Face and scalp US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Face and scalp. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Face and scalp US Medical PG Question 1: A 17-year-old girl presents to an urgent care clinic after waking up in the morning with a left-sided facial droop and an inability to fully close her left eye. Of note, she is currently on oral contraceptives and escitalopram and smokes half a pack of cigarettes per day. Her temperature is 98.2°F (36.8°C), blood pressure is 110/68 mmHg, pulse is 82/min, and respirations are 12/min. On exam, she has generalized, unilateral left-sided drooping of her upper and lower face, and an inability to move the left side of her mouth or close her left eye. Her extraocular movements and swallow are intact. She has no other neurologic deficits. Which of the following interventions would most likely address the most likely cause of this patient's symptoms?
- A. Head CT without contrast
- B. Implantation of gold weight for eyelid
- C. Prednisone alone (Correct Answer)
- D. Valacyclovir alone
- E. Intravenous immunoglobulin
Face and scalp Explanation: **Prednisone alone**
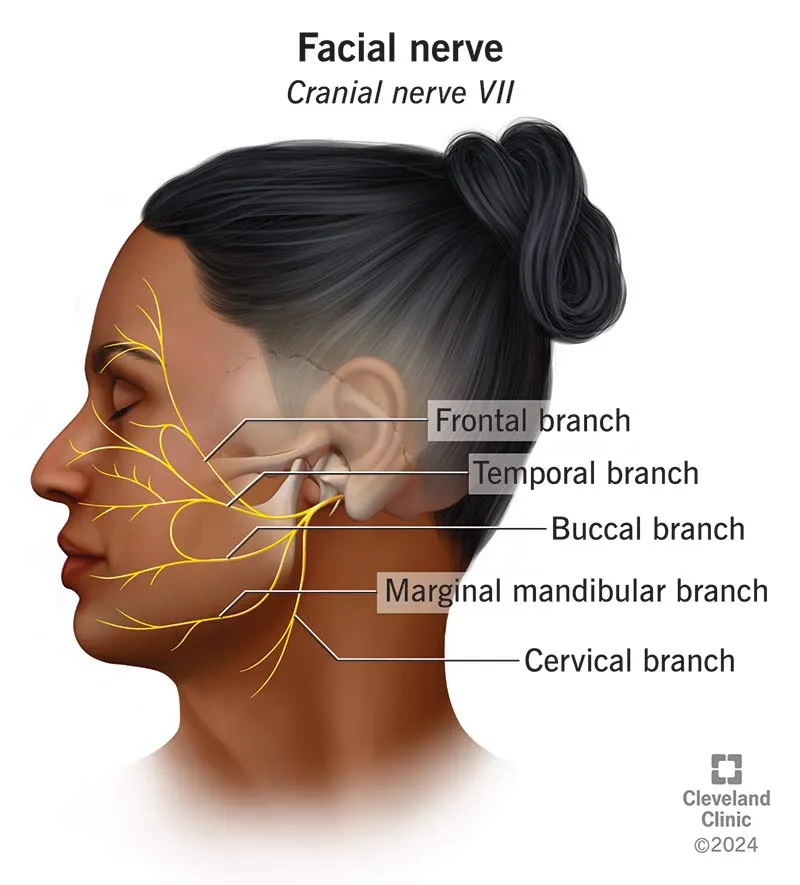
- The patient's presentation of **unilateral facial droop**, inability to close the eye, and intact extraocular movements points to **Bell's palsy**, an idiopathic peripheral facial nerve paralysis.
- **Corticosteroids like prednisone** are the mainstay of treatment for Bell's palsy, significantly improving the chances of full recovery, especially when started early.
*Head CT without contrast*
- A head CT is primarily for detecting **central causes of facial weakness** (e.g., stroke, tumor), which would spare the forehead and present with other neurological deficits.
- Since the patient has **generalized facial weakness** (affecting both upper and lower face) and no other neurological signs, a central lesion is less likely.
*Implantation of gold weight for eyelid*
- This is a **surgical intervention** to help with **lagophthalmos** (inability to close the eyelid) and prevent corneal damage.
- It is typically considered for **persistent Bell's palsy** or severe cases not responding to medical therapy, not as an initial treatment.
*Valacyclovir alone*
- **Antiviral agents like valacyclovir** are sometimes used in conjunction with corticosteroids if there's a suspected viral etiology (e.g., herpes simplex virus), but their benefit as monotherapy is not established.
- The **evidence for their benefit** even as adjunctive therapy is mixed and less robust than for corticosteroids.
*Intravenous immunoglobulin*
- **IVIG** is used for various immune-mediated neurological conditions, such as **Guillain-Barré syndrome**.
- There is **no evidence** to support the use of IVIG for Bell's palsy.
Face and scalp US Medical PG Question 2: A 63-year-old man is brought to the emergency department by his wife because she is concerned he is having another stroke. The patient says he woke up with right-sided facial weakness and drooping. Past medical history is significant for a recent case of shingles treated with acyclovir, and a stroke, diagnosed 10 years ago, from which he recovered with no residual functional deficits. On physical examination, there is weakness and drooping of the entire right side of the face. Sensation is intact. The remainder of the physical examination is unremarkable. Which of the following additional findings would also most likely be seen in this patient?
- A. Decreased salivation (Correct Answer)
- B. Wrinkled forehead
- C. Expressive aphasia
- D. Complete loss of taste to the tongue
- E. Partial hearing loss
Face and scalp Explanation: ***Decreased salivation***
- This is the **correct answer** for a patient with **Bell's palsy** (peripheral facial nerve palsy)
- The **facial nerve (CN VII)** carries **parasympathetic fibers** via the **chorda tympani** to innervate the **submandibular and sublingual salivary glands**
- A **lower motor neuron lesion** affecting CN VII results in **decreased salivation** on the affected side
- The clinical presentation of **complete facial weakness** (entire right side) with **recent shingles** strongly suggests **peripheral facial nerve palsy**, potentially **Ramsay Hunt syndrome** (VZV reactivation affecting CN VII)
*Wrinkled forehead*
- This finding would **NOT** be seen in this patient
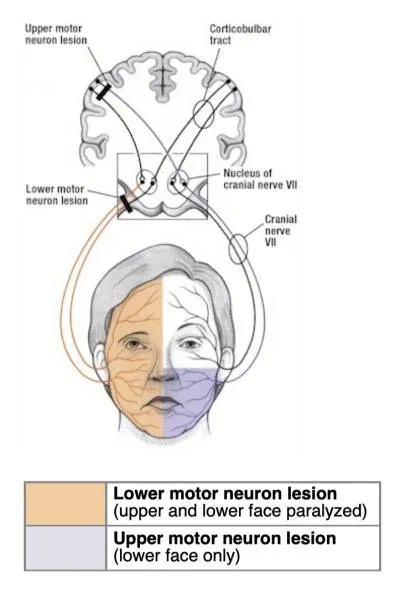
- A **lower motor neuron (LMN) lesion** of CN VII causes **complete ipsilateral facial paralysis**, including **inability to wrinkle the forehead** on the affected side
- **Forehead sparing** (preserved ability to wrinkle forehead) indicates an **upper motor neuron (UMN) lesion** due to bilateral cortical innervation of the frontalis muscle
- Since this patient has **complete facial weakness** including the forehead, he would be **unable to wrinkle his forehead**
*Expressive aphasia*
- **Expressive aphasia (Broca's aphasia)** results from damage to the **dominant frontal lobe** (Broca's area)
- This represents a **cortical lesion**, typically from stroke affecting the middle cerebral artery territory
- The patient's symptoms are isolated to **CN VII dysfunction** without evidence of cortical involvement
- No language, motor, or sensory deficits outside the facial nerve distribution are present
*Complete loss of taste to the tongue*
- While **partial taste loss** can occur in Bell's palsy, **complete loss of taste to the entire tongue** would not be expected
- The **facial nerve (CN VII)** carries taste from the **anterior two-thirds of the tongue** via the **chorda tympani**
- The **glossopharyngeal nerve (CN IX)** innervates taste from the **posterior one-third of the tongue**
- Complete taste loss would require involvement of both CN VII and CN IX, which is not typical for Bell's palsy
*Partial hearing loss*
- The facial nerve innervates the **stapedius muscle**, and CN VII palsy can cause **hyperacusis** (increased sensitivity to sound) due to loss of the acoustic reflex
- **Hearing loss** itself is mediated by the **vestibulocochlear nerve (CN VIII)**, not CN VII
- While **Ramsay Hunt syndrome** can sometimes involve CN VIII, the primary finding would be **hyperacusis**, not hearing loss
Face and scalp US Medical PG Question 3: A 31-year-old man comes to the emergency department because of drooping of the left side of his face since awakening that morning. He had difficulty chewing his food at breakfast. He was treated the previous day at the hospital after sustaining a head injury from falling off a ladder while working on his roof. A plain CT of the brain at that visit showed no abnormalities. He is in no apparent distress. His vital signs are within normal limits. The pupils are equal and reactive to light. There is drooping of the left corner of the mouth. The left nasolabial fold is flattened. When asked to close both eyes, the left eye remains partially open. There are no wrinkles on the left side of the forehead when the eyebrows are raised. Which of the following is the most appropriate next step in management?
- A. Steroid therapy (Correct Answer)
- B. Acyclovir therapy
- C. Reassurance
- D. Surgical decompression
- E. Surgical repair
Face and scalp Explanation: ***Steroid therapy***
- The patient presents with unilateral facial weakness affecting both the upper and lower face (inability to close the eye, flattened nasolabial fold, no forehead wrinkles), which is characteristic of **Bell's palsy**, an idiopathic **facial nerve paralysis**.
- **Corticosteroids** (e.g., prednisone) are the most appropriate initial treatment for Bell's palsy, especially when started within 72 hours of symptom onset, to reduce inflammation and improve recovery rates.
*Acyclovir therapy*
- While Bell's palsy is often associated with reactivation of **herpes simplex virus**, routine antiviral therapy (like acyclovir) in addition to corticosteroids for Bell's palsy does not provide significant additional benefit over corticosteroids alone.
- Antivirals are typically reserved for severe cases or those with evidence of **herpes zoster oticus (Ramsay Hunt syndrome)**, which is not indicated here.
*Reassurance*
- Although Bell's palsy often resolves spontaneously, simply reassuring the patient without offering treatment is not appropriate management given the availability of effective therapies.
- Delaying treatment with corticosteroids can lead to a lower chance of full recovery.
*Surgical decompression*
- **Surgical decompression** of the facial nerve is a controversial and rarely indicated treatment for Bell's palsy.
- It is typically reserved for very severe cases with complete facial paralysis and evidence of nerve compression, and its efficacy is not consistently proven.
*Surgical repair*
- **Surgical repair** is usually reserved for facial nerve paralysis caused by trauma with confirmed nerve transection, which is not suggested by the patient's presentation or prior CT scan.
- Bell's palsy is an inflammatory rather than structural injury to the nerve.
Face and scalp US Medical PG Question 4: A 43-year-old woman presents to the neurology clinic in significant pain. She reports a sharp, stabbing electric-like pain on the right side of her face. The pain started suddenly 2 weeks ago. The pain is so excruciating that she can no longer laugh, speak, or eat her meals as these activities cause episodes of pain. She had to miss work last week as a result. Her attacks last about 3 minutes and go away when she goes to sleep. She typically has 2–3 attacks per day now. The vital signs include: blood pressure 132/84 mm Hg, heart rate 79/min, and respiratory rate 14/min. A neurological examination shows no loss of crude touch, tactile touch, or pain sensations on the right side of the face. The pupillary light and accommodation reflexes are normal. There is no drooping of her mouth, ptosis, or anhidrosis noted. Which of the following is the most likely diagnosis?
- A. Atypical facial pain
- B. Cluster headache
- C. Trigeminal neuralgia (Correct Answer)
- D. Bell’s palsy
- E. Basilar migraine
Face and scalp Explanation: ***Trigeminal neuralgia***
- The patient's presentation of sudden, sharp, stabbing, electric-shock-like pain on one side of the face, triggered by activities like speaking, eating, and laughing, is highly characteristic of **trigeminal neuralgia**.
- The attacks are typically brief (lasting seconds to minutes), severe, and can cause significant functional impairment, consistent with the patient's report of missed work and inability to eat or speak.
*Atypical facial pain*
- This condition involves persistent, aching, or burning facial pain without clear neurological deficits, and it often does not have the paroxysmal, electric-shock quality seen in trigeminal neuralgia.
- Unlike **trigeminal neuralgia**, atypical facial pain is usually continuous rather than episodic and is not typically triggered by specific activities.
*Cluster headache*
- Characterized by severe, unilateral pain, often periorbital or temporal, accompanied by autonomic symptoms such as **lacrimation, conjunctival injection, nasal congestion, rhinorrhea, sweating, miosis, ptosis, and eyelid edema**.
- While very painful, the pain quality is usually deep and boring, not typically described as sharp, electric-shock like, and it is not triggered by facial movements like eating or speaking.
*Bell’s palsy*
- This condition involves **acute unilateral facial weakness or paralysis** due to inflammation of the facial nerve (CN VII), not pain as the primary symptom.
- While some patients may experience mild pain around the ear, the hallmark is facial muscle weakness leading to drooping of the mouth and inability to close the eye, which are absent in this patient.
*Basilar migraine*
- A rare type of migraine with aura symptoms originating from the brainstem, including **vertigo, dysarthria, tinnitus, bilateral visual symptoms, ataxia, and sometimes decreased level of consciousness**.
- While it can cause severe headache, it does not typically present with the described electric-shock-like facial pain triggered by movement, and the neurological examination did not reveal brainstem symptoms.
Face and scalp US Medical PG Question 5: A 29-year-old man presents to the emergency room with facial weakness. He first noticed that he was having trouble smiling normally while at dinner with friends the night before. He also noticed that his food had less taste than usual during the dinner. He woke up on the day of presentation with a complete inability to move the right side of his face. He recently returned from an extended camping trip in the Appalachian Mountains, but he did not find any tick bites following the camping trip. His past medical history is notable for Achilles tendonitis and carpal tunnel syndrome. He works as a computer programmer. He smokes marijuana occasionally but does not smoke cigarettes. His temperature is 98.6°F (37°C), blood pressure is 120/75 mmHg, pulse is 80/min, and respirations are 18/min. On exam, he is well-appearing in no acute distress. There is loss of facial wrinkles along the forehead, eyelids, and nasolabial folds. He is unable to completely close his right eye, raise his eyebrows, or smile with the right side of his mouth. Sensation is intact to light touch along the forehead, maxilla, and mandible bilaterally. Where is the most likely source of this patient’s lesion?
- A. Superior orbital fissure
- B. Petrotympanic fissure
- C. Inferior orbital fissure
- D. Dorsal frontal lobe
- E. Stylomastoid foramen (Correct Answer)
Face and scalp Explanation: ***Stylomastoid foramen***
- The patient presents with classic signs of **Bell's palsy**, characterized by unilateral **facial weakness affecting both the upper and lower face**, including loss of forehead wrinkles, inability to close the eye, and loss of nasolabial folds.
- The **stylomastoid foramen** is the exit point of the **facial nerve (CN VII)** from the skull, and inflammation or compression at this site is the most common cause of idiopathic facial nerve paralysis (Bell's palsy).
*Superior orbital fissure*
- Lesions in the **superior orbital fissure** would primarily affect cranial nerves **III, IV, V1, and VI**, leading to symptoms like ophthalmoplegia, ptosis, and sensory loss in the V1 distribution of the face, not a facial nerve palsy.
- While it is a bony canal, it is not the primary exit for the facial nerve.
*Petrotympanic fissure*
- The **petrotympanic fissure** transmits the **chorda tympani nerve**, which carries taste sensation from the anterior two-thirds of the tongue and parasympathetic fibers to the submandibular and sublingual glands.
- A lesion here would cause **loss of taste** and potentially dry mouth, but would not typically explain the extensive motor deficits of the entire ipsilateral face as seen in this patient, which indicates a more proximal or complete facial nerve involvement.
*Inferior orbital fissure*
- The **inferior orbital fissure** transmits the **maxillary nerve (V2)**, the zygomatic nerve, and branches of the inferior ophthalmic vein, affecting sensation to the mid-face.
- Damage here would result in **sensory deficits in the V2 distribution** and potentially orbital symptoms, not motor weakness of the facial muscles.
*Dorsal frontal lobe*
- A lesion in the **dorsal frontal lobe**, specifically involving the **motor cortex**, would cause contralateral facial weakness. However, it would typically spare the forehead and eyelid muscles due to bilateral cortical innervation of the upper facial muscles.
- The patient's presentation of **forehead and entire facial weakness** is characteristic of a **lower motor neuron lesion** of the facial nerve, not a central (upper motor neuron) lesion.
Face and scalp US Medical PG Question 6: A 50-year-old man undergoes parathyroidectomy for treatment-resistant hyperparathyroidism. The procedure is complicated by brisk bleeding from the superior thyroid artery near the external branch of the superior laryngeal nerve. To stop the bleeding, the artery is ligated at its origin. Which of the following is most likely the origin of the artery that was injured in this patient?
- A. Thyrocervical trunk
- B. Ascending pharyngeal artery
- C. Internal carotid artery
- D. Subclavian artery
- E. External carotid artery (Correct Answer)
Face and scalp Explanation: ***External carotid artery***
- The **superior thyroid artery** is the first branch to arise from the **external carotid artery** in the neck.
- Ligation of this artery at its origin is a common surgical maneuver to control bleeding during thyroid or parathyroid surgery.
*Thyrocervical trunk*
- The **thyrocervical trunk** is a branch of the **subclavian artery** and gives rise to the inferior thyroid artery, not the superior thyroid artery.
- Injury to the superior thyroid artery would not necessitate ligation of a vessel originating from the thyrocervical trunk.
*Ascending pharyngeal artery*
- The **ascending pharyngeal artery** is a small artery that branches from the **external carotid artery** but supplies the pharynx, not the thyroid gland.
- It is not typically implicated in bleeding during parathyroidectomy or in relation to the superior laryngeal nerve.
*Internal carotid artery*
- The **internal carotid artery** primarily supplies the brain and does not have branches in the neck that supply the thyroid or parathyroid glands.
- It arises from the common carotid artery but does not give off the superior thyroid artery.
*Subclavian artery*
- The **subclavian artery** gives rise to the **thyrocervical trunk**, which then supplies the inferior thyroid artery, but not directly the superior thyroid artery.
- The superior thyroid artery originates higher up from the external carotid artery.
Face and scalp US Medical PG Question 7: A 65-year-old man presents with facial weakness. He says he noticed that his face appeared twisted when he looked in the bathroom mirror this morning. He is otherwise well and does not have any other complaints. He denies any facial pain or paresthesia. No significant past medical history. The patient is afebrile and vital signs are within normal limits. Neurological examination reveals difficulty shutting the right eye tight and inability to bring up the right corner of his mouth when asked to smile. Remainder of the exam, including the left side of the face, is unremarkable. Which of the following is the most likely diagnosis in this patient?
- A. Idiopathic facial paralysis (Correct Answer)
- B. Right hemisphere stroke
- C. Left middle cerebral artery stroke
- D. Facial nerve schwannoma
- E. Acoustic neuroma
Face and scalp Explanation: ***Idiopathic facial paralysis***
- The sudden onset of **unilateral facial weakness** affecting both the upper and lower face (inability to shut eye and inability to smile on the same side) without other neurological symptoms is characteristic of **Bell's palsy**.
- It is a diagnosis of exclusion, and the absence of other symptoms and normal vital signs support this benign, self-limiting condition.
*Right hemisphere stroke*
- A stroke typically causes **upper motor neuron facial weakness**, primarily affecting the **lower half of the contralateral face**, sparing the forehead.
- Would likely present with other neurological deficits such as **hemiparesis** or sensory changes, which are absent here.
*Left middle cerebral artery stroke*
- Similar to a right hemisphere stroke, a left MCA stroke would typically cause **contralateral facial weakness**, predominantly in the **lower face**.
- Would also likely present with additional symptoms such as **aphasia** (if the dominant hemisphere is affected) or right-sided motor/sensory deficits, which are not described.
*Facial nerve schwannoma*
- This condition tends to cause a **slowly progressive facial weakness**, not the acute onset described.
- Often associated with other symptoms such as **persistent facial pain** or paresthesia, which this patient denies.
*Acoustic neuroma*
- Primarily causes **hearing loss** and **tinnitus**, and later, **vestibular symptoms** like dizziness or imbalance.
- While it can eventually compress the facial nerve causing weakness, the onset would be gradual and accompanied by **auditory symptoms**, which are absent here.
Face and scalp US Medical PG Question 8: A 65-year-old female with a past medical history of hypertension presents to her primary care doctor with a 3 month history of spasmodic facial pain. The pain is located in her right cheek and seems to be triggered when she smiles, chews, or brushes her teeth. The pain is sharp and excruciating, lasts for a few seconds, and occurs up to twenty times per day. She denies headaches, blurry vision, facial weakness, or changes in her memory. She feels rather debilitated and has modified much of her daily activities to avoid triggering the spasms. In the clinic, her physical exam is within normal limits. Her primary care doctor prescribes carbamazepine and asks her to follow up in a few weeks. Which cranial nerve is most likely involved in the patient's disease process?
- A. CN III
- B. CN V (Correct Answer)
- C. CN VI
- D. CN VII
- E. CN IV
Face and scalp Explanation: ***CN V***
- The patient's presentation of **recurrent, sharp, excruciating, unilateral facial pain** triggered by movements like chewing, smiling, or brushing teeth is classic for **trigeminal neuralgia**.
- **Trigeminal neuralgia** specifically affects the **trigeminal nerve (CN V)**, which has sensory branches covering the face, and is often treated with **carbamazepine**.
*CN III*
- The **oculomotor nerve (CN III)** is primarily involved in **eye movement** and **pupillary constriction**.
- Damage to CN III typically causes **diplopia, ptosis,** and **pupil dilation**, which are not present in this patient's symptoms.
*CN VI*
- The **abducens nerve (CN VI)** controls the **lateral rectus muscle**, responsible for **abducting the eye** (moving it outward).
- Dysfunction typically results in **diplopia** and an inability to move the eye laterally, not facial pain.
*CN VII*
- The **facial nerve (CN VII)** controls **facial expressions**, taste sensation from the anterior two-thirds of the tongue, and lacrimation/salivation.
- While it innervates facial muscles, its involvement typically presents as **facial weakness** or **paralysis** (e.g., Bell's palsy), not sharp, spasmodic pain.
*CN IV*
- The **trochlear nerve (CN IV)** innervates the **superior oblique muscle**, which is involved in rotating and depressing the eye.
- Lesions usually lead to **vertical diplopia**, particularly when looking down and inward, which is unrelated to the described facial pain.
Face and scalp US Medical PG Question 9: A 24-year-old man is brought to the emergency department 30 minutes after being involved in a high-speed motor vehicle collision in which he was a restrained driver. On arrival, he is alert and oriented. His pulse is 112/min, respirations are 29/min, and blood pressure is 100/60 mm Hg. The pupils are equal and reactive to light. There is a 3-cm laceration over the forehead and multiple bruises over the trunk. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. The right knee is swollen and tender; range of motion is limited by pain. Infusion of 0.9% saline is begun and intravenous acetaminophen is administered. Two hours later, blood-tinged fluid spontaneously drains from both nostrils, and is made worse by leaning forward. On a piece of gauze, it shows up as a rapidly-expanding clear ring of fluid surrounding blood. Further evaluation of this patient is most likely to show which of the following?
- A. Numbness of upper cheek area
- B. Retroauricular ecchymosis
- C. Bilateral periorbital ecchymosis (Correct Answer)
- D. Cranial nerve XII palsy
- E. Carotid artery dissection
Face and scalp Explanation: **Bilateral periorbital ecchymosis**
- The clinical presentation, including head trauma from a **high-speed motor vehicle collision**, neurological symptoms like **blood-tinged fluid draining from both nostrils with a halo sign**, and hemodynamic instability (tachycardia and hypotension), points towards a **basilar skull fracture**.
- **Bilateral periorbital ecchymosis** (raccoon eyes) is a classic sign of a basilar skull fracture, particularly one involving the **anterior cranial fossa**, indicating extravasation of blood into the periorbital tissues.
*Numbness of upper cheek area*
- **Numbness of the upper cheek area** is associated with injury to the **infraorbital nerve**, which often occurs with **maxillary (Le Fort II or III) fractures** or **orbital floor fractures**.
- While midface fractures can occur in severe trauma, the **halo sign** from the nostrils is more indicative of a **CSF leak** associated with a **basilar skull fracture**, rather than isolated maxillary injury.
*Retroauricular ecchymosis*
- **Retroauricular ecchymosis** (Battle's sign) is also a sign of a **basilar skull fracture**, but it specifically indicates a fracture involving the **middle cranial fossa** and the **temporal bone**.
- While possible, the spontaneous draining of CSF from the nostrils (rhinorrhea) is more directly linked to an **anterior cranial fossa fracture** and involvement of the **cribriform plate**, making bilateral periorbital ecchymosis a more likely and specific finding in this context.
*Cranial nerve XII palsy*
- **Cranial nerve XII (hypoglossal) palsy** would result in **tongue deviation** and weakness, typically associated with injuries to the **posterior cranial fossa** or the **neck**.
- This is not a common finding with the presented symptoms of **rhinorrhea with a halo sign**, which points to an **anterior cranial fossa fracture**.
*Carotid artery dissection*
- **Carotid artery dissection** can occur after significant trauma and may present with headaches, neck pain, and focal neurological deficits such as **hemiparesis** or **cranial nerve deficits (e.g., Horner's syndrome)**.
- While trauma increases the risk, the specific symptom of **CSF rhinorrhea with a halo sign** is not characteristic of a carotid dissection but rather indicative of a **communication between the subarachnoid space and the nasal cavity** due to a skull base fracture.
Face and scalp US Medical PG Question 10: A 71-year-old woman presents to the emergency department with a headache for the past 30 minutes. She says that this is the worst headache of her life and that it came on suddenly after she hit her head. She says that she has also been experiencing visual problems with double vision when she looks to the left or the right. Visual examination reveals that her right eye cannot move right past the midline and her left eye cannot move left past the midline. Which of the following is most likely responsible for this patient's visual defects?
- A. Bilateral uncal herniation
- B. Unilateral uncal herniation
- C. Central herniation (Correct Answer)
- D. Subfalcine herniation
- E. Tonsillar herniation
Face and scalp Explanation: ***Central herniation***
- The sudden onset of severe headache after head trauma with **bilateral lateral rectus palsies** (right eye cannot move right, left eye cannot move left) indicates **bilateral abducens nerve (CN VI) dysfunction**.
- Central herniation involves **downward displacement of the diencephalon and midbrain** through the tentorial notch, which causes **increased intracranial pressure** and **stretching of CN VI bilaterally** as it has the longest intracranial course.
- CN VI is particularly vulnerable to **stretching over the petrous ridge** with increased ICP, and bilateral involvement is characteristic of **diffuse increased pressure** or **rostrocaudal deterioration** seen in central herniation.
- While central herniation can progress to pupillary changes and posturing, **early bilateral CN VI palsies** are a recognized finding with increased ICP.
*Bilateral uncal herniation*
- This is an extremely rare occurrence that would primarily affect **CN III (oculomotor nerve) bilaterally**, causing bilateral pupil dilation and "down and out" eye positioning.
- **Uncal herniation does NOT typically cause CN VI palsy**; it compresses CN III as the uncus herniates over the tentorial edge.
- The described findings (bilateral lateral rectus weakness) are not consistent with uncal herniation.
*Unilateral uncal herniation*
- Causes **ipsilateral CN III palsy** with a dilated pupil and "down and out" eye on one side.
- Would not explain the **bilateral abducens nerve deficits** described in this case.
- This is the classic herniation syndrome from temporal lobe mass effect.
*Subfalcine herniation*
- Involves the **cingulate gyrus** passing beneath the **falx cerebri**.
- Typically affects the **anterior cerebral artery**, leading to leg weakness, but **spares cranial nerves entirely**.
- Would not cause any extraocular movement abnormalities.
*Tonsillar herniation*
- Occurs when **cerebellar tonsils** descend through the **foramen magnum**.
- Presents with **respiratory depression, bradycardia, and cardiovascular instability** due to medullary compression.
- Does not typically affect CN VI or cause isolated extraocular movement deficits.
More Face and scalp US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.