Atrial septation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Atrial septation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Atrial septation US Medical PG Question 1: An obese 37-year-old woman is brought to the emergency department 2 hours after the onset of weakness in her left arm and leg. She fell from the stairs the day prior but did not have any loss of consciousness or nausea after the fall. She travels to Asia regularly on business; her last trip was 4 days ago. She has no history of serious illness. Her only medication is an oral contraceptive. Her temperature is 37.8°C (100°F), pulse is 113/min and regular, and blood pressure is 162/90 mm Hg. Examination shows decreased muscle strength on the left side. Deep tendon reflexes are 4+ on the left. Babinski sign is present on the left. The right lower leg is swollen, erythematous, and tender to palpation. Further evaluation is most likely to show which of the following?
- A. Atrial fibrillation
- B. Patent foramen ovale (Correct Answer)
- C. Atrial myxoma
- D. Ventricular septal defect
- E. Carotid artery dissection
Atrial septation Explanation: ***Patent foramen ovale***
- This patient presents with a **cryptogenic stroke** (stroke of undetermined cause) in the context of being **obese**, taking **oral contraceptives**, recent **long-distance travel**, and symptoms of a **deep vein thrombosis (DVT)** in her right leg.
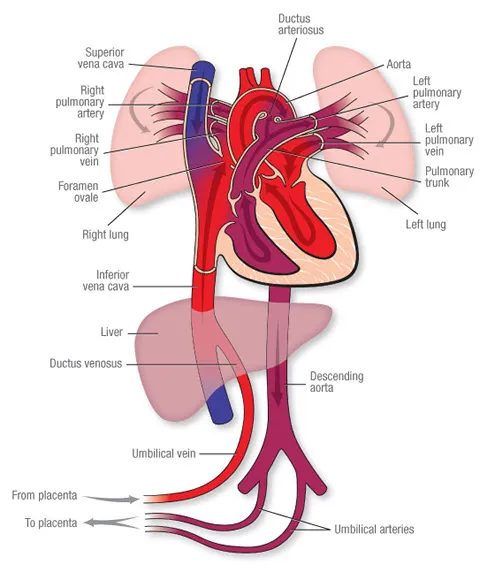
- A **paradoxical embolism** through a **patent foramen ovale (PFO)** is a strong possibility, where a clot from the DVT could bypass the pulmonary circulation and enter the systemic circulation, leading to a stroke.
*Atrial fibrillation*
- While **atrial fibrillation** is a common cause of **embolic stroke**, the patient's pulse is described as **regular**, making this diagnosis less likely.
- There are no other indications of atrial fibrillation on physical exam, such as an irregularly irregular pulse.
*Atrial myxoma*
- An **atrial myxoma** can cause **embolic stroke** due to tumor fragments breaking off, but this is a rare cause.
- There are no other signs or symptoms suggestive of a cardiac tumor, such as constitutional symptoms or cardiac murmurs.
*Ventricular septal defect*
- A **ventricular septal defect (VSD)** typically causes a left-to-right shunt and is associated with a **loud holosystolic murmur** at the lower left sternal border.
- While a **right-to-left shunt** can occur in the presence of **pulmonary hypertension (Eisenmenger syndrome)**, there is no mention of a murmur or signs of pulmonary hypertension.
*Carotid artery dissection*
- **Carotid artery dissection** can cause stroke, often preceded by **neck pain** or **headache**, which is not reported by the patient.
- The presence of a **DVT** and associated risk factors for thromboembolism makes a paradoxical embolism a more probable cause in this clinical scenario.
Atrial septation US Medical PG Question 2: A 9-year-old boy is brought to the clinic by his parents for an annual wellness examination. He is a relatively healthy boy who was born at term via vaginal delivery. He is meeting his developmental milestones and growth curves and is up-to-date on his immunizations. The father complains that he is picky with his food and would rather eat pizza. The patient denies any trouble at school, fevers, pain, or other concerns. A physical examination demonstrates a healthy boy with a grade 3 midsystolic ejection murmur at the second intercostal space that does not disappear when he sits up. What is the most likely explanation for this patient’s findings?
- A. Physiologic conditions outside the heart
- B. Inflammation of the visceral and parietal pericardium
- C. Failure of the septum primum to fuse with the endocardial cushions
- D. Defect of the septum secundum (Correct Answer)
- E. Prolonged patency of the ductus arteriosus
Atrial septation Explanation: **Defect of the septum secundum**
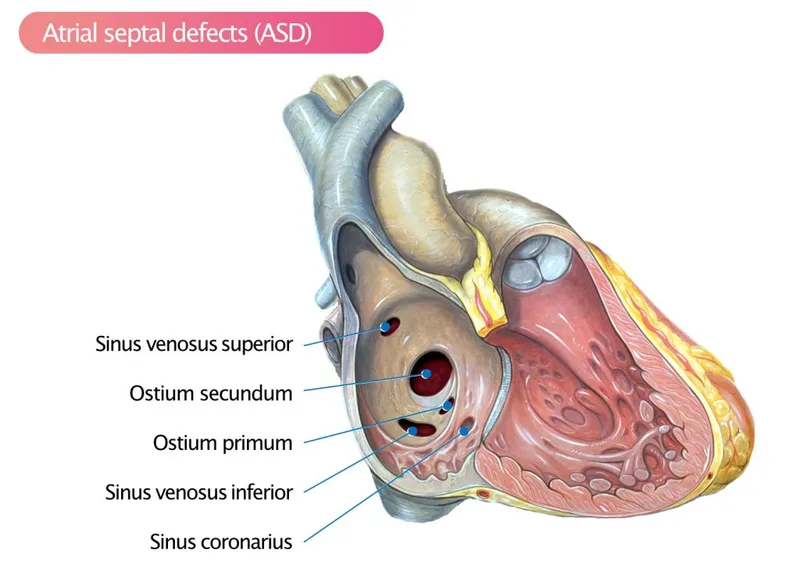
- A **grade 3 midsystolic ejection murmur** that does not disappear when sitting up in an otherwise healthy 9-year-old child is characteristic of an **atrial septal defect (ASD)**.
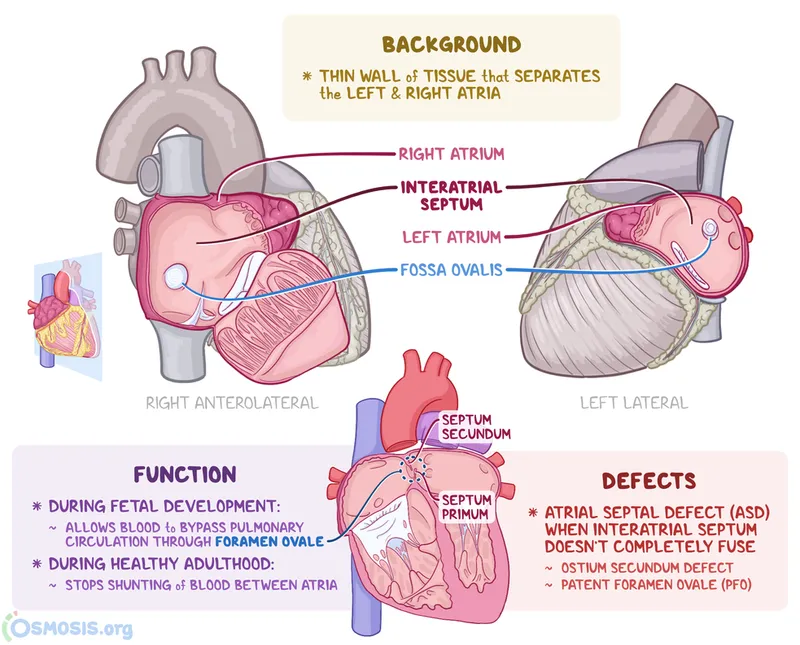
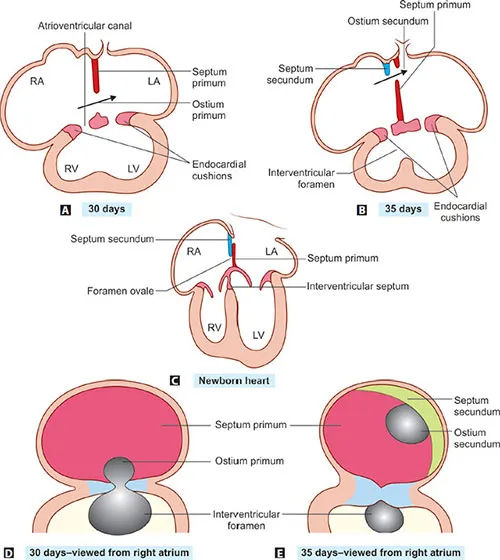
- Defects of the **septum secundum** are the most common type of ASD, allowing blood to shunt from the left to the right atrium, leading to increased pulmonary blood flow and the generation of such a murmur.
*Physiologic conditions outside the heart*
- A **physiologic murmur** (also known as a Still's murmur) is typically described as a grade 1-2 innocent murmur that often disappears or changes with positional changes (e.g., sitting up).
- The **grade 3 intensity** and persistence with positional changes make a common physiologic murmur less likely in this case.
*Inflammation of the visceral and parietal pericardium*
- **Pericarditis** typically presents with chest pain that can worsen with inspiration and lying down, and a characteristic **pericardial friction rub**, not a midsystolic ejection murmur.
- This condition is unlikely in an otherwise healthy child with no other systemic symptoms or signs of inflammation.
*Failure of the septum primum to fuse with the endocardial cushions*
- This describes a **primum ASD**, which is a type of ASD often associated with **endocardial cushion defects** and other congenital heart anomalies, such as cleft mitral valve.
- While it is a type of ASD, the description typically refers to the larger, more clinically significant defects and doesn't explicitly refer to the most common type of ASD, which is the septum secundum defect.
*Prolonged patency of the ductus arteriosus*
- A **patent ductus arteriosus (PDA)** produces a **continuous, machine-like murmur** that is typically heard best at the left upper sternal border.
- The murmur described in the patient is a **midsystolic ejection murmur**, which is distinct from the continuous murmur of a PDA.
Atrial septation US Medical PG Question 3: A 2-year-old girl is brought to the physician by her mother for a well-child examination. Cardiac auscultation is shown. When she clenches her fist forcefully for a sustained time, the intensity of the murmur increases. Which of the following is the most likely cause of this patient's auscultation findings?
- A. Failure of the ductus arteriosus to close
- B. Defect in the atrial septum
- C. Fusion of the right and left coronary leaflets
- D. Prolapse of the mitral valve
- E. Defect in the ventricular septum (Correct Answer)
Atrial septation Explanation: ***Defect in the ventricular septum***
- A **ventricular septal defect (VSD)** causes a holosystolic, harsh murmur, often loudest at the **left lower sternal border**.
- **Clenching the fist forcefully increases systemic vascular resistance (afterload)**, which enhances the left-to-right shunting through a VSD, thereby **increasing the intensity** of the murmur.
*Failure of the ductus arteriosus to close*
- A **patent ductus arteriosus (PDA)** typically presents with a **continuous "machinery-like" murmur**, not one that increases with clenching a fist.
- The murmur of a PDA is usually best heard in the **pulmonary area** (left upper sternal border).
*Defect in the atrial septum*
- An **atrial septal defect (ASD)** usually causes a **systolic ejection murmur** over the pulmonic area due to increased flow across the pulmonary valve, and a **fixed split S2**.
- Its intensity is generally **not significantly altered by acute changes in systemic vascular resistance** like clenching a fist.
*Fusion of the right and left coronary leaflets*
- This description is characteristic of a **bicuspid aortic valve** leading to **aortic stenosis**.
- Aortic stenosis typically causes a **systolic ejection murmur** that **decreases** in intensity with maneuvers that increase afterload (like clenching a fist) due to reduced stroke volume.
*Prolapse of the mitral valve*
- **Mitral valve prolapse (MVP)** is characterized by a **mid-systolic click** followed by a **late-systolic murmur**.
- **Increasing afterload** (clenching a fist) would typically **delay the click and shorten the murmur**, or make it softer, as it *reduces* the degree of prolapse.
Atrial septation US Medical PG Question 4: A 4-year-old male is brought into your office because his mother states he has been fatigued. He has not been acting like himself and has been getting tired easily while running around and playing with other children. As of last week, he has also been complaining of being short of breath. His vitals are temperature 98.6 deg F (37.2 deg C), blood pressure 100/75 mmHg, pulse 98/min, and respirations 22/min. On exam, the patient is short of breath, and there is a holosystolic murmur with an appreciable thrill along the left sternal border. There are no other noticeable abnormalities, and the mother states that the child's prenatal course along with genetic testing was normal. What is the most likely diagnosis?
- A. Atrial septal defect (ASD)
- B. Endocardial cushion defect
- C. Ventricular septal defect (VSD) (Correct Answer)
- D. Patent ductus arteriosus (PDA)
- E. Tetralogy of Fallot
Atrial septation Explanation: ***Ventricular septal defect (VSD)***
- A **holosystolic murmur** at the **left sternal border** with an associated **thrill** is a classic finding for a VSD.
- The patient's fatigue and shortness of breath (evidencing activity intolerance) are signs of **left-to-right shunting** causing increased pulmonary blood flow and eventual heart failure.
*Atrial septal defect (ASD)*
- An ASD typically presents with a **systolic ejection murmur** at the upper left sternal border due to increased flow across the pulmonic valve, not a holosystolic murmur.
- While it can cause fatigue and dyspnea, a thrill is less common, and the murmur quality is distinct.
*Endocardial cushion defect*
- This defect involves the atrioventricular septum, often resulting in a **split S2** and a **holosystolic murmur** best heard at the lower left sternal border.
- However, it is strongly associated with **Down syndrome**, which is ruled out by the normal genetic testing.
*Patent ductus arteriosus (PDA)*
- PDA is characterized by a **continuous "machinery" murmur** best heard below the left clavicle, which is distinct from the holosystolic murmur described.
- The associated symptoms of fatigue and dyspnea can occur, but the murmur differentiates it.
*Tetralogy of Fallot*
- This condition presents with **cyanosis** and a **crescendo-decrescendo systolic ejection murmur** at the left sternal border, not a holosystolic murmur with a thrill.
- Patients often exhibit "tet spells" and **clubbing**, which are absent in this presentation.
Atrial septation US Medical PG Question 5: A 26-year-old man is brought to the emergency department due to right-sided facial and upper extremity weakness and aphasia. The patient was in his usual state of health until two hours prior to presentation, when he was eating breakfast with a friend and acutely developed the aforementioned symptoms. Medical history is unremarkable except for mild palpitations that occur during times of stress or when drinking coffee. Physical examination is consistent with the clinical presentation. Laboratory testing is unremarkable and a 12-lead electrocardiogram is normal. A non-contrast head CT and diffusion-weighted MRI shows no intracranial hemorrhage and an isolated superficial cerebral infarction. Transthoracic echocardiography with agitated saline mixed with air shows microbubbles in the left heart. There is a possible minor effusion surrounding the heart and the ejection fraction is within normal limits. Which of the following is most likely the cause of this patient's clinical presentation?
- A. Aortic embolism
- B. Amyloid deposition within vessels
- C. Cardiac arrhythmia
- D. Berry aneurysm rupture
- E. Patent foramen ovale (Correct Answer)
Atrial septation Explanation: ***Patent foramen ovale***
- The presence of **microbubbles in the left heart** after agitated saline injection, combined with a **superficial cerebral infarction** in a young patient with an otherwise unremarkable medical history, is highly suggestive of a **paradoxical embolism** through a patent foramen ovale (PFO).
- A PFO allows venous clots to bypass the pulmonary circulation and enter the systemic arterial circulation, leading to a stroke.
*Aortic embolism*
- While an aortic embolism can lead to stroke, there is no evidence provided (e.g., severe **aortic atherosclerosis**, valvular disease) to suggest an aortic source for the embolism.
- The echocardiogram showing microbubbles passing from right to left heart points more strongly towards an intracardiac shunt.
*Amyloid deposition within vessels*
- **Cerebral amyloid angiopathy** typically affects older individuals and presents with **lobar hemorrhages** rather than isolated ischemic stroke.
- Furthermore, there is no imaging or pathological evidence to suggest amyloid deposition.
*Cardiac arrhythmia*
- Although **cardiac arrhythmias** (e.g., **atrial fibrillation**) are a common cause of embolic stroke, the **normal 12-lead ECG** and the specific echocardiographic finding of microbubbles crossing the heart make an arrhythmia less likely to be the direct cause of this specific embolic event.
- The mild palpitations are non-specific and are likely stress-induced.
*Berry aneurysm rupture*
- **Berry aneurysm rupture** causes a **subarachnoid hemorrhage**, which would be visible on non-contrast CT and would present with sudden, severe headache, not an isolated ischemic stroke.
- The imaging showed no intracranial hemorrhage, ruling out this diagnosis.
Atrial septation US Medical PG Question 6: An 18-month-old boy presents to the pediatrician by his mother for a routine check-up. The mother has no concerns, although she asks about the "hole in his heart" that the patient had at birth. The patient has no history of cyanosis or heart failure; however, a holosystolic, harsh murmur was noted at the 3- and 6-month check-ups. On examination, the patient is playful and alert. He has met all developmental milestones. The cardiac examination reveals a regular rate and rhythm with persistence of the holosystolic, harsh murmur. What is the most likely cause of the murmur in this child?
- A. Patent foramen ovale
- B. Defect of muscular interventricular septum
- C. Failure of endocardial cushion to form
- D. Defect of the membranous interventricular septum (Correct Answer)
- E. Defective dynein functioning
Atrial septation Explanation: ***Defect of the membranous interventricular septum***
- A **holosystolic, harsh murmur** is characteristic of a **ventricular septal defect (VSD)**, particularly one in the membranous septum due to its common occurrence and typical presentation.
- The patient's lack of cyanosis or heart failure, despite the persistent murmur since birth, suggests a small to moderate VSD, which can often remain asymptomatic and sometimes close spontaneously.
*Patent foramen ovale*
- A **patent foramen ovale (PFO)** typically produces no murmur or a soft systolic ejection murmur, not a harsh holosystolic murmur.
- PFOs are usually asymptomatic unless there's a significant pressure difference causing a right-to-left shunt, which is not indicated here.
*Failure of endocardial cushion to form*
- Failure of the **endocardial cushions** to form leads to **atrioventricular septal defects (AVSDs)**, which typically present with a combination of murmurs (systolic and sometimes diastolic) and often with symptoms of heart failure and recurrent respiratory infections.
- AVSDs are usually associated with **Down syndrome** and present with more severe clinical features than described.
*Defect of muscular interventricular septum*
- While a **muscular VSD** can cause a holosystolic murmur, it often has a **rougher, "swiss cheese" appearance** on imaging due to multiple defects and is less common than membranous VSDs.
- Small muscular VSDs are more prone to spontaneous closure and may have a different murmur intensity or location.
*Defective dynein functioning*
- **Defective dynein functioning** causes conditions like **Kartagener syndrome** (a type of primary ciliary dyskinesia), characterized by **situs inversus**, chronic sinusitis, bronchiectasis, and infertility.
- This condition does not directly cause an isolated holosystolic heart murmur or structural heart defects like a VSD.
Atrial septation US Medical PG Question 7: A patient in the neonatal intensive care unit develops severe cyanosis. Cardiac exam reveals a single loud S2 with a right ventricular heave. Echocardiography reveals an aorta lying anterior and right of the pulmonary artery. Which of the following processes failed during fetal development?
- A. Aorticopulmonary septum to spiral (Correct Answer)
- B. Reentry of viscera from yolk sac
- C. Fusion of the membranous ventricular septum
- D. Fusion of septum primum and septum secondum
- E. Constriction by ductal tissue
Atrial septation Explanation: ***Aorticopulmonary septum to spiral***
- The clinical presentation describes **transposition of the great arteries (TGA)**, characterized by **severe cyanosis**, a **single loud S2**, and the **aorta lying anterior and right of the pulmonary artery**.
- TGA results from the failure of the **aorticopulmonary septum** to spiral correctly during development, causing the aorta to originate from the right ventricle and the pulmonary artery from the left ventricle.
*Reentry of viscera from yolk sac*
- Failure of this process leads to **omphalocele** or **gastroschisis**, which are abdominal wall defects with extrusion of visceral organs.
- These conditions do not cause severe neonatal cyanosis or specific cardiac malformations like TGA.
*Constriction by ductal tissue*
- This refers to the mechanism of **coarctation of the aorta**, where ectopic ductal tissue causes narrowing of the aortic arch.
- While coarctation can cause cyanosis in the lower body, it does not cause transposition of the great vessels and would not present with the echocardiographic findings described.
*Fusion of the membranous ventricular septum*
- Failure of fusion of the membranous ventricular septum results in a **ventricular septal defect (VSD)**.
- While a VSD can be associated with TGA, it is not the fundamental embryological defect that causes the transposition of the great arteries.
*Fusion of septum primum and septum secondum*
- Failure of fusion between the **septum primum** and **septum secundum** leads to an **atrial septal defect (ASD)**.
- An ASD allows for mixing of blood at the atrial level but is not the primary cause of the transposed great arteries.
Atrial septation US Medical PG Question 8: A 7-year-old boy is brought by his parents to his pediatrician due to progressive fatigue and shortness of breath while playing sports. He is otherwise healthy with no known medical disorders and no other symptoms. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. On physical examination, his temperature is 36.9ºC (98.4ºF), pulse rate is 90/min, blood pressure is 100/70 mm Hg, and respiratory rate is 18/min. Pulses in all four extremities are equal and normally palpated; there is no radio-femoral delay. The pediatrician suspects a congenital heart disease after auscultation of the heart. Which of the following congenital heart diseases is most likely to present with the clinical features listed above?
- A. Atrial septal defect (Correct Answer)
- B. Double-outlet right ventricle with subaortic ventricular septal defect
- C. Coarctation of the aorta
- D. Aortopulmonary window defect
- E. Complete atrioventricular septal defect
Atrial septation Explanation: ***Atrial septal defect***
- An **atrial septal defect (ASD)** typically presents in older children or adults with symptoms like **fatigue** and **shortness of breath on exertion (dyspnea)** due to increased pulmonary blood flow, after years of being asymptomatic.
- The absence of cyanosis and normal pulses are consistent with an ASD, as it's typically an **acyanotic heart defect** where shunting occurs from left to right.
*Double-outlet right ventricle with subaortic ventricular septal defect*
- This condition involves both great arteries originating from the **right ventricle**, often leading to **cyanosis** from birth or early infancy due to mixing of oxygenated and deoxygenated blood.
- Patients typically present much earlier with signs of **heart failure**, **cyanosis**, and **failure to thrive**, which are not reported in this 7-year-old boy.
*Coarctation of the aorta*
- **Coarctation of the aorta** is characterized by a **narrowing of the aorta**, leading to a classic finding of **radio-femoral delay** and **different blood pressures in the upper and lower extremities**, which are specifically stated to be absent in this patient.
- While it can cause shortness of breath and fatigue, the lack of radio-femoral delay makes this diagnosis unlikely.
*Aortopulmonary window defect*
- An **aortopulmonary window (APW)** is a rare defect involving a communication between the aorta and pulmonary artery, usually presenting in **infancy** with severe symptoms of **heart failure** and **pulmonary hypertension** due to a large left-to-right shunt.
- This patient's presentation at 7 years of age without early severe symptoms makes APW less likely.
*Complete atrioventricular septal defect*
- A **complete atrioventricular septal defect (AVSD)** involves a defect in both the atrial and ventricular septa and a common AV valve, usually causing **severe symptoms of heart failure** and **pulmonary hypertension in infancy**.
- It is also strongly associated with **Down syndrome**, which is not mentioned, and severe symptoms would have presented much earlier than age 7.
Atrial septation US Medical PG Question 9: A 28-year-old man comes to the physician because of a persistent tingling sensation in the right side of his face. The sensation began after he underwent an extraction of an impacted molar 2 weeks ago. Examination shows decreased sensation of the skin over the right side of the mandible, chin, and the anterior portion of the tongue. Taste sensation is preserved. The affected nerve exits the skull through which of the following openings?
- A. Foramen rotundum
- B. Hypoglossal canal
- C. Foramen magnum
- D. Foramen ovale (Correct Answer)
- E. Stylomastoid foramen
Atrial septation Explanation: ***Foramen ovale***
- This patient presents with **paresthesia** in the distribution of branches of the **mandibular nerve (V3)** following molar extraction. The affected areas (mandible, chin, and anterior tongue sensation) indicate injury to the **inferior alveolar nerve** (lower teeth, chin, lower lip) and/or **lingual nerve** (general sensation to anterior 2/3 of tongue).
- Both the **inferior alveolar nerve** and **lingual nerve** are branches of the **mandibular nerve (V3)**, which exits the skull through the **foramen ovale**. These nerves run in close proximity during molar extraction and are commonly injured together.
- Taste sensation is preserved because the **chorda tympani** (taste fibers from CN VII) travels with the lingual nerve but does not exit through foramen ovale.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, which innervates the midface, upper teeth, and palate.
- Injury to this nerve would cause sensory deficits in the upper lip and cheek, not the mandible or chin.
*Hypoglossal canal*
- The **hypoglossal canal** transmits the **hypoglossal nerve (CN XII)**, which is a motor nerve to the intrinsic and extrinsic muscles of the tongue.
- Damage to this nerve would result in **tongue weakness** or **atrophy**, not sensory changes to the face or tongue.
*Foramen magnum*
- The **foramen magnum** is the largest opening in the skull, transmitting the **spinal cord**, vertebral arteries, and accessory nerve (CN XI).
- Damage here would likely involve severe neurological deficits, not isolated sensory loss to the lower face.
*Stylomastoid foramen*
- The **stylomastoid foramen** transmits the **facial nerve (CN VII)**, which is primarily responsible for facial expression and taste sensation to the anterior two-thirds of the tongue via the chorda tympani.
- While CN VII provides taste to the tongue, it does not provide general sensory innervation to the skin of the mandible or chin, and taste is preserved in this patient.
Atrial septation US Medical PG Question 10: A 28-year-old woman with corrected transposition of the great arteries (L-TGA) who has been asymptomatic presents for preconception counseling. She has a systemic right ventricle supporting systemic circulation and asks about pregnancy risks. Her cardiologist notes mild tricuspid regurgitation. Evaluate the embryologic basis of her condition and synthesize recommendations regarding pregnancy.
- A. Simple transposition with late correction; pregnancy is safe with standard monitoring
- B. Both AV and ventriculoarterial discordance creating physiologically corrected circulation; pregnancy acceptable if systemic RV function normal, but requires high-risk obstetric and cardiology co-management (Correct Answer)
- C. Uncorrected transposition incompatible with pregnancy; recommend adoption
- D. Iatrogenic correction; pregnancy safe as anatomy is normalized
- E. Partial transposition; standard prenatal care is sufficient
Atrial septation Explanation: ***Both AV and ventriculoarterial discordance creating physiologically corrected circulation; pregnancy acceptable if systemic RV function normal, but requires high-risk obstetric and cardiology co-management***
- **L-TGA** involves **levo-looping** of the heart tube where the **morphologic right ventricle** (RV) supports the systemic circulation due to double discordance (atrioventricular and ventriculoarterial).
- Pregnancy is generally tolerated (maternal WHO class III) if **systemic RV function** is preserved, but requires multidisciplinary care to monitor for **heart failure**, **arrhythmias**, and worsening **tricuspid regurgitation**.
*Simple transposition with late correction; pregnancy is safe with standard monitoring*
- **D-TGA** (simple transposition) requires surgical correction (e.g., Arterial Switch) and has a distinct embryology involving failure of **conotruncal septation** spiral.
- Unlike L-TGA, corrected D-TGA carries different risks and would not be classified as having a "systemic right ventricle" if an **arterial switch** was performed.
*Uncorrected transposition incompatible with pregnancy; recommend adoption*
- **L-TGA** is "congenitally corrected," meaning blood flows in the correct physiological sequence; it is not inherently incompatible with pregnancy if the **systemic RV** is functional.
- Maternal mortality is not high enough to warrant absolute contraindication unless there is severe **RV dysfunction** or NYHA Class III/IV symptoms.
*Iatrogenic correction; pregnancy safe as anatomy is normalized*
- This condition is **congenitally corrected**, meaning the "correction" occurred during **embryogenesis** due to the double mismatch, not through surgery.
- The anatomy is never truly "normalized" because the **tricuspid valve** and **RV** are not designed for high-pressure systemic resistance, making pregnancy a high-risk event.
*Partial transposition; standard prenatal care is sufficient*
- There is no clinical entity termed "partial transposition" in this context; L-TGA is a complete, albeit **physiologically corrected**, malformation.
- Standard prenatal care is insufficient because the hemodynamic stress of pregnancy can trigger **systemic RV failure** or significant **heart block**.
More Atrial septation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.