Lower limb fascial compartments US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lower limb fascial compartments. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lower limb fascial compartments US Medical PG Question 1: A patient presents with difficulty extending their wrist following trauma to the posterior forearm. Which of the following muscles would be most affected by injury to the posterior interosseous nerve?
- A. Extensor carpi ulnaris
- B. Extensor carpi radialis brevis
- C. Extensor pollicis longus
- D. Extensor digitorum (Correct Answer)
Lower limb fascial compartments Explanation: ***Extensor digitorum***
- The **posterior interosseous nerve (PIN)** innervates most muscles of the **posterior compartment of the forearm**, including the extensor digitorum. [1]
- Loss of function in the **extensor digitorum** would directly impair **extension of the fingers** and contribute significantly to difficulty extending the wrist. [1]
*Extensor carpi ulnaris*
- This muscle is also innervated by the **posterior interosseous nerve (PIN)** and contributes to **wrist extension** and **ulnar deviation**.
- While its innervation by the PIN is correct, injury to the PIN would affect this muscle, but the *extensor digitorum* is more broadly responsible for the stated primary symptom (difficulty extending the wrist), as its primary action is finger and thus wrist extension.
*Extensor carpi radialis brevis*
- While it is a **wrist extensor**, it is innervated by the **deep branch of the radial nerve** *before* it becomes the posterior interosseous nerve.
- Therefore, an isolated injury to the **posterior interosseous nerve** proper would typically spare the extensor carpi radialis brevis.
*Extensor pollicis longus*
- This muscle is indeed innervated by the **posterior interosseous nerve (PIN)** and acts to extend the **thumb**. [1]
- While it would be affected, the primary problem described is difficulty extending the *wrist*, for which the extensor digitorum plays a more significant and general role than the extensor pollicis longus.
Lower limb fascial compartments US Medical PG Question 2: A 34-year-old man is brought to the emergency department 3 hours after being bitten by a rattlesnake. He was hiking in the Arizona desert when he accidentally stepped on the snake and it bit his right leg. His pulse is 135/min and blood pressure is 104/81 mm Hg. Examination shows right lower leg swelling, ecchymosis, and blistering. Right ankle dorsiflexion elicits severe pain. A manometer inserted in the lateral compartment of the lower leg shows an intracompartmental pressure of 67 mm Hg. In addition to administration of the antivenom, the patient undergoes fasciotomy. Two weeks later, he reports difficulty in walking. Neurologic examination shows a loss of sensation over the lower part of the lateral side of the right leg and the dorsum of the right foot. Right foot eversion is 1/5. There is no weakness in dorsiflexion. Which of the following nerves is most likely injured in this patient?
- A. Sural nerve
- B. Tibial nerve
- C. Saphenous nerve
- D. Superficial peroneal nerve (Correct Answer)
- E. Deep peroneal nerve
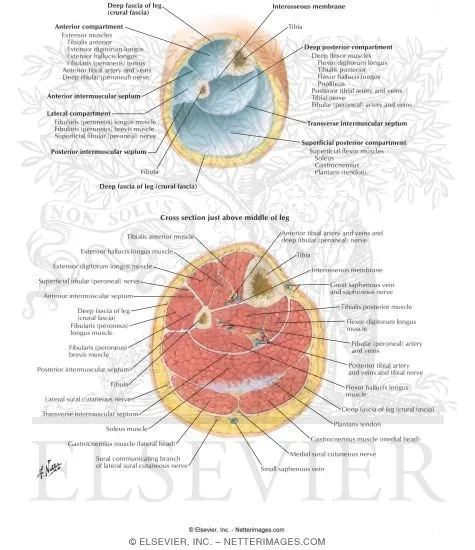
Lower limb fascial compartments Explanation: ***Superficial peroneal nerve***
- The **superficial peroneal nerve** (also known as the superficial fibular nerve) is responsible for **foot eversion** (peroneus longus and brevis muscles) and provides sensory innervation to the **dorsum of the foot**, except for the web space between the first and second toes.
- The patient's inability to evert the foot and sensory loss on the dorsum of the foot, combined with a history of **compartment syndrome** and fasciotomy in the lateral compartment, strongly indicates injury to the superficial peroneal nerve.
*Sural nerve*
- The **sural nerve** provides sensory innervation to the **posterolateral aspect of the lower leg** and the lateral aspect of the foot.
- It does not innervate muscles involved in foot eversion or dorsiflexion, so its injury would not lead to the motor deficits described.
*Tibial nerve*
- The **tibial nerve** innervates the muscles of the posterior compartment of the leg, responsible for **plantarflexion** and inversion of the foot, and provides sensation to the sole of the foot.
- Its injury would lead to weakness in plantarflexion and sensory loss on the sole, not the symptoms described.
*Saphenous nerve*
- The **saphenous nerve** is a pure sensory nerve, supplying sensation to the **medial aspect of the lower leg and foot**.
- Its injury would result in sensory loss in this distribution but no motor deficits affecting foot eversion or dorsiflexion.
*Deep peroneal nerve*
- The **deep peroneal nerve** (also known as the deep fibular nerve) innervates the muscles of the anterior compartment of the leg, primarily responsible for **foot dorsiflexion** and toe extension, and provides sensation to the web space between the first and second toes.
- The patient has no weakness in dorsiflexion, ruling out significant injury to the deep peroneal nerve.
Lower limb fascial compartments US Medical PG Question 3: A 31-year-old woman with multiple sclerosis comes to the physician because of a 4-day history of cramps in her left leg. Physical examination shows flexion of the left hip and increased tone in the thigh muscles. A local anesthetic block of which of the following nerves would most likely improve this patient's condition the most?
- A. Inferior gluteal nerve
- B. Superior gluteal nerve
- C. Femoral nerve (Correct Answer)
- D. Sciatic nerve
- E. Obturator nerve
Lower limb fascial compartments Explanation: ***Femoral nerve***
- The **femoral nerve** innervates the **iliacus** (a primary hip flexor) and the **rectus femoris** (part of the quadriceps that assists in hip flexion), as well as the entire **quadriceps femoris group** (responsible for knee extension and contributing to increased thigh muscle tone).
- In this patient with spasticity, **hip flexion** is caused by hypertonicity of iliopsoas and rectus femoris, while **increased tone in thigh muscles** reflects quadriceps involvement.
- Blocking the femoral nerve would relax these muscles, thereby improving the **cramps, hip flexion, and increased thigh tone**.
*Inferior gluteal nerve*
- The **inferior gluteal nerve** primarily innervates the **gluteus maximus muscle**, which is involved in hip extension and external rotation, not hip flexion.
- Blocking this nerve would not directly address the symptoms of increased thigh muscle tone and hip flexion.
*Superior gluteal nerve*
- The **superior gluteal nerve** mainly innervates the **gluteus medius, gluteus minimus**, and **tensor fasciae latae muscles**, which are involved in hip abduction and internal rotation.
- Its blockade would not relieve hip flexion or thigh muscle cramps.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (hip extension, knee flexion) and all muscles below the knee.
- While it affects leg muscles, it does not directly control the muscles causing **hip flexion and increased thigh tone** in this context.
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles** of the thigh (adductor longus, brevis, magnus, gracilis), leading to hip adduction.
- Blocking this nerve would not address hip flexion or the increased tone in the quadriceps muscles described.
Lower limb fascial compartments US Medical PG Question 4: A 48-year-old male presents to his primary care provider with a two-week history of low back pain and left leg pain. He reports that his symptoms started while he was working at his job as a construction worker. He has since experienced intermittent achy pain over his lumbar spine. He has also noticed pain radiating into his left leg and weakness in left ankle dorsiflexion. On exam, he demonstrates the following findings on strength testing of the left leg: 5/5 in knee extension, 4/5 in ankle dorsiflexion, 4/5 in great toe extension, 5/5 in ankle plantarflexion, and 5/5 in great toe flexion. The patellar reflexes are 5/5 bilaterally. He is able to toe walk but has difficulty with heel walking. Weakness in which of the following compartments of the leg is most likely causing this patient’s foot drop?
- A. Lateral compartment
- B. Superficial posterior compartment
- C. Deep posterior compartment
- D. Anterior compartment (Correct Answer)
- E. Medial compartment
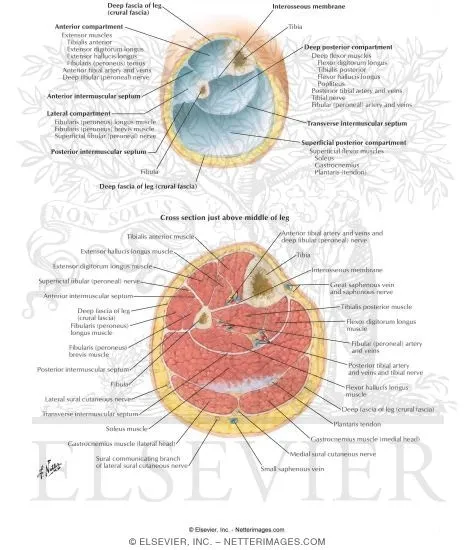
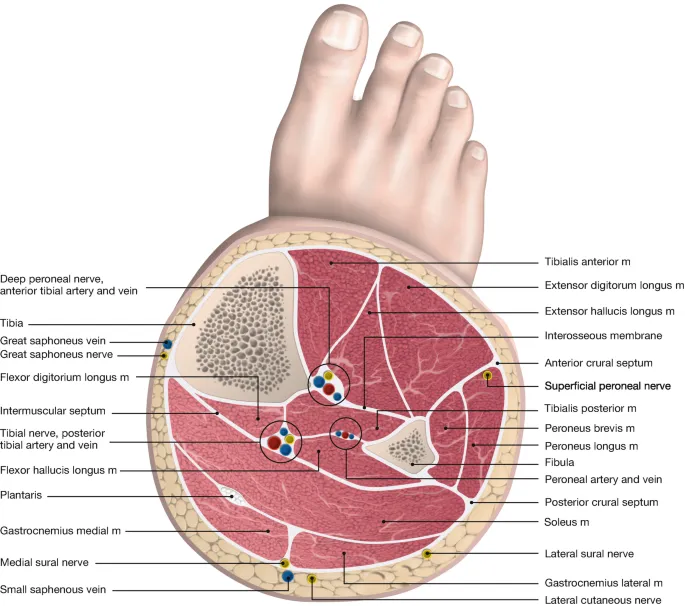
Lower limb fascial compartments Explanation: ***Anterior compartment***
- Weakness in **ankle dorsiflexion** and **great toe extension**, coupled with difficulty **heel walking**, indicates a foot drop due to dysfunction of muscles in the anterior compartment, such as the **tibialis anterior**, **extensor hallucis longus**, and **extensor digitorum longus**.
- These muscles are primarily innervated by the **deep fibular nerve**, which is susceptible to compression from conditions like **lumbar radiculopathy** (L4-L5 nerve root involvement).
*Lateral compartment*
- Muscles in the lateral compartment (**fibularis longus** and **brevis**) are responsible for **eversion** of the foot.
- Weakness in this compartment would manifest as difficulty everting the foot, not primarily ankle dorsiflexion or great toe extension deficits.
*Superficial posterior compartment*
- This compartment contains muscles like the **gastrocnemius** and **soleus**, which are primarily responsible for **ankle plantarflexion**.
- The patient exhibits 5/5 strength in ankle plantarflexion and is able to toe walk, indicating these muscles are functioning well.
*Deep posterior compartment*
- Muscles in the deep posterior compartment (**tibialis posterior**, **flexor digitorum longus**, **flexor hallucis longus**) are involved in **inversion** and **toe flexion**.
- The patient has 5/5 strength in great toe flexion, suggesting intact function of these muscles, and his primary deficit is in dorsiflexion.
*Medial compartment*
- There is no distinct "medial compartment" of the leg in the anatomical sense comparable to the other listed compartments; rather, various muscles contribute to medial actions.
- The symptoms described specifically point to weakness in dorsiflexion and toe extension, localizing the problem to the anterior compartment.
Lower limb fascial compartments US Medical PG Question 5: A 23-year-old patient presents to the emergency department after a motor vehicle accident. The patient was an unrestrained driver involved in a head-on collision. The patient is heavily intoxicated on what he claims is only alcohol. An initial trauma assessment is performed, and is notable for significant bruising of the right forearm. The patient is in the trauma bay, and complains of severe pain in his right forearm. A physical exam is performed and is notable for pallor, decreased sensation, and cool temperature of the skin of the right forearm. Pain is elicited upon passive movement of the right forearm and digits. A thready radial pulse is palpable. A FAST exam is performed, and is negative for signs of internal bleeding. The patient's temperature is 99.5°F (37.5°C), pulse is 100/min, blood pressure is 110/70 mmHg, respirations are 12/min, and oxygen saturation is 98% on room air. Radiography of the right forearm is ordered. The patient is still heavily intoxicated. Which of the following is the best next step in management?
- A. Fasciotomy (Correct Answer)
- B. IV fluids
- C. Analgesics
- D. Pressure measurement
- E. Detoxification
Lower limb fascial compartments Explanation: ***Fasciotomy***
- The patient exhibits classic signs of **acute compartment syndrome**, including severe pain out of proportion to injury, pain on passive stretch, pallor, decreased sensation, and cool extremity, despite a palpable pulse. These symptoms necessitate immediate surgical intervention to relieve pressure.
- A **fasciotomy** is the definitive treatment for acute compartment syndrome to prevent irreversible muscle and nerve damage, and potentially limb loss.
*IV fluids*
- While fluid resuscitation is important in trauma, the patient's current vital signs (BP 110/70 mmHg, pulse 100/min) do not indicate immediate shock requiring aggressive IV fluid administration over addressing the limb-threatening compartment syndrome.
- Prioritizing IV fluids without addressing **compartment syndrome** could lead to permanent loss of limb function.
*Analgesics*
- Administering analgesics might mask the escalating pain a key symptom of compartment syndrome, which could delay diagnosis and definitive treatment.
- While pain control is important, it should not supersede measures to prevent irreversible tissue damage.
*Pressure measurement*
- While compartment pressure measurement can confirm the diagnosis of compartment syndrome, the clinical presentation in this case is so compelling that delaying definitive treatment for pressure measurement is not the best next step.
- Clinical signs and symptoms are often sufficient for diagnosis, and surgical intervention should not be deferred pending pressure readings in clear-cut cases.
*Detoxification*
- Detoxification for alcohol intoxication is not an emergent and immediate priority in comparison to the limb-threatening condition of acute compartment syndrome.
- Addressing the **compartment syndrome** is critical for preserving limb viability, whereas detoxification can be managed once acute medical emergencies are controlled.
Lower limb fascial compartments US Medical PG Question 6: A 35-year-old man is referred to a physical therapist due to limitation of movement in the wrist and fingers of his left hand. He cannot hold objects or perform daily activities with his left hand. He broke his left arm at the humerus one month ago. The break was simple and treatment involved a cast for one month. Then he lost his health insurance and could not return for follow up. Only after removing the cast did he notice the movement issues in his left hand and wrist. His past medical history is otherwise insignificant, and vital signs are within normal limits. On examination, the patient’s left hand is pale and flexed in a claw-like position. It is firm and tender to palpation. Right radial pulse is 2+ and left radial pulse is 1+. The patient is unable to actively extend his fingers and wrist, and passive extension is difficult and painful. Which of the following is a proper treatment for the presented patient?
- A. Surgical release (Correct Answer)
- B. Botulinum toxin injections
- C. Collagenase injections
- D. Needle fasciotomy
- E. Corticosteroid injections
Lower limb fascial compartments Explanation: ***Surgical release***
- The patient presents with classic signs of **established Volkmann's ischemic contracture** (claw-like hand, firm fibrotic tissue, limited movement, decreased radial pulse), which is the end-stage result of untreated compartment syndrome that occurred during fracture healing.
- Since this is **chronic contracture (one month post-injury)**, the appropriate surgical treatment involves **reconstructive procedures** such as muscle slide operations, tendon lengthening, tendon transfers, neurolysis, or in severe cases, free functional muscle transfer to restore hand function.
- Emergency fasciotomy would have been appropriate for **acute compartment syndrome** (within 6-8 hours of onset), but at this stage, the treatment focuses on releasing fibrotic tissue and restoring function through reconstructive surgery.
*Botulinum toxin injections*
- **Botulinum toxin** is used to relax spastic muscles in neurological conditions (e.g., cerebral palsy, stroke), but it does not address the underlying **ischemic fibrosis and muscle necrosis** of Volkmann's contracture.
- It would not improve the structural contracture or restore blood flow in this patient.
*Collagenase injections*
- **Collagenase injections** are used for localized fascial contractures like Dupuytren's contracture, where enzymatic breakdown of collagen cords can restore finger extension.
- They are ineffective for **Volkmann's contracture**, which involves widespread ischemic muscle necrosis, fibrosis, and nerve damage requiring surgical reconstruction.
*Needle fasciotomy*
- **Needle fasciotomy** is a minimally invasive technique for Dupuytren's contracture, involving percutaneous disruption of fascial cords.
- It is not suitable for **Volkmann's contracture**, which requires extensive surgical release of fibrotic muscle compartments, possible tendon transfers, and neurolysis—procedures that cannot be accomplished with needle techniques.
*Corticosteroid injections*
- **Corticosteroids** reduce inflammation in conditions like tenosynovitis or trigger finger.
- They would not address the **ischemic muscle necrosis and fibrotic contracture** in Volkmann's contracture and could potentially delay appropriate surgical treatment.
Lower limb fascial compartments US Medical PG Question 7: A 45-year-old male presents to his primary care provider with an abnormal gait. He was hospitalized one week prior for acute cholecystitis and underwent a laparoscopic cholecystectomy. He received post-operative antibiotics via intramuscular injection. He recovered well and he was discharged on post-operative day #3. However, since he started walking after the operation, he noticed a limp that has not improved. On exam, his left hip drops every time he raises his left foot to take a step. In which of the following locations did this patient likely receive the intramuscular injection?
- A. Superomedial quadrant of the buttock (Correct Answer)
- B. Superolateral quadrant of the buttock
- C. Anteromedial thigh
- D. Inferomedial quadrant of the buttock
- E. Inferolateral quadrant of the buttock
Lower limb fascial compartments Explanation: ***Superomedial quadrant of the buttock***
- An injection in the **superomedial quadrant of the buttock** is the most common site for iatrogenic injury to the **superior gluteal nerve**.
- The superior gluteal nerve exits the pelvis through the greater sciatic foramen above the piriformis muscle and runs in the **superomedial** region of the buttock.
- Injury to the superior gluteal nerve results in weakness of the **gluteus medius and minimus muscles**, leading to a **Trendelenburg gait** (hip drops on the contralateral side when lifting that leg), which is consistent with the patient's symptoms.
- This is why the **superolateral quadrant** is recommended for safe IM injections.
*Superolateral quadrant of the buttock*
- The **superolateral quadrant** is the **safest site** for intramuscular gluteal injections precisely because it avoids the superior gluteal nerve.
- This is the recommended injection site to prevent the complication that this patient experienced.
- An injection here would not cause superior gluteal nerve injury or Trendelenburg gait.
*Inferomedial quadrant of the buttock*
- Injections in the **inferomedial quadrant** put the **sciatic nerve** at significant risk of injury.
- Sciatic nerve injury would lead to symptoms affecting the posterior thigh and lower leg, such as **foot drop, loss of ankle reflexes, or paresthesias in the posterior leg and foot**, not isolated hip abductor weakness.
*Inferolateral quadrant of the buttock*
- This area is close to the **sciatic nerve** and **inferior gluteal nerve**.
- Inferior gluteal nerve injury would affect the **gluteus maximus**, leading to difficulty with hip extension (trouble climbing stairs, rising from a chair), not a Trendelenburg gait.
- Sciatic nerve injury would present with foot drop and sensory deficits.
*Anteromedial thigh*
- Injections in the **anteromedial thigh** could injure the **femoral nerve** or its branches.
- This would cause **quadriceps weakness** with impaired knee extension and difficulty walking (buckling knee), not hip abductor weakness or Trendelenburg gait.
- The femoral nerve does not control hip abduction.
Lower limb fascial compartments US Medical PG Question 8: A 31-year-old man presents to the Emergency Department with severe left leg pain and paresthesias 4 hours after his leg got trapped by the closing door of a bus. Initially, he had a mild pain which gradually increased to unbearable levels. Past medical history is noncontributory. In the Emergency Department, his blood pressure is 130/80 mm Hg, heart rate is 87/min, respiratory rate is 14/min, and temperature is 36.8℃ (98.2℉). On physical exam, his left calf is firm and severely tender on palpation. The patient cannot actively dorsiflex his left foot, and passive dorsiflexion is limited. Posterior tibial and dorsalis pedis pulses are 2+ in the right leg and 1+ in the left leg. Axial load does not increase the pain. Which of the following is the best next step in the management of this patient?
- A. Lower limb CT scan
- B. Lower limb ultrasound
- C. Splinting and limb rest
- D. Fasciotomy (Correct Answer)
- E. Lower limb X-ray in two projections
Lower limb fascial compartments Explanation: ***Fasciotomy***
- The patient presents with classic signs and symptoms of **acute compartment syndrome**, including unrelieved pain by analgesics, paresthesias, pain with passive stretching, and a tense compartment due to the bus door trauma.
- **Fasciotomy** is the definitive and urgent treatment to relieve pressure within the muscle compartments, prevent muscle ischemia, and avoid permanent nerve damage or limb loss.
*Lower limb CT scan*
- A **CT scan** is primarily used to evaluate bony structures and soft tissue injuries but is not the most immediate or definitive diagnostic tool for acute compartment syndrome.
- Delaying **fasciotomy** for imaging in a clear case of compartment syndrome can lead to irreversible damage.
*Lower limb ultrasound*
- **Ultrasound** can assess vascular flow and some soft tissue aspects but is not accurate or rapid enough for diagnosing compartment syndrome.
- It would not provide the necessary information to guide urgent surgical intervention.
*Splinting and limb rest*
- This approach is appropriate for fractures or soft tissue injuries without compartment syndrome; however, in acute compartment syndrome, **splinting or limb rest** will worsen the condition.
- **Immobilization** and elevation are contraindicated as they can further decrease blood flow and increase compartment pressure.
*Lower limb X-ray in two projections*
- An **X-ray** is useful for ruling out fractures but will not provide information about compartment pressure or muscle viability.
- While a fracture can sometimes cause compartment syndrome, the immediate concern here is the compartment syndrome itself, for which **X-rays** are not diagnostic.
Lower limb fascial compartments US Medical PG Question 9: An MRI of a patient with low back pain reveals compression of the L5 nerve root. Which of the following muscles would most likely show weakness during physical examination?
- A. Tibialis posterior
- B. Tibialis anterior (Correct Answer)
- C. Gastrocnemius
- D. Quadriceps femoris
Lower limb fascial compartments Explanation: ***Tibialis anterior***
- The **L5 nerve root** primarily innervates muscles responsible for **dorsiflexion** of the foot, with the **tibialis anterior** being the primary dorsiflexor.
- Weakness of the tibialis anterior would manifest as difficulty lifting the front of the foot, potentially leading to a **foot drop** gait.
*Tibialis posterior*
- The **tibialis posterior** is primarily innervated by the **tibial nerve** (S1-S2) and is responsible for **plantarflexion** and **inversion** of the foot.
- Weakness in this muscle would not be the most likely presentation of L5 nerve root compression.
*Gastrocnemius*
- The **gastrocnemius** muscle is primarily innervated by the **tibial nerve** (S1-S2) and is a powerful **plantarflexor** of the foot.
- Weakness in this muscle would indicate an S1 or S2 nerve root issue, not typically L5.
*Quadriceps femoris*
- The **quadriceps femoris** is innervated by the **femoral nerve**, predominantly originating from the **L2, L3, and L4 nerve roots**.
- Weakness would manifest as difficulty extending the knee, which is not characteristic of L5 compression.
Lower limb fascial compartments US Medical PG Question 10: A 23-year-old woman presents to the emergency department with an acute exacerbation of her 3-month history of low back and right leg pain. She says she has had similar symptoms in the past, but this time the pain was so excruciating, it took her breath away. She describes the pain as severe, shock-like, and localized to her lower back and radiating straight down the back of her right thigh and to her calf, stopping at the ankle. Her pain is worse in the morning, and, sometimes, the pain wakes her up at night with severe buttock and posterior thigh pain but walking actually makes the pain subside somewhat. The patient reports no smoking history or alcohol or drug use. She has been working casually as a waitress and does find bending over tables a strain. She is afebrile, and her vital signs are within normal limits. On physical examination, her left straight leg raise test is severely limited and reproduces her buttock pain at 20° of hip flexion. Pain is worsened by the addition of ankle dorsiflexion. The sensation is intact. Her L4 and L5 reflexes are normal, but her S1 reflex is absent on the right side. A CT of the lumbar spine shows an L5–S1 disc protrusion with right S1 nerve root compression. Which of the following muscle-nerve complexes is involved in producing an S1 reflex?
- A. Adductors-obturator nerve
- B. Gastrocnemius/soleus-tibial nerve (Correct Answer)
- C. Sartorius-femoral nerve
- D. Tibialis posterior-tibial nerve
- E. Quadriceps femoris-femoral nerve
Lower limb fascial compartments Explanation: ***Gastrocnemius/soleus-tibial nerve***
- The S1 reflex (also known as the **Achilles reflex**) tests the integrity of the **S1 nerve root**.
- This reflex arc involves the **gastrocnemius and soleus muscles**, which are innervated by the **tibial nerve** (derived primarily from S1).
*Adductors-obturator nerve*
- The **adductor muscles** of the thigh are primarily innervated by the **obturator nerve** (L2-L4).
- This complex is not involved in generating the **Achilles reflex**.
*Sartorius-femoral nerve*
- The **sartorius muscle** is innervated by the **femoral nerve** (L2-L4).
- This muscle and nerve are not part of the **S1 reflex arc**.
*Tibialis posterior-tibial nerve*
- The **tibialis posterior muscle** is innervated by the **tibial nerve** (L4-S3), but its primary role is in ankle inversion and plantarflexion, not the main component of the **Achilles reflex**.
- While the tibial nerve is involved in the S1 reflex, the **gastrocnemius and soleus** are the primary muscles for this reflex.
*Quadriceps femoris-femoral nerve*
- The **quadriceps femoris muscle** is responsible for the **patellar reflex** (knee jerk reflex), which tests the integrity of the **L3-L4 nerve roots**.
- It is innervated by the **femoral nerve** and is not involved in the **S1 reflex**.
More Lower limb fascial compartments US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.