Larynx and vocal apparatus US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Larynx and vocal apparatus. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Larynx and vocal apparatus US Medical PG Question 1: A 45-year-old man presents to an urgent care clinic because he coughed up blood this morning. Although he had a persistent cough for the past 3 weeks, he had never coughed up blood until now. His voice is hoarse and admits that it has been like that for the past few months. Both his past medical history and family history are insignificant. He has smoked a pack of cigarettes a day since the age of 20 and drinks wine every night before bed. His vitals are: heart rate of 78/min, respiratory rate of 14/min, temperature of 36.5°C (97.8°F), blood pressure of 140/88 mm Hg. An indirect laryngoscopy reveals a rough vegetating lesion on the free border of the right vocal cord. Which of the following is the most likely diagnosis?
- A. Acute laryngitis
- B. Polypoid corditis
- C. Leukoplakia
- D. Laryngeal carcinoma (Correct Answer)
- E. Vocal cord nodule
Larynx and vocal apparatus Explanation: ***Laryngeal carcinoma***
- The patient's long history of **smoking**, chronic **hoarseness** (lasting months), and especially the new onset of **hemoptysis** (coughing up blood) are highly suspicious for laryngeal carcinoma. The **rough vegetating lesion** on the vocal cord seen on laryngoscopy further supports this diagnosis.
- Alcohol consumption, in addition to smoking, significantly increases the risk of head and neck cancers, including **laryngeal carcinoma**. The duration of symptoms and the nature of the lesion point towards a malignant process rather than a benign or acute condition.
*Acute laryngitis*
- This is typically an **acute inflammatory condition** of the larynx, often viral in origin, lasting a few days to a couple of weeks, and usually resolves spontaneously.
- The patient's symptoms have been present for **months**, and the finding of a distinct **vegetating lesion** is not characteristic of acute laryngitis.
*Polypoid corditis*
- Also known as **Reinke's edema**, this condition is characterized by **edematous degeneration** of the vocal cords, primarily due to chronic irritation from smoking.
- While it causes hoarseness, it rarely presents with **hemoptysis** and the lesion described as "rough vegetating" is more suggestive of malignancy than the smooth, baggy appearance of Reinke's edema.
*Leukoplakia*
- **Leukoplakia** refers to white patches on mucous membranes that cannot be scraped off and are often **premalignant**. They can be caused by chronic irritation, such as smoking.
- Although leukoplakia can progress to carcinoma, the presence of **hemoptysis** and a "vegetating lesion" indicates a more advanced, likely malignant process rather than just a benign or premalignant white patch.
*Vocal cord nodule*
- **Vocal cord nodules** are benign growths, often bilateral, resulting from vocal abuse or misuse, and typically cause hoarseness and vocal fatigue.
- Nodules are usually **smooth** and rarely cause **hemoptysis** or appear as a "vegetating lesion." The patient's smoking history and hemoptysis point away from simple vocal cord nodules.
Larynx and vocal apparatus US Medical PG Question 2: A 55-year-old man is brought to the emergency department by ambulance from a long term nursing facility complaining of severe shortness of breath. He suffers from amyotrophic lateral sclerosis and lives at the nursing home full time. He has had the disease for 2 years and it has been getting harder to breath over the last month. He is placed on a rebreather mask and responds to questions while gasping for air. He denies cough or any other upper respiratory symptoms and denies a history of cardiovascular or respiratory disease. The blood pressure is 132/70 mm Hg, the heart rate is 98/min, the respiratory rate is 40/min, and the temperature is 37.6°C (99.7°F). During the physical exam, he begs to be placed in a sitting position. After he is repositioned his breathing improves a great deal. On physical examination, his respiratory movements are shallow and labored with paradoxical inward movement of his abdomen during inspiration. Auscultation of the chest reveals a lack of breath sounds in the lower lung bilaterally. At present, which of the following muscles is most important for inspiration in the patient?
- A. Muscles of anterior abdominal wall
- B. Sternocleidomastoid muscles (Correct Answer)
- C. Internal intercostal muscles
- D. Trapezius muscle
- E. External intercostal muscles
Larynx and vocal apparatus Explanation: ***Sternocleidomastoid muscles***
- In advanced **amyotrophic lateral sclerosis (ALS)**, progressive motor neuron degeneration affects both the diaphragm and intercostal muscles
- The **paradoxical inward movement of the abdomen** during inspiration indicates severe diaphragmatic weakness or paralysis
- The **shallow respiratory movements** and **severe respiratory distress** (respiratory rate 40/min) suggest that both primary inspiratory muscle groups (diaphragm and external intercostals) are significantly compromised
- At this stage, **accessory muscles of inspiration**, particularly the **sternocleidomastoid muscles**, become critically important for maintaining ventilation by elevating the sternum and upper ribs
- The dramatic improvement when sitting upright (orthopnea relief) supports accessory muscle recruitment, as this position optimizes sternocleidomastoid mechanical advantage
- **Clinical pearl:** In neuromuscular respiratory failure, neck muscle recruitment (visible SCM contraction) is a key sign of impending respiratory failure requiring ventilatory support
*External intercostal muscles*
- The **external intercostal muscles** are normally primary muscles of inspiration that elevate the ribs
- However, in advanced ALS with **2 years of progressive disease** and worsening dyspnea over the past month, these muscles would also be significantly weakened by the neurodegenerative process
- The **lack of breath sounds in the lower lungs bilaterally** suggests poor chest wall expansion, indicating compromised intercostal function
- While they continue to contribute, they are insufficient to maintain adequate ventilation alone at this stage of disease
*Internal intercostal muscles*
- The **internal intercostal muscles** function primarily in **forced expiration** by depressing the ribs
- They do not play a significant role in inspiration
*Muscles of anterior abdominal wall*
- The **anterior abdominal wall muscles** (rectus abdominis, external/internal obliques, transversus abdominis) are **expiratory muscles** used in forced expiration and coughing
- The **paradoxical inward movement** of the abdomen during inspiration is a passive phenomenon resulting from diaphragmatic weakness—the negative intrathoracic pressure pulls the weakened diaphragm upward, which in turn draws the abdominal wall inward
- These muscles are not contributing to inspiration in this patient
*Trapezius muscle*
- The **trapezius** primarily functions in scapular movement and neck stabilization
- While it provides some mechanical stability for the shoulder girdle during accessory muscle breathing, it is not directly involved in rib cage elevation
- It plays a minor supportive role compared to the sternocleidomastoid in respiratory distress
Larynx and vocal apparatus US Medical PG Question 3: A 3-year-old girl is brought to the physician by her parents because of a barking cough, a raspy voice, and noisy breathing for the last 3 days. Five days ago, she had a low-grade fever and runny nose. She attends daycare. Her immunizations are up-to-date. Her temperature is 37.8°C (100°F) and respirations are 33/min. Physical examination shows supraclavicular retractions. There is a high-pitched sound present on inspiration. Examination of the throat shows erythema without exudates. Which of the following is the most likely location of the anatomic narrowing causing this patient's symptoms?
- A. Bronchioles
- B. Pharynx
- C. Subglottic larynx (Correct Answer)
- D. Distal trachea
- E. Epiglottis
Larynx and vocal apparatus Explanation: ***Subglottic larynx***
- The patient's symptoms of **barking cough**, **raspy voice**, **stridor** (high-pitched inspiratory sound), and **supraclavicular retractions** are classic for **croup** (laryngotracheobronchitis), which is caused by inflammation and narrowing of the subglottic region of the larynx.
- The preceding low-grade fever and runny nose are typical of a viral upper respiratory infection, which commonly precedes croup.
*Bronchioles*
- Narrowing in the bronchioles typically causes **wheezing** (a high-pitched whistling sound on expiration) and **respiratory distress**, often seen in conditions like **bronchiolitis** or **asthma**.
- A barking cough and raspy voice are not characteristic symptoms of bronchiolar obstruction.
*Pharynx*
- Inflammation and narrowing of the pharynx primarily cause **sore throat**, **difficulty swallowing** (dysphagia), and sometimes **muffled voice**.
- It would not typically lead to a barking cough, stridor, or severe inspiratory distress.
*Distal trachea*
- While tracheal narrowing can cause stridor, the classic **barking cough** and **hoarseness** (raspy voice) are more specifically localized to the laryngeal area.
- Obstruction in the distal trachea would be less likely to affect voice quality as significantly as subglottic narrowing.
*Epiglottis*
- **Epiglottitis** presents as a rapidly progressive, life-threatening condition with **high fever**, **dysphagia**, **drooling**, and a **muffled "hot potato" voice**.
- The patient would typically appear toxic and prefer to sit in the **tripod position**, which is not described in this case, and her symptoms are less acute.
Larynx and vocal apparatus US Medical PG Question 4: A 2-year-old boy is brought to the physician by his parents for the evaluation of an unusual cough, a raspy voice, and noisy breathing for the last 2 days. During this time, the symptoms have always occurred in the late evening. The parents also report that prior to the onset of these symptoms, their son had a low-grade fever and a runny nose for 2 days. He attends daycare. His immunizations are up-to-date. His temperature is 37.8°C (100°F) and respirations are 33/min. Physical examination shows supraclavicular retractions. There is a high-pitched breath sound on inspiration. Which of the following is the most likely location of the abnormality?
- A. Epiglottis
- B. Subglottic larynx (Correct Answer)
- C. Supraglottic larynx
- D. Bronchioles
- E. Bronchi
Larynx and vocal apparatus Explanation: ***Subglottic larynx***
- The symptoms of **barking cough**, **raspy voice**, and **inspiratory stridor** (high-pitched breath sound on inspiration) are classic for **croup (laryngotracheobronchitis)**.
- Croup is characterized by **inflammation and edema of the subglottic larynx**, which is the narrowest part of the pediatric airway, leading to obstruction.
*Epiglottis*
- **Epiglottitis** typically presents with a sudden onset of **high fever**, **dysphagia**, drooling, and a muffled voice, often without a preceding viral prodrome.
- Patients with epiglottitis usually appear severely ill and may adopt a **tripod position** to maximize airway opening, which is not described here.
*Supraglottic larynx*
- While inflammation can occur here, severe **supraglottic edema** leading to the described symptoms (especially the barking cough) is uncommon in typical croup.
- Conditions affecting the supraglottic area, such as **supraglottitis**, often cause a muffled voice and severe dysphagia, rather than a raspy voice and classic croupy cough.
*Bronchioles*
- Inflammation of the bronchioles typically causes **bronchiolitis**, characterized by **wheezing**, tachypnea, and increased work of breathing due to small airway obstruction.
- This condition does not typically present with a **barking cough** or **stridor**, which are indicative of upper airway obstruction.
*Bronchi*
- Inflammation of the bronchi (**bronchitis**) primarily causes a **cough** (often productive) and sometimes wheezing or rhonchi.
- It does not typically result in **stridor** or a **raspy voice**, as these symptoms arise from laryngeal or tracheal involvement.
Larynx and vocal apparatus US Medical PG Question 5: A 27-year-old man comes to the physician because of a 1-day history of right-sided facial weakness and sound intolerance. Three days ago, he hit the right side of his head in a motor vehicle collision. He neither lost consciousness nor sought medical attention. Physical examination shows drooping of the mouth on the right side. Sensation over the face is not impaired. Impedance audiometry shows an absence of the acoustic reflex in the right ear. Which of the following muscles is most likely paralyzed in this patient?
- A. Anterior belly of the digastric
- B. Stylopharyngeus
- C. Cricothyroid
- D. Tensor tympani
- E. Stylohyoid (Correct Answer)
Larynx and vocal apparatus Explanation: ***Stylohyoid***
- The patient presents with **facial nerve (CN VII) injury** following head trauma, evidenced by **facial weakness** and **hyperacusis** (sound intolerance).
- The **absent acoustic reflex** indicates paralysis of the **stapedius muscle** (the primary muscle responsible for the acoustic reflex and sound dampening).
- Among the options provided, **stylohyoid** is the only muscle innervated by the **facial nerve (CN VII)**, making it the correct answer in this context.
- The stylohyoid is innervated by the **nerve to stylohyoid**, a branch of CN VII.
*Anterior belly of the digastric*
- The **anterior belly of the digastric** is innervated by the **mylohyoid nerve**, a branch of the **trigeminal nerve (CN V3)**.
- This would not be affected in facial nerve injury.
*Stylopharyngeus*
- The **stylopharyngeus muscle** is innervated by the **glossopharyngeal nerve (CN IX)**.
- Damage would cause **dysphagia** and **loss of taste** on the posterior third of the tongue, not facial weakness or hyperacusis.
*Cricothyroid*
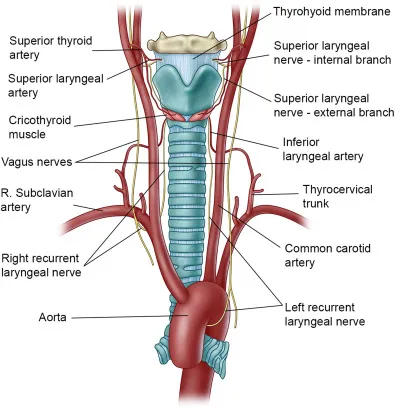
- The **cricothyroid muscle** is innervated by the **external branch of the superior laryngeal nerve** (from **vagus nerve, CN X**).
- Its paralysis causes **voice changes** and difficulty with high-pitched phonation, not facial nerve symptoms.
*Tensor tympani*
- The **tensor tympani muscle** is innervated by the **nerve to tensor tympani**, a branch of the **trigeminal nerve (V3)**.
- Although it dampens sound, it would not be affected in facial nerve injury; the **stapedius muscle** (CN VII) is responsible for the acoustic reflex and hyperacusis when paralyzed.
Larynx and vocal apparatus US Medical PG Question 6: An 85-year-old man who recently immigrated to the US from Spain presents to your office complaining of hoarseness and dysphagia for the past 2 months. He says his symptoms have been getting progressively worse, and he expresses concerns about the difficulty swallowing as he cannot eat well and has even lost 9 kg (20 lb) since his last visit 3 months ago. He denies any shortness of breath, coughing of blood, and chest pain. His bowel and bladder habit are normal. Past medical history is unremarkable. He has a 60-pack-year history of smoking tobacco and drinks alcohol occasionally. Which of the following is the most likely cause of his symptoms?
- A. Malignant proliferation of squamous cells (Correct Answer)
- B. Transformation leading to metaplasia in the lower esophagus
- C. Chronic autoimmune gastritis
- D. Malignant proliferation of glandular tissue in the esophagus
- E. Reduced lower esophageal pressure
Larynx and vocal apparatus Explanation: ***Malignant proliferation of squamous cells***
- The patient's presentation with **progressive hoarseness, dysphagia, and significant weight loss** in an 85-year-old male with a significant **60-pack-year smoking history** strongly suggests **squamous cell carcinoma of the esophagus or larynx/pharynx**.
- **Tobacco and alcohol use** are major risk factors for squamous cell carcinoma of the upper aerodigestive tract, and his symptoms align with advanced disease.
*Transformation leading to metaplasia in the lower esophagus*
- This describes **Barrett's esophagus**, a metaplastic change from squamous to columnar epithelium in the lower esophagus, usually due to **chronic gastroesophageal reflux disease (GERD)**.
- While Barrett's esophagus can progress to **adenocarcinoma** (with smoking as an additional risk factor), the primary presentation here with **hoarseness** strongly suggests squamous cell carcinoma of the upper aerodigestive tract rather than adenocarcinoma of the distal esophagus.
*Chronic autoimmune gastritis*
- This condition primarily affects the **stomach**, leading to **vitamin B12 deficiency** and megaloblastic anemia, and generally does not cause hoarseness or dysphagia as primary symptoms.
- The patient's symptoms are localized to the throat and esophagus, with systemic signs of disease progression (weight loss), rather than gastric issues.
*Malignant proliferation of glandular tissue in the esophagus*
- This refers to **esophageal adenocarcinoma**, which typically arises from **Barrett's esophagus** in the **distal esophagus**.
- While dysphagia and weight loss can occur, the prominent **hoarseness** points more towards a lesion affecting the pharynx or larynx, which are more commonly sites of **squamous cell carcinoma** due to smoking, rather than glandular tissue (adenocarcinoma).
*Reduced lower esophageal pressure*
- This is a characteristic feature of **achalasia**, a motility disorder where the lower esophageal sphincter fails to relax, leading to **dysphagia** and regurgitation.
- However, achalasia does not typically cause **hoarseness**, nor does it inherently explain the rapid and significant **weight loss** in the context of extensive smoking history, which strongly points to malignancy.
Larynx and vocal apparatus US Medical PG Question 7: A professional musician visits his physician after a morning concert. He complains of painless swelling in his right cheek when he plays his tuba. Physical examination of the patient reveals slight facial asymmetry due to minor swelling on the right side of the face. The skin over the swelling is smooth without any secondary changes. Palpation reveals a soft and non-tender swelling. The oral opening is normal without any trismus. Further examination reveals swelling of the right buccal mucosa extending from the first to the third molar. Bedside ultrasound shows small areas of high echogenicity consistent with pneumoparotid. Which nerve is associated with motor function to prevent air from entering the affected duct in this patient?
- A. CN VII – Zygomatic branch
- B. V3 – Mandibular nerve
- C. CN VII – Buccal branch (Correct Answer)
- D. CN VII – Marginal mandibular branch
- E. V2 – Maxillary nerve
Larynx and vocal apparatus Explanation: ***CN VII – Buccal branch***
- The **buccal branch** of the facial nerve (CN VII) innervates the **buccinator muscle**, which is crucial in preventing air from entering Stensen's duct during playing a wind instrument.
- **Pneumoparotid** results from air reflux into the parotid duct, typically prevented by the buccinator muscle's action in compressing the duct opening.
*CN VII – Zygomatic branch*
- The **zygomatic branch** of the facial nerve innervates muscles around the **eyes**, primarily controlling eyelid closure and facial expressions in that region.
- It does not directly affect the muscles responsible for preventing air entry into the parotid duct.
*V3 – Mandibular nerve*
- The **mandibular nerve (V3)** is a branch of the trigeminal nerve and provides **sensory innervation** to the lower face, as well as **motor innervation** to the muscles of mastication.
- Its primary role is in chewing and sensation, not in controlling the buccinator muscle or preventing parotid duct air entry.
*CN VII – Marginal mandibular branch*
- The **marginal mandibular branch** of the facial nerve innervates the muscles of the **lower lip and chin**, controlling expressions like frowning and pouting.
- It does not have a direct role in the function of the buccinator muscle or preventing air from entering the parotid duct.
*V2 – Maxillary nerve*
- The **maxillary nerve (V2)** is a branch of the trigeminal nerve that provides **sensory innervation** to the midface, upper teeth, and palate.
- It has no motor function related to the muscles of facial expression or the prevention of pneumoparotid.
Larynx and vocal apparatus US Medical PG Question 8: A 50-year-old man undergoes parathyroidectomy for treatment-resistant hyperparathyroidism. The procedure is complicated by brisk bleeding from the superior thyroid artery near the external branch of the superior laryngeal nerve. To stop the bleeding, the artery is ligated at its origin. Which of the following is most likely the origin of the artery that was injured in this patient?
- A. Thyrocervical trunk
- B. Ascending pharyngeal artery
- C. Internal carotid artery
- D. Subclavian artery
- E. External carotid artery (Correct Answer)
Larynx and vocal apparatus Explanation: ***External carotid artery***
- The **superior thyroid artery** is the first branch to arise from the **external carotid artery** in the neck.
- Ligation of this artery at its origin is a common surgical maneuver to control bleeding during thyroid or parathyroid surgery.
*Thyrocervical trunk*
- The **thyrocervical trunk** is a branch of the **subclavian artery** and gives rise to the inferior thyroid artery, not the superior thyroid artery.
- Injury to the superior thyroid artery would not necessitate ligation of a vessel originating from the thyrocervical trunk.
*Ascending pharyngeal artery*
- The **ascending pharyngeal artery** is a small artery that branches from the **external carotid artery** but supplies the pharynx, not the thyroid gland.
- It is not typically implicated in bleeding during parathyroidectomy or in relation to the superior laryngeal nerve.
*Internal carotid artery*
- The **internal carotid artery** primarily supplies the brain and does not have branches in the neck that supply the thyroid or parathyroid glands.
- It arises from the common carotid artery but does not give off the superior thyroid artery.
*Subclavian artery*
- The **subclavian artery** gives rise to the **thyrocervical trunk**, which then supplies the inferior thyroid artery, but not directly the superior thyroid artery.
- The superior thyroid artery originates higher up from the external carotid artery.
Larynx and vocal apparatus US Medical PG Question 9: A patient undergoes an MRI of the brain that reveals a tumor compressing the facial nerve at the internal acoustic meatus. Which of the following symptoms would most likely be present?
- A. Loss of taste in the posterior third of the tongue
- B. Loss of taste in the anterior two-thirds of the tongue
- C. Decreased salivation
- D. Facial muscle weakness and hyperacusis (Correct Answer)
- E. Decreased lacrimation
Larynx and vocal apparatus Explanation: ***Facial muscle weakness and hyperacusis***
- Compression of the **facial nerve (CN VII)** before it branches within the facial canal affects both its motor and special visceral afferent functions. [1]
- **Facial muscle weakness** results from damage to the motor fibers, while **hyperacusis** occurs due to paralysis of the stapedius muscle, innervated by the facial nerve's branch to the stapedius. [1]
*Loss of taste in the posterior third of the tongue*
- **Taste sensation** from the posterior third of the tongue is conveyed by the **glossopharyngeal nerve (CN IX)**, not the facial nerve.
- Therefore, compression of the facial nerve at the internal acoustic meatus would not impact taste in this region.
*Loss of taste in the anterior two-thirds of the tongue*
- While the **chorda tympani nerve** (a branch of the facial nerve) carries taste from the anterior two-thirds of the tongue, this branch typically separates from the facial nerve **distal to the internal acoustic meatus**.
- Compression at the internal acoustic meatus would affect the main trunk before this branching, but other symptoms are more prominent. [1]
*Decreased salivation*
- **Salivation** (specifically from the submandibular and sublingual glands) is mediated by the **chorda tympani nerve**, a branch of the facial nerve. [1]
- Similar to taste, this branch usually separates later, and while salivation can be affected, other symptoms like facial weakness and hyperacusis are more consistently prominent with proximal compression.
*Decreased lacrimation*
- **Lacrimation** is primarily controlled by the **greater petrosal nerve**, which branches off the facial nerve earlier in its course.
- While theoretically possible with very proximal compression affecting all components, compression at the internal acoustic meatus is more commonly associated with the motor and stapedius muscle function impairments first due to the spatial arrangement of fibers.
Larynx and vocal apparatus US Medical PG Question 10: An otherwise healthy 58-year-old man comes to the physician because of a 1-year history of episodic coughing whenever he cleans his left ear. There is no history of hearing loss, tinnitus, or vertigo. Stimulating his left ear canal with a cotton swab triggers a bout of coughing. The physician informs him that these symptoms are caused by hypersensitivity of a cranial nerve. A peripheral lesion of this nerve is most likely to manifest with which of the following findings on physical examination?
- A. Ipsilateral sensorineural hearing loss
- B. Ipsilateral deviation of the tongue
- C. Inability to raise ipsilateral eyebrow
- D. Decreased secretion from ipsilateral sublingual gland
- E. Ipsilateral vocal cord palsy (Correct Answer)
Larynx and vocal apparatus Explanation: ***Ipsilateral vocal cord palsy***
- The sensation in the external auditory canal that triggers a cough reflex is mediated by the **auricular branch of the vagus nerve (CN X)**, also known as Arnold's nerve.
- A peripheral lesion of the vagus nerve would most likely affect its motor functions, including the innervation of the **larynx**, leading to **ipsilateral vocal cord palsy** and hoarseness.
*Ipsilateral sensorineural hearing loss*
- Hearing loss is primarily associated with pathology of the **vestibulocochlear nerve (CN VIII)**, not the vagus nerve.
- The patient's presentation does not describe any auditory symptoms.
*Ipsilateral deviation of the tongue*
- Tongue deviation is a sign of compromise of the **hypoglossal nerve (CN XII)**, which controls the intrinsic and extrinsic muscles of the tongue.
- This is not a function of the vagus nerve.
*Inability to raise ipsilateral eyebrow*
- The ability to raise the eyebrow is controlled by the **facial nerve (CN VII)**, which innervates the muscles of facial expression.
- Vagus nerve lesions do not typically present with facial weakness.
*Decreased secretion from ipsilateral sublingual gland*
- Secretion from the sublingual gland is controlled by the **facial nerve (CN VII)** via the submandibular ganglion.
- While the vagus nerve has autonomic functions, it does not directly control sublingual gland secretion.
More Larynx and vocal apparatus US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.