Cranial nerves and their pathways US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cranial nerves and their pathways. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cranial nerves and their pathways US Medical PG Question 1: An otherwise healthy 45-year-old man comes to the physician because of a painful ulcer on his tongue for 3 days. Examination shows a shallow, tender 5-mm wide ulcer on the lateral aspect of the tongue, adjacent to his left first molar. There is no induration surrounding the ulcer or cervical lymphadenopathy. A lesion of the cranial nerve responsible for the transmission of pain from this ulcer would most likely result in which of the following?
- A. Loss of taste from the supraglottic region
- B. Lateral deviation of the tongue
- C. Inability to wrinkle the forehead
- D. Decreased sensation in the upper lip
- E. Loss of sensation in the anterior two-thirds of the tongue (Correct Answer)
Cranial nerves and their pathways Explanation: ***Loss of sensation in the anterior two-thirds of the tongue***
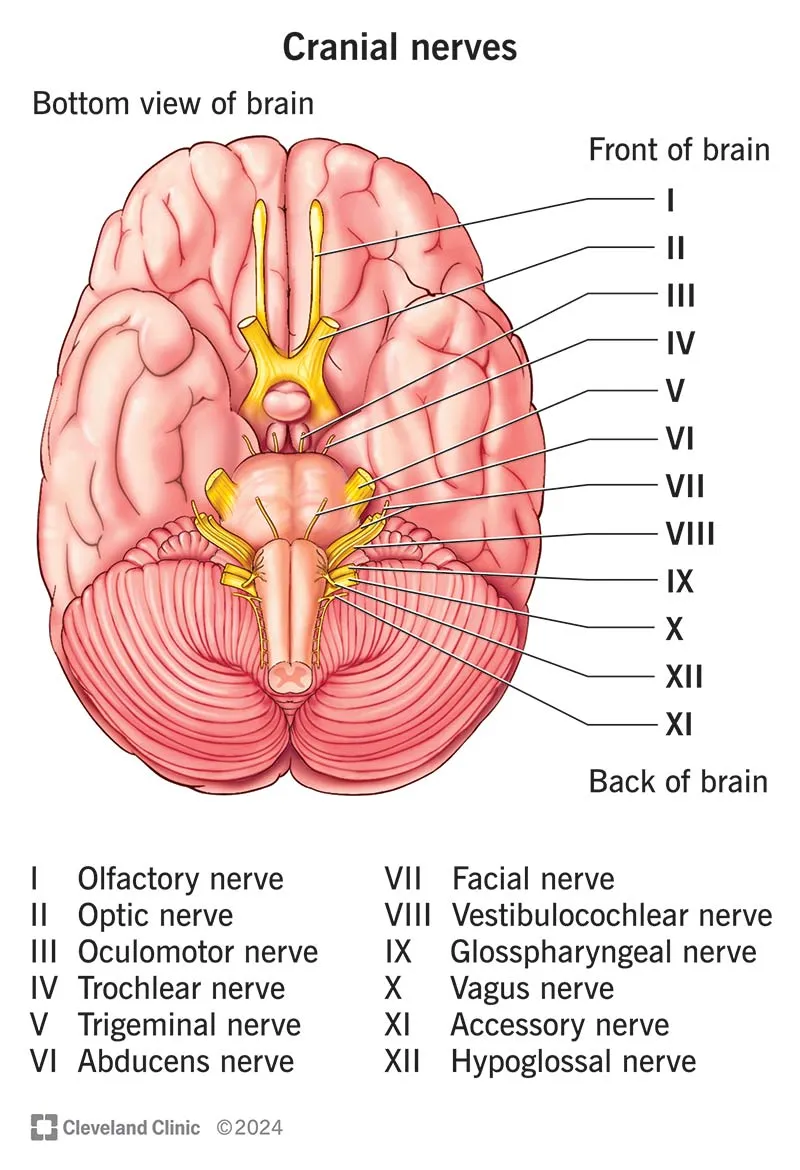
- The sensation of pain from the **anterior two-thirds of the tongue** is transmitted by the **lingual nerve**, which is a branch of the mandibular division (V3) of the **trigeminal nerve**. A lesion affecting this nerve would therefore cause loss of sensation in this region.
- The ulcer is located on the **lateral aspect of the tongue**, placing it within the distribution of the lingual nerve.
*Loss of taste from the supraglottic region*
- **Taste sensation** from the **supraglottic region** and epiglottis is primarily mediated by the **superior laryngeal nerve** (a branch of the vagus nerve, CN X), not the nerve responsible for pain sensation from the anterior tongue.
- A lesion of the lingual nerve would affect taste sensation from the **anterior two-thirds of the tongue** (carried by the chorda tympani, a branch of CN VII, which joins the lingual nerve), but not the supraglottic region.
*Lateral deviation of the tongue*
- **Lateral deviation of the tongue** (towards the side of the lesion) occurs due to damage to the **hypoglossal nerve (CN XII)**, which innervates the intrinsic and extrinsic muscles of the tongue.
- This is a motor deficit, whereas the question describes a sensory issue related to pain transmission from an ulcer on the tongue.
*Inability to wrinkle the forehead*
- The **inability to wrinkle the forehead** (along with other facial expressions) results from damage to the **facial nerve (CN VII)**, specifically its temporal branch.
- This is a motor deficit affecting the muscles of facial expression, unrelated to pain sensation from the tongue.
*Decreased sensation in the upper lip*
- **Sensation in the upper lip** is supplied by the **infraorbital nerve**, a branch of the maxillary division (V2) of the **trigeminal nerve**.
- A lesion affecting the nerve responsible for pain from the anterior two-thirds of the tongue (lingual nerve, V3) would not directly impact sensation in the upper lip.
Cranial nerves and their pathways US Medical PG Question 2: A 54-year-old man is brought to the emergency department 30 minutes after being hit by a car while crossing the street. He had a left-sided tonic-clonic seizure and one episode of vomiting while being transported to the hospital. On arrival, he is not oriented to person, place, or time. Physical examination shows flaccid paralysis of all extremities. A CT scan of the head is shown. This patient's symptoms are most likely the result of a hemorrhage in which of the following structures?
- A. Between the dura mater and the arachnoid mater
- B. Into the cerebral parenchyma
- C. Between the skull and the dura mater
- D. Between the arachnoid mater and the pia mater (Correct Answer)
- E. Into the ventricular system
Cranial nerves and their pathways Explanation: ***Between the arachnoid mater and the pia mater (Correct)***
- The CT scan demonstrates diffuse high-density (white) material within the sulci and basal cisterns, indicative of a **subarachnoid hemorrhage**. This space is located between the arachnoid mater and the pia mater.
- The patient's presentation with altered mental status, seizures, vomiting, and flaccid paralysis following trauma is consistent with the severe neurological impact of a **traumatic subarachnoid hemorrhage**.
*Between the dura mater and the arachnoid mater (Incorrect)*
- Hemorrhage in this location is known as a **subdural hematoma**, which typically appears as a crescent-shaped collection of blood.
- While possible in trauma, the CT image shows blood primarily filling the sulci, not a subdural collection.
*Into the cerebral parenchyma (Incorrect)*
- This would be an **intraparenchymal hemorrhage**, appearing as a focal area of high density within the brain tissue itself.
- Although there might be some associated parenchymal injury in severe trauma, the predominant pattern seen on the CT is diffuse blood in the subarachnoid space.
*Between the skull and the dura mater (Incorrect)*
- This describes an **epidural hematoma**, often characterized by a lenticular (lens-shaped) collection of blood due to its confinement by dural attachments.
- The CT image does not show a lenticular collection of blood in this space.
*Into the ventricular system (Incorrect)*
- **Intraventricular hemorrhage** would show blood filling the cerebral ventricles.
- While subarachnoid hemorrhage can sometimes extend into the ventricles, the primary finding on this CT is diffuse blood in the subarachnoid space, not isolated ventricular blood.
Cranial nerves and their pathways US Medical PG Question 3: A 55-year-old woman with a 1-year history of left-sided tinnitus is diagnosed with a tumor at the left cerebellopontine angle affecting the glossopharyngeal nerve. Sialometry shows decreased production of saliva from the left parotid gland. The finding on sialometry is best explained by a lesion of the nerve that is also responsible for which of the following?
- A. Protrusion of the tongue
- B. Afferent limb of the cough reflex
- C. Afferent limb of the gag reflex (Correct Answer)
- D. Equilibrium and balance
- E. Taste sensation of tip of the tongue
Cranial nerves and their pathways Explanation: ***Afferent limb of the gag reflex***
- The **glossopharyngeal nerve (CN IX)** provides **parasympathetic innervation** to the **parotid gland**, explaining the decreased saliva production on sialometry.
- CN IX is also responsible for the **afferent limb of the gag reflex** and taste sensation from the posterior one-third of the tongue.
*Protrusion of the tongue*
- **Protrusion of the tongue** is primarily controlled by the **hypoglossal nerve (CN XII)**.
- A lesion affecting the glossopharyngeal nerve would not directly impact the ability to protrude the tongue.
*Afferent limb of the cough reflex*
- The **afferent limb of the cough reflex** is primarily mediated by the **vagus nerve (CN X)**, which innervates the laryngeal and tracheobronchial mucosa.
- While there can be some overlap, the glossopharyngeal nerve is not the primary mediator for this reflex.
*Equilibrium and balance*
- **Equilibrium and balance** are primarily maintained by the **vestibulocochlear nerve (CN VIII)**, which is responsible for transmitting vestibular information.
- A lesion of the glossopharyngeal nerve would not primarily affect these functions, although cerebellopontine angle tumors can affect CN VIII.
*Taste sensation of tip of the tongue*
- **Taste sensation from the anterior two-thirds of the tongue** (including the tip) is conveyed by the **facial nerve (CN VII)** via the chorda tympani.
- The glossopharyngeal nerve (CN IX) provides taste sensation to the posterior one-third of the tongue.
Cranial nerves and their pathways US Medical PG Question 4: A 72-year-old woman is brought in to the emergency department after her husband noticed that she appeared to be choking on her dinner. He performed a Heimlich maneuver but was concerned that she may have aspirated something. The patient reports a lack of pain and temperature on the right half of her face, as well as the same lack of sensation on the left side of her body. She also states that she has been feeling "unsteady" on her feet. On physical exam you note a slight ptosis on the right side. She is sent for an emergent head CT. Where is the most likely location of the neurological lesion?
- A. Pons
- B. Internal capsule
- C. Cervical spinal cord
- D. Medulla (Correct Answer)
- E. Midbrain
Cranial nerves and their pathways Explanation: ***Medulla***
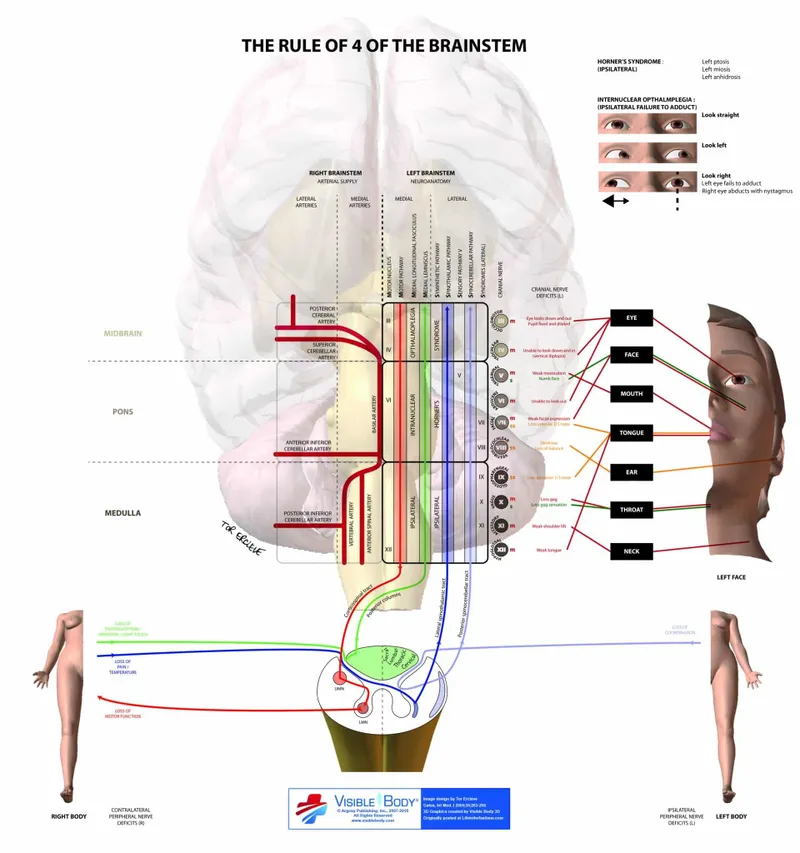
- This presentation describes **Wallenberg syndrome** (lateral medullary syndrome), characterized by **ipsilateral facial sensory loss**, **contralateral body sensory loss**, and **ataxia** due to involvement of the spinothalamic tracts, trigeminal nucleus, and cerebellar pathways.
- **Dysphagia** (choking) and **Horner's syndrome** (ptosis, miosis, anhidrosis) are also classic signs, specifically the ptosis seen here, pointing to an infarct in the **lateral medulla**.
*Pons*
- Lesions in the pons typically present with varying degrees of **cranial nerve deficits** (e.g., trigeminal, abducens, facial) and **motor or sensory deficits** affecting both sides of the body due to the decussation of tracts.
- The specific combination of **crossed sensory loss** and other symptoms seen here is not characteristic of isolated pontine lesions.
*Internal capsule*
- A lesion in the internal capsule would primarily cause **contralateral motor weakness (hemiparesis)** and **sensory loss** affecting both the face and body on the same side, without the ipsilateral facial involvement.
- It would not explain the **ataxia** or specific cranial nerve signs like ptosis.
*Cervical spinal cord*
- Spinal cord lesions result in **sensory and motor deficits below the level of the lesion**, affecting both sides of the body symmetrically, or ipsilaterally depending on the tract involved.
- They do not cause **facial sensory disturbances**, **dysphagia**, or **ataxia** in the manner described.
*Midbrain*
- Midbrain lesions typically involve the **oculomotor nerve** (CN III), causing eye movement abnormalities, and can result in **contralateral hemiparesis**.
- They do not produce the **crossed sensory deficits** (ipsilateral face, contralateral body) or **ataxia** characteristic of this case.
Cranial nerves and their pathways US Medical PG Question 5: A 47-year-old man presents to you with gradual loss of voice and difficulty swallowing for the past couple of months. The difficulty of swallowing is for both solid and liquid foods. His past medical history is insignificant except for occasional mild headaches. Physical exam also reveals loss of taste sensation on the posterior third of his tongue and palate, weakness in shrugging his shoulders, an absent gag reflex, and deviation of the uvula away from the midline. MRI scanning was suggested which revealed a meningioma that was compressing some cranial nerves leaving the skull. Which of the following openings in the skull transmit the affected cranial nerves?
- A. Jugular foramen (Correct Answer)
- B. Foramen rotundum
- C. Foramen spinosum
- D. Foramen ovale
- E. Foramen lacerum
Cranial nerves and their pathways Explanation: ***Jugular foramen***
- The symptoms described—loss of voice, difficulty swallowing, loss of taste on the posterior third of the tongue, absent gag reflex, and uvula deviation—point to impairment of **cranial nerves IX (glossopharyngeal), X (vagus), XI (accessory)**, which all exit the skull via the **jugular foramen**.
- The **vagus nerve** (CN X) is responsible for voice and swallowing (via innervation of the pharynx and larynx), the **glossopharyngeal nerve** (CN IX) for taste from the posterior third of the tongue and the gag reflex, and the **accessory nerve** (CN XI) for shoulder shrugging (trapezius and sternocleidomastoid muscles).
- Note: Loss of taste on the palate may involve CN VII (facial nerve) fibers, but the dominant clinical picture with absent gag reflex, uvula deviation, dysphagia, and dysphonia clearly indicates jugular foramen pathology.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, a branch of the trigeminal nerve.
- Damage to V2 would primarily cause sensory deficits in the midface and upper teeth, which are not described in this patient.
*Foramen spinosum*
- The **foramen spinosum** transmits the **middle meningeal artery** and the **meningeal branch of the mandibular nerve (V3)**.
- Injury here would not explain the constellation of symptoms related to voice, swallowing, taste, or shoulder movement.
*Foramen ovale*
- The **foramen ovale** transmits the **mandibular nerve (V3)**, the **accessory meningeal artery**, and occasionally the superficial petrosal nerve.
- Damage to V3 would result in sensory loss to the lower face and motor deficits in the muscles of mastication, which are not reported.
*Foramen lacerum*
- The **foramen lacerum** is filled with cartilage in vivo and does not typically transmit major neurovascular structures directly through its aperture.
- The **internal carotid artery** passes superior to it, and some small nerves may traverse its vicinity, but not the specific cranial nerves indicated by the patient's symptoms.
Cranial nerves and their pathways US Medical PG Question 6: A 26-year-old man comes to the physician for a follow-up examination. Two weeks ago, he was treated in the emergency department for head trauma after being hit by a bicycle while crossing the street. Neurological examination shows decreased taste on the right anterior tongue. This patient's condition is most likely caused by damage to a cranial nerve that is also responsible for which of the following?
- A. Facial sensation
- B. Parotid gland salivation
- C. Uvula movement
- D. Tongue protrusion
- E. Eyelid closure (Correct Answer)
Cranial nerves and their pathways Explanation: ***Eyelid closure***
- The patient's **decreased taste on the right anterior tongue** indicates damage to the **facial nerve (CN VII)**, specifically the chorda tympani branch.
- The facial nerve is also responsible for innervating the muscles of **facial expression**, including the **orbicularis oculi** which closes the eyelid.
*Facial sensation*
- **Facial sensation** (touch, pain, temperature) is primarily mediated by the **trigeminal nerve (CN V)**, not the facial nerve.
- Damage to the trigeminal nerve would result in sensory deficits, not taste disturbances on the anterior tongue.
*Parotid gland salivation*
- **Parotid gland salivation** is primarily controlled by the **glossopharyngeal nerve (CN IX)** via the otic ganglion.
- The facial nerve (CN VII) innervates the **submandibular and sublingual glands**, but not the parotid gland.
*Uvula movement*
- **Uvula movement** and elevation of the soft palate are primarily controlled by the **vagus nerve (CN X)**, specifically through the pharyngeal plexus.
- Damage to CN X would typically lead to deviation of the uvula away from the paralyzed side.
*Tongue protrusion*
- **Tongue protrusion** (moving the tongue out) is the primary function of the **hypoglossal nerve (CN XII)**.
- Damage to the hypoglossal nerve would cause the tongue to deviate towards the lesioned side upon protrusion due to unopposed action of the healthy genioglossus muscle.
Cranial nerves and their pathways US Medical PG Question 7: A 4-year-old boy is brought to the physician because of a progressive headache and neck pain for 2 weeks. During this period, he has had multiple episodes of dizziness and tingling sensations in his arms and hands. A year ago, he underwent closed reduction of a dislocated shoulder that he suffered after a fall. He underwent surgical removal of a sac-like protuberance on his lower back, soon after being born. His temperature is 36.7°C (98°F), pulse is 80/min, and blood pressure is 100/80 mm Hg. His neck is supple. Neurological examination shows sensorineural hearing loss bilaterally and normal gross motor function. Fundoscopy reveals bilateral optic disk swelling. An MRI of the brain is shown. Which of the following is the most likely cause of this patient's symptoms?
- A. Brachial plexus injury
- B. Vestibular schwannoma
- C. Chiari II malformation (Correct Answer)
- D. Medulloblastoma
- E. Intraventricular hemorrhage
Cranial nerves and their pathways Explanation: ***Chiari II malformation***
- The patient's history of surgical removal of a "sac-like protuberance" on his lower back soon after birth suggests a **myelomeningocele**, which is strongly associated with Chiari II malformation.
- Symptoms like progressive headache, neck pain, dizziness, tingling in arms/hands, bilateral optic disk swelling (indicating **increased intracranial pressure**), and sensorineural hearing loss are consistent with brainstem and cranial nerve compression common in Chiari II.
*Brachial plexus injury*
- This typically presents with acute, localized weakness, numbness, or pain in the arm and hand **due to nerve damage**, often following trauma like a dislocated shoulder.
- It would not explain the **progressive headache**, optic disc swelling, or the patient's congenital history of a lower back malformation.
*Vestibular schwannoma*
- This tumor primarily affects the **vestibulocochlear nerve (CN VIII)**, causing **unilateral hearing loss**, tinnitus, and balance issues.
- It would not typically present with bilateral hearing loss, increased intracranial pressure symptoms (like optic disc swelling), or be linked to a congenital spinal defect.
*Medulloblastoma*
- While a **medulloblastoma** can cause symptoms of increased intracranial pressure (headache, optic disc swelling) and sometimes dizziness, it is a **malignant brain tumor**.
- It does not explain the patient's history of a congenital spinal defect (myelomeningocele) or the specific tingling sensations in the arms and hands in the context of brainstem compression.
*Intraventricular hemorrhage*
- This usually occurs in **neonates, especially premature infants**, and presents with acute neurological deficits, apnea, bradycardia, or seizures.
- It is unlikely to present as progressive headache and neck pain in a 4-year-old and does not account for the congenital spinal defect or chronic symptoms.
Cranial nerves and their pathways US Medical PG Question 8: A 28-year-old man presents with visual disturbances. He says that he is having double vision since he woke up this morning. His past medical history is insignificant except for occasional mild headaches. The patient is afebrile and his vitals are within normal limits. On physical examination of his eyes, there is paralysis of left lateral gaze. Also, at rest, there is esotropia of the left eye. A noncontrast CT scan of the head reveals a tumor impinging on one of his cranial nerves. Which of the following nerves is most likely affected?
- A. Trigeminal nerve
- B. Optic nerve
- C. Oculomotor nerve
- D. Trochlear nerve
- E. Abducens nerve (Correct Answer)
Cranial nerves and their pathways Explanation: ***Abducens nerve***
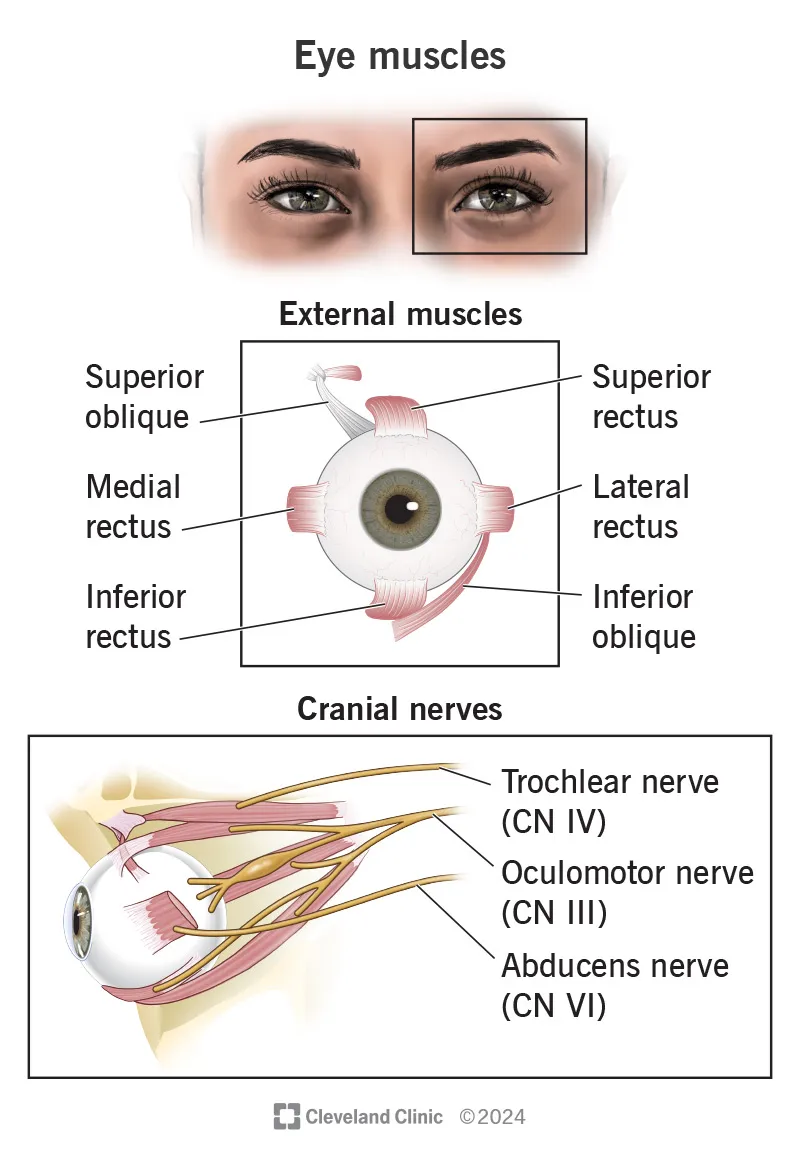
- **Paralysis of left lateral gaze** and **esotropia** (inward turning of the eye) at rest are classic signs of a **left abducens nerve (CN VI) palsy**. This nerve exclusively innervates the **lateral rectus muscle**, which is responsible for abducting (moving outward) the eye.
- Impingement from a **tumor** is a common cause of cranial nerve palsies, and the presentation perfectly matches the function of the abducens nerve.
*Trigeminal nerve*
- The **trigeminal nerve (CN V)** is responsible for **facial sensation** and **mastication** (chewing).
- Dysfunction would present as facial numbness, pain, or weakness in chewing, not visual disturbances or eye movement issues.
*Optic nerve*
- The **optic nerve (CN II)** transmits **visual information** from the retina to the brain.
- Lesions typically cause **vision loss** (e.g., blindness, scotoma, visual field defects), not double vision or eye movement paralysis.
*Oculomotor nerve*
- The **oculomotor nerve (CN III)** controls most **extraocular muscles** (medial, superior, inferior rectus, inferior oblique) and the **levator palpebrae superioris** (eyelid elevation), as well as pupillary constriction.
- A palsy would typically present with a **"down and out" eye**, **ptosis** (drooping eyelid), and **mydriasis** (dilated pupil), which are not described.
*Trochlear nerve*
- The **trochlear nerve (CN IV)** innervates the **superior oblique muscle**, which depresses and intorts the eye.
- A palsy typically causes **vertical double vision**, especially when looking down and inward, and a compensatory head tilt away from the affected side. This does not match the described lateral gaze paralysis.
Cranial nerves and their pathways US Medical PG Question 9: A 65-year-old female with a past medical history of hypertension presents to her primary care doctor with a 3 month history of spasmodic facial pain. The pain is located in her right cheek and seems to be triggered when she smiles, chews, or brushes her teeth. The pain is sharp and excruciating, lasts for a few seconds, and occurs up to twenty times per day. She denies headaches, blurry vision, facial weakness, or changes in her memory. She feels rather debilitated and has modified much of her daily activities to avoid triggering the spasms. In the clinic, her physical exam is within normal limits. Her primary care doctor prescribes carbamazepine and asks her to follow up in a few weeks. Which cranial nerve is most likely involved in the patient's disease process?
- A. CN III
- B. CN V (Correct Answer)
- C. CN VI
- D. CN VII
- E. CN IV
Cranial nerves and their pathways Explanation: ***CN V***
- The patient's presentation of **recurrent, sharp, excruciating, unilateral facial pain** triggered by movements like chewing, smiling, or brushing teeth is classic for **trigeminal neuralgia**.
- **Trigeminal neuralgia** specifically affects the **trigeminal nerve (CN V)**, which has sensory branches covering the face, and is often treated with **carbamazepine**.
*CN III*
- The **oculomotor nerve (CN III)** is primarily involved in **eye movement** and **pupillary constriction**.
- Damage to CN III typically causes **diplopia, ptosis,** and **pupil dilation**, which are not present in this patient's symptoms.
*CN VI*
- The **abducens nerve (CN VI)** controls the **lateral rectus muscle**, responsible for **abducting the eye** (moving it outward).
- Dysfunction typically results in **diplopia** and an inability to move the eye laterally, not facial pain.
*CN VII*
- The **facial nerve (CN VII)** controls **facial expressions**, taste sensation from the anterior two-thirds of the tongue, and lacrimation/salivation.
- While it innervates facial muscles, its involvement typically presents as **facial weakness** or **paralysis** (e.g., Bell's palsy), not sharp, spasmodic pain.
*CN IV*
- The **trochlear nerve (CN IV)** innervates the **superior oblique muscle**, which is involved in rotating and depressing the eye.
- Lesions usually lead to **vertical diplopia**, particularly when looking down and inward, which is unrelated to the described facial pain.
Cranial nerves and their pathways US Medical PG Question 10: Where does the only cranial nerve without a thalamic relay nucleus enter the skull?
- A. Superior orbital fissure
- B. Internal auditory meatus
- C. Foramen rotundum
- D. Jugular foramen
- E. Cribriform plate (Correct Answer)
Cranial nerves and their pathways Explanation: ***Cribriform plate***
- The **olfactory nerve (CN I)** is the only cranial nerve that does not have a thalamic relay nucleus before reaching the cerebral cortex.
- It passes through the **cribriform plate** of the ethmoid bone to reach the olfactory bulbs.
*Superior orbital fissure*
- This opening transmits the **oculomotor (CN III), trochlear (CN IV), ophthalmic division of trigeminal (CN V1)**, and **abducens (CN VI)** nerves.
- These nerves all have sensory or motor components that relay through the thalamus, directly or indirectly.
*Internal auditory meatus*
- This canal transmits the **facial (CN VII)** and **vestibulocochlear (CN VIII)** nerves.
- The vestibulocochlear nerve's auditory pathway involves a thalamic relay in the **medial geniculate nucleus**.
*Foramen rotundum*
- The **maxillary division of the trigeminal nerve (CN V2)** passes through the foramen rotundum.
- Sensory information carried by CN V2 relays through the **thalamus**.
*Jugular foramen*
- This opening transmits the **glossopharyngeal (CN IX), vagus (CN X)**, and **accessory (CN XI)** nerves.
- Sensory components of these nerves, particularly taste and visceral sensation, involve thalamic nuclei.
More Cranial nerves and their pathways US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.