is eating well and produces several wet diapers every day. He is occasionally fussy, but overall a happy and curious child. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. On physical examination his vital signs are stable. His weight and height are above the 85th percentile for his age and sex. On chest auscultation, the pediatrician detects a loud harsh holosystolic murmur over the left lower sternal border. The first and second heart sounds are normal. An echocardiogram confirms the diagnosis of the muscular ventricular septal defect without pulmonary hypertension. Which of the following is the best management strategy for this patient?
- A. Surgical closure of the defect using cardiopulmonary bypass
- B. Reassurance of the parents and regular follow-up (Correct Answer)
- C. Oral digoxin and regular follow-up
- D. Antibiotic prophylaxis against infective endocarditis
- E. Transcatheter occlusion closure of the defect
Congenital heart defects Explanation: **Reassurance of the parents and regular follow-up**
- Most **small muscular VSDs (Ventricular Septal Defects)**, especially in asymptomatic children with normal growth and no signs of heart failure or pulmonary hypertension, **close spontaneously**.
- Given the patient's normal development, stable vital signs, good feeding, and lack of pulmonary hypertension, a conservative approach with **monitoring for spontaneous closure** is appropriate.
*Surgical closure of the defect using cardiopulmonary bypass*
- **Surgical VSD closure** is typically reserved for large defects causing **symptoms, growth failure, pulmonary hypertension**, or those that fail to close spontaneously.
- The patient in the scenario is asymptomatic and thriving, which does not warrant an invasive procedure at this time.
*Oral digoxin and regular follow-up*
- **Digoxin** is a medication used to improve **cardiac contractility** and manage symptoms of **heart failure**, which this patient does not exhibit.
- It would only be considered if there were signs of **congestive heart failure** due to a large VSD, which is not the case here.
*Antibiotic prophylaxis against infective endocarditis*
- Current guidelines from the American Heart Association (AHA) generally **do not recommend routine antibiotic prophylaxis** for VSDs unless there's a history of infective endocarditis or uncorrected cyanotic heart disease.
- The risk of **infective endocarditis** is very low in isolated VSDs and the potential side effects of prophylactic antibiotics outweigh the benefits.
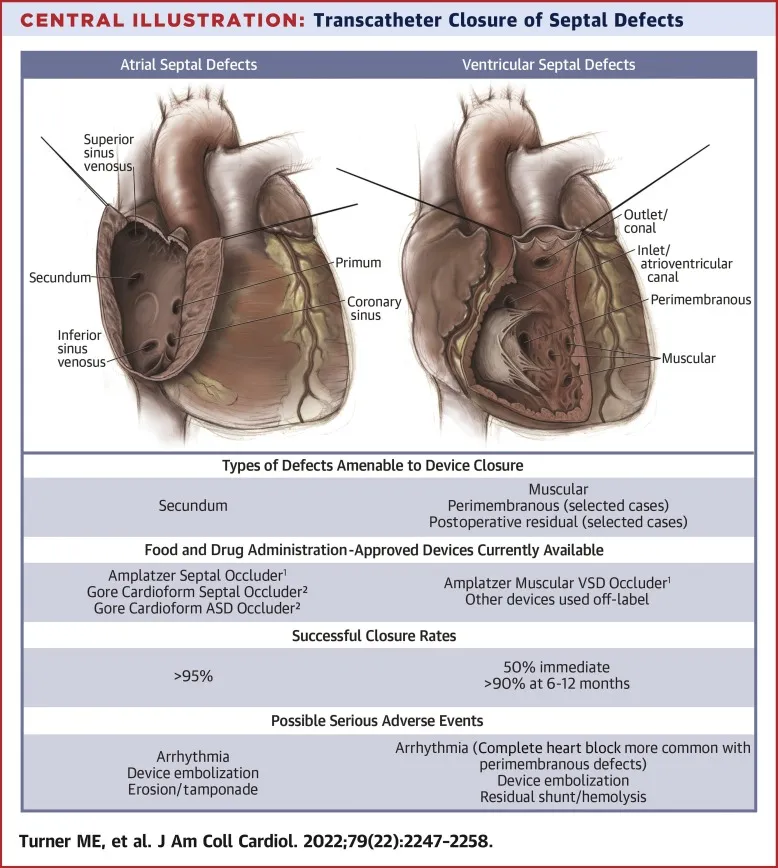
*Transcatheter occlusion closure of the defect*
- **Transcatheter closure** is an option for certain types of VSDs, often **muscular VSDs**, but typically for those that are **larger, symptomatic**, and have not closed spontaneously.
- Similar to surgical closure, this invasive procedure is not indicated for an **asymptomatic, thriving child** with a muscular VSD that is likely to close on its own.
Congenital heart defects US Medical PG Question 5: The medical student on the pediatric cardiology team is examining a 9-year-old girl who was referred by her primary care physician for unexplained hypertension. She is accompanied by her mother who reveals that the child is generally well but has been significantly less active than her peers for the past year. On exam, the medical student notes a thin girl in no apparent distress appearing slightly younger than stated age. Vital signs reveal a BP is 160/80, HR 80, RR 16. Physical exam is notable only for a clicking sound is noted around the time of systole but otherwise the cardiac exam is normal. Pedal pulses could not be palpated. Which of the following physical exam findings was most likely missed by both the medical student and primary care physician?
- A. Long philtrum
- B. Prominent occiput
- C. Webbed neck (Correct Answer)
- D. Cleft palate
- E. Single palmar crease
Congenital heart defects Explanation: ***Webbed neck***
- The combination of **hypertension** with **unpalpable pedal pulses** and a **systolic click** in a pediatric patient strongly suggests **coarctation of the aorta**.
- **Webbed neck** (or **pterygium colli**) is a classic phenotypic feature associated with **Turner syndrome**, which frequently co-occurs with coarctation of the aorta.
*Long philtrum*
- A **long philtrum** is a craniofacial feature sometimes associated with certain genetic syndromes like **fetal alcohol syndrome** or **Marfan syndrome**, but it is not specifically linked to coarctation of the aorta or Turner syndrome.
- While these syndromes can have cardiovascular manifestations, a long philtrum does not directly point to the specific findings presented.
*Prominent occiput*
- A **prominent occiput** is a non-specific finding that can be seen in various conditions, including some **chromosomal abnormalities** or **skeletal dysplasias**.
- It is not a characteristic feature of **Turner syndrome** or **coarctation of the aorta**.
*Cleft palate*
- **Cleft palate** is a birth defect affecting the roof of the mouth, often associated with a wide range of genetic or environmental factors.
- While patients with cleft palate can have associated congenital heart defects, it is not a direct or common association with **Turner syndrome** or **coarctation of the aorta**.
*Single palmar crease*
- A **single palmar crease** (simian crease) is a dermatoglyphic feature often associated with **Down syndrome** (Trisomy 21).
- While Down syndrome is associated with various congenital heart defects (e.g., AV septal defect), it is not typically associated with **coarctation of the aorta** or **Turner syndrome**.
Congenital heart defects US Medical PG Question 6: A 4-year-old Caucasian male suffers from cyanosis and dyspnea relieved by squatting. Which of the following abnormalities is most likely present?
- A. Atrial septal defect
- B. Coarctation of the aorta
- C. Bicuspid aortic valve
- D. Ventricular septal defect
- E. Tetralogy of Fallot (Correct Answer)
Congenital heart defects Explanation: ***Tetralogy of Fallot***
- **Cyanosis** and **dyspnea relieved by squatting** are the hallmark clinical features of **Tetralogy of Fallot**, making this the correct diagnosis.
- The condition consists of four anatomic abnormalities: **ventricular septal defect (VSD)**, **right ventricular outflow tract obstruction**, **right ventricular hypertrophy**, and **overriding aorta**.
- The right-to-left shunt across the VSD causes **deoxygenated blood** to enter systemic circulation, producing **cyanosis**.
- **Squatting increases systemic vascular resistance (SVR)**, which decreases the right-to-left shunt, improves pulmonary blood flow, and relieves cyanosis and dyspnea during **"tet spells"**.
*Atrial septal defect*
- ASDs typically cause **left-to-right shunts** and are **acyanotic lesions**.
- Patients may be asymptomatic or present with **exertional dyspnea** and **fatigue** in later childhood or adulthood.
- Cyanosis would only occur if **Eisenmenger syndrome** develops (reversal to right-to-left shunt due to pulmonary hypertension), which is rare at age 4 and does not improve with squatting.
*Coarctation of the aorta*
- This is an **acyanotic** lesion characterized by **narrowing of the descending aorta**.
- Classic findings include **upper extremity hypertension**, **diminished or delayed femoral pulses**, and **lower extremity hypotension**.
- Does not cause cyanosis or squatting relief.
*Bicuspid aortic valve*
- A common **acyanotic** congenital abnormality that may lead to **aortic stenosis** or **regurgitation** over time.
- Usually asymptomatic in childhood; may present with **murmur**, chest pain, or syncope in adulthood.
- Does not cause cyanosis or relief with squatting.
*Ventricular septal defect*
- Isolated VSDs typically cause **left-to-right shunts** and are **acyanotic**.
- May present with **heart failure symptoms** (tachypnea, poor feeding, failure to thrive) in infancy if the defect is large.
- Cyanosis occurs only if **Eisenmenger syndrome** develops (usually takes years to decades), and symptoms are not relieved by squatting.
Congenital heart defects US Medical PG Question 7: A 69-year-old smoker presents to physician after noticing that his face seems to be more swollen than usual. Upon further questioning, he reports increasing shortness of breath and cough over the past 6 months. On exam, his physician notices venous distention in his neck and distended veins in the upper chest and arms. Chest radiograph shows a right upper lobe mass. What is the embryologic origin of the vessel being compressed by this patient's tumor?
- A. Cardinal veins (Correct Answer)
- B. Primitive ventricle
- C. Left horn of sinus venosus
- D. Truncus arteriosus
- E. Bulbus cordis
Congenital heart defects Explanation: ***Cardinal veins***
- The symptoms of facial swelling, neck vein distention, and upper chest/arm vein distention, especially with a right upper lobe mass, are classic for **superior vena cava (SVC) syndrome**.
- The **SVC** is formed from the fusion of the anterior **cardinal veins**, which drain the upper body during embryonic development.
*Primitive ventricle*
- The **primitive ventricle** develops into parts of the left and right **ventricles** of the heart.
- It is not directly involved in the formation of major systemic veins like the SVC.
*Left horn of sinus venosus*
- The **left horn of the sinus venosus** mostly regresses and contributes to structures like the **coronary sinus** and the oblique vein of the left atrium.
- It does not form the SVC, which drains the upper body.
*Truncus arteriosus*
- The **truncus arteriosus** is an embryonic structure that separates to form the **aorta** and the **pulmonary artery**.
- It is an arterial structure, not a venous structure that would be compressed in SVC syndrome.
*Bulbus cordis*
- The **bulbus cordis** develops into the **conus arteriosus** (infundibulum) of the right ventricle and the **aortic vestibule** of the left ventricle.
- Like the truncus arteriosus, it is involved in arterial outflow tracts and not the formation of the SVC.
Congenital heart defects US Medical PG Question 8: A 2-year-old child is brought to the emergency department with rapid breathing and a severe cyanotic appearance of his lips, fingers, and toes. He is known to have occasional episodes of mild cyanosis, especially when he is extremely agitated. This is the worst episode of this child’s life, according to his parents. He was born with an APGAR score of 8 via a normal vaginal delivery. His development is considered delayed compared to children of his age. History is significant for frequent squatting after strenuous activity. On auscultation, there is evidence of a systolic ejection murmur at the left sternal border. On examination, his oxygen saturation is 71%, blood pressure is 81/64 mm Hg, respirations are 42/min, pulse is 129/min, and temperature is 36.7°C (98.0°F). Which of the following will most likely be seen on chest x-ray (CXR)?
- A. Egg on a string
- B. Boot-shaped heart (Correct Answer)
- C. Increased pulmonary vascular markings
- D. Cardiomegaly with globular heart
- E. Figure-3 sign
Congenital heart defects Explanation: ***Boot-shaped heart***
- The patient's presentation with **cyanosis**, **squatting spells**, and a **systolic ejection murmur** is classic for **Tetralogy of Fallot** (TOF).
- A **boot-shaped heart** (Coeur en sabot) on chest X-ray is a characteristic finding in TOF, caused by **right ventricular hypertrophy** and an upturned cardiac apex, leading to a concave pulmonary artery segment.
*Egg on a string*
- This CXR finding is characteristic of **Transposition of the Great Arteries (TGA)**, where the aorta and pulmonary artery are switched, creating an "egg" outline with a narrow vascular pedicle ("string").
- TGA typically presents with severe **cyanosis** from birth and does not usually involve squatting spells or a loud systolic murmur from a prominent **right ventricular outflow tract obstruction**.
*Increased pulmonary vascular markings*
- This finding is common in conditions with **left-to-right shunting** or **increased pulmonary blood flow**, such as a **ventricular septal defect (VSD)** or **patent ductus arteriosus (PDA)**.
- In Tetralogy of Fallot, there is typically **decreased pulmonary blood flow** due to **pulmonic stenosis**, leading to *decreased* pulmonary vascular markings.
*Cardiomegaly with globular heart*
- A **globular heart** is a non-specific finding often associated with **pericardial effusion** or **dilated cardiomyopathy**, where the heart appears enlarged and rounded.
- While TOF can cause cardiomegaly (specifically **right ventricular hypertrophy**), the characteristic shape is "boot-shaped," not globally enlarged or globular.
*Figure-3 sign*
- The **figure-3 sign** on CXR is pathognomonic for **aortic coarctation**, caused by indentation of the aorta at the coarctation site and post-stenotic dilation.
- This condition presents with signs of **heart failure**, **differential cyanosis** (if preductal), and **blood pressure discrepancies** between upper and lower extremities, not the cyanotic spells and squatting seen in this case.
Congenital heart defects US Medical PG Question 9: A 5-day-old boy is brought to the emergency department by his mother because of a 2-day history of difficulty feeding and multiple episodes of his lips turning blue. He was born at home via spontaneous vaginal delivery and Apgar scores were 7 and 8 at 1 and 5 minutes, respectively. Physical examination shows grunting and moderate intercostal and subcostal retractions. Echocardiography shows a single vessel exiting from the heart. Which of the following is the most likely underlying cause of this patient's condition?
- A. Abnormal placement of the infundibular septum
- B. Absent fusion of septum primum and septum secundum
- C. Failure of neural crest cell migration (Correct Answer)
- D. Insufficient growth of endocardial cushions
- E. Abnormal cardiac looping
Congenital heart defects Explanation: ***Failure of neural crest cell migration***
- The echocardiography finding of a **single vessel exiting the heart** is characteristic of **truncus arteriosus**, a congenital heart defect.
- This condition arises from the **failure of neural crest cells** to migrate properly and spiralize the **aortopulmonary septum**, which normally divides the truncus arteriosus into the aorta and pulmonary artery.
*Abnormal placement of the infundibular septum*
- Abnormal placement of the infundibular septum is typically associated with **Tetralogy of Fallot**, leading to an overriding aorta, pulmonary stenosis, ventricular septal defect, and right ventricular hypertrophy.
- While Tetralogy of Fallot is a cyanotic heart disease, it presents with a **bifurcated outflow tract** not a single great vessel.
*Absent fusion of septum primum and septum secundum*
- The absent fusion of the **septum primum** and **septum secundum** results in a **patent foramen ovale** or an **atrial septal defect**.
- These defects primarily cause left-to-right shunting, leading to volume overload in the right heart, but do not explain the presence of a single great vessel.
*Insufficient growth of endocardial cushions*
- Insufficient growth of the **endocardial cushions** can lead to **atrioventricular septal defects** and certain types of **ventricular septal defects**.
- These conditions involve issues with valve formation and septal development but do not directly cause a single great vessel to exit the heart.
*Abnormal cardiac looping*
- Abnormal cardiac looping is associated with conditions like **dextrocardia** or **transposition of the great arteries**.
- While **transposition of the great arteries** also causes cyanosis, it involves **two great vessels** that are improperly connected, not a single great vessel.
Congenital heart defects US Medical PG Question 10: Shortly after delivery, a female newborn develops bluish discoloration of the lips, fingers, and toes. She was born at term to a 38-year-old primigravid woman. Pregnancy was complicated by maternal diabetes mellitus. Pulse oximetry on room air shows an oxygen saturation of 81%. Echocardiography shows immediate bifurcation of the vessel arising from the left ventricle; the vessel emerging from the right ventricle gives out coronary, head, and neck vessels. An abnormality in which of the following developmental processes most likely accounts for this patient's condition?
- A. Alignment of infundibular septum
- B. Fusion of endocardial cushion
- C. Spiraling of aorticopulmonary septum (Correct Answer)
- D. Separation of tricuspid valve tissue from myocardium
- E. Division of aorta and pulmonary artery
Congenital heart defects Explanation: ***Spiraling of aorticopulmonary septum***
- The description of a vessel arising from the left ventricle that immediately bifurcates (pulmonary artery) and a vessel from the right ventricle that gives off coronary, head, and neck vessels (aorta) is characteristic of **transposition of the great arteries (TGA)**.
- TGA results from a failure of the **aorticopulmonary septum** to spiral during embryological development, leading to the aorta originating from the right ventricle and the pulmonary artery from the left ventricle.
*Alignment of infundibular septum*
- Abnormal alignment of the infundibular septum is associated with conditions like **tetralogy of Fallot**, which involves a maligned interventricular septum and a shifted aorta, presenting with a different set of echocardiographic findings.
- While also a **cyanotic heart defect**, tetralogy of Fallot's anatomy (e.g., interventricular septal defect, pulmonary stenosis) differs from the described TGA.
*Fusion of endocardial cushion*
- Failure of fusion of the **endocardial cushions** leads to **atrioventricular septal defects**, which involve defects in both the atria and ventricular septa, and often affect the mitral and tricuspid valves.
- These defects typically present with heart failure symptoms and different echocardiographic findings than those described for TGA.
*Separation of tricuspid valve tissue from myocardium*
- An abnormality in the separation of tricuspid valve tissue from the myocardium is the cause of **Ebstein anomaly**, where the tricuspid valve leaflets are displaced downwards into the right ventricle, leading to tricuspid regurgitation.
- Ebstein anomaly is characterized by right atrial enlargement and a largely functional right ventricle, leading to issues with right heart output but not the great artery transposition described.
*Division of aorta and pulmonary artery*
- The division of the truncus arteriosus into the aorta and pulmonary artery is a normal developmental process, which when complete usually produces the correct great artery connections. However, the exact arrangement of these vessels is determined by the **spiraling of the aorticopulmonary septum**, not just the division itself.
- Failure of this division, resulting in a **persistent truncus arteriosus**, would present as a single great artery arising from both ventricles, which is distinct from the two separate but transposed vessels seen in TGA.
More Congenital heart defects US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.