Upper limb fascial compartments US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Upper limb fascial compartments. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Upper limb fascial compartments US Medical PG Question 1: A patient presents with difficulty extending their wrist following trauma to the posterior forearm. Which of the following muscles would be most affected by injury to the posterior interosseous nerve?
- A. Extensor carpi ulnaris
- B. Extensor carpi radialis brevis
- C. Extensor pollicis longus
- D. Extensor digitorum (Correct Answer)
Upper limb fascial compartments Explanation: ***Extensor digitorum***
- The **posterior interosseous nerve (PIN)** innervates most muscles of the **posterior compartment of the forearm**, including the extensor digitorum. [1]
- Loss of function in the **extensor digitorum** would directly impair **extension of the fingers** and contribute significantly to difficulty extending the wrist. [1]
*Extensor carpi ulnaris*
- This muscle is also innervated by the **posterior interosseous nerve (PIN)** and contributes to **wrist extension** and **ulnar deviation**.
- While its innervation by the PIN is correct, injury to the PIN would affect this muscle, but the *extensor digitorum* is more broadly responsible for the stated primary symptom (difficulty extending the wrist), as its primary action is finger and thus wrist extension.
*Extensor carpi radialis brevis*
- While it is a **wrist extensor**, it is innervated by the **deep branch of the radial nerve** *before* it becomes the posterior interosseous nerve.
- Therefore, an isolated injury to the **posterior interosseous nerve** proper would typically spare the extensor carpi radialis brevis.
*Extensor pollicis longus*
- This muscle is indeed innervated by the **posterior interosseous nerve (PIN)** and acts to extend the **thumb**. [1]
- While it would be affected, the primary problem described is difficulty extending the *wrist*, for which the extensor digitorum plays a more significant and general role than the extensor pollicis longus.
Upper limb fascial compartments US Medical PG Question 2: A 34-year-old woman comes to the physician because of a 3-month history of pain in her right thumb and wrist that radiates to her elbow. It is worse when she holds her infant son and improves with the use of an ice pack. Six months ago, she slipped on a wet floor and fell on her right outstretched hand. Her mother takes methotrexate for chronic joint pain. The patient takes ibuprofen as needed for her current symptoms. Examination of the right hand shows tenderness over the radial styloid with swelling but no redness. There is no crepitus. Grasping her right thumb and exerting longitudinal traction toward the ulnar side elicits pain. Range of motion of the finger joints is normal. There is no swelling, redness, or tenderness of any other joints. Which of the following is the most likely diagnosis?
- A. De Quervain tenosynovitis (Correct Answer)
- B. Carpal tunnel syndrome
- C. Swan neck deformity
- D. Mallet finger
- E. Stenosing tenosynovitis
Upper limb fascial compartments Explanation: ***De Quervain tenosynovitis***
- The patient's symptoms of **radial-sided wrist pain** radiating to the elbow, worsened by activities involving thumb movement (like holding her infant), and tenderness over the **radial styloid** are classic for De Quervain tenosynovitis.
- The pain elicited by grasping the thumb and exerting traction toward the ulnar side (ulnar deviation of the wrist while the thumb is grasped - **Finkelstein's test**) is a pathognomonic finding for this condition.
*Carpal tunnel syndrome*
- Typically causes **numbness and tingling** in the thumb, index, middle, and radial half of the ring finger, often worse at night.
- Pain is usually in the **volar wrist** and does not primarily involve the radial styloid or produce a positive Finkelstein's test.
*Swan neck deformity*
- Characterized by **hyperextension of the PIP joint** and flexion of the DIP joint of the fingers, resulting in a characteristic S-shaped appearance.
- This is a **deformity** rather than an acute or subacute pain syndrome like the patient's presentation.
*Mallet finger*
- An injury to the **extensor tendon** of the finger, resulting in an inability to fully extend the DIP joint.
- There is no mention of a traumatic injury to the DIP joint or a persistent flexion deformity in this patient.
*Stenosing tenosynovitis*
- Also known as **trigger finger**, it involves **tendon sheath inflammation** that restricts the smooth gliding of tendons, typically causing catching or locking of a finger.
- This condition affects the **flexor tendons** and does not present with pain over the radial styloid or positive Finkelstein's test.
Upper limb fascial compartments US Medical PG Question 3: A 43-year-old woman comes to the physician because of tingling and weakness in her left arm for the past 2 days. An image of the brachial plexus is shown. Nerve conduction study shows decreased transmission of electrical impulses in the labeled structure. Physical examination is most likely to show impairment of which of the following movements?
- A. Opposition of the thumb
- B. Flexion of the forearm
- C. Abduction of the shoulder above 100 degrees
- D. Extension of the wrist and fingers (Correct Answer)
- E. Flexion of the metacarpophalangeal joints
Upper limb fascial compartments Explanation: ***Extension of the wrist and fingers***
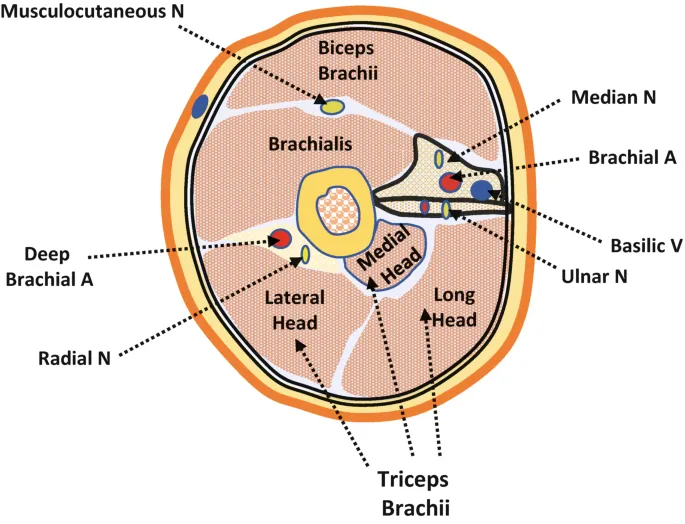
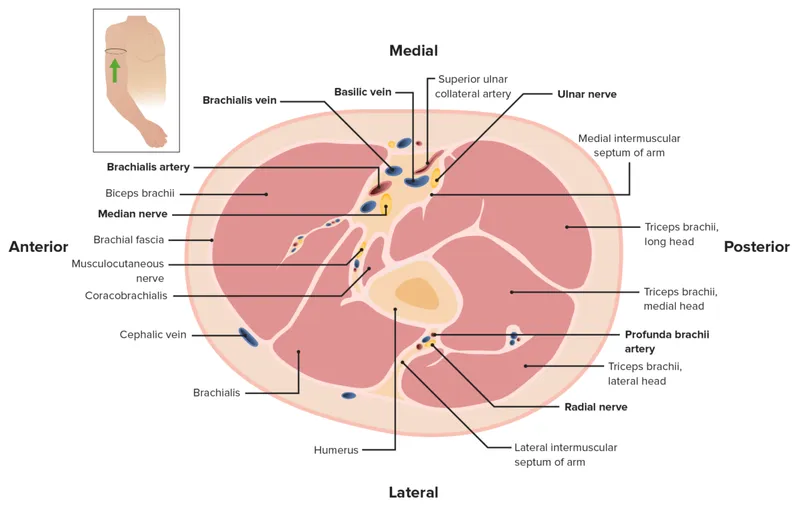
- The image and description indicate the injury affects the **posterior cord** of the brachial plexus, which gives rise to the **radial nerve**.
- The **radial nerve** innervates the muscles responsible for **extension of the wrist and fingers**, so damage to its parent cord would impair these movements.
*Opposition of the thumb*
- **Opposition of the thumb** is primarily mediated by the **median nerve**, which arises from the lateral and medial cords, not the posterior cord.
- Damage to the posterior cord due to injury would not affect this movement directly.
*Flexion of the forearm*
- **Flexion of the forearm** is primarily controlled by the **musculocutaneous nerve** and a portion by the **median nerve**.
- Both of these nerves originate from the lateral and medial cords, not the posterior cord, making impairment unlikely with posterior cord injury.
*Abduction of the shoulder above 100 degrees*
- **Abduction of the shoulder above 100 degrees** primarily requires **scapular rotation** mediated by the **trapezius muscle** (accessory nerve) and **serratus anterior** (long thoracic nerve).
- While the **axillary nerve** (from the posterior cord) innervates the **deltoid** for initial shoulder abduction, the question stem emphasizes **wrist and finger symptoms**, suggesting the labeled structure is specifically the **radial nerve** branch rather than the axillary nerve branch.
- This makes extension deficits more likely than shoulder abduction impairment.
*Flexion of the metacarpophalangeal joints*
- **Flexion of the metacarpophalangeal joints** is predominantly carried out by the **lumbricals and interossei muscles**, which are primarily innervated by the **ulnar nerve** and partially by the **median nerve**.
- These nerves originate from the medial and lateral cords, not the posterior cord, making impairment unlikely.
Upper limb fascial compartments US Medical PG Question 4: A 45-year-old man comes to the physician for the evaluation of limited mobility of his right hand for 1 year. The patient states he has had difficulty actively extending his right 4th and 5th fingers, and despite stretching exercises, his symptoms have progressed. He has type 2 diabetes mellitus. He has been working as a mason for over 20 years. His father had similar symptoms and was treated surgically. The patient has smoked one pack of cigarettes daily for 25 years and drinks 2–3 beers every day after work. His only medication is metformin. Vital signs are within normal limits. Physical examination shows skin puckering near the proximal flexor crease. There are several painless palmar nodules adjacent to the distal palmar crease. Active and passive extension of the 4th and 5th digits of the right hand is limited. Which of the following is the most likely underlying mechanism of this patient's symptoms?
- A. Ulnar nerve lesion
- B. Ganglion cyst
- C. Palmar fibromatosis (Correct Answer)
- D. Tendon sheath tumor
- E. Tenosynovitis
Upper limb fascial compartments Explanation: ***Palmar fibromatosis***
- The patient's symptoms, including **painless palmar nodules**, skin puckering near the flexor crease, and inability to actively extend the 4th and 5th fingers (a classic presentation of **Dupuytren's contracture**), are indicative of palmar fibromatosis.
- Risk factors like **male sex**, **age > 40**, **smoking**, **alcohol use**, **diabetes mellitus**, and a **family history** of similar symptoms are all present in this patient, strongly supporting the diagnosis.
*Ulnar nerve lesion*
- An ulnar nerve lesion would primarily cause **sensory deficits** (numbness/tingling in the 4th and 5th digits) and **motor weakness** in intrinsic hand muscles, leading to a **claw hand deformity**, not typically the presence of palmar nodules or skin puckering.
- While it can affect the 4th and 5th digits, the mechanism of limitation would be due to muscle weakness rather than fixed contracture.
*Ganglion cyst*
- A ganglion cyst is a **fluid-filled sac** that typically presents as a smooth, mobile, sometimes painful lump, often on the dorsal aspect of the wrist or fingers.
- It does not cause progressive finger contracture, skin puckering, or diffuse palmar nodules.
*Tendon sheath tumor*
- A tendon sheath tumor (e.g., giant cell tumor of the tendon sheath) is a **benign soft tissue mass** that presents as a firm, localized nodule, usually associated with a tendon.
- While it can limit finger movement, it typically does so by mass effect and does not cause the characteristic diffuse fibrotic changes and skin puckering seen in Dupuytren's contracture.
*Tenosynovitis*
- Tenosynovitis is **inflammation of the tendon sheath**, often causing pain, swelling, and tenderness along the course of the tendon, and sometimes a "triggering" sensation with movement.
- It does not typically manifest as painless, firm palmar nodules or progressive contracture with skin puckering.
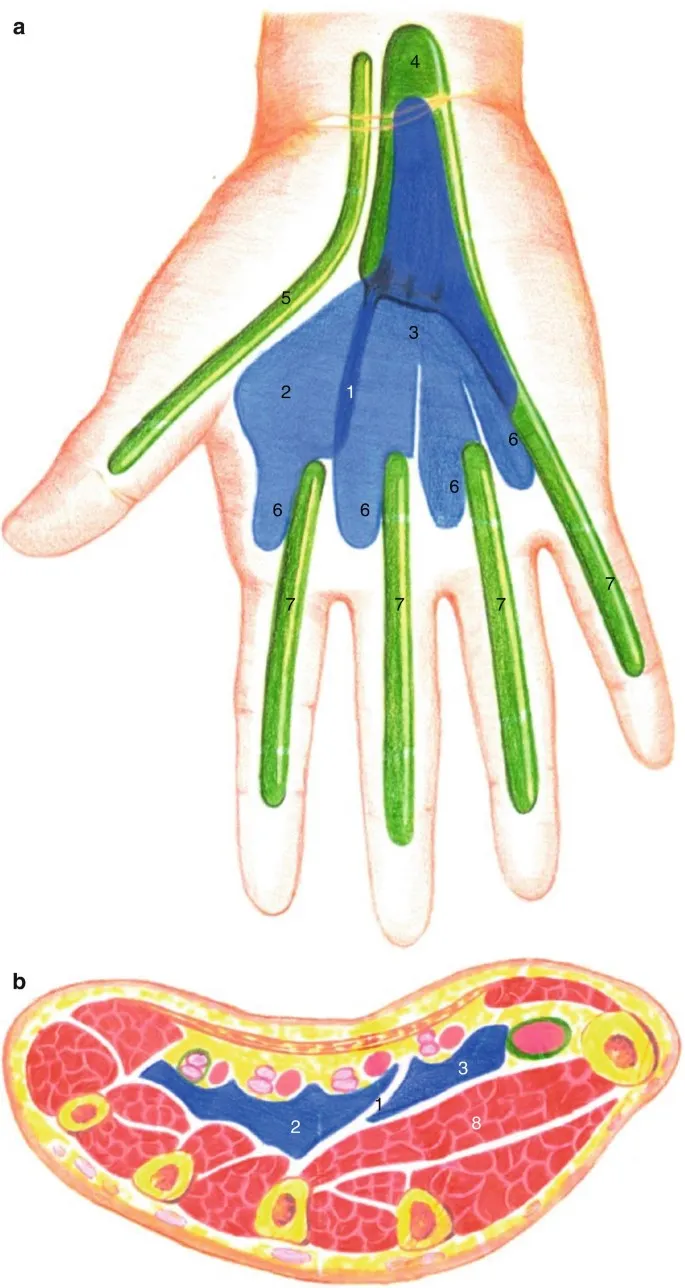
Upper limb fascial compartments US Medical PG Question 5: A 30-year-old man presents with weakness in his right hand. He says he has been an avid cyclist since the age of 20. He denies any recent trauma. Physical examination reveals decreased sensations over the 4th and 5th digits with difficulty extending the 4th and 5th digits. Strength is 4 out of 5 in the extensor muscles of the right hand and wrist. When the patient is asked to extend his fingers, the result is shown in the image. Which of the following nerves is most likely damaged in this patient?
- A. Median nerve
- B. Musculocutaneous nerve
- C. Axillary nerve
- D. Ulnar nerve (Correct Answer)
- E. Radial nerve
Upper limb fascial compartments Explanation: ***Ulnar nerve***
- The symptoms, including weakness in the **right hand**, decreased sensation over the **4th and 5th digits**, and difficulty extending the 4th and 5th digits (which suggests **ulnar claw**), are characteristic of **ulnar nerve damage**.
- **Avid cycling** can lead to compression of the ulnar nerve in the **Guyon's canal** (handlebar palsy) or at the **cubital tunnel** in the elbow, causing these specific signs.
*Median nerve*
- Damage to the median nerve typically affects the **thumb**, **index**, **middle finger**, and radial half of the ring finger, causing **ape hand deformity** or **carpal tunnel syndrome**.
- It controls movements like **thumb opposition** and **flexion of the first three digits**, which are not primarily described as impaired here.
*Musculocutaneous nerve*
- This nerve primarily innervates the **biceps brachii**, **brachialis**, and **coracobrachialis muscles**, affecting **elbow flexion** and **forearm supination**.
- It provides sensory innervation to the **lateral forearm**, symptoms not consistent with this patient's presentation.
*Axillary nerve*
- Damage to the axillary nerve results in weakness of the **deltoid** and **teres minor muscles**, leading to impaired **shoulder abduction** and external rotation.
- Sensory loss would be over the **lateral aspect of the shoulder**, which is unrelated to the described hand symptoms.
*Radial nerve*
- Radial nerve damage typically results in **wrist drop** and impaired **extension of the fingers and thumb** due to innervation of the extensors.
- While there is difficulty extending the 4th and 5th digits, the sensory loss pattern (4th and 5th digits) and specific **ulnar claw** appearance are more indicative of ulnar nerve involvement.
Upper limb fascial compartments US Medical PG Question 6: A 23-year-old patient presents to the emergency department after a motor vehicle accident. The patient was an unrestrained driver involved in a head-on collision. The patient is heavily intoxicated on what he claims is only alcohol. An initial trauma assessment is performed, and is notable for significant bruising of the right forearm. The patient is in the trauma bay, and complains of severe pain in his right forearm. A physical exam is performed and is notable for pallor, decreased sensation, and cool temperature of the skin of the right forearm. Pain is elicited upon passive movement of the right forearm and digits. A thready radial pulse is palpable. A FAST exam is performed, and is negative for signs of internal bleeding. The patient's temperature is 99.5°F (37.5°C), pulse is 100/min, blood pressure is 110/70 mmHg, respirations are 12/min, and oxygen saturation is 98% on room air. Radiography of the right forearm is ordered. The patient is still heavily intoxicated. Which of the following is the best next step in management?
- A. Fasciotomy (Correct Answer)
- B. IV fluids
- C. Analgesics
- D. Pressure measurement
- E. Detoxification
Upper limb fascial compartments Explanation: ***Fasciotomy***
- The patient exhibits classic signs of **acute compartment syndrome**, including severe pain out of proportion to injury, pain on passive stretch, pallor, decreased sensation, and cool extremity, despite a palpable pulse. These symptoms necessitate immediate surgical intervention to relieve pressure.
- A **fasciotomy** is the definitive treatment for acute compartment syndrome to prevent irreversible muscle and nerve damage, and potentially limb loss.
*IV fluids*
- While fluid resuscitation is important in trauma, the patient's current vital signs (BP 110/70 mmHg, pulse 100/min) do not indicate immediate shock requiring aggressive IV fluid administration over addressing the limb-threatening compartment syndrome.
- Prioritizing IV fluids without addressing **compartment syndrome** could lead to permanent loss of limb function.
*Analgesics*
- Administering analgesics might mask the escalating pain a key symptom of compartment syndrome, which could delay diagnosis and definitive treatment.
- While pain control is important, it should not supersede measures to prevent irreversible tissue damage.
*Pressure measurement*
- While compartment pressure measurement can confirm the diagnosis of compartment syndrome, the clinical presentation in this case is so compelling that delaying definitive treatment for pressure measurement is not the best next step.
- Clinical signs and symptoms are often sufficient for diagnosis, and surgical intervention should not be deferred pending pressure readings in clear-cut cases.
*Detoxification*
- Detoxification for alcohol intoxication is not an emergent and immediate priority in comparison to the limb-threatening condition of acute compartment syndrome.
- Addressing the **compartment syndrome** is critical for preserving limb viability, whereas detoxification can be managed once acute medical emergencies are controlled.
Upper limb fascial compartments US Medical PG Question 7: A 35-year-old man is referred to a physical therapist due to limitation of movement in the wrist and fingers of his left hand. He cannot hold objects or perform daily activities with his left hand. He broke his left arm at the humerus one month ago. The break was simple and treatment involved a cast for one month. Then he lost his health insurance and could not return for follow up. Only after removing the cast did he notice the movement issues in his left hand and wrist. His past medical history is otherwise insignificant, and vital signs are within normal limits. On examination, the patient’s left hand is pale and flexed in a claw-like position. It is firm and tender to palpation. Right radial pulse is 2+ and left radial pulse is 1+. The patient is unable to actively extend his fingers and wrist, and passive extension is difficult and painful. Which of the following is a proper treatment for the presented patient?
- A. Surgical release (Correct Answer)
- B. Botulinum toxin injections
- C. Collagenase injections
- D. Needle fasciotomy
- E. Corticosteroid injections
Upper limb fascial compartments Explanation: ***Surgical release***
- The patient presents with classic signs of **established Volkmann's ischemic contracture** (claw-like hand, firm fibrotic tissue, limited movement, decreased radial pulse), which is the end-stage result of untreated compartment syndrome that occurred during fracture healing.
- Since this is **chronic contracture (one month post-injury)**, the appropriate surgical treatment involves **reconstructive procedures** such as muscle slide operations, tendon lengthening, tendon transfers, neurolysis, or in severe cases, free functional muscle transfer to restore hand function.
- Emergency fasciotomy would have been appropriate for **acute compartment syndrome** (within 6-8 hours of onset), but at this stage, the treatment focuses on releasing fibrotic tissue and restoring function through reconstructive surgery.
*Botulinum toxin injections*
- **Botulinum toxin** is used to relax spastic muscles in neurological conditions (e.g., cerebral palsy, stroke), but it does not address the underlying **ischemic fibrosis and muscle necrosis** of Volkmann's contracture.
- It would not improve the structural contracture or restore blood flow in this patient.
*Collagenase injections*
- **Collagenase injections** are used for localized fascial contractures like Dupuytren's contracture, where enzymatic breakdown of collagen cords can restore finger extension.
- They are ineffective for **Volkmann's contracture**, which involves widespread ischemic muscle necrosis, fibrosis, and nerve damage requiring surgical reconstruction.
*Needle fasciotomy*
- **Needle fasciotomy** is a minimally invasive technique for Dupuytren's contracture, involving percutaneous disruption of fascial cords.
- It is not suitable for **Volkmann's contracture**, which requires extensive surgical release of fibrotic muscle compartments, possible tendon transfers, and neurolysis—procedures that cannot be accomplished with needle techniques.
*Corticosteroid injections*
- **Corticosteroids** reduce inflammation in conditions like tenosynovitis or trigger finger.
- They would not address the **ischemic muscle necrosis and fibrotic contracture** in Volkmann's contracture and could potentially delay appropriate surgical treatment.
Upper limb fascial compartments US Medical PG Question 8: A 47-year-old woman presents to her primary care provider because of numbness and tingling on the palmar aspects of both hands. She denies any symptoms at the base of her thumbs. The symptoms are worse on the right (dominant hand) and are increased with activities such as driving or brushing her hair. She frequently wakes up with pain and has to shake her hand for pain relief. She has had rheumatoid arthritis for 9 years, for which she takes methotrexate. Her blood pressure is 124/76 mm Hg, the heart rate is 75/min, and the respiratory rate is 15/min. Lightly tapping over the middle of the anterior aspect of the right wrist leads to a tingling sensation in the palm. In this patient, electromyography (EMG) will most likely show which of the following results?
- A. Neuropathic changes in the palmar branch of the median nerve
- B. Denervation in C7 innervated paraspinal, arms, and shoulder muscles
- C. Focal slowing of conduction velocity in the median nerve in the carpal tunnel (Correct Answer)
- D. Widespread symmetrical neuropathic changes without focal abnormalities
- E. Widespread denervation in proximal muscles with normal sensory nerves
Upper limb fascial compartments Explanation: ***Focal slowing of conduction velocity in the median nerve in the carpal tunnel***
- The patient's symptoms (numbness, tingling in palmar hands, worsening with activity, nocturnal pain relieved by shaking, **Tinel's sign** at the wrist) are classic for **carpal tunnel syndrome (CTS)**, caused by compression of the **median nerve** at the wrist.
- **Electromyography (EMG)** and **nerve conduction studies (NCS)** are confirmatory tests for CTS, demonstrating slowed conduction velocity specifically through the carpal tunnel.
*Neuropathic changes in the palmar branch of the median nerve*
- The **palmar cutaneous branch** of the median nerve typically branches off **proximal to the carpal tunnel** and supplies sensation to the base of the thumb.
- Since the patient specifically denies symptoms at the base of her thumbs, isolated involvement of the palmar cutaneous branch is unlikely in this case, pointing to compression within the carpal tunnel.
*Denervation in C7 innervated paraspinal, arms, and shoulder muscles*
- **C7 radiculopathy** would involve symptoms in the C7 dermatome and myotome, potentially affecting muscles in the arm and shoulder.
- Her symptoms are primarily wrist and hand-focused, without signs of cervical spine involvement or widespread muscle weakness.
*Widespread symmetrical neuropathic changes without focal abnormalities*
- This pattern suggests a **generalized peripheral neuropathy**, which would likely present with more diffuse and possibly symmetrical symptoms, often involving the feet first.
- This patient's symptoms are distinctly focal and related to the distribution of the median nerve in the hand.
*Widespread denervation in proximal muscles with normal sensory nerves*
- This presentation is more consistent with a **motor neuron disease** or a **myopathy**, where there is primarily motor involvement and sensory nerves are typically spared.
- The patient's primary symptoms are sensory (numbness and tingling), and there is no indication of widespread muscle weakness or atrophy typical of denervation in proximal muscles.
Upper limb fascial compartments US Medical PG Question 9: A 35-year-old man is brought to the trauma bay by ambulance after sustaining a gunshot wound to the right arm. The patient is in excruciating pain and states that he can't move or feel his hand. The patient states that he has no other medical conditions. On exam, the patient's temperature is 98.4°F (36.9°C), blood pressure is 140/86 mmHg, pulse is 112/min, and respirations are 14/min. The patient is alert and his Glasgow coma scale is 15. On exam, he has a single wound on his right forearm without continued bleeding. The patient has preserved motor and sensation in his right elbow; however, he is unable to extend his wrist or extend his fingers further. He is able to clench his hand, but this is limited by pain. On sensory exam, the patient has no sensation to the first dorsal web space but has preserved sensation on most of the volar surface. Which of the following structures is most likely injured?
- A. Recurrent motor branch of the median nerve
- B. Main median nerve
- C. Lower trunk
- D. Ulnar nerve
- E. Radial nerve (Correct Answer)
Upper limb fascial compartments Explanation: ***Radial nerve***
- The inability to **extend the wrist and fingers** (wrist drop) is a classic sign of **radial nerve injury**, as it innervates the extensors of the forearm and hand.
- **Loss of sensation in the first dorsal web space** is also characteristic of radial nerve damage, as this area is supplied by the superficial radial nerve.
*Recurrent motor branch of the median nerve*
- This nerve primarily innervates the **thenar muscles** (flexor pollicis brevis, abductor pollicis brevis, opponens pollicis), affecting **thumb opposition**.
- Injury would primarily lead to **weakness in thumb movements**, not wrist or finger extension, and would spare sensation in the first dorsal web space.
*Main median nerve*
- The median nerve primarily innervates the **flexors of the forearm and hand**, and contributes to sensation on the **volar aspect of the thumb**, index, middle, and radial half of the ring finger.
- Injury would cause difficulty with **flexion of the wrist and fingers**, and loss of sensation on the volar surface, which is largely preserved in this patient.
*Lower trunk*
- The lower trunk of the brachial plexus (C8-T1) gives rise to the ulnar nerve and part of the median nerve, affecting **flexion of the wrist and fingers**, and intrinsic hand muscles.
- Injury would result in more widespread weakness affecting the **intrinsic hand muscles** and flexion, and would include sensory loss in the **ulnar nerve distribution**, which is not described.
*Ulnar nerve*
- The ulnar nerve primarily innervates the **intrinsic hand muscles** (excluding the thenar group) and the **flexor carpi ulnaris** and **medial half of flexor digitorum profundus**.
- Injury would typically cause **weakness in intrinsic hand functions** (e.g., finger abduction/adduction, ring and little finger flexion) and sensory loss on the **ulnar side of the hand**, not the dorsal web space.
Upper limb fascial compartments US Medical PG Question 10: A 35-year-old woman presents with progressive vision loss and severe headache. MRI shows cavernous sinus thrombosis with extension into the superior ophthalmic vein. Blood cultures grow Staphylococcus aureus. History reveals she had squeezed a facial pustule near her upper lip 5 days prior. Evaluate the anatomical explanation and risk stratification for this complication.
- A. Direct lymphatic spread from facial infection due to rich subcutaneous lymphatic network
- B. Valveless facial venous system allowing retrograde flow from danger triangle to cavernous sinus (Correct Answer)
- C. Contiguous spread through cribriform plate from nasal cavity involvement
- D. Hematogenous seeding via internal jugular vein and sigmoid sinus
- E. Extension through pterygoid venous plexus communicating with middle meningeal vein
Upper limb fascial compartments Explanation: ***Valveless facial venous system allowing retrograde flow from danger triangle to cavernous sinus***
- The **danger triangle of the face** (perioral and nasal areas) contains **valveless veins**, which allows blood to flow in a **retrograde** direction toward the intracranial space.
- Infections in this region can spread via the **angular vein** into the **superior ophthalmic vein**, directly reaching the **cavernous sinus** and causing septic thrombosis.
*Direct lymphatic spread from facial infection due to rich subcutaneous lymphatic network*
- While the face has a rich **lymphatic network**, lymphatic drainage typically leads to **submandibular or cervical lymph nodes**, not the cavernous sinus.
- Cavernous sinus thrombosis is a **vascular complication** specifically involving the **venous system**, not the lymphatic system.
*Contiguous spread through cribriform plate from nasal cavity involvement*
- The **cribriform plate** is a route for infections to enter the **subarachnoid space**, primarily leading to **meningitis** or brain abscesses.
- It does not serve as the primary anatomical conduit for superficial facial infections to localize within the **cavernous sinus**.
*Hematogenous seeding via internal jugular vein and sigmoid sinus*
- The **internal jugular vein** and **sigmoid sinus** represent the **outflow tract** away from the brain; flow to the cavernous sinus through this route would be highly atypical.
- Bacterial seeding via this route would usually imply **systemic bacteremia** or infection in the **mastoid air cells**, rather than a localized facial pustule.
*Extension through pterygoid venous plexus communicating with middle meningeal vein*
- The **pterygoid venous plexus** can communicate with the cavernous sinus, but it primarily drains the **infratemporal fossa** and deep face, not the superficial upper lip.
- The **middle meningeal vein** drains into the pterygoid plexus or sphenoparietal sinus and is not the classic path for **danger triangle** infections.
More Upper limb fascial compartments US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.