Deep structures of the neck US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Deep structures of the neck. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Deep structures of the neck US Medical PG Question 1: A 17-year-old boy comes to the physician because of a 3-month history of pain in his right shoulder. He reports that he has stopped playing for his high school football team because of persistent difficulty lifting his right arm. Physical examination shows impaired active abduction of the right arm from 0 to 15 degrees. After passive abduction of the right arm to 15 degrees, the patient is able to raise his arm above his head. The dysfunctional muscle in this patient is most likely to be innervated by which of the following nerves?
- A. Long thoracic nerve
- B. Suprascapular nerve (Correct Answer)
- C. Upper subscapular nerve
- D. Accessory nerve
- E. Axillary nerve
Deep structures of the neck Explanation: ***Suprascapular nerve***
- The patient exhibits impaired active abduction from 0 to 15 degrees but normal abduction after passive assistance, indicating dysfunction of the **supraspinatus muscle**.
- The **supraspinatus muscle** is responsible for **initiating shoulder abduction** from 0 to 15 degrees, after which the deltoid muscle takes over for continued abduction.
- The **suprascapular nerve** innervates both the **supraspinatus** and **infraspinatus muscles**, with the supraspinatus being crucial for the initial phase of abduction.
*Long thoracic nerve*
- This nerve innervates the **serratus anterior muscle**, which is responsible for **scapular protraction** and upward rotation.
- Damage to the long thoracic nerve would typically result in **winged scapula**, not difficulty in initiating abduction.
*Upper subscapular nerve*
- The upper subscapular nerve innervates the **subscapularis muscle**, part of the rotator cuff.
- This muscle is primarily involved in **internal rotation** of the shoulder and contributes to adduction, not abduction.
*Accessory nerve*
- The accessory nerve (cranial nerve XI) innervates the **sternocleidomastoid** and **trapezius muscles**.
- Damage to this nerve would most likely present with weakness in **shrugging the shoulders** or turning the head, not difficulty with shoulder abduction.
*Axillary nerve*
- This nerve innervates the **deltoid muscle** and the **teres minor muscle**, and provides sensory input from the shoulder joint and lateral arm.
- The deltoid is responsible for **shoulder abduction** from 15 to 90 degrees; a deficit here would affect a different range of motion than what is described.
Deep structures of the neck US Medical PG Question 2: A 60-year-old woman is rushed to the emergency room after falling on her right elbow while walking down the stairs. She cannot raise her right arm. Her vital signs are stable, and the physical examination reveals loss of sensation over the upper lateral aspect of the right arm and shoulder. A radiologic evaluation shows a fracture of the surgical neck of the right humerus. Which of the following muscles is supplied by the nerve that is most likely damaged?
- A. Teres minor (Correct Answer)
- B. Teres major
- C. Subscapularis
- D. Infraspinatus
- E. Supraspinatus
Deep structures of the neck Explanation: ***Teres minor***
- A fracture of the **surgical neck of the humerus** often damages the **axillary nerve**, which innervates the **teres minor**.
- The axillary nerve also supplies the **deltoid muscle** and provides cutaneous sensation to the **upper lateral arm**, consistent with the patient's sensory loss.
*Teres major*
- This muscle is innervated by the **lower subscapular nerve**, which is less likely to be damaged in a surgical neck fracture.
- Its primary action is **adduction** and **internal rotation** of the arm.
*Subscapularis*
- The **subscapularis** is innervated by the **upper and lower subscapular nerves**.
- While it contributes to internal rotation, its nerve supply is typically protected in this type of fracture.
*Infraspinatus*
- The **infraspinatus** muscle is innervated by the **suprascapular nerve**.
- This nerve is generally not affected by a fracture of the surgical neck of the humerus.
*Supraspinatus*
- Similar to the infraspinatus, the **supraspinatus** is also innervated by the **suprascapular nerve**.
- Damage to this nerve due to a humeral surgical neck fracture is uncommon.
Deep structures of the neck US Medical PG Question 3: A 14-year-old boy is brought to the emergency department because of acute left-sided chest pain and dyspnea following a motor vehicle accident. His pulse is 122/min and blood pressure is 85/45 mm Hg. Physical examination shows distended neck veins and tracheal displacement to the right side. The left chest is hyperresonant to percussion and there are decreased breath sounds. This patient would most benefit from needle insertion at which of the following anatomical sites?
- A. 5th left intercostal space along the midclavicular line
- B. 8th left intercostal space along the posterior axillary line
- C. 2nd left intercostal space along the midclavicular line (Correct Answer)
- D. Subxiphoid space in the left sternocostal margin
- E. 5th left intercostal space along the midaxillary line
Deep structures of the neck Explanation: ***2nd left intercostal space along the midclavicular line***
- The patient's symptoms (chest pain, dyspnea, hypotension, distended neck veins, tracheal deviation, hyperresonance, and decreased breath sounds on the left) are classic signs of a **tension pneumothorax**.
- Immediate treatment for **tension pneumothorax** involves needle decompression at the **2nd intercostal space** in the midclavicular line to relieve pressure and restore hemodynamic stability.
*5th left intercostal space along the midclavicular line*
- This location is typically used for **chest tube insertion** in a more controlled setting, not for emergent needle decompression of a tension pneumothorax.
- While it's a safe location for pleural access, it is not the **first-line site** for immediate life-saving decompression.
*8th left intercostal space along the posterior axillary line*
- This site is too low and posterior for effective needle decompression of a tension pneumothorax, which requires rapid access to the **apex of the lung**.
- It is more commonly used for **thoracentesis** to drain fluid from the pleural cavity.
*Subxiphoid space in the left sternocostal margin*
- This location is primarily used for **pericardiocentesis** to drain fluid from the pericardial sac in cases of cardiac tamponade.
- It is not appropriate for addressing a **pneumothorax**, which involves air in the pleural space.
*5th left intercostal space along the midaxillary line*
- This site is a common alternative for **chest tube insertion** but is not the preferred or most immediate site for needle decompression of a tension pneumothorax.
- While it offers pleural access, the **2nd intercostal space** anteriorly is chosen for expediency and safety in an emergency.
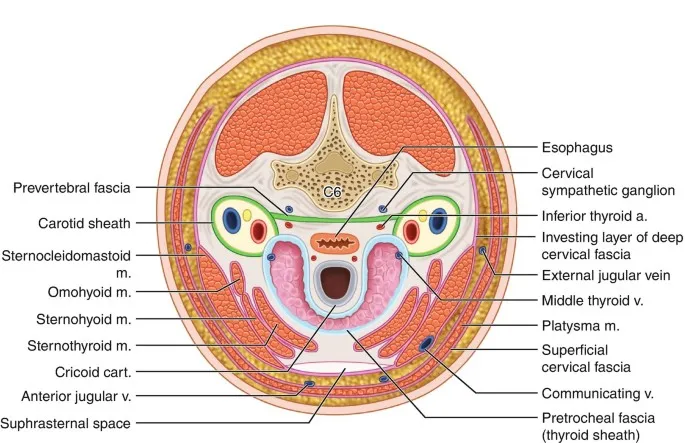
Deep structures of the neck US Medical PG Question 4: A 38-year-old woman undergoes hemithyroidectomy for treatment of localized, well-differentiated papillary thyroid carcinoma. The lesion is removed with clear margins. However, during the surgery, a structure lying directly adjacent to the superior thyroid artery at the upper pole of the thyroid lobe is damaged. This patient is most likely to experience which of the following symptoms?
- A. Shortness of breath
- B. Weakness of shoulder shrug
- C. Voice pitch limitation (Correct Answer)
- D. Difficulty swallowing
- E. Ineffective cough
Deep structures of the neck Explanation: ***Voice pitch limitation***
- Damage to the structure directly adjacent to the **superior thyroid artery** at the upper pole of the thyroid likely involves the **external branch of the superior laryngeal nerve (EBSLN)**.
- This nerve innervates the **cricothyroid muscle**, which is responsible for **tensing the vocal cords** and controlling **voice pitch**.
- Injury results in inability to change pitch, voice fatigue during prolonged speaking, and reduced vocal range.
*Shortness of breath*
- While damage to other nerves like the **recurrent laryngeal nerve** could cause vocal cord paralysis and potentially lead to airway compromise, this is less directly associated with the superior thyroid artery.
- Shortness of breath is not the specific consequence of EBSLN injury near the superior thyroid artery.
*Weakness of shoulder shrug*
- Weakness of shoulder shrug is associated with damage to the **spinal accessory nerve (cranial nerve XI)**, which innervates the **trapezius muscle**.
- This nerve is anatomically distinct from structures near the superior thyroid artery at the upper pole of the thyroid.
*Difficulty swallowing*
- Difficulty swallowing (dysphagia) can result from damage to the **vagus nerve (cranial nerve X)** or its pharyngeal branches, but it is not the direct consequence of injury near the superior thyroid artery.
- Damage to the EBSLN primarily affects voice pitch and quality, not swallowing.
*Ineffective cough*
- An ineffective cough results from paralysis of the vocal cords (preventing glottic closure) or weakness of respiratory muscles, typically from **recurrent laryngeal nerve** damage or phrenic nerve injury.
- EBSLN damage primarily affects voice pitch and does not significantly impair cough effectiveness.
Deep structures of the neck US Medical PG Question 5: A 47-year-old man presents to you with gradual loss of voice and difficulty swallowing for the past couple of months. The difficulty of swallowing is for both solid and liquid foods. His past medical history is insignificant except for occasional mild headaches. Physical exam also reveals loss of taste sensation on the posterior third of his tongue and palate, weakness in shrugging his shoulders, an absent gag reflex, and deviation of the uvula away from the midline. MRI scanning was suggested which revealed a meningioma that was compressing some cranial nerves leaving the skull. Which of the following openings in the skull transmit the affected cranial nerves?
- A. Jugular foramen (Correct Answer)
- B. Foramen rotundum
- C. Foramen spinosum
- D. Foramen ovale
- E. Foramen lacerum
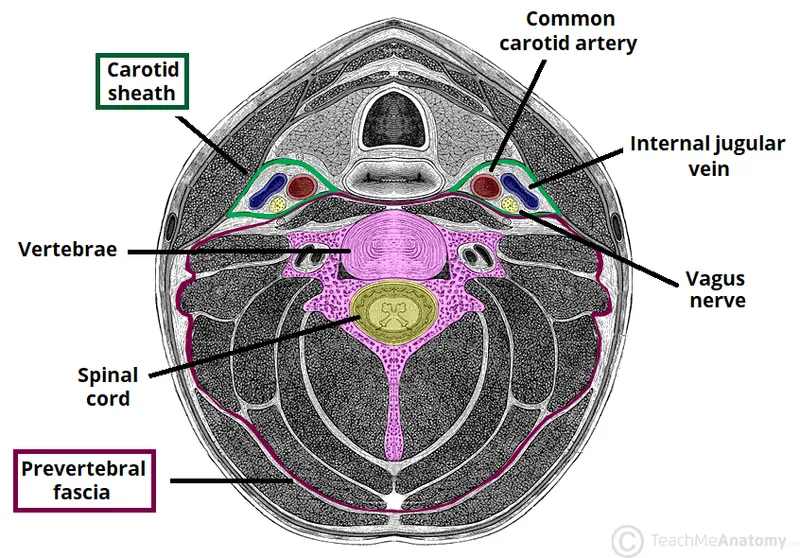
Deep structures of the neck Explanation: ***Jugular foramen***
- The symptoms described—loss of voice, difficulty swallowing, loss of taste on the posterior third of the tongue, absent gag reflex, and uvula deviation—point to impairment of **cranial nerves IX (glossopharyngeal), X (vagus), XI (accessory)**, which all exit the skull via the **jugular foramen**.
- The **vagus nerve** (CN X) is responsible for voice and swallowing (via innervation of the pharynx and larynx), the **glossopharyngeal nerve** (CN IX) for taste from the posterior third of the tongue and the gag reflex, and the **accessory nerve** (CN XI) for shoulder shrugging (trapezius and sternocleidomastoid muscles).
- Note: Loss of taste on the palate may involve CN VII (facial nerve) fibers, but the dominant clinical picture with absent gag reflex, uvula deviation, dysphagia, and dysphonia clearly indicates jugular foramen pathology.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, a branch of the trigeminal nerve.
- Damage to V2 would primarily cause sensory deficits in the midface and upper teeth, which are not described in this patient.
*Foramen spinosum*
- The **foramen spinosum** transmits the **middle meningeal artery** and the **meningeal branch of the mandibular nerve (V3)**.
- Injury here would not explain the constellation of symptoms related to voice, swallowing, taste, or shoulder movement.
*Foramen ovale*
- The **foramen ovale** transmits the **mandibular nerve (V3)**, the **accessory meningeal artery**, and occasionally the superficial petrosal nerve.
- Damage to V3 would result in sensory loss to the lower face and motor deficits in the muscles of mastication, which are not reported.
*Foramen lacerum*
- The **foramen lacerum** is filled with cartilage in vivo and does not typically transmit major neurovascular structures directly through its aperture.
- The **internal carotid artery** passes superior to it, and some small nerves may traverse its vicinity, but not the specific cranial nerves indicated by the patient's symptoms.
Deep structures of the neck US Medical PG Question 6: A patient undergoes an MRI of the brain that reveals a tumor compressing the facial nerve at the internal acoustic meatus. Which of the following symptoms would most likely be present?
- A. Loss of taste in the posterior third of the tongue
- B. Loss of taste in the anterior two-thirds of the tongue
- C. Decreased salivation
- D. Facial muscle weakness and hyperacusis (Correct Answer)
- E. Decreased lacrimation
Deep structures of the neck Explanation: ***Facial muscle weakness and hyperacusis***
- Compression of the **facial nerve (CN VII)** before it branches within the facial canal affects both its motor and special visceral afferent functions. [1]
- **Facial muscle weakness** results from damage to the motor fibers, while **hyperacusis** occurs due to paralysis of the stapedius muscle, innervated by the facial nerve's branch to the stapedius. [1]
*Loss of taste in the posterior third of the tongue*
- **Taste sensation** from the posterior third of the tongue is conveyed by the **glossopharyngeal nerve (CN IX)**, not the facial nerve.
- Therefore, compression of the facial nerve at the internal acoustic meatus would not impact taste in this region.
*Loss of taste in the anterior two-thirds of the tongue*
- While the **chorda tympani nerve** (a branch of the facial nerve) carries taste from the anterior two-thirds of the tongue, this branch typically separates from the facial nerve **distal to the internal acoustic meatus**.
- Compression at the internal acoustic meatus would affect the main trunk before this branching, but other symptoms are more prominent. [1]
*Decreased salivation*
- **Salivation** (specifically from the submandibular and sublingual glands) is mediated by the **chorda tympani nerve**, a branch of the facial nerve. [1]
- Similar to taste, this branch usually separates later, and while salivation can be affected, other symptoms like facial weakness and hyperacusis are more consistently prominent with proximal compression.
*Decreased lacrimation*
- **Lacrimation** is primarily controlled by the **greater petrosal nerve**, which branches off the facial nerve earlier in its course.
- While theoretically possible with very proximal compression affecting all components, compression at the internal acoustic meatus is more commonly associated with the motor and stapedius muscle function impairments first due to the spatial arrangement of fibers.
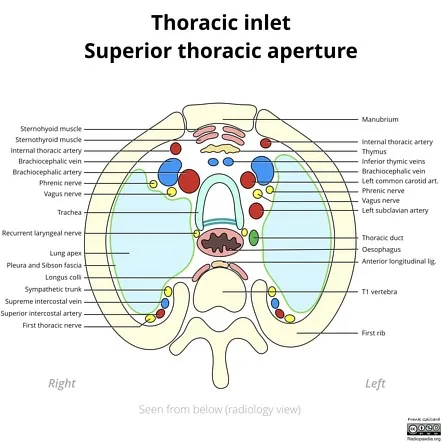
Deep structures of the neck US Medical PG Question 7: A 55-year-old male bodybuilder presents to the emergency department with weakness of his right arm. The patient states he has experienced these symptoms for a few weeks; however, today his hand felt so weak he dropped his cup of tea. The patient has a past medical history of diabetes. He drinks 2-7 alcoholic drinks per day and has smoked 2 packs of cigarettes per day since he was 25. The patient admits to using anabolic steroids. He has lost 17 pounds since he last came to the emergency department 1 month ago. His temperature is 99.5°F (37.5°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam reveals decreased sensation in the right arm and 2/5 strength in the right arm and 5/5 strength in the left arm. The patient states that he is experiencing a dull aching and burning pain in his right arm during the exam. Which of the following is the most likely diagnosis?
- A. Brachial plexopathy
- B. Apical lung tumor (Correct Answer)
- C. Subclavian steal syndrome
- D. Cerebral infarction
- E. Scalenus anticus syndrome
Deep structures of the neck Explanation: ***Apical lung tumor***
- The patient's history of **heavy smoking** and **anabolic steroid use**, along with **unexplained weight loss**, **weakness**, and **sensory deficits in the arm**, are highly suggestive of an apical lung tumor (Pancoast tumor) compressing the brachial plexus.
- The **dull aching and burning pain** in the arm is a classic symptom of brachial plexus involvement caused by tumor invasion.
*Brachial plexopathy*
- While brachial plexopathy explains the **arm weakness and sensory changes**, it is a general term and doesn't identify the underlying cause.
- The patient's risk factors (smoking, weight loss) point to a more specific etiology than just idiopathic plexopathy.
*Subclavian steal syndrome*
- This condition involves **vertebrobasilar insufficiency** due to subclavian artery stenosis, typically presenting with neurologic symptoms like vertigo, syncope, and arm claudication, especially during arm exercise.
- It does not typically cause **unilateral arm weakness and sensory deficits** associated with unexplained weight loss.
*Cerebral infarction*
- A cerebral infarction (stroke) would cause **sudden-onset neurological deficits**, which is inconsistent with the patient's several weeks of symptoms progressing to severe weakness.
- While it can cause hemiparesis, the presentation of **dull aching and burning pain** in the arm suggests peripheral nerve involvement rather than a central lesion.
*Scalenus anticus syndrome*
- Also known as **thoracic outlet syndrome**, this typically involves compression of the brachial plexus or subclavian vessels, often due to anatomical variations or trauma.
- While it can cause arm pain and weakness, the patient's significant **smoking history** and **unexplained weight loss** strongly point to a more serious underlying malignancy.
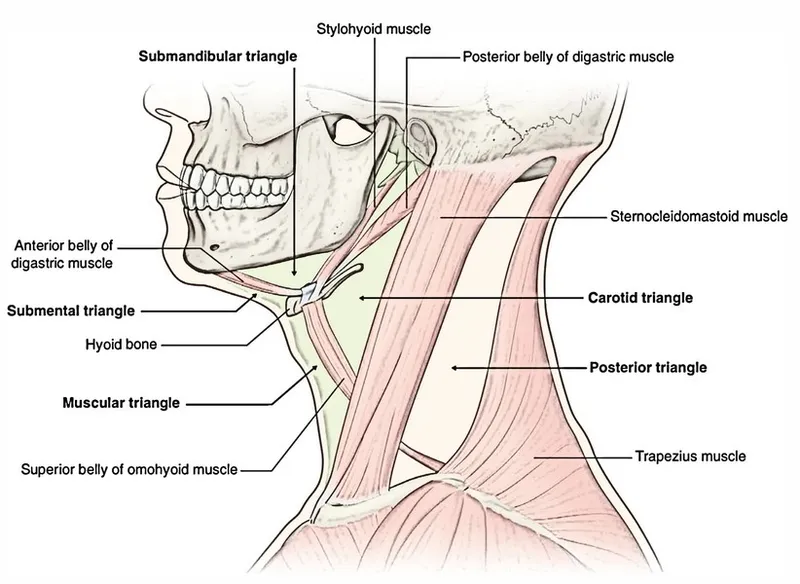
Deep structures of the neck US Medical PG Question 8: During a surgical procedure involving the posterior triangle of the neck, which of the following muscles forms its anterior boundary?
- A. Scalene anterior
- B. Trapezius
- C. Sternocleidomastoid (Correct Answer)
- D. Omohyoid
Deep structures of the neck Explanation: ***Sternocleidomastoid***
- The **sternocleidomastoid muscle** forms the **anterior boundary** of the **posterior triangle of the neck**.
- Its broad origin on the sternum and clavicle and insertion on the mastoid process help define this triangular region.
*Scalene anterior*
- The **scalene anterior muscle** is located deeper in the neck and is not a direct boundary of the posterior triangle.
- This muscle is part of the **floor** of the posterior triangle, along with other prevertebral muscles, but does not form its anterior border.
*Trapezius*
- The **trapezius muscle** forms the **posterior boundary** of the posterior triangle of the neck, running from the nuchal line and thoracic vertebrae to the clavicle and scapula.
- It would be incorrect to identify it as the anterior boundary.
*Omohyoid*
- The **inferior belly of the omohyoid muscle** crosses the posterior triangle, subdividing it into occipital and supraclavicular triangles.
- It does not form one of the main borders of the entire posterior triangle.
Deep structures of the neck US Medical PG Question 9: A 25-year-old man presents to the clinic with a midline swelling in his neck. He is unsure about when it appeared. He denies any difficulty with swallowing or hoarseness. His past medical history is insignificant. On physical examination, there is a 1 cm x 2 cm firm mildly tender nodule on the anterior midline aspect of the neck which moves with deglutition and elevates with protrusion of the tongue. Which of the following is the most likely embryologic origin of the nodule in this patient?
- A. Midline endoderm of the pharynx (Correct Answer)
- B. 1st and 2nd pharyngeal arch
- C. The branchial cleft
- D. 4th pharyngeal arch
- E. 4th pharyngeal pouch
Deep structures of the neck Explanation: ***Midline endoderm of the pharynx***
- The symptoms described, particularly a midline neck swelling that **moves with deglutition** and **elevates with tongue protrusion**, are classic for a **thyroglossal duct cyst**.
- Thyroglossal duct cysts arise from remnants of the **thyroglossal duct**, an embryonic structure that forms from the **midline endoderm of the pharyngeal floor** and descends to form the thyroid gland.
*1st and 2nd pharyngeal arch*
- The 1st and 2nd pharyngeal arches primarily contribute to the formation of structures in the **mandible**, **maxilla**, **middle ear**, and **hyoid bone**.
- Abnormalities in these arches typically lead to conditions like **Treacher Collins syndrome** or **Pierre Robin sequence**, not midline neck cysts with these specific movement characteristics.
*The branchial cleft*
- **Branchial cleft cysts** typically present as **lateral neck masses**, often anterior to the sternocleidomastoid muscle, and usually do not move with deglutition or tongue protrusion.
- They arise from incomplete obliteration of **pharyngeal clefts**, which are ectodermal structures.
*4th pharyngeal arch*
- The 4th pharyngeal arch contributes to the formation of the **cricothyroid muscle**, part of the **pharynx**, and the **laryngeal cartilages**.
- Anomalies of the 4th pharyngeal arch are rare and typically involve **vascular structures** or **recurrent laryngeal nerve** abnormalities, not midline neck cysts.
*4th pharyngeal pouch*
- The 4th pharyngeal pouch contributes to the development of the **superior parathyroid glands** and the **ultimobranchial body** (which gives rise to parafollicular C cells of the thyroid).
- Malformations of this pouch are associated with parathyroid and thyroid conditions, not midline thyroglossal duct cysts.
Deep structures of the neck US Medical PG Question 10: Impaired gag reflex is seen due to a lesion in which cranial nerves?
- A. CN V&VI
- B. CN X & XI
- C. CN IX & X (Correct Answer)
- D. CN VII & VIII
- E. CN XI & XII
Deep structures of the neck Explanation: ***Correct: CN IX & X***
The **gag reflex (pharyngeal reflex)** is a protective reflex involving two cranial nerves:
- **Afferent limb**: **CN IX (Glossopharyngeal nerve)** provides sensory innervation to the posterior third of the tongue, oropharynx, and pharyngeal walls
- **Efferent limb**: **CN X (Vagus nerve)** provides motor innervation to the pharyngeal muscles (via the pharyngeal plexus) that contract during the reflex
**Clinical correlation**: Testing the gag reflex helps assess brainstem function and the integrity of CN IX and X. Impairment suggests lesions affecting these nerves or their nuclei in the medulla.
*Incorrect: CN V & VI*
- CN V (Trigeminal) provides facial sensation and motor to muscles of mastication, not involved in gag reflex
- CN VI (Abducens) controls lateral rectus muscle for eye abduction
*Incorrect: CN X & XI*
- While CN X is involved, CN XI (Accessory nerve) innervates sternocleidomastoid and trapezius muscles, not pharyngeal muscles
*Incorrect: CN VII & VIII*
- CN VII (Facial) controls facial expression and taste from anterior 2/3 of tongue
- CN VIII (Vestibulocochlear) is involved in hearing and balance, not the gag reflex
*Incorrect: CN XI & XII*
- CN XI (Accessory) innervates SCM and trapezius
- CN XII (Hypoglossal) provides motor to intrinsic and extrinsic tongue muscles, not pharyngeal muscles involved in gag reflex
More Deep structures of the neck US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.