Integumentary system US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Integumentary system. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Integumentary system US Medical PG Question 1: A 21-year-old man comes to the physician because of painful, firm, dark bumps on his neck and jawline. He has no history of serious illness and takes no medications. His brother had a similar rash. A photograph of the rash is shown. Which of the following is the most likely underlying mechanism of this patient's condition?
- A. Trichophyton infection of the superficial hair follicle
- B. Interfollicular penetration of the skin by distal end of hair (Correct Answer)
- C. Bacterial infection of the superficial or deep hair follicle
- D. Follicular obstruction with subsequent duct rupture
- E. Cutibacterium acnes colonization of the pilosebaceous unit
Integumentary system Explanation: ***Interfollicular penetration of the skin by distal end of hair***
- The description of painful, firm, dark bumps on the neck and jawline, particularly in a young man, is classic for **pseudofolliculitis barbae**, often caused by the distal end of hair penetrating the skin after shaving.
- This condition is common in individuals with **curly hair** where shaved hairs re-enter the skin, causing a foreign body inflammatory reaction.
*Trichophyton infection of the superficial hair follicle*
- This would typically present as **tinea barbae** or **tinea capitis**, characterized by scaling, erythema, and pustules, often with hair breakage, not firm dark bumps from embedded hairs.
- While fungal infections can cause folliculitis, the clinical presentation and family history of improvement with erythromycin (an antibacterial) make this less likely.
*Bacterial infection of the superficial or deep hair follicle*
- **Bacterial folliculitis** (e.g., *Staphylococcus aureus*) usually presents as pustules, papules, and sometimes carbuncles, which are typically red, inflamed, and often pus-filled.
- The family history of improvement with erythromycin might suggest a bacterial component, but the primary mechanism described (firm, dark bumps) points away from primary bacterial infection and more towards a physical cause like pseudofolliculitis barbae, which can then become secondarily infected.
*Follicular obstruction with subsequent duct rupture*
- This mechanism is characteristic of **acne vulgaris** (comedones, papules, pustules, cysts) or **hidradenitis suppurativa** (deep-seated nodules, abscesses affecting intertriginous areas), which are different in appearance and location from the described lesions.
- While related to follicular issues, the specific description of "dark bumps" and the context of shaving make embedded hairs more likely than a primary obstruction and rupture.
*Cutibacterium acnes colonization of the pilosebaceous unit*
- This is the primary bacterial contributor to **acne vulgaris**, leading to comedones, inflamed papules, and pustules, often affecting the face, chest, and back.
- Although the jawline is a common area for acne, the "firm, dark bumps" are less typical of classic acne and more consistent with ingrown hairs.
Integumentary system US Medical PG Question 2: A 41-year-old male who takes NSAIDs regularly for his chronic back pain develops severe abdominal pain worse with eating. Upper endoscopy is performed and the medical student asks the supervising physician how the histological differentiation between a gastric ulcer and erosion is made. Which of the following layers of the gastric mucosa MUST be breached for a lesion to be considered an ulcer?
- A. Epithelium, lamina propria
- B. Epithelium
- C. Epithelium, lamina propria, muscularis mucosa (Correct Answer)
- D. Epithelium, lamina propria, muscularis mucosa, submucosa, and adventitia
- E. Epithelium, lamina propria, muscularis mucosa, and submucosa
Integumentary system Explanation: ***Epithelium, lamina propria, muscularis mucosa***
- A **gastric ulcer** by definition involves a breach of the **entire mucosal thickness**, meaning the lesion extends through the muscularis mucosa.
- This deep penetration distinguishes an ulcer from an erosion, which is a more superficial lesion confined to the epithelium and lamina propria.
*Epithelium, lamina propria*
- This describes an **erosion**, a superficial lesion of the gastric mucosa that does not penetrate the **muscularis mucosa**.
- While erosions can cause symptoms, they are generally less severe and have a lower risk of complications like perforation compared to ulcers.
*Epithelium*
- A lesion confined solely to the **epithelium** would be considered a very superficial mucosal injury, often referred to as an **erosion** or sometimes a **superficial abrasion**.
- This degree of injury does not meet the criteria for either an erosion or an ulcer in a histological context.
*Epithelium, lamina propria, muscularis mucosa, submucosa, and adventitia*
- Penetration through the **submucosa** means the ulcer has become a **deep ulcer** or potentially a **perforating ulcer**, if it breaches the entire wall to the adventitia (serosa in the GI tract).
- While an ulcer *can* extend to these layers, only reaching the muscularis mucosa is the *minimum* requirement to be classified as an ulcer.
*Epithelium, lamina propria, muscularis mucosa, and submucosa*
- An ulcer that extends into the **submucosa** is indeed a true ulcer and a more severe one, but the defining histological feature separating an erosion from an ulcer is the breach of the **muscularis mucosa**.
- Therefore, reaching the submucosa is beyond the *minimum* requirement for an ulcer classification.
Integumentary system US Medical PG Question 3: A 46-year-old woman presents to your office with oral lesions as shown in Image A. On examination, you find that her back has flaccid bullae that spread when you apply lateral pressure with your fingertips. This patient most likely has autoantibodies directed against which of the following?
- A. Type VII collagen
- B. Lamina densa
- C. Hemidesmosomes
- D. Lamina lucida
- E. Desmosomes (Correct Answer)
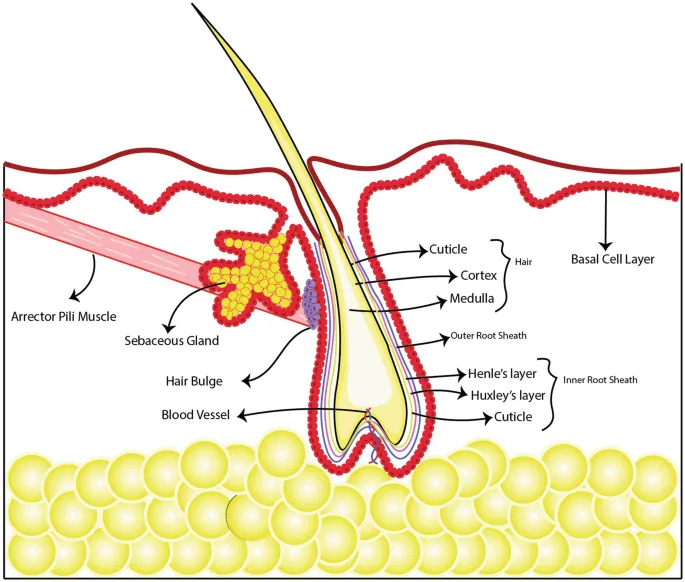
Integumentary system Explanation: ***Desmosomes***
- The presence of **flaccid bullae**, a positive **Nikolsky sign (spread with lateral pressure)**, and **oral lesions** are characteristic features of **pemphigus vulgaris**.
- **Pemphigus vulgaris** is an autoimmune disease where autoantibodies target **desmogleins 1 and 3**, which are components of desmosomes, leading to the loss of cell-to-cell adhesion within the epidermis.
*Type VII collagen*
- Autoantibodies against **type VII collagen** are associated with **epidermolysis bullosa acquisita**, which typically presents with **tense bullae** and scarring, unlike the flaccid bullae seen here.
- This condition involves the **dermal-epidermal junction**, leading to subepidermal blistering.
*Lamina densa*
- The **lamina densa** is a component of the **basement membrane zone**, and antibodies targeting it are characteristic of certain types of **bullous pemphigoid** or some forms of **epidermolysis bullosa**.
- However, typical bullous pemphigoid presents with **tense bullae** and, unlike pemphigus, usually spares the oral mucosa.
*Hemidesmosomes*
- Autoantibodies targeting **hemidesmosomes** (specifically **BP180 and BP230 antigens**) are typical of **bullous pemphigoid**, which is characterized by **tense bullae** and often pruritus.
- These antibodies lead to blistering at the **dermal-epidermal junction**, but the bullae are typically firm and do not show a positive Nikolsky sign.
*Lamina lucida*
- The **lamina lucida** is another component of the **basement membrane zone** where blistering occurs in some autoimmune bullous diseases, specifically **bullous pemphigoid**.
- However, the clinical presentation of flaccid bullae with oral involvement and a positive Nikolsky sign strongly points away from bullous pemphigoid and towards pemphigus vulgaris, which primarily involves intercellular adhesion.
Integumentary system US Medical PG Question 4: A 15-year-old boy comes to the physician because of skin changes on his face, chest, and back over the past year. Treatment with over-the-counter benzoyl peroxide has been ineffective. Physical examination shows numerous open comedones, inflammatory papules, and pustules on his face, chest, and back. Which of the following is the most likely underlying mechanism of this patient’s skin condition?
- A. Hyperkeratinization of hair follicles (Correct Answer)
- B. Type IV hypersensitivity reaction
- C. Formation of superficial epidermal inclusion cyst
- D. Excess androgen production
- E. Hyperplasia of pilosebaceous glands
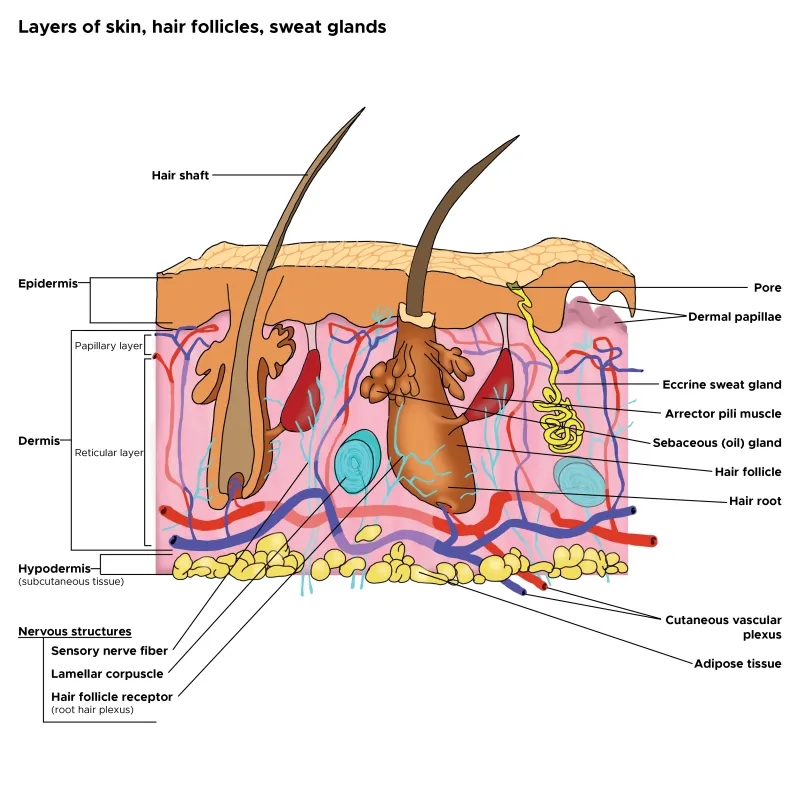
Integumentary system Explanation: **Hyperkeratinization of hair follicles**
- The primary event in the pathogenesis of **acne vulgaris** is the **shedding of hyperkeratinized corneocytes** into the lumen of the hair follicle, which then combines with sebum to form a microcomedone.
- This process leads to the **obstruction of the pilosebaceous unit**, creating an anaerobic environment conducive to the proliferation of *Cutibacterium acnes* and the development of inflammatory lesions like papules and pustules.
*Type IV hypersensitivity reaction*
- This mechanism involves **T-cell mediated delayed hypersensitivity**, leading to conditions like **allergic contact dermatitis** or **tuberculosis**.
- Acne vulgaris is not primarily an allergic reaction mediated by T cells; its pathogenesis involves follicular obstruction, sebum production, bacterial colonization, and inflammation.
*Formation of superficial epidermal inclusion cyst*
- Epidermal inclusion cysts (also known as epidermoid cysts) are typically solitary, slow-growing cysts that result from the **implantation of epidermal cells into the dermis**, often due to trauma or blocked hair follicles, but they are not the underlying mechanism for widespread acne.
- While some severe acne lesions can rarely lead to cyst formation, the presence of numerous **comedones, papules, and pustules** indicates typical acne vulgaris, not primarily cyst formation.
*Excess androgen production*
- While **androgens stimulate sebum production**, which is a contributing factor to acne, they are not the initiating mechanism for the follicular obstruction itself.
- Most adolescents with acne have **normal androgen levels**; the skin's sebaceous glands are simply more sensitive to circulating androgens, leading to increased sebum.
*Hyperplasia of pilosebaceous glands*
- **Sebaceous gland hyperplasia** refers to an increase in the number and size of sebaceous glands, leading to an overproduction of sebum, which contributes to acne.
- However, the fundamental initiating event for comedone formation in acne is the **follicular hyperkeratinization and obstruction**, rather than simply the glands being hyperplastic.
Integumentary system US Medical PG Question 5: A 52-year-old Caucasian man presents to the clinic for evaluation of a mole on his back that he finds concerning. He states that his wife noticed the lesion and believes that it has been getting larger. On inspection, the lesion is 10 mm in diameter with irregular borders. A biopsy is performed. Pathology reveals abnormal melanocytes forming nests at the dermo-epidermal junction and discohesive cell growth into the epidermis. What is the most likely diagnosis?
- A. Desmoplastic melanoma
- B. Lentigo maligna melanoma
- C. Superficial spreading melanoma (Correct Answer)
- D. Nodular melanoma
- E. Acral lentiginous melanoma
Integumentary system Explanation: ***Superficial spreading melanoma***
- This is the **most common type of melanoma**, accounting for 70% of cases, and typically presents with a **radial growth phase** showing irregular borders and enlarging size.
- Histopathology revealing **nests of abnormal melanocytes at the dermo-epidermal junction** and **discohesive cell growth into the epidermis** (pagetoid spread) is characteristic of superficial spreading melanoma.
*Desmoplastic melanoma*
- Characterized by **fibrous stroma** and often **neural invasion**, with a less pigmented appearance, which is not described.
- Typically presents as a firm, often amelanotic nodule, and can be more aggressive.
*Lentigo maligna melanoma*
- Primarily found in **chronically sun-damaged areas** of the elderly, often on the face, and begins as a flat, tan-brown macule that slowly enlarges.
- Histologically, it shows **atypical melanocytes along the basal layer** of a thinned epidermis, not necessarily forming nests or extensive discohesive growth into the epidermis early on.
*Nodular melanoma*
- This type of melanoma has a **vertical growth phase from the outset**, appearing as a rapidly growing, dark, elevated lesion without a significant preceding radial growth phase.
- Histologically, it involves a substantial dermal component with **minimal or absent intraepidermal radial growth**.
*Acral lentiginous melanoma*
- Occurs on the **palms, soles, or under the nails (subungual)**, and is less associated with sun exposure, often presenting as a dark, spreading lesion.
- Its histological features involve **lentiginous proliferation of atypical melanocytes** along the dermo-epidermal junction with spread into the rete ridges in an acral distribution.
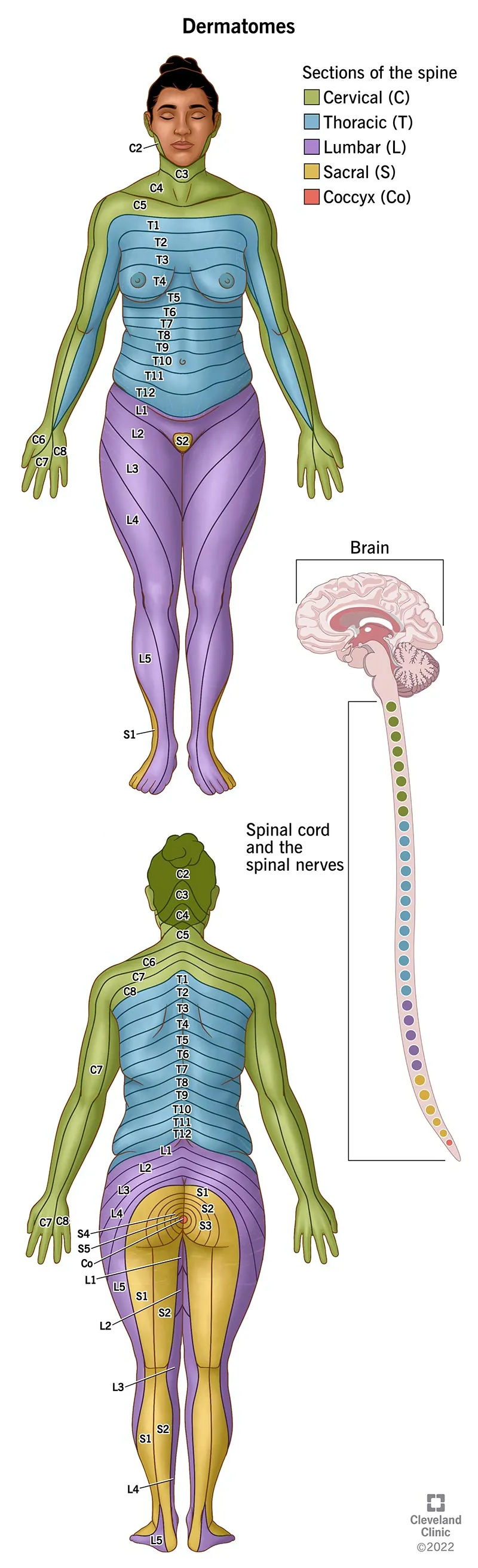
Integumentary system US Medical PG Question 6: A 9-year-old boy with a history of acute lymphoblastic leukemia is brought to the clinic by his mother because of pruritic vesicles that appeared on the left side of his torso 12 hours ago. One day earlier, before the appearance of the vesicles, the patient's mother notes that he had been complaining of a burning sensation in that area. The boy has been receiving chemotherapy consisting of methotrexate, cytarabine, and cyclophosphamide for 1 month. He received the last treatment 2 days ago. He has no other past medical history. The patient is afebrile and vital signs are within normal limits. Upon physical examination, painful vesicles are localized to the left C7 skin dermatome (see image). Which of the following is the most likely etiology of the skin lesions in this patient?
- A. Viral infection of the skin
- B. Bacterial infection of the skin
- C. Reactivation of the varicella zoster virus (VZV) due to congenital immunodeficiency
- D. Chickenpox
- E. Reactivation of VZV due to immunodeficiency caused by chemotherapy (Correct Answer)
Integumentary system Explanation: ***Reactivation of VZV due to immunodeficiency caused by chemotherapy***
- The patient's history of **acute lymphoblastic leukemia** and recent **chemotherapy** (methotrexate, cytarabine, cyclophosphamide) indicates an **immunocompromised state**, which is a significant predisposing factor for VZV reactivation (shingles).
- The clinical presentation of **pruritic vesicles** preceded by a **burning sensation**, localized to a **single dermatome (C7)**, is highly characteristic of **herpes zoster** (shingles), which is caused by the reactivation of VZV.
*Viral infection of the skin*
- While shingles is a viral infection, this option is too broad and does not specify the **underlying cause** or the **specific virus**, which is crucial for a complete diagnosis in this clinical context.
- It fails to address the unique features of **dermatomal distribution** and the patient's **immunocompromised status**.
*Bacterial infection of the skin*
- **Bacterial skin infections** (e.g., impetigo, folliculitis, cellulitis) typically present with different features like **pustules**, **crusting**, **erythema**, and often spread beyond a single dermatome.
- The initial **burning sensation** and the characteristic **vesicular rash** in a dermatomal pattern are not typical of common bacterial skin infections.
*Reactivation of the varicella zoster virus (VZV) due to congenital immunodeficiency*
- There is no mention of a **congenital immunodeficiency** in the patient's history; his immunodeficiency is clearly attributed to **chemotherapy** for acute lymphoblastic leukemia.
- While VZV reactivation is correct, attributing it to a congenital cause when an obvious iatrogenic cause exists is incorrect.
*Chickenpox*
- **Chickenpox** (primary VZV infection) typically presents as a generalized, widespread rash with vesicles in different stages of healing.
- This patient's rash is **localized to a single dermatome** and is preceded by a burning sensation, which is classic for shingles (reactivated VZV), not primary chickenpox.
Integumentary system US Medical PG Question 7: A 35-year-old man is brought to the emergency department from a kitchen fire. The patient was cooking when boiling oil splashed on his exposed skin. His temperature is 99.7°F (37.6°C), blood pressure is 127/82 mmHg, pulse is 120/min, respirations are 12/min, and oxygen saturation is 98% on room air. He has dry, nontender, and circumferential burns over his arms bilaterally, burns over the anterior portion of his chest and abdomen, and tender spot burns with blisters on his shins. A 1L bolus of normal saline is administered and the patient is given morphine and his pulse is subsequently 80/min. A Foley catheter is placed which drains 10 mL of urine. What is the best next step in management?
- A. Additional fluids and escharotomy (Correct Answer)
- B. Escharotomy
- C. Continuous observation
- D. Moist dressings and discharge
- E. Additional fluids and admission to the ICU
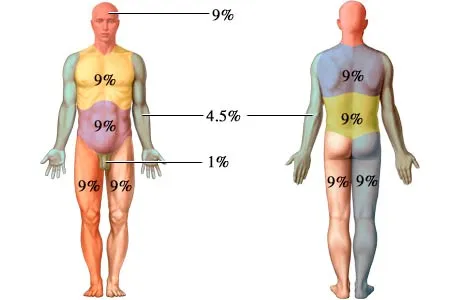
Integumentary system Explanation: ***Additional fluids and escharotomy***
- The patient has **circumferential full-thickness burns** on both arms (dry, nontender), which require **escharotomy** to prevent compartment syndrome and vascular compromise to the limbs.
- The **oliguria** (10 mL urine output) despite a 1L fluid bolus indicates **inadequate fluid resuscitation** from burn shock. With approximately 40% TBSA burns, the patient requires aggressive fluid resuscitation per the Parkland formula (4 mL/kg/% TBSA), which would be approximately 11 liters in the first 24 hours. Adequate resuscitation targets urine output of 0.5-1 mL/kg/hr (35-70 mL/hr for this patient).
- Both interventions are immediately necessary: fluids for burn shock and escharotomy for circumferential burns.
*Escharotomy*
- While **escharotomy** is essential for the circumferential full-thickness burns to prevent compartment syndrome, it alone will not address the **severe fluid deficit** causing oliguria and hypoperfusion.
- The low urine output reflects systemic hypovolemia from burn shock, not just local compartment issues, requiring aggressive fluid resuscitation.
*Continuous observation*
- **Continuous observation** is inappropriate given the patient's critical findings: circumferential full-thickness burns requiring urgent escharotomy and oliguria indicating inadequate resuscitation.
- Delaying escharotomy can lead to irreversible ischemic damage to the limbs, and inadequate fluid resuscitation can progress to multiorgan failure.
*Moist dressings and discharge*
- This option is completely inappropriate for a patient with **extensive deep burns** (approximately 40% TBSA) including full-thickness injuries requiring hospitalization and specialized burn care.
- Discharge would lead to severe complications including infection, inadequate fluid resuscitation, compartment syndrome, and potential limb loss.
*Additional fluids and admission to the ICU*
- While ICU admission and additional fluids are necessary components of care, this option is **incomplete** because it omits **escharotomy**, which is urgently needed for the circumferential full-thickness burns.
- Escharotomy is a time-sensitive procedure that must be performed promptly to prevent ischemic injury to the limbs from vascular compromise.
Integumentary system US Medical PG Question 8: A 52-year-old woman sees you in your office with a complaint of new-onset headaches over the past few weeks. On exam, you find a 2 x 2 cm dark, irregularly shaped, pigmented lesion on her back. She is concerned because her father recently passed away from skin cancer. What tissue type most directly gives rise to the lesion this patient is experiencing?
- A. Neural crest cells (Correct Answer)
- B. Endoderm
- C. Mesoderm
- D. Ectoderm
- E. Neuroectoderm
Integumentary system Explanation: ***Neural crest cells***
- The suspected lesion, given its description and the patient's family history of skin cancer, is likely a **melanoma**.
- Melanoma originates from **melanocytes**, which are derived from **neural crest cells** during embryonic development.
*Endoderm*
- The endoderm gives rise to the **lining of the gastrointestinal and respiratory tracts**, as well as organs such as the liver and pancreas.
- It is not involved in the formation of melanocytes or skin lesions like melanoma.
*Mesoderm*
- The mesoderm forms tissues such as **muscle, bone, cartilage, connective tissue**, and the circulatory system.
- It does not directly give rise to melanocytes, which are the cells of origin for melanoma.
*Ectoderm*
- The ectoderm gives rise to the **epidermis, nervous system**, and sensory organs.
- While melanocytes are found in the epidermis, they are specifically derived from the **neural crest (a sub-population of ectoderm)**, not the general ectoderm.
*Neuroectoderm*
- Neuroectoderm specifically refers to the ectoderm that develops into the **nervous system**.
- While neural crest cells originate from the neuroectoderm, "neural crest cells" is a more precise answer for the origin of melanocytes.
Integumentary system US Medical PG Question 9: An otherwise healthy 17-year-old girl comes to the physician because of multiple patches on her face, hands, abdomen, and feet that are lighter than the rest of her skin. The patches began to appear 3 years ago and have been gradually increasing in size since. There is no associated itchiness, redness, numbness, or pain. She emigrated from India 2 years ago. An image of the lesions on her face is shown. Which of the following is most likely involved in the pathogenesis of this patient's skin findings?
- A. Defective tuberin protein
- B. Infection with Malassezia globosa
- C. Infection with Mycobacterium leprae
- D. Absence of tyrosinase activity
- E. Autoimmune destruction of melanocytes (Correct Answer)
Integumentary system Explanation: ***Autoimmune destruction of melanocytes***
- The presentation of **multiple, gradually enlarging hypopigmented patches** on various body areas, particularly in an otherwise healthy individual, is highly suggestive of **vitiligo**.
- **Vitiligo** is an acquired depigmentation disorder resulting from the **autoimmune destruction of melanocytes**, leading to a complete absence of melanin in the affected areas.
*Defective tuberin protein*
- **Defective tuberin protein** is associated with **tuberous sclerosis**, a neurocutaneous syndrome.
- Skin manifestations of tuberous sclerosis include **ash-leaf spots** (hypopigmented macules), **facial angiofibromas**, and **Shagreen patches**, which are typically present from birth or early childhood and often associated with neurological symptoms.
*Infection with Malassezia globosa*
- **Malassezia globosa** causes **tinea versicolor** (pityriasis versicolor), a superficial fungal infection characterized by **hypopigmented or hyperpigmented patches** with fine scale.
- These lesions often occur on the trunk and proximal extremities and typically **fluoresce yellow-green** under Wood's lamp, which is not mentioned here.
*Infection with Mycobacterium leprae*
- **Mycobacterium leprae** causes **leprosy**, which can present with **hypopigmented macules** that are typically **anesthetic** (loss of sensation).
- While the patient is from an endemic area (India), the lack of **anesthesia**, associated neuropathic symptoms, or active inflammation makes leprosy less likely.
*Absence of tyrosinase activity*
- **Absence of tyrosinase activity** is characteristic of **oculocutaneous albinism**, a *genetic* condition leading to a *generalized lack of pigmentation* in the skin, hair, and eyes.
- This patient presents with *localized patches* of depigmentation that appeared at 14 years old, which is inconsistent with congenital albinism.
Integumentary system US Medical PG Question 10: A 65-year-old male is evaluated in clinic approximately six months after resolution of a herpes zoster outbreak on his left flank. He states that despite the lesions having resolved, he is still experiencing constant burning and hypersensitivity to touch in the distribution of the old rash. You explain to him that this complication can occur in 20-30% of patients after having herpes zoster. You also explain that vaccination with the shingles vaccine in individuals 60-70 years of age can reduce the incidence of this complication. What is the complication?
- A. Ramsay-Hunt syndrome
- B. Post-herpetic neuralgia (Correct Answer)
- C. Recurrent zoster
- D. Secondary bacterial infection
- E. Acute herpetic neuralgia
Integumentary system Explanation: ***Post-herpetic neuralgia***
- This condition is characterized by **persistent pain** (burning, throbbing, or shooting) and **allodynia** (hypersensitivity to light touch) in the dermatomal distribution of a resolved herpes zoster rash.
- It occurs due to **nerve damage** caused by the varicella-zoster virus and is more common in older adults, with symptoms persisting for months to years, consistent with the patient's presentation and the statistic of 20-30% incidence.
*Ramsay-Hunt syndrome*
- This syndrome is a complication of **herpes zoster oticus**, affecting the facial nerve (cranial nerve VII).
- It presents with **facial paralysis**, rash in the ear or mouth, and sometimes hearing loss or vertigo, which is not described in this patient's symptoms.
*Recurrent zoster*
- While possible, **recurrent zoster** would involve the reappearance of the vesicular rash and associated acute pain, not persistent burning and hypersensitivity after the original rash has resolved.
- The patient describes a "resolved" outbreak, indicating the skin lesions are gone, and only the nerve pain remains.
*Secondary bacterial infection*
- A **secondary bacterial infection** would manifest as redness, warmth, swelling, pus, and increased acute pain at the site of the skin lesions.
- The patient's symptoms of chronic burning and hypersensitivity in the absence of active lesions are not consistent with a bacterial infection.
*Acute herpetic neuralgia*
- **Acute herpetic neuralgia** refers to the pain experienced *during* the active herpes zoster outbreak and up to 30 days after the rash onset.
- In this case, the pain persists six months *after resolution* of the rash, indicating a chronic condition rather than acute pain.
More Integumentary system US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.