Musculoskeletal system overview US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Musculoskeletal system overview. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Musculoskeletal system overview US Medical PG Question 1: A scientist is studying the anatomy and function of bone growth. He is able to create a cell line of osteocytes with a mutation that prevents the osteocytes from exchanging nutrients and waste products within neighboring lamellae. This mutation most likely affected which of the following cell structures?
- A. Dynein
- B. Gap junctions (Correct Answer)
- C. Endoplasmic reticulum
- D. Plasma membrane
- E. Kinesin
Musculoskeletal system overview Explanation: ***Gap junctions***
- **Gap junctions** are specialized intercellular connections that permit direct communication and exchange of small molecules and ions between adjacent cells.
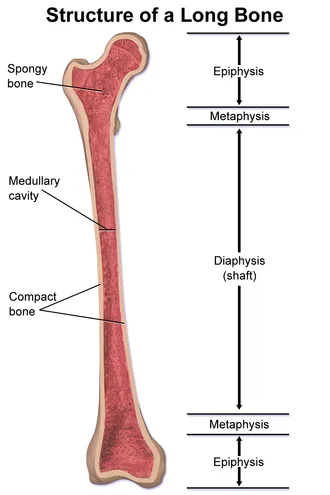
- In osteocytes, **gap junctions** located in the **canaliculi** are crucial for the exchange of nutrients, waste, and signaling molecules within and between lamellae, allowing for synchronous activity and maintaining bone health.
- These connexin-based channels physically connect the cytoplasm of neighboring osteocytes embedded in bone matrix.
*Dynein*
- **Dynein** is a motor protein involved in intracellular transport towards the minus end of **microtubules**, playing a role in moving organelles and vesicles.
- It is not directly responsible for the intercellular exchange of nutrients and waste products between cells.
*Endoplasmic reticulum*
- The **endoplasmic reticulum** is an organelle involved in protein synthesis and lipid metabolism, playing a critical role in cellular function.
- It does not directly mediate the exchange of nutrients and waste products between adjacent cells.
*Plasma membrane*
- While **gap junctions** are embedded within the **plasma membrane**, the membrane itself does not facilitate direct cytoplasmic continuity between cells.
- The question specifically refers to structures that enable direct cell-to-cell exchange; the mutation affects the gap junction channels themselves (connexins), not the general plasma membrane structure.
- Without functional gap junctions, the plasma membrane alone cannot support the intercellular communication required for osteocyte networks.
*Kinesin*
- **Kinesin** is a motor protein that moves cargo along **microtubules** towards the plus end, involved in fundamental cellular processes like cell division and organelle transport.
- It is not involved in direct intercellular communication for nutrient and waste exchange but rather internal cellular trafficking.
Musculoskeletal system overview US Medical PG Question 2: An investigator is developing a drug for muscle spasms. The drug inactivates muscular contraction by blocking the site where calcium ions bind to regulate actin-myosin interaction. Which of the following is the most likely site of action of this drug?
- A. Troponin C (Correct Answer)
- B. Myosin-binding site
- C. Acetylcholine receptor
- D. Ryanodine receptor
- E. Myosin head
Musculoskeletal system overview Explanation: ***Troponin C***
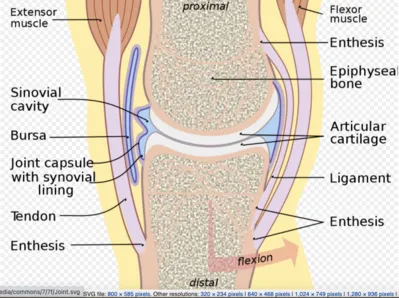
- **Calcium ions** bind to **Troponin C**, initiating a conformational change in the troponin-tropomyosin complex, which exposes the **myosin-binding sites on actin**.
- Blocking this site directly prevents the **calcium-mediated regulation** of muscle contraction, thus inactivating it.
*Myosin-binding site*
- The **myosin-binding site** is located on the **actin filament** and is where the **myosin head** attaches to form cross-bridges.
- While essential for contraction, this site doesn't directly bind calcium ions to initiate the process.
*Acetylcholine receptor*
- The **acetylcholine receptor** is located on the **neuromuscular junction** and mediates the transmission of a nerve impulse to the muscle fiber.
- Blocking this receptor would prevent muscle depolarization, but it's not the direct site where calcium ions regulate actin-myosin interaction.
*Ryanodine receptor*
- The **ryanodine receptor** is located on the **sarcoplasmic reticulum** and controls the release of calcium ions into the sarcoplasm.
- While it's involved in calcium signaling, it doesn't represent the site where calcium binds to *regulate* the actin-myosin interaction itself.
*Myosin head*
- The **myosin head** contains the **ATPase activity** and binds to actin to form cross-bridges, enabling muscle contraction.
- It does not directly bind **calcium ions** to regulate the initiation of contraction; instead, its binding to actin is regulated by the troponin-tropomyosin complex.
Musculoskeletal system overview US Medical PG Question 3: A 72-year-old woman is brought to the emergency department because of severe pain in her left hip after a fall this morning. She has smoked one pack of cigarettes daily for 45 years. Her only medication is a vitamin D supplement. Physical examination shows that her left leg is externally rotated and appears shorter than her right leg. An x-ray of the pelvis shows a fracture of the neck of the left femur. Which of the following changes in bone architecture is the most likely underlying cause of this patient's symptoms?
- A. Subperiosteal bone resorption and cystic degeneration
- B. Deposition of lamellar bone interspersed with woven bone
- C. Formation of multiple sclerotic lesions in bony cortex
- D. Loss of cortical bone mass and thinning of trabeculae (Correct Answer)
- E. Overgrowth of cortical bone and reduced marrow space
Musculoskeletal system overview Explanation: ***Loss of cortical bone mass and thinning of trabeculae***
- The patient's age (72 years), female sex, and smoking history are significant risk factors for **osteoporosis**, which leads to **reduced bone mineral density**.
- **Osteoporotic bones** are characterized by **thinning of cortical bone** and **loss of trabecular bone**, making them brittle and highly susceptible to **fragility fractures**, such as a femoral neck fracture after a fall.
*Subperiosteal bone resorption and cystic degeneration*
- This pattern of bone change is characteristic of **hyperparathyroidism**, specifically **osteitis fibrosa cystica**.
- While hyperparathyroidism can cause bone fragility, the clinical presentation (isolated fall-related fracture, no other symptoms of hyperparathyroidism) does not specifically point to this condition.
*Deposition of lamellar bone interspersed with woven bone*
- This describes bone changes seen in conditions with **disordered bone remodeling**, such as **Paget's disease of bone**.
- Paget's disease commonly presents with focal areas of enlarged, deformed, and weak bones, which would typically be reported on X-ray as thickened cortices rather than fragility fracture in this context.
*Formation of multiple sclerotic lesions in bony cortex*
- **Sclerotic lesions** indicate areas of increased bone density, which can be seen in conditions like **osteoblastic metastases** or **osteopetrosis**.
- These conditions typically increase bone mass or density, making bones harder but often more brittle, but usually not associated with the primary pathology in this scenario.
*Overgrowth of cortical bone and reduced marrow space*
- This describes changes seen in various **sclerotic bone disorders**, including **osteopetrosis** (marble bone disease) or severe forms of **sclerotic dysplasias**.
- These conditions are rare and result in abnormally dense but fragile bones, but they are not the most likely underlying cause for a hip fracture in an elderly woman with typical risk factors for osteoporosis.
Musculoskeletal system overview US Medical PG Question 4: A 66-year-old female presents to the emergency room with left hip pain after a fall. She is unable to move her hip due to pain. On exam, her left leg appears shortened and internally rotated. Hip radiographs reveal a fracture of the left femoral neck. She has a history of a distal radius fracture two years prior. Review of her medical record reveals a DEXA scan from two years ago that demonstrated a T-score of -3.0. Following acute management of her fracture, she is started on a medication that is known to induce osteoclast apoptosis. Which of the following complications is most closely associated with the medication prescribed in this case?
- A. Gingival hyperplasia
- B. Vertebral compression fracture
- C. Interstitial nephritis
- D. Osteonecrosis of the jaw (Correct Answer)
- E. Agranulocytosis
Musculoskeletal system overview Explanation: ***Osteonecrosis of the jaw***
- The patient's history of a femoral neck fracture and a **DEXA T-score of -3.0** indicates **osteoporosis**, for which a medication inducing osteoclast apoptosis (e.g., **bisphosphonates** or **denosumab**) would be prescribed.
- **Osteonecrosis of the jaw (ONJ)** is a recognized, although rare, severe complication particularly associated with bisphosphonate and denosumab use, often following dental procedures.
*Gingival hyperplasia*
- This complication is most commonly associated with **calcium channel blockers** (like nifedipine), **cyclosporine**, and **phenytoin**.
- It is not a known side effect of medications that induce osteoclast apoptosis, such as bisphosphonates or denosumab.
*Vertebral compression fracture*
- While this patient is at high risk for osteoporotic fractures, medication that *treats* osteoporosis by inducing osteoclast apoptosis **reduces** the risk of new fractures, including vertebral compression fractures.
- A new vertebral compression fracture would indicate treatment failure or an underlying progression of osteoporosis, not a direct complication of the medication if it is working effectively.
*Interstitial nephritis*
- **Interstitial nephritis** is an inflammatory kidney condition often associated with drugs like **NSAIDs**, **antibiotics (e.g., penicillins, sulfonamides)**, and **diuretics**.
- It is not a characteristic side effect of bisphosphonates or other anti-resorptive agents used for osteoporosis.
*Agranulocytosis*
- Agranulocytosis is a severe reduction in **granulocytes (a type of white blood cell)**, typically associated with drugs like **propylthiouracil**, **methimazole**, **clozapine**, and certain **NSAIDs**.
- Medications that induce osteoclast apoptosis for osteoporosis do not commonly cause agranulocytosis.
Musculoskeletal system overview US Medical PG Question 5: A 57-year-old woman presents to her primary care physician with a concern for joint pain. She states that she often feels minor joint pain and morning stiffness in both of her hands every day, particularly in the joints of her fingers. Her symptoms tend to improve as the day goes on and she states they are not impacting the quality of her life. She lives alone as her partner recently died. She smokes 1 pack of cigarettes per day and drinks 2-3 alcoholic drinks per day. Her last menses was at age 45 and she works at a library. The patient has a history of diabetes and chronic kidney disease with her last GFR at 45 mL/min. Her temperature is 97.5°F (36.4°C), blood pressure is 117/58 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical examination is within normal limits. Which of the following interventions is appropriate management of future complications in this patient?
- A. Methotrexate
- B. Ibuprofen
- C. Prednisone
- D. Alendronate (Correct Answer)
- E. Infliximab
Musculoskeletal system overview Explanation: ***Alendronate***
- This patient, a 57-year-old postmenopausal woman with **early menopause (age 45)**, **smoking**, **alcohol use**, and **chronic kidney disease**, is at **significantly increased risk for osteoporosis**. Alendronate, a **bisphosphonate**, is an appropriate intervention to prevent future osteoporotic fractures.
- While her joint pain is likely **osteoarthritis** and currently mild, the question targets **future complication management**, highlighting her significant risk factors for bone density loss.
- Her **GFR of 45 mL/min** (Stage 3a CKD) is at the lower acceptable range for bisphosphonate use; alendronate is generally avoided when GFR < 30-35 mL/min, but can be used with monitoring at GFR 45 mL/min given her high fracture risk.
*Methotrexate*
- Methotrexate is a **disease-modifying antirheumatic drug (DMARD)** typically used for inflammatory arthropathies like **rheumatoid arthritis** or **psoriatic arthritis**.
- The patient's symptoms (mild, improving with activity, no significant exam findings) are not consistent with an inflammatory arthritis requiring methotrexate, and her **chronic kidney disease** makes its use more complex due to renal elimination and toxicity risk.
*Ibuprofen*
- Ibuprofen, a **nonsteroidal anti-inflammatory drug (NSAID)**, could be used for symptomatic relief of her mild osteoarthritis.
- However, the question asks about **"future complications"** and her history of **chronic kidney disease** makes long-term NSAID use potentially harmful due to the risk of worsening renal function and increased cardiovascular risk.
*Prednisone*
- Prednisone is a powerful **corticosteroid** used for acute flares of inflammatory conditions or severe autoimmune diseases.
- Her current joint pain is mild and not indicative of an inflammatory process requiring prednisone; furthermore, long-term corticosteroid use is a significant **risk factor for osteoporosis**, which would worsen her already elevated fracture risk.
*Infliximab*
- Infliximab is a **biologic agent** (TNF-alpha inhibitor) used for severe, refractory inflammatory conditions such as **rheumatoid arthritis**, **ankylosing spondylitis**, or **inflammatory bowel disease**.
- Her symptoms are mild and do not suggest a severe inflammatory arthropathy that would warrant the use of a high-risk biologic medication, which also carries risks like increased infection susceptibility and significant cost.
Musculoskeletal system overview US Medical PG Question 6: A 59-year-old woman comes to the physician because of a 1-year history of pain and stiffness in her fingers and knees. The stiffness lasts for about 10 minutes after she wakes up in the morning. She also reports that her knee pain is worse in the evening. She drinks one glass of wine daily. Her only medication is acetaminophen. She is 175 cm (5 ft 9 in) tall and weighs 102 kg (225 lb); BMI is 33 kg/m2. Physical examination shows firm nodules on the distal interphalangeal joints of the index, ring, and little fingers of both hands. Which of the following is the most likely diagnosis?
- A. Septic arthritis
- B. Pseudogout
- C. Gout
- D. Rheumatoid arthritis
- E. Osteoarthritis (Correct Answer)
Musculoskeletal system overview Explanation: ***Osteoarthritis***
* The patient's age (59 years), obesity (BMI 33 kg/m2), short duration of morning stiffness (10 minutes), evening worsening of knee pain, and the presence of **firm nodules on the distal interphalangeal joints** (Heberden's nodes) are classic signs of **osteoarthritis**.
* This condition is a common **degenerative joint disease** associated with wear and tear, often affecting weight-bearing joints and small joints of the hands.
*Septic arthritis*
* **Septic arthritis** typically presents with an acutely painful, hot, and swollen joint, often with systemic symptoms like fever and chills, which are absent here.
* The chronic, progressive nature of the patient's symptoms and the presence of bony nodules point away from an infectious cause.
*Pseudogout*
* **Pseudogout**, or calcium pyrophosphate deposition disease, involves the deposition of calcium pyrophosphate crystals, leading to episodes of acute, painful arthritis, often in larger joints like the knee.
* While it can affect the knee, the insidious onset, chronic pain, and specific hand nodules seen in this case are not typical features of pseudogout.
*Gout*
* **Gout** is characterized by sudden, severe attacks of pain, redness, and swelling, often affecting a single joint (commonly the great toe) due to **uric acid crystal deposition**.
* The patient's chronic pain pattern, multiple joint involvement (fingers and knees), and the description of firm nodules (not tophi) make gout less likely.
*Rheumatoid arthritis*
* **Rheumatoid arthritis** typically presents with morning stiffness lasting longer than 30 minutes, symmetrical polyarthritis, and often affects the **proximal interphalangeal (PIP)** and **metacarpophalangeal (MCP) joints** of the hands, sparing the DIP joints.
* The patient's short morning stiffness, DIP joint involvement, and the absence of systemic inflammatory signs argue against rheumatoid arthritis.
Musculoskeletal system overview US Medical PG Question 7: An investigator is studying the crossbridge cycle of muscle contraction. Tissue from the biceps brachii muscle is obtained at the autopsy of an 87-year-old man. Investigation of the muscle tissue shows myosin heads attached to actin filaments. Binding of myosin heads to which of the following elements would most likely cause detachment of myosin from actin filaments?
- A. ATP (Correct Answer)
- B. Troponin C
- C. Tropomyosin
- D. ADP
- E. cGMP
Musculoskeletal system overview Explanation: ***ATP***
- The binding of **ATP** to the **myosin head** causes a conformational change that reduces its affinity for actin, leading to detachment.
- This step is crucial for the muscle to relax and for the subsequent power stroke to occur.
*Troponin C*
- **Troponin C** is a regulatory protein that binds calcium, which then causes a conformational change in the troponin-tropomyosin complex, revealing the **actin binding sites** for myosin.
- It does not directly cause myosin detachment; instead, it facilitates the binding of myosin to actin.
*Tropomyosin*
- **Tropomyosin** is a long, fibrous protein that covers the **myosin-binding sites** on actin in a relaxed muscle, preventing cross-bridge formation.
- Its movement, regulated by troponin, allows myosin to bind, but it does not directly cause detachment.
*ADP*
- **ADP** is released from the myosin head during the power stroke, but its binding does not cause detachment; rather, it is present during the strongly bound state before **ATP** binds.
- The presence of **ADP** and inorganic phosphate (Pi) often promotes the strong binding of myosin to actin.
*cGMP*
- **cGMP** (cyclic guanosine monophosphate) is a second messenger involved in various cellular processes, including smooth muscle relaxation, but it is not directly involved in the cross-bridge cycle and detachment of **myosin from actin** in skeletal muscle.
- Its primary role in muscle physiology is often linked to nitric oxide signaling and vasodilation.
Musculoskeletal system overview US Medical PG Question 8: Collagen is a very critical structural protein in many of our connective tissues. Defects in collagen produce diseases such as Ehlers-Danlos syndrome, where there is a defective lysyl hydroxylase gene, or osteogenesis imperfecta, where there is a defect in the production of type I collagen. Which of the following represents the basic repeating tripeptide of collagen?
- A. Gly-X-Y (Correct Answer)
- B. Asp-X-Y
- C. Met-X-Y
- D. Ser-X-Y
- E. Glu-X-Y
Musculoskeletal system overview Explanation: ***Gly-X-Y***
- The **basic repeating tripeptide unit of collagen** is **Glycine-X-Y**, where X and Y are often **proline** and **hydroxyproline**, respectively.
- **Glycine** is essential at every third position because its small side chain allows for the tight packing of the **collagen triple helix**.
*Asp-X-Y*
- **Aspartate (Asp)** is an **acidic amino acid** and is not typically found at the first position of the repeating tripeptide unit of collagen.
- Its bulky side chain would hinder the tight coiling of the **collagen helix**.
*Met-X-Y*
- **Methionine (Met)** is a **hydrophobic amino acid** and, while important in other proteins, it does not occupy the critical first position in the repeating collagen tripeptide.
- The unique structural requirements of collagen favor **glycine** at this position for optimal packing.
*Ser-X-Y*
- **Serine (Ser)** is a **polar, uncharged amino acid** and, like aspartate and methionine, is not the primary amino acid found at the first position of the repeating collagen tripeptide.
- The small size of **glycine** is crucial for collagen's characteristic triple helix.
*Glu-X-Y*
- **Glutamate (Glu)** is another **acidic amino acid** that is not typically found at the first position of the repeating tripeptide in collagen.
- Large or charged amino acids at this position would destabilize the **collagen secondary structure**.
Musculoskeletal system overview US Medical PG Question 9: In large neurons the nucleus can be found a large distance away from the terminal end of its axon. The body has a complex system of intracellular transporters that are able to carry essential proteins from the nucleus to the distal edge of the cell and back. Which of the following proteins are essential for this function?
- A. Kinesin, Troponin
- B. Myosin, Kinesin
- C. Actin, Dynein
- D. Dynein, Kinesin (Correct Answer)
- E. Glucose, Actin
Musculoskeletal system overview Explanation: ***Dynein, Kinesin***
- **Kinesin** is primarily responsible for **anterograde transport** (from the cell body to the axon terminal) along microtubules, carrying vesicles and organelles.
- **Dynein** handles **retrograde transport** (from the axon terminal back to the cell body), essential for recycling components and signaling.
*Kinesin, Troponin*
- While **Kinesin** is involved in axonal transport, **Troponin** is a protein found in muscle tissue that regulates muscle contraction, not intracellular transport in neurons.
- Troponin binds **calcium ions** and influences the interaction between actin and myosin.
*Myosin, Kinesin*
- **Kinesin** is involved in microtubule-based transport, but **Myosin** is primarily associated with **actin filaments** for muscle contraction and intracellular movement, not long-distance axonal transport.
- Myosin functions as a **motor protein** that converts chemical energy in ATP into mechanical force.
*Actin, Dynein*
- **Dynein** is crucial for retrograde axonal transport, but **Actin** is a structural protein forming microfilaments that are involved in cell shape, motility, and some short-distance transport, not the major long-distance axonal transport mechanism.
- Actin filaments serve as tracks for **myosin motors**, primarily in the cell cortex.
*Glucose, Actin*
- **Glucose** is a sugar molecule, the primary energy source for cells, and not a transport protein.
- **Actin** forms microfilaments for cell structure and short-range movement, not long-distance axonal transport as described.
Musculoskeletal system overview US Medical PG Question 10: An 11-year-old girl presents to her primary care physician because she has been having difficulty hearing her teachers at school. She says that the difficulty hearing started about a year ago, and it has slowly been getting worse. Her past medical history is significant for multiple fractures in both her upper and lower extremities. She also recently had a growth spurt and says that her friends say she is tall and lanky. A mutation in which of the following genes is most likely associated with this patient's condition?
- A. Type 4 collagen
- B. Type 3 collagen
- C. Fibrillin
- D. Type 1 collagen (Correct Answer)
- E. Fibroblast growth factor receptor
Musculoskeletal system overview Explanation: ***Type 1 collagen***
- This patient's symptoms—hearing difficulty, multiple fractures, and tall/lanky stature—are classic signs of **osteogenesis imperfecta (OI)**, a genetic disorder caused by mutations in genes encoding **Type I collagen**.
- **Type I collagen** is a major component of bone, so defects lead to fragile bones and susceptibility to fractures, and it also plays a role in the structure of the ear, affecting hearing.
*Type 4 collagen*
- Mutations in **Type 4 collagen** are primarily associated with **Alport syndrome**, which classically presents with **hematuria**, progressive renal failure, and hearing loss.
- While hearing loss is present, the patient's other key symptoms of **multiple fractures** and **tall, lanky stature** are not characteristic of Alport syndrome.
*Type 3 collagen*
- Defects in **Type 3 collagen** are linked to **Ehlers-Danlos syndrome, vascular type**, which is characterized by fragile blood vessels, organs, and skin, leading to easy bruising, arterial rupture, and bowel perforation.
- While Type 3 collagen is found in connective tissues, its primary clinical manifestations do not align with the patient's presentation of recurrent fractures and hearing loss.
*Fibrillin*
- Mutations in **fibrillin-1** are responsible for **Marfan syndrome**, which presents with tall stature, long limbs (**arachnodactyly**), and cardiovascular issues like aortic dilation.
- While tall stature is observed, the patient's primary complaints of **recurrent fractures** and hearing loss are not typical features of Marfan syndrome.
*Fibroblast growth factor receptor*
- Mutations in **fibroblast growth factor receptor 3 (FGFR3)** are most commonly associated with **achondroplasia**, a form of dwarfism characterized by short stature, short limbs, and a large head.
- This is inconsistent with the patient's **tall and lanky stature** and does not account for the recurrent fractures or hearing difficulties.
More Musculoskeletal system overview US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.