Surgical approaches to fascial compartments US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Surgical approaches to fascial compartments. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Surgical approaches to fascial compartments US Medical PG Question 1: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Surgical approaches to fascial compartments Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
Surgical approaches to fascial compartments US Medical PG Question 2: A 31-year-old man presents to the Emergency Department with severe left leg pain and paresthesias 4 hours after his leg got trapped by the closing door of a bus. Initially, he had a mild pain which gradually increased to unbearable levels. Past medical history is noncontributory. In the Emergency Department, his blood pressure is 130/80 mm Hg, heart rate is 87/min, respiratory rate is 14/min, and temperature is 36.8℃ (98.2℉). On physical exam, his left calf is firm and severely tender on palpation. The patient cannot actively dorsiflex his left foot, and passive dorsiflexion is limited. Posterior tibial and dorsalis pedis pulses are 2+ in the right leg and 1+ in the left leg. Axial load does not increase the pain. Which of the following is the best next step in the management of this patient?
- A. Lower limb CT scan
- B. Lower limb ultrasound
- C. Splinting and limb rest
- D. Fasciotomy (Correct Answer)
- E. Lower limb X-ray in two projections
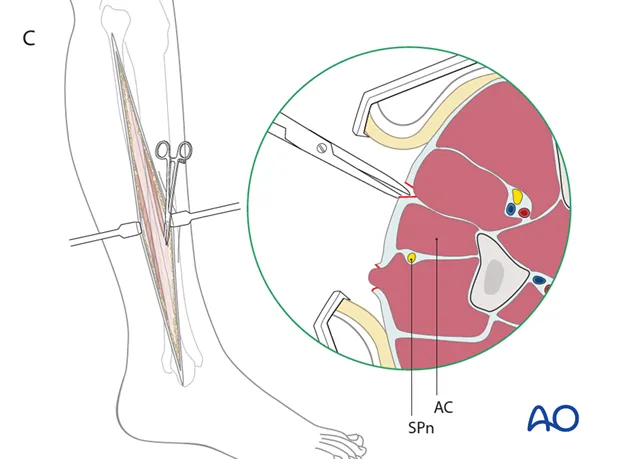
Surgical approaches to fascial compartments Explanation: ***Fasciotomy***
- The patient presents with classic signs and symptoms of **acute compartment syndrome**, including unrelieved pain by analgesics, paresthesias, pain with passive stretching, and a tense compartment due to the bus door trauma.
- **Fasciotomy** is the definitive and urgent treatment to relieve pressure within the muscle compartments, prevent muscle ischemia, and avoid permanent nerve damage or limb loss.
*Lower limb CT scan*
- A **CT scan** is primarily used to evaluate bony structures and soft tissue injuries but is not the most immediate or definitive diagnostic tool for acute compartment syndrome.
- Delaying **fasciotomy** for imaging in a clear case of compartment syndrome can lead to irreversible damage.
*Lower limb ultrasound*
- **Ultrasound** can assess vascular flow and some soft tissue aspects but is not accurate or rapid enough for diagnosing compartment syndrome.
- It would not provide the necessary information to guide urgent surgical intervention.
*Splinting and limb rest*
- This approach is appropriate for fractures or soft tissue injuries without compartment syndrome; however, in acute compartment syndrome, **splinting or limb rest** will worsen the condition.
- **Immobilization** and elevation are contraindicated as they can further decrease blood flow and increase compartment pressure.
*Lower limb X-ray in two projections*
- An **X-ray** is useful for ruling out fractures but will not provide information about compartment pressure or muscle viability.
- While a fracture can sometimes cause compartment syndrome, the immediate concern here is the compartment syndrome itself, for which **X-rays** are not diagnostic.
Surgical approaches to fascial compartments US Medical PG Question 3: A 72-year-old male presents to a cardiac surgeon for evaluation of severe aortic stenosis. He has experienced worsening dyspnea with exertion over the past year. The patient also has a history of poorly controlled hypertension, diabetes mellitus, and hyperlipidemia. An echocardiogram revealed a thickened calcified aortic valve. The surgeon is worried that the patient will be a poor candidate for open heart surgery and decides to perform a less invasive transcatheter aortic valve replacement. In order to perform this procedure, the surgeon must first identify the femoral pulse just inferior to the inguinal ligament and insert a catheter into the vessel in order to gain access to the arterial system. Which of the following structures is immediately lateral to this structure?
- A. Lymphatic vessels
- B. Femoral vein
- C. Sartorius muscle
- D. Pectineus muscle
- E. Femoral nerve (Correct Answer)
Surgical approaches to fascial compartments Explanation: ***Femoral nerve***
- The **femoral nerve** lies lateral to the **femoral artery** within the **femoral triangle**.
- The order of structures from **lateral to medial** under the inguinal ligament is remembered by the mnemonic **NAVEL**: **N**erve, **A**rtery, **V**ein, **E**mpty space, **L**ymphatics.
*Lymphatic vessels*
- **Lymphatic vessels** and nodes are located most medially within the femoral triangle, medial to the femoral vein.
- This position is not immediately lateral to the femoral artery.
*Femoral vein*
- The **femoral vein** is located immediately medial to the **femoral artery**.
- It would not be found immediately lateral to the femoral artery.
*Sartorius muscle*
- The **sartorius muscle** forms the lateral boundary of the **femoral triangle** but is not immediately adjacent and lateral to the femoral artery within the triangle itself.
- The femoral nerve is enclosed within the iliopsoas fascial compartment, which runs deep to the sartorius.
*Pectineus muscle*
- The **pectineus muscle** forms part of the floor of the **femoral triangle**, but it is deep to the neurovascular structures.
- It is not immediately lateral to the femoral artery.
Surgical approaches to fascial compartments US Medical PG Question 4: A 48-year-old male presents to his primary care provider with a two-week history of low back pain and left leg pain. He reports that his symptoms started while he was working at his job as a construction worker. He has since experienced intermittent achy pain over his lumbar spine. He has also noticed pain radiating into his left leg and weakness in left ankle dorsiflexion. On exam, he demonstrates the following findings on strength testing of the left leg: 5/5 in knee extension, 4/5 in ankle dorsiflexion, 4/5 in great toe extension, 5/5 in ankle plantarflexion, and 5/5 in great toe flexion. The patellar reflexes are 5/5 bilaterally. He is able to toe walk but has difficulty with heel walking. Weakness in which of the following compartments of the leg is most likely causing this patient’s foot drop?
- A. Lateral compartment
- B. Superficial posterior compartment
- C. Deep posterior compartment
- D. Anterior compartment (Correct Answer)
- E. Medial compartment
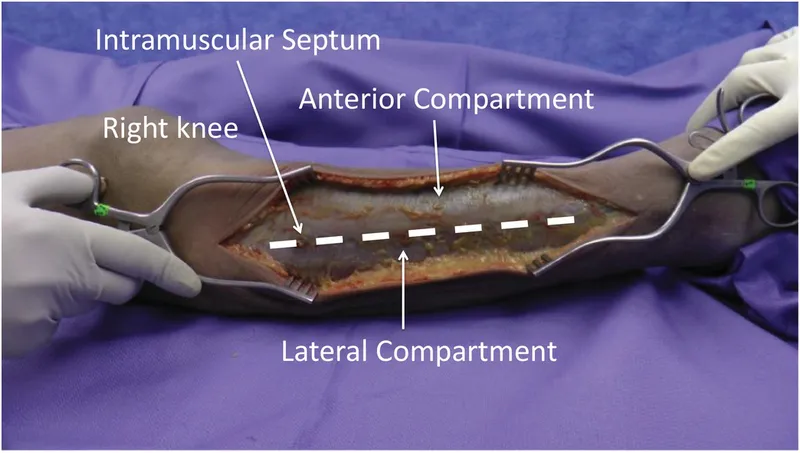
Surgical approaches to fascial compartments Explanation: ***Anterior compartment***
- Weakness in **ankle dorsiflexion** and **great toe extension**, coupled with difficulty **heel walking**, indicates a foot drop due to dysfunction of muscles in the anterior compartment, such as the **tibialis anterior**, **extensor hallucis longus**, and **extensor digitorum longus**.
- These muscles are primarily innervated by the **deep fibular nerve**, which is susceptible to compression from conditions like **lumbar radiculopathy** (L4-L5 nerve root involvement).
*Lateral compartment*
- Muscles in the lateral compartment (**fibularis longus** and **brevis**) are responsible for **eversion** of the foot.
- Weakness in this compartment would manifest as difficulty everting the foot, not primarily ankle dorsiflexion or great toe extension deficits.
*Superficial posterior compartment*
- This compartment contains muscles like the **gastrocnemius** and **soleus**, which are primarily responsible for **ankle plantarflexion**.
- The patient exhibits 5/5 strength in ankle plantarflexion and is able to toe walk, indicating these muscles are functioning well.
*Deep posterior compartment*
- Muscles in the deep posterior compartment (**tibialis posterior**, **flexor digitorum longus**, **flexor hallucis longus**) are involved in **inversion** and **toe flexion**.
- The patient has 5/5 strength in great toe flexion, suggesting intact function of these muscles, and his primary deficit is in dorsiflexion.
*Medial compartment*
- There is no distinct "medial compartment" of the leg in the anatomical sense comparable to the other listed compartments; rather, various muscles contribute to medial actions.
- The symptoms described specifically point to weakness in dorsiflexion and toe extension, localizing the problem to the anterior compartment.
Surgical approaches to fascial compartments US Medical PG Question 5: A 65-year-old man is referred by his primary care provider to a neurologist for leg pain. He reports a 6-month history of progressive bilateral lower extremity pain that is worse in his left leg. The pain is 5/10 in severity at its worst and is described as a "burning" pain. He has noticed that the pain is acutely worse when he walks downhill. He has started riding his stationary bike more often as it relieves his pain. His past medical history is notable for hypertension, diabetes mellitus, and a prior myocardial infarction. He also sustained a distal radius fracture the previous year after falling on his outstretched hand. He takes aspirin, atorvastatin, metformin, glyburide, enalapril, and metoprolol. He has a 30-pack-year smoking history and drinks 2-3 glasses of wine with dinner every night. His temperature is 99°F (37.2°C), blood pressure is 145/85 mmHg, pulse is 91/min, and respirations are 18/min. On exam, he is well-appearing and in no acute distress. A straight leg raise is negative. A valsalva maneuver does not worsen his pain. Which of the following is the most appropriate test to confirm this patient's diagnosis?
- A. Electromyography
- B. Ankle-brachial index
- C. Computerized tomography myelography
- D. Magnetic resonance imaging (Correct Answer)
- E. Radiography
Surgical approaches to fascial compartments Explanation: **Magnetic resonance imaging**
- **Magnetic resonance imaging (MRI)** is the most appropriate test for diagnosing **lumbar spinal stenosis** because it provides detailed imaging of soft tissues, including the **spinal cord, nerve roots, and intervertebral discs**.
- The patient's symptoms of bilateral lower extremity pain, worse with downhill walking and relieved by stationary biking (which typically involves a flexed spine), are classic for **neurogenic claudication** caused by spinal stenosis.
*Electromyography*
- **Electromyography (EMG)** measures electrical activity of muscles and can identify **radiculopathy** or **neuropathy** but does not directly visualize the spinal canal or its contents to diagnose the cause of nerve compression.
- While it could show nerve root involvement, it wouldn't be the primary diagnostic test to confirm **spinal stenosis** itself.
*Ankle-brachial index*
- The **ankle-brachial index (ABI)** is used to diagnose **peripheral artery disease (PAD)**, which can also cause leg pain with activity (**vascular claudication**).
- However, the patient's pain being worse with downhill walking and relieved by spine flexion (like on a stationary bike) is more consistent with **neurogenic claudication** than vascular claudication.
*Computerized tomography myelography*
- **CT myelography** involves injecting contrast into the spinal canal and then performing a CT scan. While it can visualize the spinal canal, it is more invasive than MRI and exposes the patient to **ionizing radiation**.
- It is typically reserved for cases where MRI is contraindicated (e.g., pacemakers) or when MRI findings are inconclusive.
*Radiography*
- **Radiography (X-rays)** can show bony changes such as **spondylosis** and **degenerative disc disease**, which are often associated with spinal stenosis.
- However, X-rays do not directly visualize the **spinal cord, nerve roots, or soft tissue compression**, making them inadequate for confirming spinal stenosis as the cause of neurogenic claudication.
Surgical approaches to fascial compartments US Medical PG Question 6: A 35-year-old woman presents with progressive vision loss and severe headache. MRI shows cavernous sinus thrombosis with extension into the superior ophthalmic vein. Blood cultures grow Staphylococcus aureus. History reveals she had squeezed a facial pustule near her upper lip 5 days prior. Evaluate the anatomical explanation and risk stratification for this complication.
- A. Direct lymphatic spread from facial infection due to rich subcutaneous lymphatic network
- B. Valveless facial venous system allowing retrograde flow from danger triangle to cavernous sinus (Correct Answer)
- C. Contiguous spread through cribriform plate from nasal cavity involvement
- D. Hematogenous seeding via internal jugular vein and sigmoid sinus
- E. Extension through pterygoid venous plexus communicating with middle meningeal vein
Surgical approaches to fascial compartments Explanation: ***Valveless facial venous system allowing retrograde flow from danger triangle to cavernous sinus***
- The **danger triangle of the face** (perioral and nasal areas) contains **valveless veins**, which allows blood to flow in a **retrograde** direction toward the intracranial space.
- Infections in this region can spread via the **angular vein** into the **superior ophthalmic vein**, directly reaching the **cavernous sinus** and causing septic thrombosis.
*Direct lymphatic spread from facial infection due to rich subcutaneous lymphatic network*
- While the face has a rich **lymphatic network**, lymphatic drainage typically leads to **submandibular or cervical lymph nodes**, not the cavernous sinus.
- Cavernous sinus thrombosis is a **vascular complication** specifically involving the **venous system**, not the lymphatic system.
*Contiguous spread through cribriform plate from nasal cavity involvement*
- The **cribriform plate** is a route for infections to enter the **subarachnoid space**, primarily leading to **meningitis** or brain abscesses.
- It does not serve as the primary anatomical conduit for superficial facial infections to localize within the **cavernous sinus**.
*Hematogenous seeding via internal jugular vein and sigmoid sinus*
- The **internal jugular vein** and **sigmoid sinus** represent the **outflow tract** away from the brain; flow to the cavernous sinus through this route would be highly atypical.
- Bacterial seeding via this route would usually imply **systemic bacteremia** or infection in the **mastoid air cells**, rather than a localized facial pustule.
*Extension through pterygoid venous plexus communicating with middle meningeal vein*
- The **pterygoid venous plexus** can communicate with the cavernous sinus, but it primarily drains the **infratemporal fossa** and deep face, not the superficial upper lip.
- The **middle meningeal vein** drains into the pterygoid plexus or sphenoparietal sinus and is not the classic path for **danger triangle** infections.
Surgical approaches to fascial compartments US Medical PG Question 7: A 52-year-old diabetic man undergoes emergent fasciotomy for compartment syndrome of the right leg following a tibia-fibula fracture. Intraoperatively, the anterior compartment muscles appear dusky and do not contract with stimulation. The lateral compartment muscles appear viable. Deep posterior compartment shows borderline viability with weak contraction. Superficial posterior compartment is clearly viable. Synthesize a management plan that optimizes limb salvage while minimizing morbidity.
- A. Debride anterior compartment only, leave wounds open, second look in 48 hours for other compartments
- B. Debride all nonviable muscle, preserve borderline tissue, second look in 24 hours (Correct Answer)
- C. Complete debridement of anterior and deep posterior compartments with immediate wound closure
- D. Below-knee amputation given extent of muscle necrosis and diabetes
- E. Hyperbaric oxygen therapy for 48 hours before deciding on debridement versus amputation
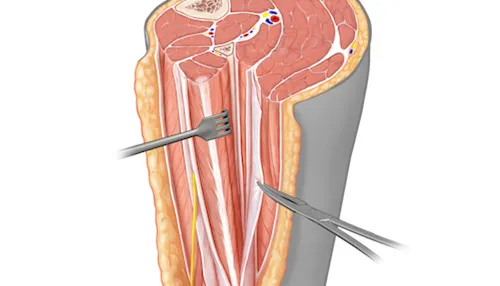
Surgical approaches to fascial compartments Explanation: ***Debride all nonviable muscle, preserve borderline tissue, second look in 24 hours***
- Immediate **debridement** of non-contractile, dusky muscle is crucial to prevent **myoglobinuria**, metabolic acidosis, and **acute kidney injury**.
- Marginal tissue should be preserved during the initial surgery to maximize potential **limb salvage**, necessitating a **mandatory second-look** procedure within 24-48 hours.
*Debride anterior compartment only, leave wounds open, second look in 48 hours for other compartments*
- Leaving known nonviable muscle in the anterior compartment for 48 hours increases the risk of **secondary infection** and systemic inflammatory response syndrome.
- Re-exploration should be performed sooner (24 hours) when multiple compartments show **borderline viability** to ensure timely intervention.
*Complete debridement of anterior and deep posterior compartments with immediate wound closure*
- **Immediate wound closure** is strictly contraindicated in compartment syndrome as it can cause a recurrence of increased pressure and facilitates **anaerobic infection**.
- Over-debridement of the **deep posterior compartment** before its viability is definitively determined could result in unnecessary loss of **plantarflexion** and sensation.
*Below-knee amputation given extent of muscle necrosis and diabetes*
- **Amputation** is premature as the lateral and superficial posterior compartments are viable, providing a foundation for a **functional limb**.
- While **diabetes** may complicate healing, it is not an absolute indication for primary amputation in the setting of salvageable muscle groups.
*Hyperbaric oxygen therapy for 48 hours before deciding on debridement versus amputation*
- Delaying surgical **debridement** of necrotic tissue to pursue **HBO therapy** is dangerous and allows for the progression of sepsis and muscle breakdown.
- HBO therapy is an **adjunct**, not a replacement for mechanical decompression and removal of dead tissue in **acute compartment syndrome**.
Surgical approaches to fascial compartments US Medical PG Question 8: A 29-year-old man sustains a gunshot wound to the medial upper arm. He presents with inability to flex his elbow and loss of sensation over the lateral forearm. Angiography shows intact brachial artery, but compartment pressures in the anterior arm compartment are 55 mmHg. His blood pressure is 90/60 mmHg after resuscitation. Evaluate the optimal surgical approach considering all clinical factors.
- A. Immediate fasciotomy of anterior compartment with nerve exploration and vascular repair
- B. Fasciotomy of both anterior and posterior compartments with primary nerve repair
- C. Further resuscitation to MAP >65, then fasciotomy with delayed nerve repair
- D. Emergent fasciotomy, debridement, and temporary vascular shunt placement
- E. Complete neurovascular exploration with definitive repair and compartment release (Correct Answer)
Surgical approaches to fascial compartments Explanation: ***Complete neurovascular exploration with definitive repair and compartment release***
- The patient exhibits clinical and objective signs of **acute compartment syndrome** (pressure 55 mmHg) and **musculocutaneous nerve** injury, requiring emergency surgical intervention.
- A total assessment is necessary because the **gunshot wound** trajectory near the medial arm risks occult damage to the **neurovascular bundle** despite initial angiographic findings.
*Immediate fasciotomy of anterior compartment with nerve exploration and vascular repair*
- While an anterior fasciotomy is vital, focusing solely on the anterior compartment may be insufficient if the high-energy trauma caused **posterior compartment** injury.
- **Vascular repair** is not indicated at this stage as angiography has already confirmed the **brachial artery** is intact.
*Fasciotomy of both anterior and posterior compartments with primary nerve repair*
- Primary nerve repair is often contraindicated in **high-velocity gunshot wounds** due to the "zone of injury" and potential for further tissue debridement needs.
- While dual-compartment release is thorough, the emphasis on **primary repair** in an unstable, potentially contaminated trauma setting is surgically premature.
*Further resuscitation to MAP >65, then fasciotomy with delayed nerve repair*
- While hemodynamic stability is important, the **Delta pressure** (60 - 55 = 5 mmHg) is critically low, meaning any delay in fasciotomy will lead to **muscle necrosis**.
- Resuscitation should occur **concurrently** with surgical preparation rather than as a prerequisite that delays limb-saving decompression.
*Emergent fasciotomy, debridement, and temporary vascular shunt placement*
- The use of a **temporary vascular shunt** is reserved for patients with confirmed arterial transection to maintain distal perfusion during damage control.
- Since the **brachial artery** is intact per angiography, shunting is unnecessary and adds pointless risk and operative time.
Surgical approaches to fascial compartments US Medical PG Question 9: A 67-year-old man develops severe abdominal pain 3 days after elective sigmoid colectomy. CT shows fluid tracking along the left psoas muscle and into the left thigh anterior compartment. No bowel perforation is identified, but there is concern for an anastomotic leak. Analyze the fascial anatomy to determine the most likely pathway of fluid spread from the retroperitoneum to the thigh.
- A. Direct extension through the inguinal canal following the spermatic cord
- B. Tracking along psoas muscle through femoral triangle via femoral sheath
- C. Spread through obturator foramen along obturator neurovascular bundle
- D. Extension along iliacus fascia through muscular lacuna beneath inguinal ligament (Correct Answer)
- E. Dissection through transversalis fascia into preperitoneal space and anterior abdominal wall
Surgical approaches to fascial compartments Explanation: ***Extension along iliacus fascia through muscular lacuna beneath inguinal ligament***
- The **iliacus fascia** and **psoas fascia** create a continuous sheath that provides a direct anatomical pathway for retroperitoneal fluid to descend into the **anterior thigh**.
- This fluid collection passes deep to the **inguinal ligament** via the **muscular lacuna**, which contains the **psoas major**, **iliacus**, and the **femoral nerve**.
*Direct extension through the inguinal canal following the spermatic cord*
- The **inguinal canal** is an oblique passage in the **anterior abdominal wall**, not a primary conduit for **retroperitoneal** fluid tracking from the psoas muscle.
- Fluid in this canal would typically lead to **scrotal swelling** or a mass in the **inguinal region** rather than tracking into the anterior thigh compartment.
*Tracking along psoas muscle through femoral triangle via femoral sheath*
- The **femoral sheath** is an extension of the **transversalis** and **iliac fasciae** that surrounds the femoral vessels, but it is distinct from the muscular compartment containing the psoas.
- While the psoas muscle enters the **femoral triangle**, the sheath primarily contains the **femoral artery, vein, and canal**, not the muscle itself.
*Spread through obturator foramen along obturator neurovascular bundle*
- The **obturator foramen** serves as a pathway for structures to move from the **lesser pelvis** into the **medial (adductor) compartment** of the thigh.
- Fluid tracking here would be located more medially and would not typically track from the high **retroperitoneal psoas region** into the anterior compartment.
*Dissection through transversalis fascia into preperitoneal space and anterior abdominal wall*
- The **transversalis fascia** provides a barrier between the abdominal muscles and the **peritoneum**; fluid tracking here would stay in the **anterior abdominal wall**.
- This pathway does not provide a direct descent into the **thigh** and would not explain fluid tracking specifically along the **psoas muscle**.
Surgical approaches to fascial compartments US Medical PG Question 10: A 42-year-old injection drug user presents with fever, dysphagia, and neck swelling. CT shows a multiloculated abscess in the retropharyngeal space with air-fluid levels extending into the posterior mediastinum to the level of T6. Despite the inferior extent, the abscess has not spread to the anterior mediastinum. Analyze the fascial anatomy to explain this pattern of spread.
- A. The danger space between alar and prevertebral fascia allows posterior but not anterior spread (Correct Answer)
- B. The buccopharyngeal fascia extends to diaphragm blocking anterior spread
- C. The prevertebral fascia prevents anterior spread into mediastinum
- D. The alar fascia fuses with the pericardium preventing anterior extension
- E. The investing layer of deep cervical fascia diverts infection posteriorly
Surgical approaches to fascial compartments Explanation: ***The danger space between alar and prevertebral fascia allows posterior but not anterior spread***
- The **danger space** is a potential space located between the **alar fascia** anteriorly and the **prevertebral fascia** posteriorly, providing a low-resistance pathway for infection to spread from the skull base to the **diaphragm**.
- Because this space is positioned behind the **visceral compartments** and is bounded by the fusion of fascial layers laterally, it anatomically directs the descent of a **retropharyngeal abscess** into the **posterior mediastinum** while isolating it from the anterior mediastinum.
*The prevertebral fascia prevents anterior spread into mediastinum*
- The **prevertebral fascia** forms the posterior boundary of the danger space; while it prevents spread into the **vertebral bodies**, it does not explain why the infection is restricted from the **anterior mediastinum**.
- This fascia continues down to the **coccyx**, meaning it helps facilitate deep vertical spread rather than serving as a transverse barrier to anterior compartments.
*The alar fascia fuses with the pericardium preventing anterior extension*
- The **alar fascia** actually ends and fuses with the **buccopharyngeal fascia** at the level of **T2**; it does not extend further to fuse with the **pericardium**.
- The **pretracheal fascia** is the layer that blends with the fibrous pericardium, and it is located much more anteriorly in the neck.
*The buccopharyngeal fascia extends to diaphragm blocking anterior spread*
- The **buccopharyngeal fascia** (the posterior part of the visceral fascia) only extends inferiorly to the level of the **superior mediastinum** (around T2-T4) where it blends with the esophagus.
- It forms the anterior wall of the **retropharyngeal space** and cannot block spread to the diaphragm as it does not reach that far inferiorly.
*The investing layer of deep cervical fascia diverts infection posteriorly*
- The **investing fascia** is the most superficial layer of deep cervical fascia, surrounding the **sternocleidomastoid** and trapezius muscles.
- It typically limits spread to the **anterior or posterior triangles** of the neck and does not communicate with the deep **retropharyngeal** or **danger spaces** involved in mediastinitis.
More Surgical approaches to fascial compartments US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.