Orbital structures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Orbital structures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Orbital structures US Medical PG Question 1: During an examination of the cranial nerves, a patient shows inability to move their eye laterally past the midline. Which of the following structures in the cavernous sinus is most likely affected?
- A. Oculomotor nerve
- B. Trochlear nerve
- C. Ophthalmic nerve
- D. Abducens nerve (Correct Answer)
Orbital structures Explanation: ***Abducens nerve***
- The **abducens nerve (CN VI)** innervates the **lateral rectus muscle**, responsible for **abduction** (lateral movement) of the eye [1].
- Inability to move the eye laterally past the midline indicates paralysis or weakness of the lateral rectus muscle, directly implicating the abducens nerve [1].
*Oculomotor nerve*
- The **oculomotor nerve (CN III)** controls most **extraocular muscles** (superior, inferior, medial rectus, inferior oblique) and the levator palpebrae superioris, as well as pupillary constriction [1], [2].
- Damage to this nerve would primarily affect **adduction**, elevation, depression, and eyelid opening, not isolated lateral gaze.
*Trochlear nerve*
- The **trochlear nerve (CN IV)** innervates the **superior oblique muscle**, which depresses and internally rotates the eye [1].
- A lesion here typically presents with **vertical diplopia**, particularly when reading or descending stairs, due to impaired eye depression and intorsion.
*Ophthalmic nerve*
- The **ophthalmic nerve (V1)** is one of the three divisions of the trigeminal nerve and is purely **sensory**.
- It provides sensation to the forehead, upper eyelid, cornea, and nose, and does not control any eye movements.
Orbital structures US Medical PG Question 2: A 45-year-old man is brought to the emergency department after being found down in the middle of the street. Bystanders reported to the police that they had seen the man as he exited a local bar, where he was subsequently assaulted. He sustained severe facial trauma, including multiple lacerations and facial bone fractures. The man is taken to the operating room by the ENT team, who attempted to reconstruct his facial bones with multiple plates and screws. Several days later, he complains of the inability to open his mouth wide or to completely chew his food, both of which he seemed able to do prior to the surgery. Where does the affected nerve exit the skull?
- A. Foramen rotundum
- B. Foramen ovale (Correct Answer)
- C. Jugular foramen
- D. Superior orbital fissure
- E. Inferior orbital fissure
Orbital structures Explanation: ***Foramen ovale***
- The symptoms of inability to open the mouth wide and difficulty chewing are indicative of damage to the **motor branches of the trigeminal nerve (mandibular nerve)**, which innervates the muscles of mastication.
- The **mandibular nerve (V3)** exits the skull through the **foramen ovale**.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, which is primarily sensory to the midface.
- Damage to this nerve would cause sensory deficits in the cheek, upper lip, and teeth, but not issues with mastication.
*Jugular foramen*
- The **jugular foramen** transmits the **glossopharyngeal (IX)**, **vagus (X)**, and **accessory (XI)** cranial nerves.
- Damage here would lead to problems with swallowing, speech, gag reflex, or shoulder movement, not specifically jaw movement or chewing.
*Superior orbital fissure*
- The **superior orbital fissure** transmits the **oculomotor (III)**, **trochlear (IV)**, **ophthalmic (V1)**, and **abducens (VI)** cranial nerves.
- Damage here would primarily affect eye movements or sensation around the eye and forehead.
*Inferior orbital fissure*
- The **inferior orbital fissure** transmits the **infraorbital nerve** (a branch of V2), **zygomatic nerve**, and other vessels.
- Damage here would result in sensory deficits in the infraorbital region and potentially affect lacrimal gland function, but not mastication.
Orbital structures US Medical PG Question 3: A 26-year-old man is brought to the emergency department by ambulance after being involved in a motor vehicle collision. He does not open his eyes on command or respond to verbal cues. A CT scan of the head shows a hyperdense fluid collection in the right medial temporal lobe with medial displacement of the uncus and parahippocampal gyrus of the temporal lobe. Which of the following cranial nerves is most likely to be injured as a result of this patient's lesion?
- A. Vagus
- B. Facial
- C. Oculomotor (Correct Answer)
- D. Abducens
- E. Trigeminal
Orbital structures Explanation: ***Oculomotor***
- The description of **medial displacement of the uncus and parahippocampal gyrus** (uncus herniation) compresses the **oculomotor nerve (CN III)** as it passes between the posterior cerebral and superior cerebellar arteries.
- Compression of the oculomotor nerve leads to a **dilated pupil** (due to parasympathetic fiber involvement) and **down-and-out deviation of the eye** (due to paralysis of extraocular muscles it innervates).
*Vagus*
- The vagus nerve (CN X) is deep within the skull and brainstem, far from the temporal lobe, and is not directly affected by uncal herniation.
- Injury to the vagus nerve typically presents with dysphagia, hoarseness, or cardiac arrhythmias, symptoms not indicated here.
*Facial*
- The facial nerve (CN VII) exits the brainstem at the pontomedullary junction and is located more superiorly and laterally than the structures involved in uncal herniation.
- Damage to the facial nerve causes facial muscle weakness or paralysis, which is not the primary concern with uncal herniation.
*Abducens*
- The abducens nerve (CN VI) is a long, slender nerve that can be affected by **generalized increases in intracranial pressure**, but is less commonly directly compressed by an uncal herniation itself.
- Injury to the abducens nerve causes **lateral rectus muscle paralysis**, leading to medial deviation of the eye, whereas uncal herniation typically affects the oculomotor nerve.
*Trigeminal*
- The trigeminal nerve (CN V) exits the pons and is located superior to the tentorial notch and medial temporal lobe, making it unlikely to be directly compressed by uncal herniation.
- Injury to the trigeminal nerve causes sensory loss in the face or weakness of the muscles of mastication, which are not consistent with the described lesion.
Orbital structures US Medical PG Question 4: A 24-year-old man is brought to the emergency department 30 minutes after being involved in a high-speed motor vehicle collision in which he was a restrained driver. On arrival, he is alert and oriented. His pulse is 112/min, respirations are 29/min, and blood pressure is 100/60 mm Hg. The pupils are equal and reactive to light. There is a 3-cm laceration over the forehead and multiple bruises over the trunk. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. The right knee is swollen and tender; range of motion is limited by pain. Infusion of 0.9% saline is begun and intravenous acetaminophen is administered. Two hours later, blood-tinged fluid spontaneously drains from both nostrils, and is made worse by leaning forward. On a piece of gauze, it shows up as a rapidly-expanding clear ring of fluid surrounding blood. Further evaluation of this patient is most likely to show which of the following?
- A. Numbness of upper cheek area
- B. Retroauricular ecchymosis
- C. Bilateral periorbital ecchymosis (Correct Answer)
- D. Cranial nerve XII palsy
- E. Carotid artery dissection
Orbital structures Explanation: **Bilateral periorbital ecchymosis**
- The clinical presentation, including head trauma from a **high-speed motor vehicle collision**, neurological symptoms like **blood-tinged fluid draining from both nostrils with a halo sign**, and hemodynamic instability (tachycardia and hypotension), points towards a **basilar skull fracture**.
- **Bilateral periorbital ecchymosis** (raccoon eyes) is a classic sign of a basilar skull fracture, particularly one involving the **anterior cranial fossa**, indicating extravasation of blood into the periorbital tissues.
*Numbness of upper cheek area*
- **Numbness of the upper cheek area** is associated with injury to the **infraorbital nerve**, which often occurs with **maxillary (Le Fort II or III) fractures** or **orbital floor fractures**.
- While midface fractures can occur in severe trauma, the **halo sign** from the nostrils is more indicative of a **CSF leak** associated with a **basilar skull fracture**, rather than isolated maxillary injury.
*Retroauricular ecchymosis*
- **Retroauricular ecchymosis** (Battle's sign) is also a sign of a **basilar skull fracture**, but it specifically indicates a fracture involving the **middle cranial fossa** and the **temporal bone**.
- While possible, the spontaneous draining of CSF from the nostrils (rhinorrhea) is more directly linked to an **anterior cranial fossa fracture** and involvement of the **cribriform plate**, making bilateral periorbital ecchymosis a more likely and specific finding in this context.
*Cranial nerve XII palsy*
- **Cranial nerve XII (hypoglossal) palsy** would result in **tongue deviation** and weakness, typically associated with injuries to the **posterior cranial fossa** or the **neck**.
- This is not a common finding with the presented symptoms of **rhinorrhea with a halo sign**, which points to an **anterior cranial fossa fracture**.
*Carotid artery dissection*
- **Carotid artery dissection** can occur after significant trauma and may present with headaches, neck pain, and focal neurological deficits such as **hemiparesis** or **cranial nerve deficits (e.g., Horner's syndrome)**.
- While trauma increases the risk, the specific symptom of **CSF rhinorrhea with a halo sign** is not characteristic of a carotid dissection but rather indicative of a **communication between the subarachnoid space and the nasal cavity** due to a skull base fracture.
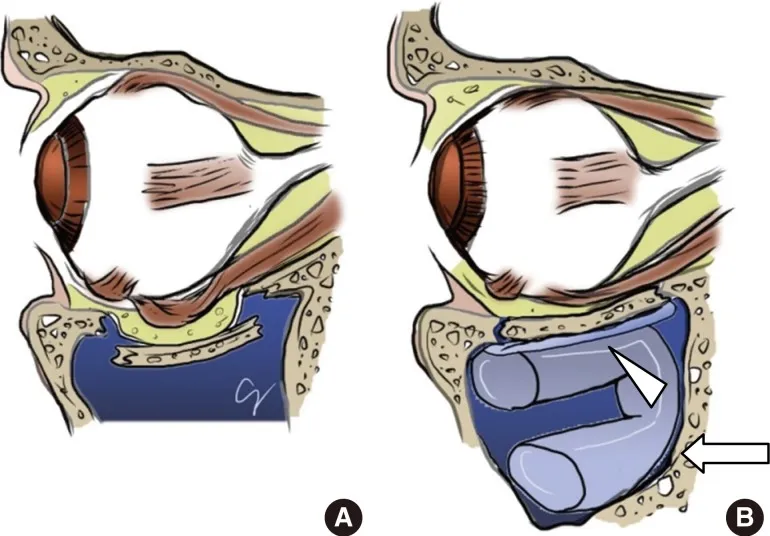
Orbital structures US Medical PG Question 5: A 36-year-old man was sent to the Emergency Department after a stray baseball hit him in the left eye during a game. Paramedics on sight could not perform the necessary testing and encouraged the patient to visit an ED for further testing and imaging. At the Emergency Department, the patient complains of slight pain in the orbital region and minimal diplopia that mildly increases with upward gaze. The patient’s blood pressure is 110/60 mm Hg, heart rate is 53/min, respiratory rate is 13/min, and temperature 36.6℃ (97.9℉). On physical examination, the patient is alert and responsive. There is an ecchymosis involving the lower lid and infraorbital area on the left side, with a slight downward deviation of the left globe, and conjunctival injection of the left eye. An upward gaze is limited on the left side. The visual acuity is 5/20 bilaterally. A head and neck CT shows a small (0.4 cm), nondisplaced, linear fracture of the left orbital floor. Which of the following statements about the condition the patient presents with is the most accurate?
- A. MRI is the best method to evaluate the patient’s condition.
- B. The patient can be initially managed conservatively with corticosteroids and observation. (Correct Answer)
- C. The patient’s condition warrants emergency surgery.
- D. There is a low chance of spontaneous improvement of the ocular motility.
- E. Surgical intervention within 3 days would help prevent enophthalmos in this patient.
Orbital structures Explanation: ***The patient can be initially managed conservatively with corticosteroids and observation.***
- The patient has a **small, nondisplaced orbital floor fracture** (0.4 cm) and minimal diplopia that only mildly increases with upward gaze, making **conservative management** appropriate.
- **Corticosteroids** can help reduce swelling and inflammation, and close **observation** is necessary to monitor for any worsening of symptoms, especially diplopia or enophthalmos.
*MRI is the best method to evaluate the patient’s condition.*
- While MRI can provide detailed soft tissue imaging, **CT scan** of the orbit is generally preferred for evaluating **orbital fractures** as it better visualizes bony structures and foreign bodies.
- The initial diagnosis was made with a CT scan, and for a small, nondisplaced fracture, a repeat or alternative imaging is not immediately necessary unless symptoms worsen.
*Surgical intervention within 3 days would allow to prevent enophthalmos in this patient.*
- **Early surgical intervention** (within days) is typically reserved for larger fractures (>50% of the orbital floor), significant enophthalmos, severe diplopia in primary gaze, or muscle entrapment.
- With a **small, nondisplaced fracture** and minimal symptoms, surgical intervention within 3 days is not indicated for this patient to prevent enophthalmos, as many such fractures heal spontaneously.
*The patient’s condition warrants emergency surgery.*
- **Emergency surgery** is reserved for severe cases, such as vision-threatening injuries (e.g., orbital compartment syndrome), globe rupture, or severe entrapment with oculocardiac reflex.
- This patient's vital signs are stable, visual acuity is relatively preserved, and the fracture is small and nondisplaced, indicating that emergency surgery is not required.
*There is a low chance of spontaneous improvement of the ocular motility.*
- For small, nondisplaced orbital floor fractures, **spontaneous improvement** of ocular motility and diplopia is common.
- The patient's minimal and gaze-dependent diplopia suggests that the issue might be related to local edema or soft tissue contusion, which often resolves with conservative management, rather than severe muscle entrapment.
Orbital structures US Medical PG Question 6: A 71-year-old woman presents to the emergency department with a headache for the past 30 minutes. She says that this is the worst headache of her life and that it came on suddenly after she hit her head. She says that she has also been experiencing visual problems with double vision when she looks to the left or the right. Visual examination reveals that her right eye cannot move right past the midline and her left eye cannot move left past the midline. Which of the following is most likely responsible for this patient's visual defects?
- A. Bilateral uncal herniation
- B. Unilateral uncal herniation
- C. Central herniation (Correct Answer)
- D. Subfalcine herniation
- E. Tonsillar herniation
Orbital structures Explanation: ***Central herniation***
- The sudden onset of severe headache after head trauma with **bilateral lateral rectus palsies** (right eye cannot move right, left eye cannot move left) indicates **bilateral abducens nerve (CN VI) dysfunction**.
- Central herniation involves **downward displacement of the diencephalon and midbrain** through the tentorial notch, which causes **increased intracranial pressure** and **stretching of CN VI bilaterally** as it has the longest intracranial course.
- CN VI is particularly vulnerable to **stretching over the petrous ridge** with increased ICP, and bilateral involvement is characteristic of **diffuse increased pressure** or **rostrocaudal deterioration** seen in central herniation.
- While central herniation can progress to pupillary changes and posturing, **early bilateral CN VI palsies** are a recognized finding with increased ICP.
*Bilateral uncal herniation*
- This is an extremely rare occurrence that would primarily affect **CN III (oculomotor nerve) bilaterally**, causing bilateral pupil dilation and "down and out" eye positioning.
- **Uncal herniation does NOT typically cause CN VI palsy**; it compresses CN III as the uncus herniates over the tentorial edge.
- The described findings (bilateral lateral rectus weakness) are not consistent with uncal herniation.
*Unilateral uncal herniation*
- Causes **ipsilateral CN III palsy** with a dilated pupil and "down and out" eye on one side.
- Would not explain the **bilateral abducens nerve deficits** described in this case.
- This is the classic herniation syndrome from temporal lobe mass effect.
*Subfalcine herniation*
- Involves the **cingulate gyrus** passing beneath the **falx cerebri**.
- Typically affects the **anterior cerebral artery**, leading to leg weakness, but **spares cranial nerves entirely**.
- Would not cause any extraocular movement abnormalities.
*Tonsillar herniation*
- Occurs when **cerebellar tonsils** descend through the **foramen magnum**.
- Presents with **respiratory depression, bradycardia, and cardiovascular instability** due to medullary compression.
- Does not typically affect CN VI or cause isolated extraocular movement deficits.
Orbital structures US Medical PG Question 7: A 33-year-old man comes to the otolaryngologist for the evaluation of a 6-month history of difficulty breathing through his nose and clear nasal discharge. He has a history of seasonal atopic rhinosinusitis. Anterior rhinoscopy shows a nasal polyp obstructing the superior nasal meatus. A CT scan of the head is most likely to show opacification of which of the following structures?
- A. Nasolacrimal duct and eustachian tube
- B. Sphenoidal sinus and posterior ethmoidal sinuses (Correct Answer)
- C. Frontal sinus and anterior ethmoidal sinus
- D. Maxillary sinus and anterior ethmoidal sinus
- E. Pterygopalatine fossa and middle ethmoidal sinus
Orbital structures Explanation: ***Sphenoidal sinus and posterior ethmoidal sinuses***
- The **posterior ethmoidal sinuses** drain directly into the **superior nasal meatus**, making them the primary structures affected by obstruction at this location.
- The **sphenoid sinus** drains into the **sphenoethmoidal recess**, which is located immediately posterior and superior to the superior nasal meatus. Due to their anatomical proximity and shared drainage region, obstruction in the superior meatus can affect drainage and lead to **opacification** of both structures due to **mucus retention** and inflammation.
- This is the most appropriate answer among the given options for superior meatus obstruction.
*Nasolacrimal duct and eustachian tube*
- The **nasolacrimal duct** drains into the **inferior nasal meatus**, not the superior meatus.
- The **eustachian tube** opens into the **nasopharynx**, which has no direct anatomical connection to the superior nasal meatus.
- These structures would not be affected by superior meatus obstruction.
*Frontal sinus and anterior ethmoidal sinus*
- The **frontal sinus** drains through the **frontonasal duct** into the **middle nasal meatus**.
- The **anterior ethmoid cells** also drain into the **middle nasal meatus** via the **infundibulum**.
- Obstruction in the **superior meatus** would not directly impact drainage of these sinuses.
*Maxillary sinus and anterior ethmoidal sinus*
- The **maxillary sinus** drains through its **ostium** into the **middle nasal meatus**.
- The **anterior ethmoid cells** drain into the **middle nasal meatus** through the **infundibulum**.
- These structures are not affected by superior meatus obstruction.
*Pterygopalatine fossa and middle ethmoidal sinus*
- The **pterygopalatine fossa** is a deep anatomical space containing neurovascular structures, not a sinus that drains into the nasal cavity.
- The **middle ethmoidal sinuses** drain into the **middle nasal meatus**, not the superior meatus.
- This option is anatomically incorrect for superior meatus obstruction.
Orbital structures US Medical PG Question 8: A 47-year-old woman presents to the emergency department with a fever and a headache. Her symptoms started yesterday and have rapidly progressed. Initially, she was experiencing just a fever and a headache which she was treating with acetaminophen. It rapidly progressed to blurry vision, chills, nausea, and vomiting. The patient has a past medical history of diabetes and hypertension and she is currently taking insulin, metformin, lisinopril, and oral contraceptive pills. Her temperature is 104°F (40.0°C), blood pressure is 157/93 mmHg, pulse is 120/min, respirations are 15/min, and oxygen saturation is 98% on room air. Upon further inspection, the patient also demonstrates exophthalmos in the affected eye. The patient's extraocular movements are notably decreased in the affected eye with reduced vertical and horizontal gaze. The patient also demonstrates decreased sensation near the affected eye in the distribution of V1 and V2. While the patient is in the department waiting for a CT scan, she becomes lethargic and acutely altered. Which of the following is the most likely diagnosis?
- A. Acute closed angle glaucoma
- B. Cavernous sinus thrombosis (Correct Answer)
- C. Brain abscess
- D. Periorbital cellulitis
- E. Intracranial hemorrhage
Orbital structures Explanation: ***Cavernous sinus thrombosis***
- The rapid progression of symptoms, **exophthalmos**, decreased extraocular movements (involving cranial nerves III, IV, and VI that pass through the cavernous sinus), and V1/V2 sensory deficits (trigeminal nerve branches) are classic signs of **cavernous sinus thrombosis**. The patient's acute alteration and lethargy point to CNS involvement.
- The patient's oral contraceptive use is a risk factor for **thrombosis**, and her diabetic and hypertensive status may contribute to her vulnerability to infections, which can lead to cavernous sinus thrombosis.
*Acute closed angle glaucoma*
- Acute closed-angle glaucoma typically presents with sudden, severe eye pain, blurred vision, and halos, often without systemic symptoms like fever or rapid progression to altered mental status.
- While it causes blurry vision, it does not typically cause **exophthalmos**, multiple extraocular muscle palsies, or deficits in V1/V2 sensation.
*Brain abscess*
- A brain abscess can cause fever, headache, and altered mental status, but it less commonly presents with the specific combination of **exophthalmos**, multiple cranial nerve palsies affecting eye movement, and V1/V2 sensory deficits.
- It would typically cause focal neurological deficits related to the specific brain region affected, rather than a constellation of orbital and systemic symptoms like this.
*Periorbital cellulitis*
- Periorbital cellulitis causes eyelid swelling, redness, and pain, and can be associated with fever, but it typically does not cause **exophthalmos**, decreased extraocular movements, or sensory deficits in the V1/V2 distribution as seen in this patient.
- Infection is limited to tissues anterior to the orbital septum and generally resolves with antibiotics without progression to severe neurological symptoms.
*Intracranial hemorrhage*
- Intracranial hemorrhage can cause sudden headache, altered mental status, and focal neurological deficits, but it rarely presents with **fever**, **exophthalmos**, or the specific cranial nerve palsies described without other clear signs of a stroke (e.g., sudden weakness or speech changes).
- The presence of fever and the constellation of orbital signs make hemorrhage less likely as the primary diagnosis.
Orbital structures US Medical PG Question 9: A 54-year-old woman comes to the physician because of a 1-day history of fever, chills, and double vision. She also has a 2-week history of headache and foul-smelling nasal discharge. Her temperature is 39.4°C (103°F). Examination shows mild swelling around the left eye. Her left eye does not move past midline on far left gaze but moves normally when looking to the right. Without treatment, which of the following findings is most likely to occur in this patient?
- A. Hemifacial anhidrosis
- B. Jaw deviation
- C. Absent corneal reflex (Correct Answer)
- D. Relative afferent pupillary defect
- E. Hypoesthesia of the earlobe
Orbital structures Explanation: ***Absent corneal reflex***
- This patient's symptoms (fever, chills, headache, foul-smelling nasal discharge, periorbital swelling, and ophthalmoplegia) suggest **cavernous sinus thrombosis** secondary to a sinus infection.
- The cavernous sinus contains cranial nerves III, IV, VI, V1, and V2. Untreated, the infection and thrombosis can easily spread to affect **cranial nerve V1 (ophthalmic branch of trigeminal nerve)**, leading to an absent corneal reflex.
*Hemifacial anhidrosis*
- This symptom, along with ptosis and miosis, is indicative of **Horner's syndrome**, which results from damage to the ipsilateral **sympathetic pathway**.
- While cavernous sinus thrombosis can rarely involve sympathetic fibers, it's not the most direct or common neurological sequela compared to trigeminal nerve involvement.
*Jaw deviation*
- **Jaw deviation** typically occurs due to weakness or paralysis of the **motor branch of the trigeminal nerve (V3)**, which innervates the muscles of mastication.
- Cavernous sinus thrombosis primarily affects V1 and V2, and V3 involvement, while possible, is less common and usually presents later than V1 or V2 deficits.
*Relative afferent pupillary defect*
- A relative afferent pupillary defect (RAPD, or Marcus Gunn pupil) indicates a lesion in the **afferent visual pathway** (e.g., optic nerve or retina).
- While vision can be affected in cavernous sinus thrombosis due to optic nerve compression or venous congestion, RAPD is not the most direct or specific neurological complication expected from the provided symptoms.
*Hypoesthesia of the earlobe*
- Sensation to the earlobe is primarily supplied by the **great auricular nerve (C2-C3 cervical spinal nerves)** with minor contribution from the **auricular branch of the vagus nerve (CN X)**.
- Cavernous sinus thrombosis does not involve these nerves, and hypoesthesia of the earlobe is not a characteristic finding.
Orbital structures US Medical PG Question 10: Impaired gag reflex is seen due to a lesion in which cranial nerves?
- A. CN V&VI
- B. CN X & XI
- C. CN IX & X (Correct Answer)
- D. CN VII & VIII
- E. CN XI & XII
Orbital structures Explanation: ***Correct: CN IX & X***
The **gag reflex (pharyngeal reflex)** is a protective reflex involving two cranial nerves:
- **Afferent limb**: **CN IX (Glossopharyngeal nerve)** provides sensory innervation to the posterior third of the tongue, oropharynx, and pharyngeal walls
- **Efferent limb**: **CN X (Vagus nerve)** provides motor innervation to the pharyngeal muscles (via the pharyngeal plexus) that contract during the reflex
**Clinical correlation**: Testing the gag reflex helps assess brainstem function and the integrity of CN IX and X. Impairment suggests lesions affecting these nerves or their nuclei in the medulla.
*Incorrect: CN V & VI*
- CN V (Trigeminal) provides facial sensation and motor to muscles of mastication, not involved in gag reflex
- CN VI (Abducens) controls lateral rectus muscle for eye abduction
*Incorrect: CN X & XI*
- While CN X is involved, CN XI (Accessory nerve) innervates sternocleidomastoid and trapezius muscles, not pharyngeal muscles
*Incorrect: CN VII & VIII*
- CN VII (Facial) controls facial expression and taste from anterior 2/3 of tongue
- CN VIII (Vestibulocochlear) is involved in hearing and balance, not the gag reflex
*Incorrect: CN XI & XII*
- CN XI (Accessory) innervates SCM and trapezius
- CN XII (Hypoglossal) provides motor to intrinsic and extrinsic tongue muscles, not pharyngeal muscles involved in gag reflex
More Orbital structures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.