Thoracic fascial planes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thoracic fascial planes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
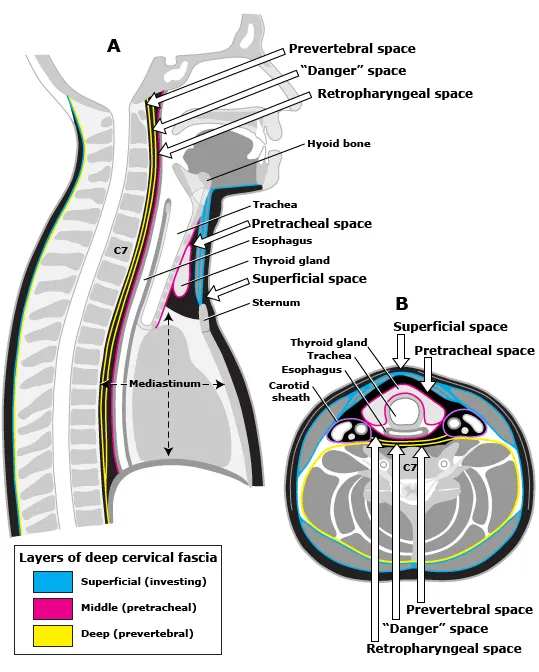
Thoracic fascial planes US Medical PG Question 1: A 26-year-old woman presents to the medicine clinic with swelling around the right side of her chin and neck (Image A). She reports pain when moving her jaw and chewing. Her symptoms developed two days after receiving an uncomplicated tonsillectomy. She has been followed by a general medical physician since birth and has received all of her standard health maintenance procedures. Vital signs are stable with the exception of a temperature of 38.4 degrees Celcius. The area in question on the right side is exquisitely tender. The remainder of her exam is benign. What is the most likely diagnosis?
- A. Superior vena cava syndrome
- B. Mumps
- C. Acute bacterial parotitis (Correct Answer)
- D. Sjogren's syndrome
- E. Pleomorphic adenoma
Thoracic fascial planes Explanation: **Acute bacterial parotitis**
- The patient's presentation with **unilateral swelling** around the chin and neck, **pain with jaw movement and chewing**, fever, and **exquisite tenderness** in the area, particularly after a recent **tonsillectomy** (which can predispose to dehydration or salivary gland dysfunction), is highly characteristic of acute bacterial parotitis.
- The elevated temperature further supports an infectious etiology, and the **post-operative setting** increases the risk for this condition due to potential retrograde infection from the oral cavity.
*Superior vena cava syndrome*
- This syndrome typically presents with **facial and neck edema**, distended neck veins, and dyspnea, resulting from obstruction of the superior vena cava, usually by a mass.
- It does not typically cause localized, **exquisitely tender swelling** or pain with jaw movement, and a recent tonsillectomy is not a risk factor.
*Mumps*
- While mumps causes **parotid gland swelling**, it is a viral infection that usually presents with **bilateral parotitis**, although unilateral cases can occur.
- The patient's history of receiving **all standard health maintenance procedures** suggests she has likely been vaccinated against mumps, making it less probable, and the rapid onset post-tonsillectomy points more towards a bacterial process.
*Sjogren's syndrome*
- This is a **chronic autoimmune disease** primarily affecting the exocrine glands, leading to **dry eyes and dry mouth**, and can cause recurrent enlargement of the parotid glands.
- It would not explain the **acute, painful, and tender swelling with fever** in a patient with no prior history of autoimmune disease, nor would it typically follow a tonsillectomy.
*Pleomorphic adenoma*
- This is a common **benign salivary gland tumor** that typically presents as a **slow-growing, painless mass** in the parotid gland.
- It would not explain the **acute onset, pain, tenderness, and fever** described in the patient, which are indicative of an inflammatory or infectious process.
Thoracic fascial planes US Medical PG Question 2: A 66-year-old man is transferred from another hospital after 3 days of progressively severe headache, vomiting, low-grade fever, and confusion. According to his partner, the patient has been dealing with some memory loss and complaining about headaches for the past 2 weeks. He has a history of interstitial pulmonary disease that required lung transplantation 2 years ago. Upon admission, he is found with a blood pressure of 160/100 mm Hg, a pulse of 58/min, a respiratory rate of 15/min, and a body temperature of 36°C (97°F). During the examination, he is found with oral thrush and symmetric and reactive pupils; there are no focal neurological signs or papilledema. A lumbar puncture is performed. Which of the following features would be expected to be found in this case?
- A. Aspect: clear, opening pressure: normal, cell count: < 5 cells/µL, protein: normal, glucose: normal
- B. Aspect: clear, opening pressure: normal, cell count: ↑ lymphocytes, protein: normal, glucose: normal
- C. Aspect: cloudy, opening pressure: ↑, cell count: ↑ neutrophils, protein: ↑, glucose: ↓
- D. Aspect: xanthochromic, opening pressure: normal, cell count: ↑ red blood cells, protein: normal, glucose: normal
- E. Aspect: clear, opening pressure: ↑, cell count: ↑ lymphocytes, protein: ↑, glucose: ↓ (Correct Answer)
Thoracic fascial planes Explanation: ***Aspect: clear, opening pressure: ↑, cell count: ↑ lymphocytes, protein: ↑, glucose: ↓***
- This patient presents with symptoms highly suggestive of **cryptococcal meningitis**, a common opportunistic infection in immunocompromised individuals like transplant recipients.
- **Cryptococcal meningitis** characteristically presents with **clear CSF** (not cloudy, which differentiates it from bacterial meningitis), **markedly elevated opening pressure** (often >25 cm H₂O), **lymphocytic pleocytosis**, **elevated protein**, and **decreased glucose** due to fungal metabolism.
- The presence of **oral thrush** strongly suggests fungal infection in this immunocompromised patient.
*Aspect: clear, opening pressure: normal, cell count: < 5 cells/µL, protein: normal, glucose: normal*
- This describes **normal cerebrospinal fluid (CSF)** parameters, which would not be expected in a patient presenting with signs and symptoms of meningitis, such as headache, vomiting, fever, and confusion.
- The patient's history of lung transplantation and oral thrush suggests an immunocompromised state and an opportunistic infection, ruling out normal CSF.
*Aspect: clear, opening pressure: normal, cell count: ↑ lymphocytes, protein: normal, glucose: normal*
- While **increased lymphocytes** can be seen in aseptic or viral meningitis, the overall picture of normal opening pressure, protein, and glucose does not fit this immunocompromised patient with subacute meningitis.
- The presence of **oral thrush** and **2 weeks of symptoms** indicate a more severe opportunistic infection like cryptococcal meningitis, which would show elevated opening pressure and abnormal protein and glucose levels.
*Aspect: cloudy, opening pressure: ↑, cell count: ↑ neutrophils, protein: ↑, glucose: ↓*
- This CSF profile is characteristic of **bacterial meningitis**, which is primarily marked by **cloudy CSF** due to significant **neutrophilic pleocytosis**.
- While the patient is immunocompromised, the history of **subacute symptoms** (2 weeks of headache/memory loss) and gradual deterioration is more typical of a fungal infection like **cryptococcal meningitis** rather than acute bacterial meningitis, which presents more acutely.
*Aspect: xanthochromic, opening pressure: normal, cell count: ↑ red blood cells, protein: normal, glucose: normal*
- **Xanthochromic CSF** with **elevated red blood cells** indicates subarachnoid hemorrhage.
- While headache is present, the patient's symptoms of fever, progressive confusion, oral thrush, and immunocompromised status point away from a primary hemorrhagic event and towards an infectious etiology.
Thoracic fascial planes US Medical PG Question 3: A 60-year-old woman is rushed to the emergency room after falling on her right elbow while walking down the stairs. She cannot raise her right arm. Her vital signs are stable, and the physical examination reveals loss of sensation over the upper lateral aspect of the right arm and shoulder. A radiologic evaluation shows a fracture of the surgical neck of the right humerus. Which of the following muscles is supplied by the nerve that is most likely damaged?
- A. Teres minor (Correct Answer)
- B. Teres major
- C. Subscapularis
- D. Infraspinatus
- E. Supraspinatus
Thoracic fascial planes Explanation: ***Teres minor***
- A fracture of the **surgical neck of the humerus** often damages the **axillary nerve**, which innervates the **teres minor**.
- The axillary nerve also supplies the **deltoid muscle** and provides cutaneous sensation to the **upper lateral arm**, consistent with the patient's sensory loss.
*Teres major*
- This muscle is innervated by the **lower subscapular nerve**, which is less likely to be damaged in a surgical neck fracture.
- Its primary action is **adduction** and **internal rotation** of the arm.
*Subscapularis*
- The **subscapularis** is innervated by the **upper and lower subscapular nerves**.
- While it contributes to internal rotation, its nerve supply is typically protected in this type of fracture.
*Infraspinatus*
- The **infraspinatus** muscle is innervated by the **suprascapular nerve**.
- This nerve is generally not affected by a fracture of the surgical neck of the humerus.
*Supraspinatus*
- Similar to the infraspinatus, the **supraspinatus** is also innervated by the **suprascapular nerve**.
- Damage to this nerve due to a humeral surgical neck fracture is uncommon.
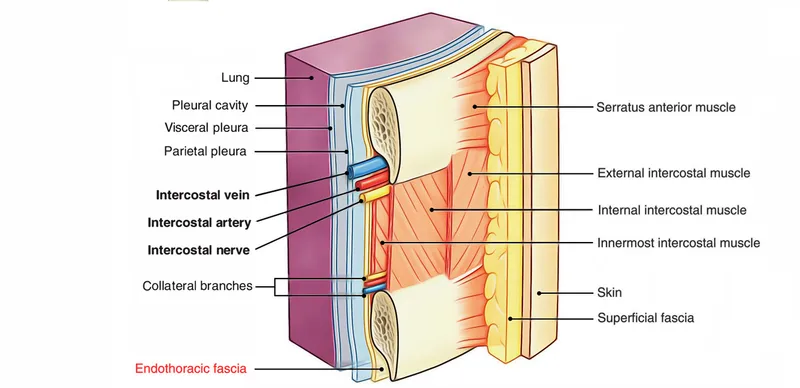
Thoracic fascial planes US Medical PG Question 4: A 14-year-old boy is brought to the emergency department because of acute left-sided chest pain and dyspnea following a motor vehicle accident. His pulse is 122/min and blood pressure is 85/45 mm Hg. Physical examination shows distended neck veins and tracheal displacement to the right side. The left chest is hyperresonant to percussion and there are decreased breath sounds. This patient would most benefit from needle insertion at which of the following anatomical sites?
- A. 5th left intercostal space along the midclavicular line
- B. 8th left intercostal space along the posterior axillary line
- C. 2nd left intercostal space along the midclavicular line (Correct Answer)
- D. Subxiphoid space in the left sternocostal margin
- E. 5th left intercostal space along the midaxillary line
Thoracic fascial planes Explanation: ***2nd left intercostal space along the midclavicular line***
- The patient's symptoms (chest pain, dyspnea, hypotension, distended neck veins, tracheal deviation, hyperresonance, and decreased breath sounds on the left) are classic signs of a **tension pneumothorax**.
- Immediate treatment for **tension pneumothorax** involves needle decompression at the **2nd intercostal space** in the midclavicular line to relieve pressure and restore hemodynamic stability.
*5th left intercostal space along the midclavicular line*
- This location is typically used for **chest tube insertion** in a more controlled setting, not for emergent needle decompression of a tension pneumothorax.
- While it's a safe location for pleural access, it is not the **first-line site** for immediate life-saving decompression.
*8th left intercostal space along the posterior axillary line*
- This site is too low and posterior for effective needle decompression of a tension pneumothorax, which requires rapid access to the **apex of the lung**.
- It is more commonly used for **thoracentesis** to drain fluid from the pleural cavity.
*Subxiphoid space in the left sternocostal margin*
- This location is primarily used for **pericardiocentesis** to drain fluid from the pericardial sac in cases of cardiac tamponade.
- It is not appropriate for addressing a **pneumothorax**, which involves air in the pleural space.
*5th left intercostal space along the midaxillary line*
- This site is a common alternative for **chest tube insertion** but is not the preferred or most immediate site for needle decompression of a tension pneumothorax.
- While it offers pleural access, the **2nd intercostal space** anteriorly is chosen for expediency and safety in an emergency.
Thoracic fascial planes US Medical PG Question 5: A 16-year-old girl presents with a sore throat. The patient says symptoms onset acutely 3 days ago and have progressively worsened. She denies any history of cough, nasal congestion or rhinorrhea. No significant past medical history or current medications. The vital signs include: temperature 37.7°C (99.9°F), blood pressure 110/70 mm Hg, pulse 74/min, respiratory rate 20/min, and oxygen saturation 99% on room air. Physical examination is significant for anterior cervical lymphadenopathy. There is edema of the oropharynx and tonsillar swelling but no tonsillar exudate. Which of the following is the next best step in management?
- A. Reassurance
- B. Empiric treatment with antibiotics
- C. Empiric treatment with antivirals
- D. Rapid strep test (Correct Answer)
- E. Ultrasound of the anterior cervical lymph nodes
Thoracic fascial planes Explanation: ***Rapid strep test***
- This patient presents with symptoms suggestive of **Streptococcal pharyngitis (Centor criteria)**, including acute onset sore throat, anterior cervical lymphadenopathy, tonsillar swelling, and absence of cough. A rapid strep test is crucial to confirm the diagnosis and guide antibiotic therapy.
- While tonsillar exudates are often present in strep throat, their absence does not rule out the diagnosis, especially given the other strong indicators.
*Reassurance*
- Reassurance alone is insufficient given the patient's symptoms are highly suggestive of a **bacterial infection** that could lead to serious complications if left untreated.
- Untreated **Streptococcal pharyngitis** can lead to complications such as acute rheumatic fever and peritonsillar abscess.
*Empiric treatment with antibiotics*
- Empiric antibiotic treatment without confirmation can contribute to **antibiotic resistance** and is not the best approach when a diagnostic test is readily available.
- Without a positive rapid strep test, the patient could be unnecessarily exposed to antibiotics, potentially leading to **adverse drug reactions** or masking other underlying conditions.
*Empiric treatment with antivirals*
- The patient's symptoms are more consistent with a **bacterial infection** (strep throat) rather than a viral illness that would benefit from antiviral treatment.
- Antivirals are generally reserved for specific viral infections like influenza or herpes, and there is no indication for their use in this clinical scenario.
*Ultrasound of the anterior cervical lymph nodes*
- While the patient has **anterior cervical lymphadenopathy**, this is a common finding in pharyngitis and an ultrasound is not necessary as a first step to diagnose the cause of a sore throat.
- Imaging of the lymph nodes would be considered if there were concerns for an **abscess** or malignancy, which are not suggested by the current presentation.
Thoracic fascial planes US Medical PG Question 6: A 40-year-old male presents to the physician's office complaining of an inability to push doors open. He has had this problem since he was playing football with his children and was tackled underneath his right arm on his lateral chest. On examination, he has a winged scapula on the right side. Which of the following nerves is most likely the cause of this presentation?
- A. Phrenic nerve
- B. Spinal accessory nerve
- C. Long thoracic nerve (Correct Answer)
- D. Greater auricular nerve
- E. Musculocutaneous nerve
Thoracic fascial planes Explanation: ***Long thoracic nerve***
- The **long thoracic nerve** innervates the **serratus anterior muscle**, which is responsible for scapular protraction and upward rotation.
- Damage to this nerve, often from trauma to the lateral chest wall (tackled underneath the arm), leads to paralysis of the serratus anterior and a characteristic **winged scapula** with lateral and inferior prominence.
- Patients have difficulty with **pushing movements** (protraction) and overhead activities.
*Phrenic nerve*
- The **phrenic nerve** primarily innervates the **diaphragm** and is crucial for respiration.
- Damage to the phrenic nerve would cause respiratory compromise, not a winged scapula or difficulty pushing doors.
*Spinal accessory nerve*
- The **spinal accessory nerve (cranial nerve XI)** innervates the **sternocleidomastoid** and **trapezius muscles**.
- Injury to this nerve can cause scapular winging due to **trapezius paralysis**, but the winging is typically **medial** with the inferior angle moving medially, unlike the lateral winging from serratus anterior paralysis.
- The mechanism of injury (lateral chest trauma during tackling) and inability to push are classic for **long thoracic nerve** injury, not spinal accessory nerve.
*Greater auricular nerve*
- The **greater auricular nerve** is a cutaneous nerve that provides sensation to the skin over the parotid gland, mastoid process, and auricle.
- Damage to this nerve would result in sensory loss in these areas and is unrelated to muscle weakness or a winged scapula.
*Musculocutaneous nerve*
- The **musculocutaneous nerve** innervates the **biceps brachii**, **brachialis**, and **coracobrachialis muscles**, responsible for elbow flexion and forearm supination.
- Damage to this nerve would primarily affect these movements and sensation in the lateral forearm, not leading to a winged scapula.
Thoracic fascial planes US Medical PG Question 7: A 50-year-old man presents with severe chest pain for a week. His pain increases with breathing and is localized to the right. He has tried over-the-counter medications at home, but they did not help. The patient has a 20-pack-year smoking history and currently smokes 2 packs of cigarettes daily, and he drinks 3 to 4 cans of beer daily before dinner. His temperature is 39.1°C (102.3°F), blood pressure is 127/85 mm Hg, pulse is 109/min, and respirations are 20/min. Respiratory examination shows dullness to percussion from the 7th rib inferiorly at the right midaxillary line, decreased vocal tactile fremitus, and diminished breath sounds in the same area. Chest radiograph is shown in the image. The patient is prepared for thoracocentesis. Which of the following locations would be the most appropriate for insertion of a chest tube?
- A. Below the inferior border of the 7th rib in the midaxillary line
- B. Above the superior border of the 8th rib in the midaxillary line (Correct Answer)
- C. Above the superior border of the 5th rib in the midclavicular line
- D. Below the inferior border of the 5th rib in the midaxillary line
- E. Above the superior border of the 7th rib in the midclavicular line
Thoracic fascial planes Explanation: ***Above the superior border of the 8th rib in the midaxillary line***
- The patient presents with symptoms and signs suggestive of a **pleural effusion** (dullness to percussion, decreased fremitus, diminished breath sounds) and potentially an **empyema** given the fever and lung consolidation on the radiograph.
- Thoracocentesis should be performed in the **midaxillary line** between the 6th and 9th ribs to avoid injuring the **diaphragm and abdominal organs**, which can rise as high as the 5th intercostal space during expiration. To prevent damage to the neurovascular bundle that runs along the inferior border of the ribs, the needle should be inserted just **above the superior border** of the rib below the chosen intercostal space.
*Below the inferior border of the 7th rib in the midaxillary line*
- Inserting below the inferior border of the 7th rib increases the risk of injuring the **neurovascular bundle** that runs along the inferior rib margin.
- Such placement might also be too low, increasing the risk of penetrating the **diaphragm** or **abdominal organs**. This location would correspond to the 8th intercostal space, but the 'below inferior border' part is incorrect.
*Above the superior border of the 5th rib in the midclavicular line*
- The **midclavicular line** is typically used for needle decompression of a tension pneumothorax (2nd intercostal space) but is not the preferred site for thoracocentesis due to the risk of striking the lung parenchyma or internal mammary artery.
- Even if considering a pneumothorax, the 5th intercostal space in the midclavicular line is not the standard site, and an effusion is indicated here.
*Below the inferior border of the 5th rib in the midaxillary line*
- Inserting below the inferior border of the 5th rib, similar to option A, risks injury to the **neurovascular bundle**.
- While in the midaxillary line, the 5th rib might be too high for an effusion, and the technique of inserting below the inferior border is incorrect.
*Above the superior border of the 7th rib in the midclavicular line*
- The **midclavicular line** is generally avoided for thoracocentesis of effusions due to the risks mentioned previously and poor drainage if the effusion is posterior.
- The 7th intercostal space in the midclavicular line is also a non-standard and less safe location for this procedure.
Thoracic fascial planes US Medical PG Question 8: A 4-year-old boy is brought to the physician because of a 5-day history of sore throat and a painful swelling on the left side of his neck that has become progressively larger. He has had pain during swallowing and has refused to eat solid foods for the past 3 days. He immigrated to the United States one year ago from India. His immunization records are unavailable. His family keeps 2 cats as pets. He appears well. He is at the 60th percentile for height and 50th percentile for weight. His temperature is 37.7°C (99.9°F), pulse is 103/min, and blood pressure is 92/60 mm Hg. The oropharynx is erythematous; the tonsils are enlarged with exudates. There is a 3-cm warm, tender, nonfluctuant cervical lymph node on the left side of the neck. His hemoglobin is 12.6 g/dL, leukocyte count is 11,100/mm3, and platelet count is 180,000/mm3. In addition to obtaining a throat swab and culture, which of the following is the most appropriate next step in management?
- A. Incision and drainage
- B. Sulfadiazine and pyrimethamine therapy
- C. Clindamycin therapy (Correct Answer)
- D. Immunoglobulin therapy
- E. Fine-needle aspiration biopsy
Thoracic fascial planes Explanation: ***Clindamycin therapy***
- The patient's symptoms (sore throat, dysphagia, warm, tender cervical lymphadenopathy, tonsillar exudates) are highly suggestive of **bacterial tonsillitis** with associated **cervical lymphadenitis**, which often involves anaerobic bacteria.
- **Clindamycin** is an appropriate empiric antibiotic choice as it targets both Group A Streptococcus (a common cause of tonsillitis) and many anaerobic bacteria commonly found in head and neck infections, making it effective for peritonsillar cellulitis or early abscess formation.
*Incision and drainage*
- This procedure is indicated for a **fluctuant abscess**, which is a collection of pus that can be felt as a soft, compressible mass.
- The patient's lymph node is described as **nonfluctuant**, indicating that a mature, drainable abscess has not yet formed.
*Sulfadiazine and pyrimethamine therapy*
- This combination is the primary treatment for **toxoplasmosis**, a parasitic infection.
- The clinical picture of acute tonsillitis, cervical lymphadenitis, and exudates is not typical for uncomplicated toxoplasmosis.
*Immunoglobulin therapy*
- **Intravenous immunoglobulin (IVIG)** is typically used for conditions like Kawasaki disease, certain immunodeficiencies, or severe autoimmune disorders.
- There is no indication for IVIG in this patient's clinical presentation, which points towards an acute bacterial infection.
*Fine-needle aspiration biopsy*
- This is primarily a **diagnostic procedure** to obtain tissue for cytologic examination, often used to evaluate suspicious masses for malignancy or specific infections like tuberculosis.
- Given the acute inflammatory signs and symptoms, empiric antibiotic therapy is more appropriate as an initial step, rather than an immediate biopsy.
Thoracic fascial planes US Medical PG Question 9: A 55-year-old man visits the clinic with his wife. He has had difficulty swallowing solid foods for the past 2 months. His wife adds that his voice is getting hoarse but they thought it was due to his recent flu. His medical history is significant for type 2 diabetes mellitus for which he is on metformin. He suffered from many childhood diseases due to lack of medical care and poverty. His blood pressure is 125/87 mm Hg, pulse 95/min, respiratory rate 14/min, and temperature 37.1°C (98.7°F). On examination, an opening snap is heard over the cardiac apex. An echocardiogram shows an enlarged cardiac chamber pressing into his esophagus. Changes in which of the following structures is most likely responsible for this patient’s symptoms?
- A. Patent ductus arteriosus
- B. Right ventricle
- C. Left ventricle
- D. Left atrium (Correct Answer)
- E. Right atrium
Thoracic fascial planes Explanation: ***Left atrium***
- The patient's symptoms of **dysphagia (difficulty swallowing)** and **hoarseness** suggest compression of anatomical structures by an enlarged cardiac chamber, which the echocardiogram confirms.
- An enlarged **left atrium**, typically due to **mitral stenosis**, can compress the esophagus (leading to dysphagia) and the **recurrent laryngeal nerve** (leading to hoarseness, known as Ortner's syndrome). The **opening snap** at the apex is also highly characteristic of mitral stenosis.
*Patent ductus arteriosus*
- A **patent ductus arteriosus (PDA)** is a congenital heart defect that typically causes a **continuous murmur** and may lead to pulmonary hypertension or heart failure, but not direct compression of the esophagus or recurrent laryngeal nerve.
- The symptoms of PDA are usually present earlier in life, though uncorrected large PDAs can cause symptoms in adulthood, they do not cause dysphagia or hoarseness through direct esophageal compression.
*Right ventricle*
- An enlarged **right ventricle** usually causes symptoms related to right heart failure like **peripheral edema** or **dyspnea** due to pulmonary hypertension.
- It is not anatomically positioned to compress the esophagus or recurrent laryngeal nerve in a way that would cause dysphagia or hoarseness.
*Left ventricle*
- An enlarged **left ventricle** (e.g., due to hypertension or aortic stenosis) primarily causes symptoms like **dyspnea on exertion** or **angina**.
- While a severely dilated left ventricle can displace other structures, it does not typically cause direct esophageal compression leading to dysphagia or recurrent laryngeal nerve compression leading to hoarseness.
*Right atrium*
- An enlarged **right atrium** might be seen in conditions like tricuspid regurgitation or right heart failure but can manifest as **edema** or **jugular venous distention**.
- It is not anatomically positioned to cause dysphagia or hoarseness from esophageal or recurrent laryngeal nerve compression.
Thoracic fascial planes US Medical PG Question 10: A 45-year-old woman comes to the physician because of progressive difficulty swallowing solids and liquids over the past 4 months. She has lost 4 kg (9 lb) during this period. There is no history of serious illness. She emigrated to the US from Panama 7 years ago. She does not smoke cigarettes or drink alcohol. Cardiopulmonary examination shows a systolic murmur and an S3 gallop. A barium radiograph of the chest is shown. Histopathologic examination of the esophageal wall is most likely to show which of the following?
- A. Presence of intranuclear basophilic inclusions
- B. Atrophy of esophageal smooth muscle cells
- C. Infiltration of eosinophils in the epithelium
- D. Presence of metaplastic columnar epithelium
- E. Absence of myenteric plexus neurons (Correct Answer)
Thoracic fascial planes Explanation: ***Absence of myenteric plexus neurons***
- This finding is pathognomonic for **Chagas disease** (American trypanosomiasis), caused by *Trypanosoma cruzi*, endemic to Central and South America including Panama.
- The parasite destroys the **myenteric (Auerbach's) plexus neurons** in the esophageal wall, disrupting normal peristalsis and leading to **megaesophagus**.
- This results in **progressive dysphagia for both solids and liquids** and weight loss, as seen in this patient.
- The **cardiac findings** (systolic murmur and S3 gallop) indicate associated **chagasic cardiomyopathy**, another manifestation of chronic Chagas disease.
*Presence of intranuclear basophilic inclusions*
- Suggestive of **cytomegalovirus (CMV) esophagitis**, typically seen in immunocompromised patients (HIV/AIDS, transplant recipients).
- This patient has no immunocompromised state, and CMV does not cause the cardiac manifestations or chronic megaesophagus seen here.
*Atrophy of esophageal smooth muscle cells*
- Not characteristic of Chagas disease or achalasia; these conditions typically show **smooth muscle hypertrophy** due to chronic obstruction.
- Muscle atrophy would not explain the dysphagia, megaesophagus, or cardiac findings.
*Infiltration of eosinophils in the epithelium*
- Indicates **eosinophilic esophagitis**, an allergic condition usually presenting with food impaction and dysphagia mainly for solids.
- Would not explain the cardiac manifestations or the epidemiological connection to Panama.
*Presence of metaplastic columnar epithelium*
- Represents **Barrett's esophagus**, a complication of chronic gastroesophageal reflux disease (GERD).
- The patient's presentation with dysphagia for both solids and liquids, cardiac disease, and megaesophagus on barium study points to a **motility disorder** (Chagas disease), not reflux disease.
More Thoracic fascial planes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.