Principles of fascial spaces US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Principles of fascial spaces. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Principles of fascial spaces US Medical PG Question 1: A patient presents with difficulty extending their wrist following trauma to the posterior forearm. Which of the following muscles would be most affected by injury to the posterior interosseous nerve?
- A. Extensor carpi ulnaris
- B. Extensor carpi radialis brevis
- C. Extensor pollicis longus
- D. Extensor digitorum (Correct Answer)
Principles of fascial spaces Explanation: ***Extensor digitorum***
- The **posterior interosseous nerve (PIN)** innervates most muscles of the **posterior compartment of the forearm**, including the extensor digitorum. [1]
- Loss of function in the **extensor digitorum** would directly impair **extension of the fingers** and contribute significantly to difficulty extending the wrist. [1]
*Extensor carpi ulnaris*
- This muscle is also innervated by the **posterior interosseous nerve (PIN)** and contributes to **wrist extension** and **ulnar deviation**.
- While its innervation by the PIN is correct, injury to the PIN would affect this muscle, but the *extensor digitorum* is more broadly responsible for the stated primary symptom (difficulty extending the wrist), as its primary action is finger and thus wrist extension.
*Extensor carpi radialis brevis*
- While it is a **wrist extensor**, it is innervated by the **deep branch of the radial nerve** *before* it becomes the posterior interosseous nerve.
- Therefore, an isolated injury to the **posterior interosseous nerve** proper would typically spare the extensor carpi radialis brevis.
*Extensor pollicis longus*
- This muscle is indeed innervated by the **posterior interosseous nerve (PIN)** and acts to extend the **thumb**. [1]
- While it would be affected, the primary problem described is difficulty extending the *wrist*, for which the extensor digitorum plays a more significant and general role than the extensor pollicis longus.
Principles of fascial spaces US Medical PG Question 2: A 62-year-old man presents to the emergency department with sudden onset of severe left leg pain accompanied by numbness and weakness. His medical history is remarkable for hypertension and hyperlipidemia. His vital signs include a blood pressure of 155/92 mm Hg, a temperature of 37.1°C (98.7°F), and an irregular pulse of 92/min. Physical examination reveals absent left popliteal and posterior tibial pulses. His left leg is noticeably cold and pale. There is no significant tissue compromise, nerve damage, or sensory loss. Which of the following will most likely be required for this patient's condition?
- A. Antibiotics
- B. Warfarin
- C. Fasciotomy
- D. Amputation
- E. Thromboembolectomy (Correct Answer)
Principles of fascial spaces Explanation: ***Thromboembolectomy***
- The sudden onset of severe leg pain, numbness, and weakness with absent pulses, a cold, pale limb, and an irregular pulse suggests **acute limb ischemia** likely due to an **arterial embolus**, which requires emergent surgical removal.
- Given the symptoms and history of an irregular pulse (suggesting possible atrial fibrillation), a thromboembolectomy is the most appropriate first-line treatment to restore blood flow and prevent permanent damage.
*Antibiotics*
- Antibiotics are used to treat **bacterial infections** and are not indicated for acute limb ischemia caused by a vascular occlusion.
- There are no signs of infection present, such as fever, redness, or purulent discharge, that would warrant antibiotic therapy.
*Warfarin*
- Warfarin is an **anticoagulant** used for long-term prevention of clot formation, particularly in conditions like atrial fibrillation or deep vein thrombosis.
- While anticoagulation may eventually be part of management to prevent future events, it is insufficient as immediate therapy for an acute, established arterial embolus causing critical limb ischemia.
*Fasciotomy*
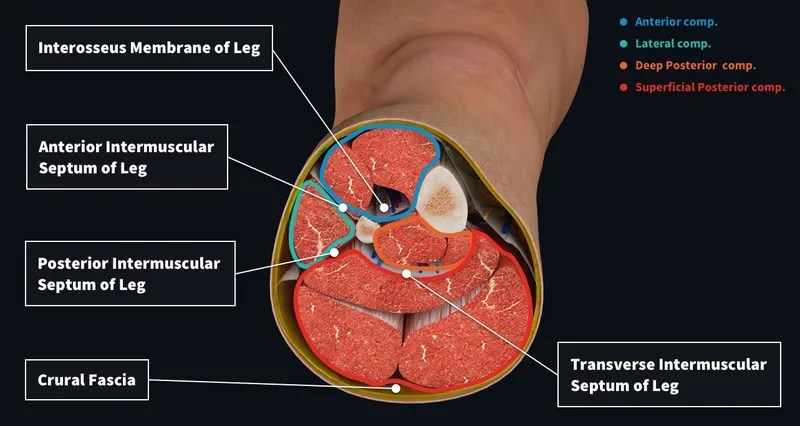
- Fasciotomy is performed to relieve **compartment syndrome**, which occurs when increased pressure within a muscle compartment compromises circulation and nerve function.
- While compartment syndrome can be a complication of reperfusion after prolonged ischemia, it is not the primary treatment for the initial arterial occlusion; the first step is to restore blood flow to prevent the need for it.
*Amputation*
- Amputation is a last resort considered when the limb is **irreversibly ischemic** and non-viable, or when revascularization attempts have failed and there is extensive tissue necrosis or infection.
- In this case, there is no significant tissue compromise or nerve damage mentioned, indicating that the limb is still salvageable with timely intervention.
Principles of fascial spaces US Medical PG Question 3: A 35-year-old man is brought to the emergency department from a kitchen fire. The patient was cooking when boiling oil splashed on his exposed skin. His temperature is 99.7°F (37.6°C), blood pressure is 127/82 mmHg, pulse is 120/min, respirations are 12/min, and oxygen saturation is 98% on room air. He has dry, nontender, and circumferential burns over his arms bilaterally, burns over the anterior portion of his chest and abdomen, and tender spot burns with blisters on his shins. A 1L bolus of normal saline is administered and the patient is given morphine and his pulse is subsequently 80/min. A Foley catheter is placed which drains 10 mL of urine. What is the best next step in management?
- A. Additional fluids and escharotomy (Correct Answer)
- B. Escharotomy
- C. Continuous observation
- D. Moist dressings and discharge
- E. Additional fluids and admission to the ICU
Principles of fascial spaces Explanation: ***Additional fluids and escharotomy***
- The patient has **circumferential full-thickness burns** on both arms (dry, nontender), which require **escharotomy** to prevent compartment syndrome and vascular compromise to the limbs.
- The **oliguria** (10 mL urine output) despite a 1L fluid bolus indicates **inadequate fluid resuscitation** from burn shock. With approximately 40% TBSA burns, the patient requires aggressive fluid resuscitation per the Parkland formula (4 mL/kg/% TBSA), which would be approximately 11 liters in the first 24 hours. Adequate resuscitation targets urine output of 0.5-1 mL/kg/hr (35-70 mL/hr for this patient).
- Both interventions are immediately necessary: fluids for burn shock and escharotomy for circumferential burns.
*Escharotomy*
- While **escharotomy** is essential for the circumferential full-thickness burns to prevent compartment syndrome, it alone will not address the **severe fluid deficit** causing oliguria and hypoperfusion.
- The low urine output reflects systemic hypovolemia from burn shock, not just local compartment issues, requiring aggressive fluid resuscitation.
*Continuous observation*
- **Continuous observation** is inappropriate given the patient's critical findings: circumferential full-thickness burns requiring urgent escharotomy and oliguria indicating inadequate resuscitation.
- Delaying escharotomy can lead to irreversible ischemic damage to the limbs, and inadequate fluid resuscitation can progress to multiorgan failure.
*Moist dressings and discharge*
- This option is completely inappropriate for a patient with **extensive deep burns** (approximately 40% TBSA) including full-thickness injuries requiring hospitalization and specialized burn care.
- Discharge would lead to severe complications including infection, inadequate fluid resuscitation, compartment syndrome, and potential limb loss.
*Additional fluids and admission to the ICU*
- While ICU admission and additional fluids are necessary components of care, this option is **incomplete** because it omits **escharotomy**, which is urgently needed for the circumferential full-thickness burns.
- Escharotomy is a time-sensitive procedure that must be performed promptly to prevent ischemic injury to the limbs from vascular compromise.
Principles of fascial spaces US Medical PG Question 4: A 23-year-old patient presents to the emergency department after a motor vehicle accident. The patient was an unrestrained driver involved in a head-on collision. The patient is heavily intoxicated on what he claims is only alcohol. An initial trauma assessment is performed, and is notable for significant bruising of the right forearm. The patient is in the trauma bay, and complains of severe pain in his right forearm. A physical exam is performed and is notable for pallor, decreased sensation, and cool temperature of the skin of the right forearm. Pain is elicited upon passive movement of the right forearm and digits. A thready radial pulse is palpable. A FAST exam is performed, and is negative for signs of internal bleeding. The patient's temperature is 99.5°F (37.5°C), pulse is 100/min, blood pressure is 110/70 mmHg, respirations are 12/min, and oxygen saturation is 98% on room air. Radiography of the right forearm is ordered. The patient is still heavily intoxicated. Which of the following is the best next step in management?
- A. Fasciotomy (Correct Answer)
- B. IV fluids
- C. Analgesics
- D. Pressure measurement
- E. Detoxification
Principles of fascial spaces Explanation: ***Fasciotomy***
- The patient exhibits classic signs of **acute compartment syndrome**, including severe pain out of proportion to injury, pain on passive stretch, pallor, decreased sensation, and cool extremity, despite a palpable pulse. These symptoms necessitate immediate surgical intervention to relieve pressure.
- A **fasciotomy** is the definitive treatment for acute compartment syndrome to prevent irreversible muscle and nerve damage, and potentially limb loss.
*IV fluids*
- While fluid resuscitation is important in trauma, the patient's current vital signs (BP 110/70 mmHg, pulse 100/min) do not indicate immediate shock requiring aggressive IV fluid administration over addressing the limb-threatening compartment syndrome.
- Prioritizing IV fluids without addressing **compartment syndrome** could lead to permanent loss of limb function.
*Analgesics*
- Administering analgesics might mask the escalating pain a key symptom of compartment syndrome, which could delay diagnosis and definitive treatment.
- While pain control is important, it should not supersede measures to prevent irreversible tissue damage.
*Pressure measurement*
- While compartment pressure measurement can confirm the diagnosis of compartment syndrome, the clinical presentation in this case is so compelling that delaying definitive treatment for pressure measurement is not the best next step.
- Clinical signs and symptoms are often sufficient for diagnosis, and surgical intervention should not be deferred pending pressure readings in clear-cut cases.
*Detoxification*
- Detoxification for alcohol intoxication is not an emergent and immediate priority in comparison to the limb-threatening condition of acute compartment syndrome.
- Addressing the **compartment syndrome** is critical for preserving limb viability, whereas detoxification can be managed once acute medical emergencies are controlled.
Principles of fascial spaces US Medical PG Question 5: In a patient with acute myocardial ischemia, which of the following cardiovascular structures is at greatest risk of damage?
- A. Pulmonary valve
- B. Cardiac conduction system (Correct Answer)
- C. Coronary artery
- D. Cardiac septum
- E. Temporal artery
Principles of fascial spaces Explanation: ***Cardiac conduction system***
- The **cardiac conduction system** is highly dependent on a constant oxygen supply, and its disruption by ischemia can lead to serious **arrhythmias** and **heart blocks**.
- Ischemia in critical areas like the **AV node** (supplied by the RCA) or the **bundle branches** can severely impair the heart's electrical activity.
*Pulmonary valve*
- The **pulmonary valve** is primarily a passive structure and is generally not directly damaged by acute myocardial ischemia.
- Its function is more affected by changes in **pulmonary artery pressure** or **ventricular remodeling**, not immediate ischemic injury.
*Coronary artery*
- While **coronary artery disease (CAD)** is the *cause* of myocardial ischemia, the coronary artery itself is not the structure *damaged* in the sense of functional impairment due to lack of blood flow in acute ischemia.
- The damage occurs downstream in the **myocardium** that the artery supplies.
*Cardiac septum*
- The **cardiac septum** can be damaged by myocardial ischemia, particularly the **interventricular septum**, leading to complications like **septal rupture**.
- However, the conduction system is at *greatest* immediate risk of functional damage leading to life-threatening events due to its critical role in rhythm generation.
*Temporal artery*
- The **temporal artery** is a blood vessel located in the head, entirely separate from the heart.
- It is not involved in myocardial ischemia and is not at risk of damage from a cardiac event.
Principles of fascial spaces US Medical PG Question 6: A 35-year-old man is referred to a physical therapist due to limitation of movement in the wrist and fingers of his left hand. He cannot hold objects or perform daily activities with his left hand. He broke his left arm at the humerus one month ago. The break was simple and treatment involved a cast for one month. Then he lost his health insurance and could not return for follow up. Only after removing the cast did he notice the movement issues in his left hand and wrist. His past medical history is otherwise insignificant, and vital signs are within normal limits. On examination, the patient’s left hand is pale and flexed in a claw-like position. It is firm and tender to palpation. Right radial pulse is 2+ and left radial pulse is 1+. The patient is unable to actively extend his fingers and wrist, and passive extension is difficult and painful. Which of the following is a proper treatment for the presented patient?
- A. Surgical release (Correct Answer)
- B. Botulinum toxin injections
- C. Collagenase injections
- D. Needle fasciotomy
- E. Corticosteroid injections
Principles of fascial spaces Explanation: ***Surgical release***
- The patient presents with classic signs of **established Volkmann's ischemic contracture** (claw-like hand, firm fibrotic tissue, limited movement, decreased radial pulse), which is the end-stage result of untreated compartment syndrome that occurred during fracture healing.
- Since this is **chronic contracture (one month post-injury)**, the appropriate surgical treatment involves **reconstructive procedures** such as muscle slide operations, tendon lengthening, tendon transfers, neurolysis, or in severe cases, free functional muscle transfer to restore hand function.
- Emergency fasciotomy would have been appropriate for **acute compartment syndrome** (within 6-8 hours of onset), but at this stage, the treatment focuses on releasing fibrotic tissue and restoring function through reconstructive surgery.
*Botulinum toxin injections*
- **Botulinum toxin** is used to relax spastic muscles in neurological conditions (e.g., cerebral palsy, stroke), but it does not address the underlying **ischemic fibrosis and muscle necrosis** of Volkmann's contracture.
- It would not improve the structural contracture or restore blood flow in this patient.
*Collagenase injections*
- **Collagenase injections** are used for localized fascial contractures like Dupuytren's contracture, where enzymatic breakdown of collagen cords can restore finger extension.
- They are ineffective for **Volkmann's contracture**, which involves widespread ischemic muscle necrosis, fibrosis, and nerve damage requiring surgical reconstruction.
*Needle fasciotomy*
- **Needle fasciotomy** is a minimally invasive technique for Dupuytren's contracture, involving percutaneous disruption of fascial cords.
- It is not suitable for **Volkmann's contracture**, which requires extensive surgical release of fibrotic muscle compartments, possible tendon transfers, and neurolysis—procedures that cannot be accomplished with needle techniques.
*Corticosteroid injections*
- **Corticosteroids** reduce inflammation in conditions like tenosynovitis or trigger finger.
- They would not address the **ischemic muscle necrosis and fibrotic contracture** in Volkmann's contracture and could potentially delay appropriate surgical treatment.
Principles of fascial spaces US Medical PG Question 7: A 31-year-old man presents to the Emergency Department with severe left leg pain and paresthesias 4 hours after his leg got trapped by the closing door of a bus. Initially, he had a mild pain which gradually increased to unbearable levels. Past medical history is noncontributory. In the Emergency Department, his blood pressure is 130/80 mm Hg, heart rate is 87/min, respiratory rate is 14/min, and temperature is 36.8℃ (98.2℉). On physical exam, his left calf is firm and severely tender on palpation. The patient cannot actively dorsiflex his left foot, and passive dorsiflexion is limited. Posterior tibial and dorsalis pedis pulses are 2+ in the right leg and 1+ in the left leg. Axial load does not increase the pain. Which of the following is the best next step in the management of this patient?
- A. Lower limb CT scan
- B. Lower limb ultrasound
- C. Splinting and limb rest
- D. Fasciotomy (Correct Answer)
- E. Lower limb X-ray in two projections
Principles of fascial spaces Explanation: ***Fasciotomy***
- The patient presents with classic signs and symptoms of **acute compartment syndrome**, including unrelieved pain by analgesics, paresthesias, pain with passive stretching, and a tense compartment due to the bus door trauma.
- **Fasciotomy** is the definitive and urgent treatment to relieve pressure within the muscle compartments, prevent muscle ischemia, and avoid permanent nerve damage or limb loss.
*Lower limb CT scan*
- A **CT scan** is primarily used to evaluate bony structures and soft tissue injuries but is not the most immediate or definitive diagnostic tool for acute compartment syndrome.
- Delaying **fasciotomy** for imaging in a clear case of compartment syndrome can lead to irreversible damage.
*Lower limb ultrasound*
- **Ultrasound** can assess vascular flow and some soft tissue aspects but is not accurate or rapid enough for diagnosing compartment syndrome.
- It would not provide the necessary information to guide urgent surgical intervention.
*Splinting and limb rest*
- This approach is appropriate for fractures or soft tissue injuries without compartment syndrome; however, in acute compartment syndrome, **splinting or limb rest** will worsen the condition.
- **Immobilization** and elevation are contraindicated as they can further decrease blood flow and increase compartment pressure.
*Lower limb X-ray in two projections*
- An **X-ray** is useful for ruling out fractures but will not provide information about compartment pressure or muscle viability.
- While a fracture can sometimes cause compartment syndrome, the immediate concern here is the compartment syndrome itself, for which **X-rays** are not diagnostic.
Principles of fascial spaces US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Principles of fascial spaces Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Principles of fascial spaces US Medical PG Question 9: A 35-year-old woman presents with progressive vision loss and severe headache. MRI shows cavernous sinus thrombosis with extension into the superior ophthalmic vein. Blood cultures grow Staphylococcus aureus. History reveals she had squeezed a facial pustule near her upper lip 5 days prior. Evaluate the anatomical explanation and risk stratification for this complication.
- A. Direct lymphatic spread from facial infection due to rich subcutaneous lymphatic network
- B. Valveless facial venous system allowing retrograde flow from danger triangle to cavernous sinus (Correct Answer)
- C. Contiguous spread through cribriform plate from nasal cavity involvement
- D. Hematogenous seeding via internal jugular vein and sigmoid sinus
- E. Extension through pterygoid venous plexus communicating with middle meningeal vein
Principles of fascial spaces Explanation: ***Valveless facial venous system allowing retrograde flow from danger triangle to cavernous sinus***
- The **danger triangle of the face** (perioral and nasal areas) contains **valveless veins**, which allows blood to flow in a **retrograde** direction toward the intracranial space.
- Infections in this region can spread via the **angular vein** into the **superior ophthalmic vein**, directly reaching the **cavernous sinus** and causing septic thrombosis.
*Direct lymphatic spread from facial infection due to rich subcutaneous lymphatic network*
- While the face has a rich **lymphatic network**, lymphatic drainage typically leads to **submandibular or cervical lymph nodes**, not the cavernous sinus.
- Cavernous sinus thrombosis is a **vascular complication** specifically involving the **venous system**, not the lymphatic system.
*Contiguous spread through cribriform plate from nasal cavity involvement*
- The **cribriform plate** is a route for infections to enter the **subarachnoid space**, primarily leading to **meningitis** or brain abscesses.
- It does not serve as the primary anatomical conduit for superficial facial infections to localize within the **cavernous sinus**.
*Hematogenous seeding via internal jugular vein and sigmoid sinus*
- The **internal jugular vein** and **sigmoid sinus** represent the **outflow tract** away from the brain; flow to the cavernous sinus through this route would be highly atypical.
- Bacterial seeding via this route would usually imply **systemic bacteremia** or infection in the **mastoid air cells**, rather than a localized facial pustule.
*Extension through pterygoid venous plexus communicating with middle meningeal vein*
- The **pterygoid venous plexus** can communicate with the cavernous sinus, but it primarily drains the **infratemporal fossa** and deep face, not the superficial upper lip.
- The **middle meningeal vein** drains into the pterygoid plexus or sphenoparietal sinus and is not the classic path for **danger triangle** infections.
Principles of fascial spaces US Medical PG Question 10: A 52-year-old diabetic man undergoes emergent fasciotomy for compartment syndrome of the right leg following a tibia-fibula fracture. Intraoperatively, the anterior compartment muscles appear dusky and do not contract with stimulation. The lateral compartment muscles appear viable. Deep posterior compartment shows borderline viability with weak contraction. Superficial posterior compartment is clearly viable. Synthesize a management plan that optimizes limb salvage while minimizing morbidity.
- A. Debride anterior compartment only, leave wounds open, second look in 48 hours for other compartments
- B. Debride all nonviable muscle, preserve borderline tissue, second look in 24 hours (Correct Answer)
- C. Complete debridement of anterior and deep posterior compartments with immediate wound closure
- D. Below-knee amputation given extent of muscle necrosis and diabetes
- E. Hyperbaric oxygen therapy for 48 hours before deciding on debridement versus amputation
Principles of fascial spaces Explanation: ***Debride all nonviable muscle, preserve borderline tissue, second look in 24 hours***
- Immediate **debridement** of non-contractile, dusky muscle is crucial to prevent **myoglobinuria**, metabolic acidosis, and **acute kidney injury**.
- Marginal tissue should be preserved during the initial surgery to maximize potential **limb salvage**, necessitating a **mandatory second-look** procedure within 24-48 hours.
*Debride anterior compartment only, leave wounds open, second look in 48 hours for other compartments*
- Leaving known nonviable muscle in the anterior compartment for 48 hours increases the risk of **secondary infection** and systemic inflammatory response syndrome.
- Re-exploration should be performed sooner (24 hours) when multiple compartments show **borderline viability** to ensure timely intervention.
*Complete debridement of anterior and deep posterior compartments with immediate wound closure*
- **Immediate wound closure** is strictly contraindicated in compartment syndrome as it can cause a recurrence of increased pressure and facilitates **anaerobic infection**.
- Over-debridement of the **deep posterior compartment** before its viability is definitively determined could result in unnecessary loss of **plantarflexion** and sensation.
*Below-knee amputation given extent of muscle necrosis and diabetes*
- **Amputation** is premature as the lateral and superficial posterior compartments are viable, providing a foundation for a **functional limb**.
- While **diabetes** may complicate healing, it is not an absolute indication for primary amputation in the setting of salvageable muscle groups.
*Hyperbaric oxygen therapy for 48 hours before deciding on debridement versus amputation*
- Delaying surgical **debridement** of necrotic tissue to pursue **HBO therapy** is dangerous and allows for the progression of sepsis and muscle breakdown.
- HBO therapy is an **adjunct**, not a replacement for mechanical decompression and removal of dead tissue in **acute compartment syndrome**.
More Principles of fascial spaces US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.