Ear anatomy and vestibular system US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ear anatomy and vestibular system. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ear anatomy and vestibular system US Medical PG Question 1: A 72-year-old man presents to his primary care physician with progressively worsening hearing loss. He states that his trouble with hearing began approximately 7-8 years ago. He is able to hear when someone is speaking to him; however, he has difficulty with understanding what is being said, especially when there is background noise. In addition to his current symptoms, he reports a steady ringing in both ears, and at times experiences dizziness. Medical history is significant for three prior episodes of acute otitis media. Family history is notable for his father being diagnosed with cholesteatoma. His temperature is 98.6°F (37°C), blood pressure is 138/88 mmHg, pulse is 74/min, and respirations are 13/min. On physical exam, when a tuning fork is placed in the middle of the patient's forehead, sound is appreciated equally on both ears. When a tuning fork is placed by the external auditory canal and subsequently on the mastoid process, air conduction is greater than bone conduction. Which of the following is most likely the cause of this patient's symptoms?
- A. Stapedial abnormal bone growth
- B. Endolymphatic hydrops
- C. Cochlear hair cell degeneration (Correct Answer)
- D. Accumulation of desquamated keratin debris
Ear anatomy and vestibular system Explanation: ***Cochlear hair cell degeneration***
- The patient's **progressive, bilateral hearing loss** over several years, difficulty understanding speech in noise, and **tinnitus** are classic symptoms of **presbycusis**, which results from age-related **degeneration of cochlear hair cells**.
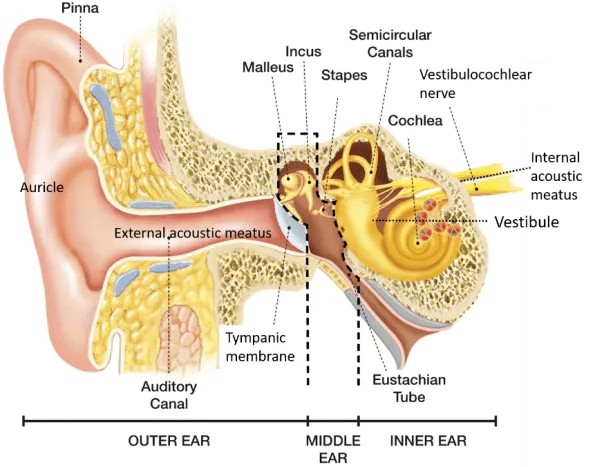
- The **normal Weber test** (no lateralization) and **Rinne test** (air conduction > bone conduction) indicate a **sensorineural hearing loss**, consistent with cochlear pathology rather than conductive issues.
*Stapedial abnormal bone growth*
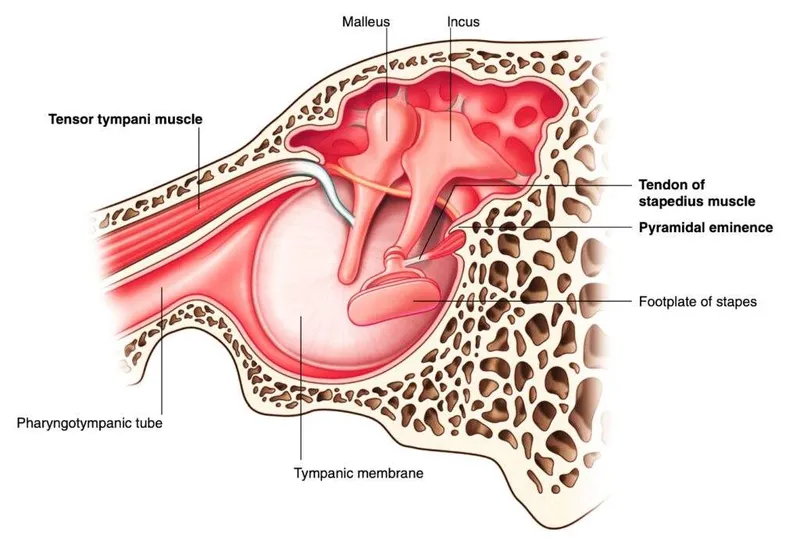
- This condition (**otosclerosis**) causes **conductive hearing loss** due to fixation of the stapes, which would present with an **abnormal Rinne test** (bone conduction > air conduction) in the affected ear.
- While it can cause progressive hearing loss and tinnitus, the normal Rinne test contradicts this diagnosis.
*Endolymphatic hydrops*
- This is the underlying pathology of **Ménière's disease**, which typically presents with episodic vertigo, fluctuating sensorineural hearing loss, tinnitus, and aural fullness.
- The patient's dizziness is non-episodic, and the absence of fluctuating hearing loss and aural fullness makes Ménière's less likely.
*Accumulation of desquamated keratin debris*
- This describes a **cholesteatoma**, which typically causes **conductive hearing loss** and often presents with otorrhea, earache, and possibly vestibular symptoms.
- The normal Rinne test (indicating sensorineural loss) and lack of otorrhea or earache make cholesteatoma unlikely, despite a family history.
Ear anatomy and vestibular system US Medical PG Question 2: A professional musician visits his physician after a morning concert. He complains of painless swelling in his right cheek when he plays his tuba. Physical examination of the patient reveals slight facial asymmetry due to minor swelling on the right side of the face. The skin over the swelling is smooth without any secondary changes. Palpation reveals a soft and non-tender swelling. The oral opening is normal without any trismus. Further examination reveals swelling of the right buccal mucosa extending from the first to the third molar. Bedside ultrasound shows small areas of high echogenicity consistent with pneumoparotid. Which nerve is associated with motor function to prevent air from entering the affected duct in this patient?
- A. CN VII – Zygomatic branch
- B. V3 – Mandibular nerve
- C. CN VII – Buccal branch (Correct Answer)
- D. CN VII – Marginal mandibular branch
- E. V2 – Maxillary nerve
Ear anatomy and vestibular system Explanation: ***CN VII – Buccal branch***
- The **buccal branch** of the facial nerve (CN VII) innervates the **buccinator muscle**, which is crucial in preventing air from entering Stensen's duct during playing a wind instrument.
- **Pneumoparotid** results from air reflux into the parotid duct, typically prevented by the buccinator muscle's action in compressing the duct opening.
*CN VII – Zygomatic branch*
- The **zygomatic branch** of the facial nerve innervates muscles around the **eyes**, primarily controlling eyelid closure and facial expressions in that region.
- It does not directly affect the muscles responsible for preventing air entry into the parotid duct.
*V3 – Mandibular nerve*
- The **mandibular nerve (V3)** is a branch of the trigeminal nerve and provides **sensory innervation** to the lower face, as well as **motor innervation** to the muscles of mastication.
- Its primary role is in chewing and sensation, not in controlling the buccinator muscle or preventing parotid duct air entry.
*CN VII – Marginal mandibular branch*
- The **marginal mandibular branch** of the facial nerve innervates the muscles of the **lower lip and chin**, controlling expressions like frowning and pouting.
- It does not have a direct role in the function of the buccinator muscle or preventing air from entering the parotid duct.
*V2 – Maxillary nerve*
- The **maxillary nerve (V2)** is a branch of the trigeminal nerve that provides **sensory innervation** to the midface, upper teeth, and palate.
- It has no motor function related to the muscles of facial expression or the prevention of pneumoparotid.
Ear anatomy and vestibular system US Medical PG Question 3: A 39-year-old man comes to the physician for evaluation of hearing loss. He reports difficulty hearing sounds like the beeping of the microwave or birds chirping, but can easily hear the pipe organ at church. He works as an aircraft marshaller. A Rinne test shows air conduction greater than bone conduction bilaterally. A Weber test does not lateralize. Which of the following is the most likely underlying cause of this patient's condition?
- A. Excess endolymphatic fluid pressure
- B. Immobility of the stapes
- C. Perforation of the tympanic membrane
- D. Destruction of the organ of Corti (Correct Answer)
- E. Compression of the vestibulocochlear nerve
Ear anatomy and vestibular system Explanation: ***Destruction of the organ of Corti***
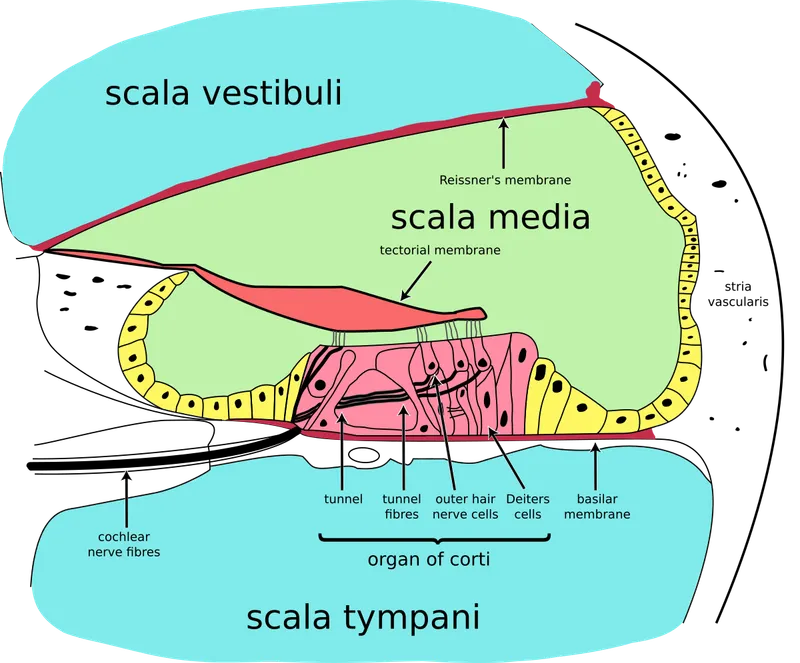
- This patient's **selective hearing loss** (difficulty with high-pitched sounds like chirping and beeping, but normal hearing for low-pitched sounds like an organ) combined with his occupation as an **aircraft marshaller** strongly suggests **noise-induced hearing loss**.
- **Noise-induced hearing loss** primarily damages the **hair cells** in the **organ of Corti**, particularly those sensitive to high frequencies, leading to a **sensorineural hearing loss**.
*Excess endolymphatic fluid pressure*
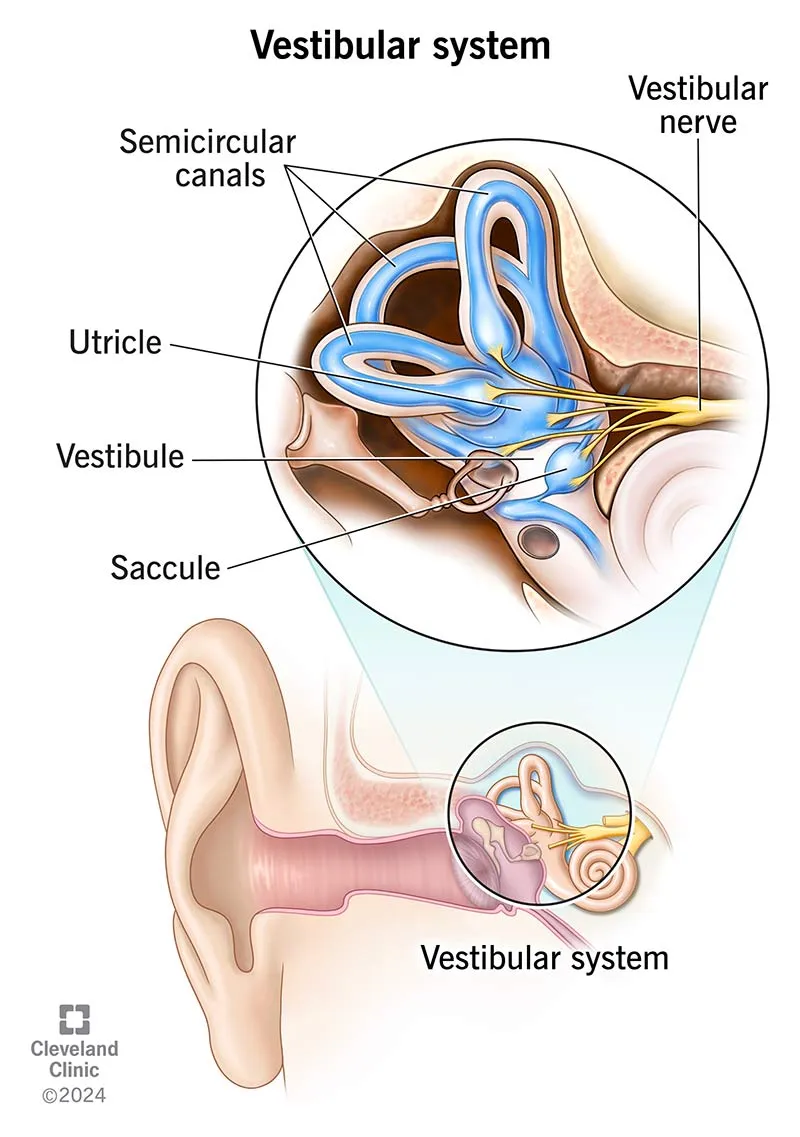
- This is characteristic of **Ménière's disease**, which typically presents with a triad of **fluctuating sensorineural hearing loss**, **tinnitus**, and **vertigo**.
- The patient's symptoms do not include vertigo or tinnitus, and his hearing loss pattern is more suggestive of noise exposure rather than endolymphatic hydrops.
*Immobility of the stapes*
- This suggests **otosclerosis**, a cause of **conductive hearing loss**.
- In conductive hearing loss, the **Rinne test** would typically show **bone conduction greater than air conduction (BC>AC)** in the affected ear, which contradicts the given finding of air conduction greater than bone conduction bilaterally.
*Perforation of the tympanic membrane*
- A **perforated tympanic membrane** causes **conductive hearing loss**.
- Similar to immobility of the stapes, this would result in **BC>AC** on the Rinne test, which is not what is observed in this patient.
*Compression of the vestibulocochlear nerve*
- This could be caused by an **acoustic neuroma** (vestibular schwannoma), which typically presents with **unilateral progressive sensorineural hearing loss**, **tinnitus**, and balance issues.
- The patient's symptoms describe a **bilateral hearing loss** pattern consistent with chronic noise exposure rather than a unilateral nerve compression.
Ear anatomy and vestibular system US Medical PG Question 4: A 45-year-old woman comes to the physician because of multiple episodes of dizziness over the past 3 months. Episodes last between 20 minutes and 1 hour. During the episodes she experiences the sudden onset of spinning sensations and imbalance, associated with a ringing in her left ear. She also reports progressive left-sided hearing loss and is unable to follow conversations in noisy surroundings. She has had an upper respiratory infection for the past 5 days, which is being treated with erythromycin. She has been otherwise healthy. Her vital signs are within normal limits. Examination shows no abnormalities. Pure tone audiometry shows a combined low- and high-frequency sensory loss of the left ear with normal hearing in the mid frequencies. Which of the following is the most appropriate initial step in management?
- A. Begin topiramate therapy
- B. Perform Epley maneuver
- C. Reduce caffeine intake (Correct Answer)
- D. Discontinue erythromycin
- E. Begin fluoxetine therapy
Ear anatomy and vestibular system Explanation: ***Reduce caffeine intake***
- The patient presents with classic **Ménière's disease**: episodic vertigo lasting 20 minutes to 1 hour, unilateral tinnitus, progressive unilateral sensorineural hearing loss, and characteristic audiometry showing low- and high-frequency loss with preserved mid-frequencies.
- **Lifestyle modifications** including **reducing caffeine, alcohol, and sodium intake** are the **most appropriate initial step** in management and represent evidence-based first-line conservative treatment.
- These dietary changes help reduce endolymphatic pressure and may decrease the frequency and severity of attacks.
- The symptoms have been present for **3 months**, predating the recent URI and erythromycin use by months, supporting a primary vestibular disorder rather than drug-induced pathology.
*Discontinue erythromycin*
- While macrolide antibiotics can rarely cause ototoxicity, this typically occurs with **high-dose intravenous erythromycin**, not standard oral doses for URI.
- The patient's symptoms began **3 months ago**, well before starting erythromycin **5 days ago**, making drug-induced ototoxicity unlikely.
- Aminoglycosides, loop diuretics, and platinum-based chemotherapy are the classic ototoxic agents, not typical oral erythromycin.
*Begin topiramate therapy*
- **Topiramate** is used for **migraine prophylaxis**, which may be considered for vestibular migraine, but there is no evidence of migraine features in this presentation.
- Not indicated as initial management for Ménière's disease.
*Perform Epley maneuver*
- The **Epley maneuver** is specific for **benign paroxysmal positional vertigo (BPPV)**, characterized by brief (seconds to minutes) episodes triggered by specific head positions.
- This patient's episodes last **20 minutes to 1 hour**, are associated with tinnitus and hearing loss, and are not positionally triggered, making BPPV unlikely.
*Begin fluoxetine therapy*
- **Fluoxetine** may be used for chronic vestibular disorders with comorbid anxiety or depression, or as part of vestibular migraine management.
- Not appropriate as initial management for Ménière's disease without evidence of psychiatric comorbidity.
Ear anatomy and vestibular system US Medical PG Question 5: A 75-year-old woman with hypertension presents to your office for a routine health exam. Her medications include hydrochlorothiazide and a multivitamin. She has been feeling well; however, she mentions that her family has been complaining about the volume of the television. She also reports difficulty hearing when others have called her name. On physical examination, her temperature is 99°F (37.2°C), blood pressure is 120/85 mmHg, pulse is 70/min, respirations are 17/min, and pulse oximetry is 99% on room air. The tympanic membrane is gray with no drainage or granulation tissue. Audiometry is consistent with high frequency sensorineural hearing loss. Which of the following is the most likely physiology behind this patient’s presentation?
- A. Bacterial infection of the middle ear
- B. Destruction of cochlear hair cells (Correct Answer)
- C. Increased endolymph production
- D. Abnormal skin growth in the middle ear
- E. Fixation of the stapes to the cochlea
Ear anatomy and vestibular system Explanation: ***Destruction of cochlear hair cells***
- The patient's age and history of **high-frequency sensorineural hearing loss** on audiometry are characteristic of **presbycusis**, which is primarily caused by **age-related degeneration of cochlear hair cells**.
- **Sensory hair cells** in the **basal turn of the cochlea**, which are responsible for detecting high-frequency sounds, are particularly vulnerable to age-related damage and are often the first to be affected.
*Bacterial infection of the middle ear*
- A bacterial infection of the middle ear, or **otitis media**, would typically present with **ear pain**, **fever**, and signs of inflammation on **tympanic membrane examination**, none of which are noted here.
- Furthermore, otitis media primarily causes a **conductive hearing loss**, whereas the patient has **sensorineural hearing loss**.
*Increased endolymph production*
- **Increased endolymph production** or **Meniere's disease** is characterized by episodic **vertigo**, **tinnitus**, and ** fluctuating sensorineural hearing loss**, often affecting low frequencies initially.
- The patient's chronic, progressive high-frequency hearing loss without vertigo does not align with Meniere's disease.
*Abnormal skin growth in the middle ear*
- An **abnormal skin growth** in the middle ear, or **cholesteatoma**, typically presents with **conductive hearing loss**, **otorrhea (ear discharge)**, and possibly **tinnitus** or **vertigo**.
- The patient has **sensorineural hearing loss**, and there is no mention of discharge or other symptoms indicative of a cholesteatoma.
*Fixation of the stapes to the cochlea*
- **Otosclerosis**, which involves the **fixation of the stapes** to the oval window (not the cochlea), leads to **conductive hearing loss** due to impaired sound transmission to the inner ear.
- The patient's audiometry specifically indicates **sensorineural hearing loss**, ruling out otosclerosis as the primary cause.
Ear anatomy and vestibular system US Medical PG Question 6: A 45-year-old male presents to his primary care physician for complaints of dizziness. The patient reports he experiences room-spinning dizziness lasting several hours at a time, approximately 2-3 times a month, starting 3 months ago. Upon questioning, the patient also reports right sided diminished hearing, tinnitus, and a sensation of ear fullness. His temperature is 99 deg F (37.2 deg C), pulse 70/min, respirations 12, blood pressure 130 mmHg/85 mmHg, SpO2 99%. You decide to order an audiometric evaluation. What is the most likely finding of the audiogram?
- A. Low frequency sensorineural hearing loss (Correct Answer)
- B. Normal audiogram
- C. High frequency conductive hearing loss
- D. High frequency sensorineural hearing loss
- E. Low frequency conductive hearing loss
Ear anatomy and vestibular system Explanation: ***Low frequency sensorineural hearing loss***
- The constellation of **episodic vertigo**, **tinnitus**, **aural fullness**, and **fluctuating hearing loss** is classic for **Ménière's disease**.
- In Ménière's disease, the characteristic audiogram finding is a **sensorineural hearing loss** that predominantly affects the **low frequencies**.
*Normal audiogram*
- A normal audiogram would not explain the patient's reported symptoms of **diminished hearing** and **tinnitus**.
- These symptoms indicate an underlying auditory dysfunction, which a normal audiogram would rule out.
*High frequency conductive hearing loss*
- **Conductive hearing loss** indicates an issue with sound transmission through the outer or middle ear (e.g., **otosclerosis**, **cerumen impaction**).
- The reported symptoms and the characteristic low-frequency involvement in Ménière's disease do not align with high-frequency conductive hearing loss.
*High frequency sensorineural hearing loss*
- While sensorineural hearing loss is correct, **high-frequency loss** is more typical of **presbycusis** (age-related hearing loss) or **noise-induced hearing loss**.
- Ménière's disease characteristically affects the **low frequencies** initially.
*Low frequency conductive hearing loss*
- **Conductive hearing loss** implies a problem in the outer or middle ear, which is not consistent with the pathology of **Ménière's disease** (endolymphatic hydrops affecting the inner ear).
- While the frequency range is correct, the type of hearing loss (conductive vs. sensorineural) is incorrect for Ménière's disease.
Ear anatomy and vestibular system US Medical PG Question 7: A 27-year-old man presents to a physician for evaluation of 3 months of increased vertigo. He says that occasionally he will experience several seconds of intense vertigo that makes him lose his balance. He came in for evaluation because this symptom is affecting his ability to drive to work. He has also been occasionally experiencing tinnitus. Physical exam reveals rotatory nystagmus that is delayed in onset and stops with visual fixation. The nerve that is most likely causing these symptoms exits the skull at which of the following locations?
- A. Internal auditory meatus (Correct Answer)
- B. Cribriform plate
- C. Foramen ovale
- D. Jugular foramen
- E. Foramen rotundum
Ear anatomy and vestibular system Explanation: ***Internal auditory meatus***
- The symptoms described, particularly **vertigo** and **tinnitus**, are indicative of an issue with the **vestibulocochlear nerve (CN VIII)**.
- The **vestibulocochlear nerve** exits the skull through the **internal auditory meatus**, which is also the pathway for the **facial nerve (CN VII)**.
*Cribriform plate*
- The **cribriform plate** is associated with the passage of the **olfactory nerves (CN I)**, which are responsible for the sense of smell.
- Damage to this area would typically cause **anosmia**, not vertigo or tinnitus.
*Foramen ovale*
- The **foramen ovale** is the exit point for the **mandibular nerve (V3)**, a branch of the trigeminal nerve.
- Dysfunction here would lead to problems with **mastication** or altered sensation in the lower face, not vertigo.
*Jugular foramen*
- The **jugular foramen** transmits several cranial nerves: the **glossopharyngeal (CN IX)**, **vagus (CN X)**, and **accessory (CN XI)** nerves.
- Issues in this region would manifest as difficulties with **swallowing**, **speech**, or **shoulder/neck movement**, not balance or hearing.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, another branch of the trigeminal nerve.
- Damage to this nerve would primarily affect **sensation in the middle third of the face**, not balance or hearing.
Ear anatomy and vestibular system US Medical PG Question 8: A 27-year-old man presents to the emergency department with dizziness. He states he has experienced a sustained sensation of the room spinning that is low grade and constant since this morning. The patient occasionally feels nauseous and has been taking diphenydramine to sleep which helps with his symptoms. The patient is generally healthy, has no other medical conditions, and only endorses eating more garlic recently to get over a cold he had a few days ago. His temperature is 98.7°F (37.1°C), blood pressure is 122/81 mmHg, pulse is 82/min, respirations are 15/min, and oxygen saturation is 99% on room air. Physical exam is notable for a healthy man. The patient is sat upright, his head is turned slightly to the right, and he is laid back flat rapidly. This does not provoke any symptoms even when repeated on the left side. A nystagmus is notable on cranial nerve exam as well as bilateral decreased hearing. The patient’s tandem gait is unstable; however, his baseline gait appears unremarkable despite the patient stating he has a sustained sensation of imbalance. Which of the following is the most likely diagnosis?
- A. Labyrinthitis (Correct Answer)
- B. Vertebrobasilar stroke
- C. Vestibular neuritis
- D. Meniere disease
- E. Benign paroxysmal positional vertigo
Ear anatomy and vestibular system Explanation: ***Labyrinthitis***
- The patient presents with **vertigo, nystagmus, and bilateral decreased hearing** following a recent cold, which is highly suggestive of **labyrinthitis**.
- **Labyrinthitis** is typically caused by a viral infection of the inner ear, affecting both the **vestibular and cochlear functions**.
*Vertebrobasilar stroke*
- While a **vertebrobasilar stroke** can cause dizziness and nystagmus, it would typically present with **focal neurological deficits** such as ataxia, dysarthria, or diplopia, which are absent here.
- The patient's otherwise healthy status and the history of a recent infection make a stroke less likely in this young individual.
*Vestibular neuritis*
- **Vestibular neuritis** presents with sudden, severe vertigo and nystagmus, but it **does not involve hearing loss**, unlike labyrinthitis.
- The patient's complaint of **bilateral decreased hearing** rules out isolated vestibular neuritis.
*Meniere disease*
- **Meniere disease** is characterized by recurrent episodes of vertigo, fluctuating sensorineural hearing loss, tinnitus, and aural fullness.
- The patient's symptoms are described as a **sustained, constant sensation of spinning** and not episodic, making Meniere disease less likely.
*Benign paroxysmal positional vertigo*
- **BPPV** causes brief episodes of vertigo triggered by specific head movements, and it is usually diagnosed with a **positive Dix-Hallpike test**.
- The patient's symptoms are **constant and sustained**, and the **Dix-Hallpike maneuver did not provoke symptoms**, ruling out BPPV.
Ear anatomy and vestibular system US Medical PG Question 9: A 28-year-old man comes to the physician because of a persistent tingling sensation in the right side of his face. The sensation began after he underwent an extraction of an impacted molar 2 weeks ago. Examination shows decreased sensation of the skin over the right side of the mandible, chin, and the anterior portion of the tongue. Taste sensation is preserved. The affected nerve exits the skull through which of the following openings?
- A. Foramen rotundum
- B. Hypoglossal canal
- C. Foramen magnum
- D. Foramen ovale (Correct Answer)
- E. Stylomastoid foramen
Ear anatomy and vestibular system Explanation: ***Foramen ovale***
- This patient presents with **paresthesia** in the distribution of branches of the **mandibular nerve (V3)** following molar extraction. The affected areas (mandible, chin, and anterior tongue sensation) indicate injury to the **inferior alveolar nerve** (lower teeth, chin, lower lip) and/or **lingual nerve** (general sensation to anterior 2/3 of tongue).
- Both the **inferior alveolar nerve** and **lingual nerve** are branches of the **mandibular nerve (V3)**, which exits the skull through the **foramen ovale**. These nerves run in close proximity during molar extraction and are commonly injured together.
- Taste sensation is preserved because the **chorda tympani** (taste fibers from CN VII) travels with the lingual nerve but does not exit through foramen ovale.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, which innervates the midface, upper teeth, and palate.
- Injury to this nerve would cause sensory deficits in the upper lip and cheek, not the mandible or chin.
*Hypoglossal canal*
- The **hypoglossal canal** transmits the **hypoglossal nerve (CN XII)**, which is a motor nerve to the intrinsic and extrinsic muscles of the tongue.
- Damage to this nerve would result in **tongue weakness** or **atrophy**, not sensory changes to the face or tongue.
*Foramen magnum*
- The **foramen magnum** is the largest opening in the skull, transmitting the **spinal cord**, vertebral arteries, and accessory nerve (CN XI).
- Damage here would likely involve severe neurological deficits, not isolated sensory loss to the lower face.
*Stylomastoid foramen*
- The **stylomastoid foramen** transmits the **facial nerve (CN VII)**, which is primarily responsible for facial expression and taste sensation to the anterior two-thirds of the tongue via the chorda tympani.
- While CN VII provides taste to the tongue, it does not provide general sensory innervation to the skin of the mandible or chin, and taste is preserved in this patient.
Ear anatomy and vestibular system US Medical PG Question 10: A 29-year-old man presents to the emergency room with facial weakness. He first noticed that he was having trouble smiling normally while at dinner with friends the night before. He also noticed that his food had less taste than usual during the dinner. He woke up on the day of presentation with a complete inability to move the right side of his face. He recently returned from an extended camping trip in the Appalachian Mountains, but he did not find any tick bites following the camping trip. His past medical history is notable for Achilles tendonitis and carpal tunnel syndrome. He works as a computer programmer. He smokes marijuana occasionally but does not smoke cigarettes. His temperature is 98.6°F (37°C), blood pressure is 120/75 mmHg, pulse is 80/min, and respirations are 18/min. On exam, he is well-appearing in no acute distress. There is loss of facial wrinkles along the forehead, eyelids, and nasolabial folds. He is unable to completely close his right eye, raise his eyebrows, or smile with the right side of his mouth. Sensation is intact to light touch along the forehead, maxilla, and mandible bilaterally. Where is the most likely source of this patient’s lesion?
- A. Superior orbital fissure
- B. Petrotympanic fissure
- C. Inferior orbital fissure
- D. Dorsal frontal lobe
- E. Stylomastoid foramen (Correct Answer)
Ear anatomy and vestibular system Explanation: ***Stylomastoid foramen***
- The patient presents with classic signs of **Bell's palsy**, characterized by unilateral **facial weakness affecting both the upper and lower face**, including loss of forehead wrinkles, inability to close the eye, and loss of nasolabial folds.
- The **stylomastoid foramen** is the exit point of the **facial nerve (CN VII)** from the skull, and inflammation or compression at this site is the most common cause of idiopathic facial nerve paralysis (Bell's palsy).
*Superior orbital fissure*
- Lesions in the **superior orbital fissure** would primarily affect cranial nerves **III, IV, V1, and VI**, leading to symptoms like ophthalmoplegia, ptosis, and sensory loss in the V1 distribution of the face, not a facial nerve palsy.
- While it is a bony canal, it is not the primary exit for the facial nerve.
*Petrotympanic fissure*
- The **petrotympanic fissure** transmits the **chorda tympani nerve**, which carries taste sensation from the anterior two-thirds of the tongue and parasympathetic fibers to the submandibular and sublingual glands.
- A lesion here would cause **loss of taste** and potentially dry mouth, but would not typically explain the extensive motor deficits of the entire ipsilateral face as seen in this patient, which indicates a more proximal or complete facial nerve involvement.
*Inferior orbital fissure*
- The **inferior orbital fissure** transmits the **maxillary nerve (V2)**, the zygomatic nerve, and branches of the inferior ophthalmic vein, affecting sensation to the mid-face.
- Damage here would result in **sensory deficits in the V2 distribution** and potentially orbital symptoms, not motor weakness of the facial muscles.
*Dorsal frontal lobe*
- A lesion in the **dorsal frontal lobe**, specifically involving the **motor cortex**, would cause contralateral facial weakness. However, it would typically spare the forehead and eyelid muscles due to bilateral cortical innervation of the upper facial muscles.
- The patient's presentation of **forehead and entire facial weakness** is characteristic of a **lower motor neuron lesion** of the facial nerve, not a central (upper motor neuron) lesion.
More Ear anatomy and vestibular system US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.