Congenital anomalies of GI tract US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Congenital anomalies of GI tract. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Congenital anomalies of GI tract US Medical PG Question 1: A 28-year-old primigravid woman is brought to the emergency department after complaining of severe abdominal pain for 3 hours. She has had no prenatal care. There is no leakage of amniotic fluid. Since arrival, she has had 5 contractions in 10 minutes, each lasting 70 to 90 seconds. Pelvic examination shows a closed cervix and a uterus consistent in size with a 38-week gestation. Ultrasound shows a single live intrauterine fetus in a breech presentation consistent with a gestational age of approximately 37 weeks. The amniotic fluid index is 26 and the fetal heart rate is 92/min. The placenta is not detached. She is scheduled for an emergency lower segment transverse cesarean section because of a nonreassuring fetal heart rate. The infant is delivered and APGAR score is noted to be 8 at 1 minute. The doctor soon notices cyanosis of the lips and oral mucosa, which does not resolve when the infant cries. The infant is foaming at the mouth and drooling. He also has an intractable cough. Which of the following is the most likely diagnosis?
- A. Pulmonary hypoplasia
- B. Defective swallowing reflex
- C. Esophageal stricture
- D. Achalasia
- E. Esophageal atresia (Correct Answer)
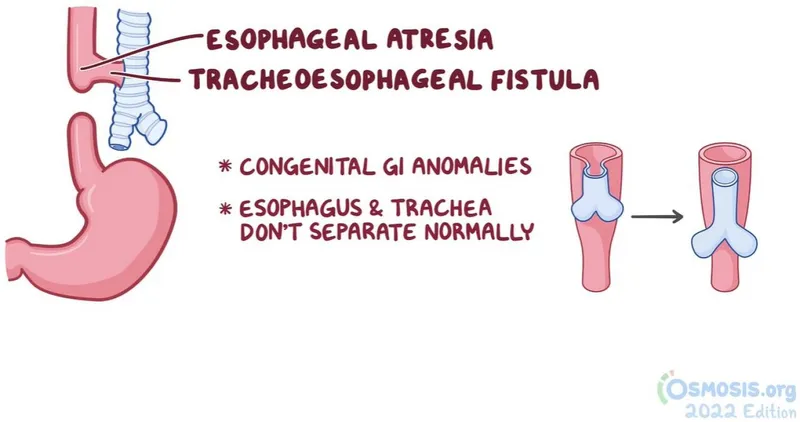
Congenital anomalies of GI tract Explanation: ***Esophageal atresia***
- The triad of **cyanosis**, **foaming at the mouth** (due to inability to swallow saliva), and **intractable coughing** strongly suggests esophageal atresia, especially given the history of polyhydramnios (amniotic fluid index of 26) which often accompanies this condition.
- The inability of the newborn to clear secretions due to the blind-ending esophagus leads to aspiration and respiratory distress.
*Pulmonary hypoplasia*
- This condition is characterized by underdeveloped lungs and would present with severe respiratory distress, but typically without the prominent signs of **excessive oral secretions** and **foaming at the mouth**.
- Pulmonary hypoplasia is often associated with conditions causing oligohydramnios (e.g., renal agenesis), whereas this case presents with polyhydramnios.
*Defective swallowing reflex*
- While a defective swallowing reflex could lead to aspiration, it usually wouldn't cause the rapid accumulation of **foaming at the mouth** and intractable coughing to the degree seen with a complete esophageal obstruction.
- This is a more generalized neurological issue, whereas esophageal atresia is a structural malformation.
*Esophageal stricture*
- An esophageal stricture would cause difficulty swallowing (dysphagia), but typically allows some passage of liquids and wouldn't present with immediate, complete inability to swallow saliva and copious **foaming at the mouth** from birth.
- Strictures are more commonly acquired (e.g., from reflux or injury) rather than presenting congenitally with such acute and severe symptoms.
*Achalasia*
- Achalasia is a motility disorder of the esophagus characterized by impaired relaxation of the lower esophageal sphincter and absence of peristalsis; it is extremely rare in neonates.
- Symptoms like **dysphagia** and **regurgitation** typically develop gradually and are less likely to cause the acute, severe respiratory distress and foaming at the mouth seen immediately after birth in this case.
Congenital anomalies of GI tract US Medical PG Question 2: A 4-week-old infant is brought to the emergency department by his parents with violent vomiting. It started about 3 days ago and has slowly gotten worse. He vomits after most feedings but seems to keep some formula down. His mother notes that he is eager to feed between episodes and seems to be putting on weight. Other than an uncomplicated course of chlamydia conjunctivitis, the infant has been healthy. He was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. The physical exam is significant for a palpable mass in the right upper quadrant. What is the first-line confirmatory diagnostic test and associated finding?
- A. Abdominal ultrasound; elongated pyloric channel and muscle hypertrophy (Correct Answer)
- B. Barium upper GI series; GE junction and portion of the stomach in thorax
- C. Air enema; filling defect and coil spring sign
- D. Barium upper GI series; bird beak sign and corkscrewing
- E. Abdominal X-ray; ‘double bubble’ sign
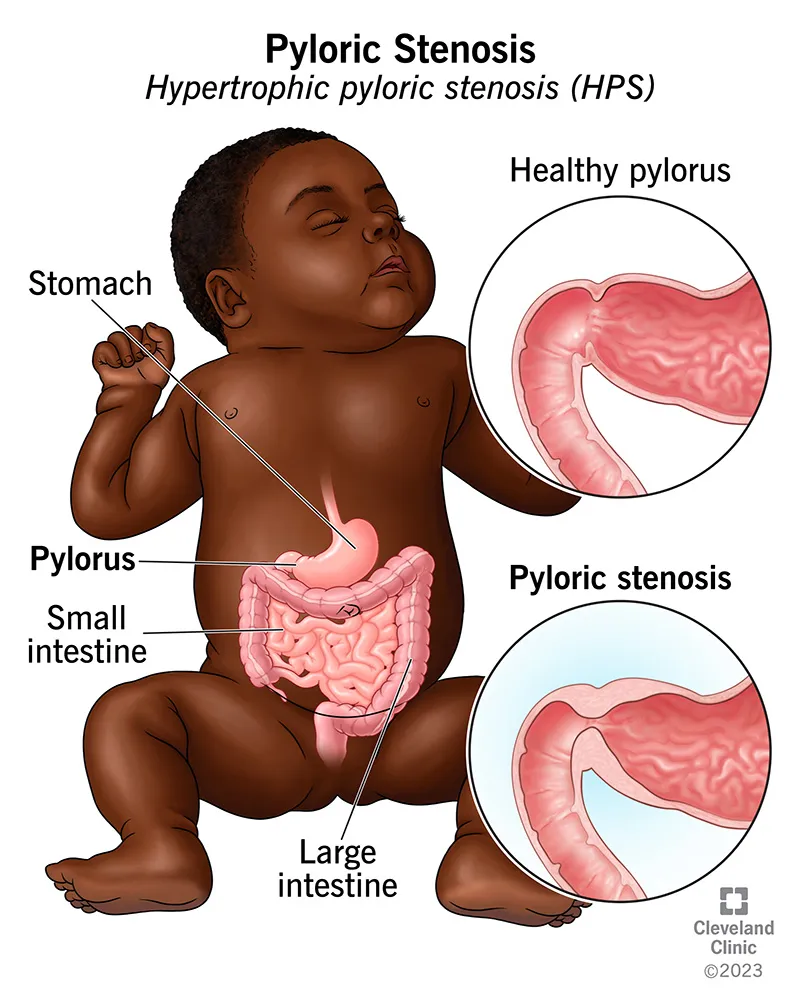
Congenital anomalies of GI tract Explanation: ***Abdominal ultrasound; elongated pyloric channel and muscle hypertrophy***
- The clinical picture of **projectile vomiting** in a 4-week-old infant, **eagerness to feed** ("hungry vomiter"), and **palpable olive-shaped mass** in the right upper quadrant is classic for **pyloric stenosis**.
- **Abdominal ultrasonography** is the gold standard for diagnosis, revealing an **elongated pyloric channel** (>16mm) and thickened pyloric muscle (>3-4mm).
- Pyloric stenosis typically presents between 3-6 weeks of age with progressive non-bilious vomiting.
*Barium upper GI series; GE junction and portion of the stomach in thorax*
- A **barium upper GI series** showing the **GE junction and stomach in the thorax** would indicate a **hiatal hernia**, which is not consistent with the palpable mass or "hungry vomiter" presentation.
- While hiatal hernias can cause vomiting and reflux, they typically don't present with this specific type of projectile vomiting or a palpable abdominal mass.
*Air enema; filling defect and coil spring sign*
- An **air enema** showing a **filling defect** and **coil spring sign** is characteristic of **intussusception**, which usually presents with sudden onset of **crampy abdominal pain**, **currant jelly stools**, and a palpable mass in the right lower quadrant.
- The clinical presentation does not fit intussusception, which typically occurs in older infants (6-36 months) and has a more acute presentation.
*Barium upper GI series; bird beak sign and corkscrewing*
- A **barium upper GI series** showing a **bird beak sign** and **corkscrewing** is pathognomonic for **midgut volvulus**, a surgical emergency.
- While volvulus can cause bilious vomiting and abdominal distension, the presentation of non-bilious vomiting with a palpable pyloric mass is more typical of pyloric stenosis.
*Abdominal X-ray; 'double bubble' sign*
- An **abdominal X-ray** revealing a **'double bubble' sign** is indicative of **duodenal atresia** or **annular pancreas**, leading to complete duodenal obstruction.
- This condition typically presents with **bilious vomiting** shortly after birth (within first day of life) and does not involve a palpable hypertrophied pylorus.
Congenital anomalies of GI tract US Medical PG Question 3: A 3-week-old boy has non-bilious projectile vomiting that occurred after feeding. After vomiting, the infant is still hungry. The infant appears dehydrated and malnourished. A firm, “olive-like” mass of about 1.5 cm in diameter is palpated in the right upper quadrant, by the lateral edge of the rectus abdominus muscle. On laboratory testing, the infant is found to have a hypochloremic, hypokalemic metabolic alkalosis. Which of the following is most likely the cause of this patient’s symptoms?
- A. Hypertrophy of the pylorus muscle (Correct Answer)
- B. Intussusception
- C. Achalasia
- D. Duodenal atresia
- E. Aganglionic colon segment
Congenital anomalies of GI tract Explanation: ***Hypertrophy of the pylorus muscle***
- The classic presentation of **pyloric stenosis** includes **non-bilious projectile vomiting** in an infant, followed by continued hunger, a palpable **"olive-like" mass** in the right upper quadrant, and findings of **hypochloremic, hypokalemic metabolic alkalosis** due to fluid and acid loss from vomiting.
- The hypertrophy of the pylorus obstructs gastric emptying, leading to the characteristic vomiting pattern and subsequent electrolyte imbalances.
*Intussusception*
- This condition presents with sudden onset of intermittent, **severe abdominal pain**, often drawing the legs up to the chest, and produces **"currant jelly" stools** (blood and mucus).
- A palpable **sausage-shaped mass** may be felt, but projectile vomiting and the classic electrolyte abnormalities described are not typical features.
*Achalasia*
- Achalasia is a motility disorder of the **esophagus** characterized by impaired relaxation of the lower esophageal sphincter and absence of esophageal peristalsis.
- While it causes **dysphagia** and regurgitation, it does not typically present in a **3-week-old infant** with projectile vomiting or an "olive-like" mass.
*Duodenal atresia*
- This is a congenital obstruction of the duodenum, often presenting with **bilious vomiting** within the first 24-48 hours of life, and a characteristic **"double bubble" sign** on abdominal X-ray.
- It does not involve a palpable "olive-like" mass or the specific electrolyte imbalance seen in pyloric stenosis.
*Aganglionic colon segment*
- This describes **Hirschsprung disease**, which is characterized by the absence of ganglion cells in the distal colon, leading to **functional obstruction**.
- Symptoms typically involve **delayed passage of meconium** and chronic constipation, abdominal distension, and sometimes bilious vomiting, not the projectile non-bilious vomiting or palpable mass of pyloric stenosis.
Congenital anomalies of GI tract US Medical PG Question 4: A 5-year-old girl is brought to a medical office for evaluation of persistent abdominal pain that has worsened over the past 24 hours. The mother states that the girl often has constipation which has worsened over the last 3 days. The mother denies that the girl has had bloody stools. The girl has not had a bowel movement or passed flatulence in 72 hours. She has vomited 3 times since last night and refuses to eat. She has no significant medical history, including no history of surgeries. On exam, there are no abdominal masses; however, the upper abdomen is distended and tympanic. What is the most likely underlying cause of the girl’s symptoms?
- A. Duodenal atresia
- B. Malrotation of the gut (Correct Answer)
- C. Pyloric stenosis
- D. Meckel’s diverticulum
- E. Volvulus
Congenital anomalies of GI tract Explanation: ***Malrotation of the gut***
- The question asks for the **underlying cause** of symptoms in a 5-year-old presenting with her **first episode** of acute bowel obstruction and **no prior surgical history**. **Malrotation** is the congenital anatomical abnormality that predisposes to **midgut volvulus**.
- **Malrotation** occurs when the bowel fails to rotate properly during fetal development, leaving the mesentery on a narrow pedicle. This anatomical defect is the underlying cause that makes volvulus possible.
- While volvulus (twisting) is the acute mechanical event causing obstruction, **malrotation is the underlying anatomical defect** being asked for in the question.
- The presentation of **abdominal pain**, **vomiting**, **abdominal distension**, inability to pass **flatus or stool** for 72 hours, and **tympanic upper abdomen** indicates acute bowel obstruction from midgut volvulus occurring on the background of malrotation.
*Volvulus*
- **Volvulus** (twisting of the bowel) is the **acute complication** that occurs, not the underlying cause.
- Volvulus is the mechanism of obstruction, but it occurs because of the underlying anatomical defect (malrotation).
- The question specifically asks for "underlying cause" - volvulus is the acute event, while malrotation is the predisposing anatomical abnormality.
*Duodenal atresia*
- **Duodenal atresia** is a congenital complete obstruction that presents in the **neonatal period** with vomiting (bilious), the classic "double bubble" sign, and feeding intolerance.
- This would have been diagnosed much earlier than 5 years of age and is not compatible with this presentation.
*Pyloric stenosis*
- **Pyloric stenosis** presents with **non-bilious projectile vomiting** in infants between **2 to 6 weeks of age**, not in a 5-year-old child.
- Physical exam classically reveals an **olive-shaped mass** in the epigastrium and visible gastric peristaltic waves.
*Meckel's diverticulum*
- **Meckel's diverticulum** most commonly presents with **painless rectal bleeding** (from ectopic gastric mucosa causing ulceration) following the "rule of 2s."
- While it can cause obstruction via intussusception or serve as a lead point, it is not the most likely underlying cause of this presentation in a 5-year-old with acute complete bowel obstruction and no prior symptoms.
Congenital anomalies of GI tract US Medical PG Question 5: A new imaging modality is being tested to study vitelline duct morphology. A fetus at 20 weeks' gestation is found to have partial obliteration of this duct. Which of the following is the most likely sequela of this condition?
- A. Discharge of urine from the umbilicus
- B. Dilation of the descending colon
- C. Swelling in the genital region
- D. Protrusion of abdominal viscera into the umbilical cord
- E. Bleeding from the gastrointestinal tract (Correct Answer)
Congenital anomalies of GI tract Explanation: ***Bleeding from the gastrointestinal tract***
- Partial obliteration of the vitelline duct can lead to a **Meckel's diverticulum**, which is a remnant of the **yolk sac**.
- Meckel's diverticulum may contain **ectopic gastric or pancreatic tissue**, leading to acid secretion, ulceration, and subsequent **gastrointestinal bleeding**.
*Discharge of urine from the umbilicus*
- This symptom is characteristic of a **patent urachus**, which is an abnormal connection between the **bladder and the umbilicus**, not related to the vitelline duct.
- The urachus is a remnant of the **allantois**, a different embryonic structure.
*Dilation of the descending colon*
- **Dilation of the colon** is more commonly associated with conditions like **Hirschsprung's disease** or other causes of intestinal obstruction, which are not directly linked to vitelline duct anomalies.
- Vitelline duct issues primarily affect the **small intestine** (ileum).
*Swelling in the genital region*
- Swelling in the genital region could indicate conditions such as a **hydrocele**, **hernia**, or **ambiguous genitalia**, which are unrelated to vitelline duct pathology.
- Vitelline duct remnants typically present around the **umbilical region or within the small bowel**.
*Protrusion of abdominal viscera into the umbilical cord*
- This description is characteristic of an **omphalocele**, a congenital defect where abdominal contents herniate through the **umbilical ring**, covered by a sac.
- While related to umbilical development, an omphalocele is a distinct condition from vitelline duct anomalies, which involve the vestigial connection between the **midgut and the yolk sac**.
Congenital anomalies of GI tract US Medical PG Question 6: A 2-year-old boy is brought in to his pediatrician for a routine checkup. The parents mention that the child has been developing appropriately, although they have been noticing that the child appears to have chronic constipation. The parents report that their child does not routinely have daily bowel movements, and they have noticed that his abdomen has become more distended recently. In the past, they report that the patient was also delayed in passing meconium, but this was not further worked up. On exam, his temperature is 98.6°F (37.0°C), blood pressure is 110/68 mmHg, pulse is 74/min, and respirations are 14/min. The patient is noted to have a slightly distended abdomen that is nontender. Eventually, this patient undergoes a biopsy. Which of the following layers most likely reveals the causative pathologic finding of this disease?
- A. Submucosa
- B. Mucosa
- C. Lamina propria
- D. Muscularis mucosa
- E. Muscularis propria (between muscle layers) (Correct Answer)
Congenital anomalies of GI tract Explanation: ***Muscularis propria (between muscle layers)***
- This patient's presentation with **chronic constipation**, **abdominal distention**, and **delayed meconium passage** is highly suggestive of **Hirschsprung disease**.
- The causative pathology in Hirschsprung disease is the **absence of ganglion cells** in the **myenteric (Auerbach's) and submucosal (Meissner's) plexuses**, which is definitively diagnosed by a rectal biopsy showing this lack of innervation.
- The **myenteric plexus** is located **between the inner circular and outer longitudinal layers** of the **muscularis propria**, making this the primary layer examined for diagnostic findings.
*Submucosa*
- While the **submucosal (Meissner's) plexus** is also affected in Hirschsprung disease and the submucosa can show absent ganglion cells, the **myenteric plexus** in the muscularis propria is the primary diagnostic target in rectal biopsies.
- Both plexuses are affected, but the muscularis propria is considered the most definitive layer for diagnosis.
*Mucosa*
- The **mucosa** is the innermost layer of the gastrointestinal tract, consisting of epithelium, lamina propria, and muscularis mucosa.
- This layer does **not** contain the enteric nervous system plexuses (myenteric or submucosal) responsible for gut motility, so biopsy of this layer alone would not reveal the absent ganglion cells characteristic of Hirschsprung disease.
*Lamina propria*
- The **lamina propria** is a thin layer of connective tissue found within the **mucosa**, beneath the epithelium.
- This layer primarily contains blood vessels, lymphatics, and immune cells, and it is **not** where the ganglion cells of the enteric nervous system are located or where the primary pathology of Hirschsprung disease is found.
*Muscularis mucosa*
- The **muscularis mucosa** is a thin layer of smooth muscle that forms the outermost layer of the **mucosa**.
- It does not contain the enteric plexuses (myenteric or submucosal) responsible for gut motility, so its biopsy would not reveal the absent ganglion cells characteristic of Hirschsprung disease.
Congenital anomalies of GI tract US Medical PG Question 7: An 8-month-old boy is brought to a medical office by his mother. The mother states that the boy has been very fussy and has not been feeding recently. The mother thinks the baby has been gaining weight despite not feeding well. The boy was delivered vaginally at 39 weeks gestation without complications. On physical examination, the boy is noted to be crying in his mother’s arms. There is no evidence of cyanosis, and the cardiac examination is within normal limits. The crying intensifies when the abdomen is palpated. The abdomen is distended with tympany in the left lower quadrant. You suspect a condition caused by the failure of specialized cells to migrate. What is the most likely diagnosis?
- A. Duodenal atresia
- B. Hirschsprung disease (Correct Answer)
- C. Meckel diverticulum
- D. Pyloric stenosis
- E. DiGeorge syndrome
Congenital anomalies of GI tract Explanation: ***Correct: Hirschsprung disease***
- This diagnosis is characterized by the **failure of neural crest cells** to migrate, leading to an **aganglionic segment of the colon** that cannot relax.
- Symptoms like **abdominal distension**, **vomiting**, and **failure to thrive** in an 8-month-old are consistent with Hirschsprung disease.
*Incorrect: Duodenal atresia*
- **Duodenal atresia** typically presents in the **neonatal period** with **bilious vomiting** and a **double-bubble sign** on imaging.
- It is a congenital obstruction but does not involve the failed migration of specialized cells, and distension with tympany in the lower quadrant is not a primary feature.
*Incorrect: Meckel diverticulum*
- A **Meckel diverticulum** is a remnant of the **vitelline duct** and is often asymptomatic or can cause **painless rectal bleeding**.
- It does not present with the described symptoms of abdominal distention and fussiness related to an intestinal obstruction or motility disorder caused by cellular migration failure.
*Incorrect: Pyloric stenosis*
- **Pyloric stenosis** typically presents with **projectile non-bilious vomiting** and an **olive-shaped mass** in the epigastrium, usually between 2 and 8 weeks of age.
- The symptoms described, such as marked abdominal distention and crying intensifying with abdominal palpation, are not typical for pyloric stenosis.
*Incorrect: DiGeorge syndrome*
- **DiGeorge syndrome** is a genetic disorder associated with **thymic and parathyroid hypoplasia**, leading to **T-cell immunodeficiency** and **hypocalcemia**.
- While it involves developmental anomalies, it does not directly present with gastrointestinal obstruction or motility issues caused by failed cell migration as the primary symptom.
Congenital anomalies of GI tract US Medical PG Question 8: A 3-week-old firstborn baby girl is brought to the pediatric emergency room with projectile vomiting. She started vomiting while feeding 12 hours ago and has been unable to keep anything down since then. After vomiting, she appears well and hungry, attempting to feed again. The vomitus has been non-bloody and non-bilious. The last wet diaper was 10 hours ago. The child was born at 40 weeks gestation to a healthy mother. On examination, the child appears sleepy but has a healthy cry during the exam. The child has dry mucous membranes and delayed capillary refill. There is a palpable olive-shaped epigastric mass on palpation. Which of the following is the most likely cause of this patient's condition?
- A. Failure of neural crest cell migration into the rectum
- B. Telescoping of the small bowel into the large bowel
- C. Hypertrophic muscularis externa (Correct Answer)
- D. Patent tract between the trachea and esophagus
- E. Failure of duodenal lumen recanalization
Congenital anomalies of GI tract Explanation: ***Hypertrophic muscularis externa***
- The presented symptoms, including **projectile vomiting** in a 3-week-old, **non-bilious** emesis, post-vomiting **hunger**, and a **palpable olive-shaped mass** in the epigastrium, are classic signs of **pyloric stenosis**. This condition is caused by the **hypertrophy of the pyloric sphincter's muscularis externa**.
- Pyloric stenosis commonly presents between **2-8 weeks of age** and leads to an obstruction of gastric outflow, causing the characteristic vomiting and signs of dehydration like **dry mucous membranes** and **delayed capillary refill**.
*Failure of neural crest cell migration into the rectum*
- This describes **Hirschsprung disease**, which typically presents with **constipation**, **abdominal distension**, and a **failure to pass meconium** in the neonatal period.
- While it involves GI obstruction, its symptoms and location of obstruction are distinctly different from the projectile vomiting seen in this case.
*Telescoping of the small bowel into the large bowel*
- This is known as **intussusception**, which usually presents with **intermittent, colicky abdominal pain**, **"currant jelly" stools** (due to blood and mucus), and a sausage-shaped abdominal mass, typically in older infants (3 months to 3 years).
- The type of vomiting (often bilious) and stool characteristics are different from the patient's presentation.
*Patent tract between the trachea and esophagus*
- This describes a **tracheoesophageal fistula (TEF)**, often associated with esophageal atresia. Infants with TEF typically present with **choking, coughing, and cyanosis** during feeds, as well as aspiration, due to misdirection of fluid into the lungs.
- The symptoms are immediate and severe with initial feeds and do not typically involve progressive projectile vomiting after several weeks of life.
*Failure of duodenal lumen recanalization*
- This leads to **duodenal atresia**, which typically presents with **bilious vomiting** within the first 24-48 hours of life, and the classic "double bubble" sign on X-ray.
- The vomiting in this case is **non-bilious** and started later, which rules out duodenal atresia.
Congenital anomalies of GI tract US Medical PG Question 9: A 72-year-old male with a past medical history significant for aortic stenosis and hypertension presents to the emergency department complaining of weakness for the past 3 weeks. He states that, apart from feeling weaker, he also has noted lightheadedness, pallor, and blood-streaked stools. The patient's vital signs are stable, and he is in no acute distress. Laboratory workup reveals that the patient is anemic. Fecal occult blood test is positive for bleeding. EGD was performed and did not reveal upper GI bleeding. Suspecting a lower GI bleed, a colonoscopy is performed after prepping the patient, and it is unremarkable. What would be an appropriate next step for localizing a lower GI bleed in this patient?
- A. Technetium-99 labelled erythrocyte scintigraphy (Correct Answer)
- B. Flexible sigmoidoscopy
- C. Nasogastric tube lavage
- D. Ultrasound of the abdomen
- E. CT of the abdomen
Congenital anomalies of GI tract Explanation: ***Technetium-99 labelled erythrocyte scintigraphy***
- This test can detect **slow-rate lower GI bleeds** (as low as 0.2-0.5 mL/min) that may be missed by endoscopy or colonoscopy, especially when the bleeding is intermittent or subtle.
- Given the **negative EGD** and **unremarkable colonoscopy** despite evidence of an ongoing lower GI bleed, this nuclear medicine study is appropriate for localization.
- Particularly useful in this patient with **aortic stenosis**, where angiodysplasia (vascular malformations, often in the small bowel) is a common cause of obscure GI bleeding (Heyde's syndrome).
*Flexible sigmoidoscopy*
- This procedure only visualizes the **rectum and a portion of the sigmoid colon**, which is insufficient given the negative full colonoscopy.
- It would not provide any new information for localizing a bleed that has already been ruled out from the accessible colon.
*Nasogastric tube lavage*
- This procedure is used to assess for **upper GI bleeding** by checking for blood in the gastric contents.
- The EGD already ruled out an upper GI bleed, making this step unnecessary and unhelpful for a suspected lower GI source.
*Ultrasound of the abdomen*
- Abdominal ultrasound is primarily used to evaluate **solid organs** (e.g., liver, gallbladder, kidneys) and potential fluid collections.
- It is generally **not effective** for localizing or diagnosing the source of active GI bleeding.
*CT of the abdomen*
- A standard CT abdomen without specialized imaging protocol has **limited sensitivity** for detecting the source of GI bleeding.
- While **CT angiography** (a different test with IV contrast timed to arterial phase) can detect active bleeding at rates >0.3-0.5 mL/min, a routine "CT of the abdomen" as listed in this option would not be adequate for localizing occult GI bleeding.
Congenital anomalies of GI tract US Medical PG Question 10: A 23-year-old woman, gravida 2, para 1, at 26 weeks gestation comes to the physician for a routine prenatal visit. Physical examination shows a uterus consistent in size with a 26-week gestation. Fetal ultrasonography shows a male fetus with a thick band constricting the right lower arm; the limb distal to the constrictive band cannot be visualized. The most likely condition is an example of which of the following embryological abnormalities?
- A. Agenesis
- B. Disruption (Correct Answer)
- C. Aplasia
- D. Deformation
- E. Malformation
Congenital anomalies of GI tract Explanation: ***Disruption***
- A **disruption** is a morphological defect of an organ or a larger body region resulting from an **extrinsic breakdown** of a previously normal developmental process.
- The **amniotic band syndrome**, causing the constricting band and absent distal limb, is a classic example of disruption due to **amniotic bands** entrapping fetal parts.
*Agenesis*
- **Agenesis** refers to the complete **absence of an organ** due to the absence of the primordial tissue from which it develops.
- In this case, the limb was initially present but was subsequently damaged, which is not agenesis.
*Aplasia*
- **Aplasia** refers to the complete **absence of an organ** when the primordial tissue was present but failed to develop.
- This differs from the scenario where a previously normally developing structure is destroyed by an extrinsic factor (disruption).
*Deformation*
- A **deformation** is an abnormality in form or position of a body part caused by **mechanical forces**, usually occurring in later fetal stages.
- Examples include clubfoot due to intrauterine compression, but it does not involve the intrinsic destruction of tissue observed here.
*Malformation*
- A **malformation** is a **primary defect** in the development of an organ or tissue due to an intrinsic abnormal developmental process.
- Examples include **cleft lip** or congenital heart defects; it is not due to an external disruptive force.
More Congenital anomalies of GI tract US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.