Compartment syndrome pathophysiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Compartment syndrome pathophysiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Compartment syndrome pathophysiology US Medical PG Question 1: A 37‐year‐old woman presents with a severe, deep, sharp pain in her right hand and forearm. A week before she presented her pain symptoms, she fell on her right forearm and developed mild bruising. She has type-1 diabetes mellitus and is on an insulin treatment. The physical examination reveals that her right hand and forearm were warmer, more swollen, and had a more reddish appearance than the left side. She feels an intense pain upon light touching of her right hand and forearm. Her radial and brachial pulses are palpable. The neurological examination is otherwise normal. The laboratory test results are as follows:
Hemoglobin 15.2 g/dL
White blood cell count 6,700 cells/cm3
Platelets 300,000 cells/cm3
Alanine aminotransferase 32 units/L
Aspartate aminotransferase 38 units/L
C-reactive protein 0.4 mg/L
Erythrocyte sedimentation rate 7 mm/1st hour
The X-ray of the right hand and forearm do not show a fracture. The nerve conduction studies are also within normal limits. What is the most likely diagnosis?
- A. Complex regional pain syndrome (Correct Answer)
- B. Compartment syndrome
- C. Diabetic neuropathy
- D. Cellulitis
- E. Limb ischemia
Compartment syndrome pathophysiology Explanation: ***Complex regional pain syndrome***
- This patient's symptoms of **severe pain**, **allodynia** (pain from light touch), **vasomotor changes** (warmth, swelling, redness), and **trophic changes** (initially normal X-ray) following a mild trauma align with the diagnosis of CRPS I.
- The absence of significant inflammation markers (normal CRP, ESR), normal pulses, and normal neurological exam further supports CRPS over other inflammatory or ischemic conditions.
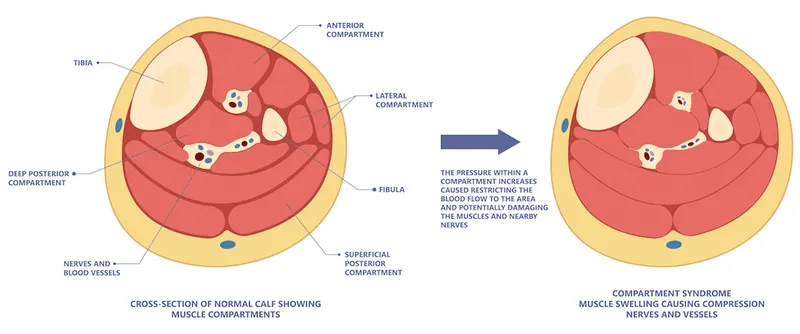
*Compartment syndrome*
- This condition is characterized by the **"6 Ps"** – pain, pallor, paresthesia, pulselessness, paralysis, and poikilothermia – resulting from increased pressure within a muscle compartment.
- While pain is severe, the patient's **palpable pulses** and normal neurological exam make compartment syndrome less likely, as it typically involves significant neurological deficits and vascular compromise, often requiring urgent fasciotomy.
*Diabetic neuropathy*
- This condition typically presents as **bilateral, symmetrical pain** and sensory loss, often described as burning or tingling, primarily affecting the distal extremities (stocking-glove distribution).
- The patient's **unilateral, acute onset of severe pain** and the presence of significant vasomotor changes do not fit the typical presentation of diabetic neuropathy.
*Cellulitis*
- Cellulitis is a **bacterial skin infection** characterized by localized redness, warmth, swelling, and pain, often with fever and elevated inflammatory markers.
- The patient's **normal white blood cell count**, **normal CRP**, and **normal ESR** make an active infectious process like cellulitis highly unlikely.
*Limb ischemia*
- **Acute limb ischemia** typically presents with severe pain, pallor, paresthesia, pulselessness, and paralysis, due to a sudden lack of blood flow to the limb.
- The patient's **palpable radial and brachial pulses** rule out significant large vessel obstruction, making limb ischemia an improbable diagnosis.
Compartment syndrome pathophysiology US Medical PG Question 2: A 37-year-old man is brought to the emergency department by ambulance after a motor vehicle accident. He suffered multiple deep lacerations and experienced significant blood loss during transport. In the emergency department, his temperature is 98.6°F (37°C), blood pressure is 102/68 mmHg, pulse is 112/min, and respirations are 22/min. His lacerations are sutured and he is given 2 liters of saline by large bore intravenous lines. Which of the following changes will occur in this patient's cardiac physiology due to this intervention?
- A. Increased cardiac output and unchanged right atrial pressure
- B. Decreased cardiac output and increased right atrial pressure
- C. Increased cardiac output and decreased right atrial pressure
- D. Increased cardiac output and increased right atrial pressure (Correct Answer)
- E. Decreased cardiac output and decreased right atrial pressure
Compartment syndrome pathophysiology Explanation: ***Increased cardiac output and increased right atrial pressure***
- The patient experienced significant blood loss, leading to a **decreased preload** and subsequent **reduced cardiac output**. Volume resuscitation with saline directly increases the **intravascular volume** which bolsters **venous return** and **right atrial pressure**.
- According to the **Frank-Starling mechanism**, increased right atrial pressure (a measure of preload) results in an increase in ventricular stretch and a more forceful contraction, thereby increasing **stroke volume** and **cardiac output**.
*Increased cardiac output and unchanged right atrial pressure*
- While fluid administration will increase **cardiac output** by improving preload, it will also directly lead to an increase in **right atrial pressure** due to the augmented venous return.
- An unchanged right atrial pressure would imply no significant increase in central venous volume, which contradicts the effect of a large volume fluid resuscitation.
*Decreased cardiac output and increased right atrial pressure*
- This scenario is unlikely because increasing **intravascular volume** through fluid resuscitation typically aims to raise **cardiac output** by optimizing preload, not decrease it.
- A decrease in cardiac output despite increased right atrial pressure could indicate **cardiac pump failure**, which is not suggested by the clinical picture of hypovolemic shock treated with fluids.
*Increased cardiac output and decreased right atrial pressure*
- An increase in **cardiac output** as a result of fluid resuscitation is expected, but a **decreased right atrial pressure** would contradict the mechanism of increased venous return and volume expansion.
- Decreased right atrial pressure would typically indicate ongoing volume loss or inadequate fluid resuscitation to restore central venous volume.
*Decreased cardiac output and decreased right atrial pressure*
- Both decreasing **cardiac output** and decreasing **right atrial pressure** indicate a worsening state of **hypovolemia** or an inadequate response to fluid resuscitation.
- The administration of 2 liters of saline is intended to correct the hypovolemia and improve cardiodynamics, not to worsen them.
Compartment syndrome pathophysiology US Medical PG Question 3: A 27-year-old soldier stationed in Libya sustains a shrapnel injury during an attack, causing a traumatic above-elbow amputation. The resulting arterial bleed is managed with a tourniquet prior to transport to the military treatment facility. On arrival, he is alert and oriented to person, place, and time. His armor and clothing are removed. His pulse is 145/min, respirations are 28/min, and blood pressure is 95/52 mm Hg. Pulmonary examination shows symmetric chest rise. The lungs are clear to auscultation. Abdominal examination shows no abnormalities. There are multiple shrapnel wounds over the upper and lower extremities. A tourniquet is in place around the right upper extremity; the right proximal forearm has been amputated. One large-bore intravenous catheter is placed in the left antecubital fossa. Despite multiple attempts, medical staff is unable to establish additional intravenous access. Which of the following is the most appropriate next step in management?
- A. Irrigate the shrapnel wounds
- B. Perform endotracheal intubation
- C. Establish intraosseous access (Correct Answer)
- D. Establish central venous access
- E. Replace the tourniquet with a pressure dressing
Compartment syndrome pathophysiology Explanation: ***Establish intraosseous access***
- The patient is in **hemorrhagic shock** (tachycardia, hypotension) and requires rapid fluid resuscitation, but peripheral intravenous access is difficult to obtain. **Intraosseous (IO) access** provides a rapid and reliable route for fluids and medications, especially in emergencies when IV access is challenging.
- IO access is a **bridge to definitive venous access** and is crucial for immediate life-saving interventions in trauma.
*Irrigate the shrapnel wounds*
- While wound irrigation is important for preventing infection, it is **not the immediate priority** when the patient is in hemorrhagic shock.
- Addressing the circulatory compromise takes precedence over local wound care.
*Perform endotracheal intubation*
- The patient is **alert and oriented** with symmetric chest rise and clear lungs, indicating he does not currently have an airway crisis requiring intubation.
- Intubation is an invasive procedure that carries risks and should only be performed when indicated for airway protection or respiratory failure.
*Establish central venous access*
- While central venous access is useful for long-term fluid management and monitoring, it is generally **more time-consuming and technically challenging** to establish than IO access, especially in an emergent, unstable patient.
- Given the urgency of rapid fluid administration, IO access is preferred as the immediate next step.
*Replace the tourniquet with a pressure dressing*
- The patient has an above-elbow amputation, suggesting significant injury, and the tourniquet is currently controlling the bleed. Removing the tourniquet prematurely without proximal surgical control can lead to **recurrent catastrophic hemorrhage**.
- A definitive surgical approach is needed to manage the amputation, not simply replacing the tourniquet with a pressure dressing, which may be insufficient to control arterial bleeding.
Compartment syndrome pathophysiology US Medical PG Question 4: A 38-year-old man is brought to the emergency department 35 minutes after he sustained a gunshot wound to the right thigh. He has type 1 diabetes mellitus. On arrival, his pulse is 112/min, respirations are 20/min, and blood pressure is 115/69 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. There is an entrance wound on the anteromedial surface of the right thigh 2 cm below the inguinal ligament. There is no bruit or thrill. There is no exit wound. The pedal pulse is diminished on the right side compared to the left. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hematocrit 46%
Serum
Urea nitrogen 24 mg/dL
Glucose 160 mg/dL
Creatinine 3.1 mg/dL
Which of the following is the most appropriate next step in management?
- A. Digital subtraction angiography
- B. Wound cleaning and tetanus toxoid
- C. CT angiography
- D. Duplex ultrasonography (Correct Answer)
- E. Fasciotomy
Compartment syndrome pathophysiology Explanation: ***Duplex ultrasonography***
- The patient has suffered a **gunshot wound** to the thigh with a **diminished pedal pulse**, indicating potential **vascular injury** (a "soft sign" requiring imaging).
- Given his **significantly elevated creatinine (3.1 mg/dL)** and **type 1 diabetes mellitus**, imaging studies requiring **IV iodinated contrast** carry substantial risk for **contrast-induced nephropathy** and further renal deterioration.
- **Duplex ultrasonography** is a **non-invasive, contrast-free method** to assess vascular flow and identify injuries like **arterial dissection**, **thrombosis**, or **pseudoaneurysm**. While operator-dependent, it is the most appropriate initial diagnostic step in this hemodynamically stable patient with significant renal impairment.
- This allows vascular assessment while **minimizing nephrotoxic risk** in a patient with pre-existing renal dysfunction.
*CT angiography*
- **CT angiography** is the **gold standard** for evaluating penetrating extremity trauma with soft signs of vascular injury in most cases, offering rapid and highly accurate vascular imaging.
- However, it requires administration of **intravenous iodinated contrast**, which poses significant risk for **contrast-induced nephropathy** in this patient with **baseline creatinine of 3.1 mg/dL** and **diabetes mellitus**.
- While CTA would typically be preferred in trauma settings, the severe renal impairment makes duplex ultrasonography the safer initial choice in this stable patient.
*Digital subtraction angiography*
- This is an **invasive angiographic technique** that uses **iodinated contrast** and carries even higher contrast load than CTA, posing substantial risk for **contrast-induced nephropathy** given the patient's **elevated creatinine**.
- While it offers high resolution and therapeutic capability, the risks associated with contrast and invasive arterial access outweigh its benefits for initial assessment in this scenario.
- Reserved for cases where intervention is anticipated or non-invasive imaging is inconclusive.
*Wound cleaning and tetanus toxoid*
- These are essential components of wound care for any penetrating injury but do not address the immediate concern of **potential vascular injury** causing the diminished pedal pulse.
- Prioritizing definitive diagnosis of vascular compromise is critical before focusing solely on local wound management, as a missed arterial injury could lead to limb loss.
*Fasciotomy*
- **Fasciotomy** is a surgical procedure to relieve **compartment syndrome**, which can develop secondary to vascular injury, reperfusion, or significant soft tissue trauma.
- While compartment syndrome is a risk with this injury, there is no immediate clinical evidence of it (no severe pain out of proportion to exam, no tense compartments documented).
- Diagnosis of the vascular injury should be established first, as fasciotomy may be needed later if ischemia is prolonged or after revascularization.
Compartment syndrome pathophysiology US Medical PG Question 5: A patient presents to the emergency department with arm pain. The patient recently experienced an open fracture of his radius when he fell from a ladder while cleaning his house. Surgical reduction took place and the patient's forearm was put in a cast. Since then, the patient has experienced worsening pain in his arm. The patient has a past medical history of hypertension and asthma. His current medications include albuterol, fluticasone, loratadine, and lisinopril. His temperature is 99.5°F (37.5°C), blood pressure is 150/95 mmHg, pulse is 90/min, respirations are 19/min, and oxygen saturation is 99% on room air. The patient's cast is removed. On physical exam, the patient's left arm is tender to palpation. Passive motion of the patient's wrist and fingers elicits severe pain. The patient's left radial and ulnar pulse are both palpable and regular. The forearm is soft and does not demonstrate any bruising but is tender to palpation. Which of the following is the next best step in management?
- A. Replace the cast with a sling
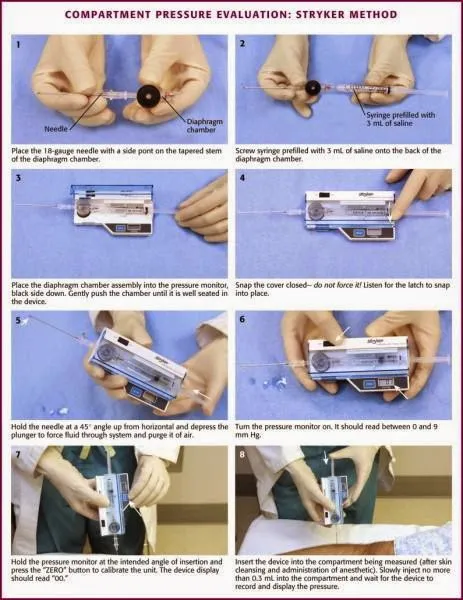
- B. Measurement of compartment pressure (Correct Answer)
- C. Ibuprofen and reassurance
- D. Emergency fasciotomy
- E. Radiography
Compartment syndrome pathophysiology Explanation: ***Measurement of compartment pressure***
- The patient exhibits classic signs of **compartment syndrome**, including severe pain out of proportion to injury, pain with passive stretching, and a history of trauma followed by casting. Measuring compartment pressure is crucial for diagnosis despite palpable pulses.
- Early measurement of compartment pressures can confirm the diagnosis and guide the decision for an **emergency fasciotomy** to prevent irreversible tissue damage.
*Replace the cast with a sling*
- This action would likely worsen the patient's condition by delaying the diagnosis and treatment of potential **compartment syndrome**.
- A sling does not address the underlying issue of increased pressure within the muscle compartments.
*Ibuprofen and reassurance*
- Administering **Ibuprofen (NSAID)** might mask the pain but will not resolve the increased pressure within the compartment, which is a surgical emergency.
- Reassurance without proper assessment of compartment syndrome could lead to irreversible muscle and nerve damage.
*Emergency fasciotomy*
- While a fasciotomy is the definitive treatment for confirmed compartment syndrome, it should only be performed **after compartment pressures have been measured** and the diagnosis confirmed, unless the clinical suspicion is extremely high and pressures cannot be obtained.
- Performing a fasciotomy without objective confirmation is generally not the immediate next step, as it is an invasive procedure with its own risks.
*Radiography*
- **Radiography** would be useful to assess the healing of the fracture or rule out new fractures, but it will not provide information about the soft tissue pressure changes characteristic of compartment syndrome.
- The patient's symptoms are more indicative of a circulatory or soft tissue issue rather than a new bony problem.
Compartment syndrome pathophysiology US Medical PG Question 6: A 31-year-old man presents to the Emergency Department with severe left leg pain and paresthesias 4 hours after his leg got trapped by the closing door of a bus. Initially, he had a mild pain which gradually increased to unbearable levels. Past medical history is noncontributory. In the Emergency Department, his blood pressure is 130/80 mm Hg, heart rate is 87/min, respiratory rate is 14/min, and temperature is 36.8℃ (98.2℉). On physical exam, his left calf is firm and severely tender on palpation. The patient cannot actively dorsiflex his left foot, and passive dorsiflexion is limited. Posterior tibial and dorsalis pedis pulses are 2+ in the right leg and 1+ in the left leg. Axial load does not increase the pain. Which of the following is the best next step in the management of this patient?
- A. Lower limb CT scan
- B. Lower limb ultrasound
- C. Splinting and limb rest
- D. Fasciotomy (Correct Answer)
- E. Lower limb X-ray in two projections
Compartment syndrome pathophysiology Explanation: ***Fasciotomy***
- The patient presents with classic signs and symptoms of **acute compartment syndrome**, including unrelieved pain by analgesics, paresthesias, pain with passive stretching, and a tense compartment due to the bus door trauma.
- **Fasciotomy** is the definitive and urgent treatment to relieve pressure within the muscle compartments, prevent muscle ischemia, and avoid permanent nerve damage or limb loss.
*Lower limb CT scan*
- A **CT scan** is primarily used to evaluate bony structures and soft tissue injuries but is not the most immediate or definitive diagnostic tool for acute compartment syndrome.
- Delaying **fasciotomy** for imaging in a clear case of compartment syndrome can lead to irreversible damage.
*Lower limb ultrasound*
- **Ultrasound** can assess vascular flow and some soft tissue aspects but is not accurate or rapid enough for diagnosing compartment syndrome.
- It would not provide the necessary information to guide urgent surgical intervention.
*Splinting and limb rest*
- This approach is appropriate for fractures or soft tissue injuries without compartment syndrome; however, in acute compartment syndrome, **splinting or limb rest** will worsen the condition.
- **Immobilization** and elevation are contraindicated as they can further decrease blood flow and increase compartment pressure.
*Lower limb X-ray in two projections*
- An **X-ray** is useful for ruling out fractures but will not provide information about compartment pressure or muscle viability.
- While a fracture can sometimes cause compartment syndrome, the immediate concern here is the compartment syndrome itself, for which **X-rays** are not diagnostic.
Compartment syndrome pathophysiology US Medical PG Question 7: A previously healthy 5-year-old boy is brought to the emergency department 15 minutes after sustaining an injury to his right hand. His mother says that she was cleaning the bathroom when he accidentally knocked over the drain cleaner bottle and spilled the liquid onto his hand. On arrival, he is crying and holding his right hand in a flexed position. His temperature is 37.7°C (99.8°F), pulse is 105/min, respirations are 25/min, and blood pressure is 105/65 mm Hg. Examination of the right hand shows a 4 x 4 cm area of reddened, blistered skin. The area is very tender to light touch. His ability to flex and extend the right hand are diminished. Radial pulses are palpable. Capillary refill time is less than 3 seconds. Which of the following is the most appropriate next step in management?
- A. Irrigate with water (Correct Answer)
- B. Apply split-thickness skin graft
- C. Apply silver sulfadiazine
- D. Apply mineral oil
- E. Perform escharotomy
Compartment syndrome pathophysiology Explanation: ***Irrigate with water***
- The immediate and most crucial step for a **chemical burn** is copious **irrigation with water** to remove the offending agent and prevent further tissue damage.
- This action minimizes the duration of contact between the **corrosive substance** and the skin, halting the chemical reaction.
*Apply split-thickness skin graft*
- A **skin graft** is a surgical procedure typically reserved for **deep burns** and is not the immediate first step for chemical exposure.
- It would be considered later in management if the burn resulted in **full-thickness tissue loss** and incomplete wound healing.
*Apply silver sulfadiazine*
- **Silver sulfadiazine** is an antimicrobial cream used to prevent infection in **thermal burns** after initial wound care.
- It is not indicated as the first line of treatment for a **chemical burn** and would not remove the chemical agent from the skin.
*Apply mineral oil*
- Applying **mineral oil** is not the appropriate initial treatment for a **chemical burn** and could potentially trap the chemical, worsening the injury.
- The priority is to dilute and remove the chemical, which mineral oil cannot do effectively.
*Perform escharotomy*
- An **escharotomy** is a surgical incision through burn eschar used to relieve pressure in **circumferential full-thickness burns** that compromise circulation.
- This procedure is not indicated as the initial management for a **chemical burn** and is only considered for severe, deep burns with vascular compromise.
Compartment syndrome pathophysiology US Medical PG Question 8: A 34-year-old man is brought to the emergency department 3 hours after being bitten by a rattlesnake. He was hiking in the Arizona desert when he accidentally stepped on the snake and it bit his right leg. His pulse is 135/min and blood pressure is 104/81 mm Hg. Examination shows right lower leg swelling, ecchymosis, and blistering. Right ankle dorsiflexion elicits severe pain. A manometer inserted in the lateral compartment of the lower leg shows an intracompartmental pressure of 67 mm Hg. In addition to administration of the antivenom, the patient undergoes fasciotomy. Two weeks later, he reports difficulty in walking. Neurologic examination shows a loss of sensation over the lower part of the lateral side of the right leg and the dorsum of the right foot. Right foot eversion is 1/5. There is no weakness in dorsiflexion. Which of the following nerves is most likely injured in this patient?
- A. Sural nerve
- B. Tibial nerve
- C. Saphenous nerve
- D. Superficial peroneal nerve (Correct Answer)
- E. Deep peroneal nerve
Compartment syndrome pathophysiology Explanation: ***Superficial peroneal nerve***
- The **superficial peroneal nerve** (also known as the superficial fibular nerve) is responsible for **foot eversion** (peroneus longus and brevis muscles) and provides sensory innervation to the **dorsum of the foot**, except for the web space between the first and second toes.
- The patient's inability to evert the foot and sensory loss on the dorsum of the foot, combined with a history of **compartment syndrome** and fasciotomy in the lateral compartment, strongly indicates injury to the superficial peroneal nerve.
*Sural nerve*
- The **sural nerve** provides sensory innervation to the **posterolateral aspect of the lower leg** and the lateral aspect of the foot.
- It does not innervate muscles involved in foot eversion or dorsiflexion, so its injury would not lead to the motor deficits described.
*Tibial nerve*
- The **tibial nerve** innervates the muscles of the posterior compartment of the leg, responsible for **plantarflexion** and inversion of the foot, and provides sensation to the sole of the foot.
- Its injury would lead to weakness in plantarflexion and sensory loss on the sole, not the symptoms described.
*Saphenous nerve*
- The **saphenous nerve** is a pure sensory nerve, supplying sensation to the **medial aspect of the lower leg and foot**.
- Its injury would result in sensory loss in this distribution but no motor deficits affecting foot eversion or dorsiflexion.
*Deep peroneal nerve*
- The **deep peroneal nerve** (also known as the deep fibular nerve) innervates the muscles of the anterior compartment of the leg, primarily responsible for **foot dorsiflexion** and toe extension, and provides sensation to the web space between the first and second toes.
- The patient has no weakness in dorsiflexion, ruling out significant injury to the deep peroneal nerve.
Compartment syndrome pathophysiology US Medical PG Question 9: A 35-year-old man is brought to the emergency department from a kitchen fire. The patient was cooking when boiling oil splashed on his exposed skin. His temperature is 99.7°F (37.6°C), blood pressure is 127/82 mmHg, pulse is 120/min, respirations are 12/min, and oxygen saturation is 98% on room air. He has dry, nontender, and circumferential burns over his arms bilaterally, burns over the anterior portion of his chest and abdomen, and tender spot burns with blisters on his shins. A 1L bolus of normal saline is administered and the patient is given morphine and his pulse is subsequently 80/min. A Foley catheter is placed which drains 10 mL of urine. What is the best next step in management?
- A. Additional fluids and escharotomy (Correct Answer)
- B. Escharotomy
- C. Continuous observation
- D. Moist dressings and discharge
- E. Additional fluids and admission to the ICU
Compartment syndrome pathophysiology Explanation: ***Additional fluids and escharotomy***
- The patient has **circumferential full-thickness burns** on both arms (dry, nontender), which require **escharotomy** to prevent compartment syndrome and vascular compromise to the limbs.
- The **oliguria** (10 mL urine output) despite a 1L fluid bolus indicates **inadequate fluid resuscitation** from burn shock. With approximately 40% TBSA burns, the patient requires aggressive fluid resuscitation per the Parkland formula (4 mL/kg/% TBSA), which would be approximately 11 liters in the first 24 hours. Adequate resuscitation targets urine output of 0.5-1 mL/kg/hr (35-70 mL/hr for this patient).
- Both interventions are immediately necessary: fluids for burn shock and escharotomy for circumferential burns.
*Escharotomy*
- While **escharotomy** is essential for the circumferential full-thickness burns to prevent compartment syndrome, it alone will not address the **severe fluid deficit** causing oliguria and hypoperfusion.
- The low urine output reflects systemic hypovolemia from burn shock, not just local compartment issues, requiring aggressive fluid resuscitation.
*Continuous observation*
- **Continuous observation** is inappropriate given the patient's critical findings: circumferential full-thickness burns requiring urgent escharotomy and oliguria indicating inadequate resuscitation.
- Delaying escharotomy can lead to irreversible ischemic damage to the limbs, and inadequate fluid resuscitation can progress to multiorgan failure.
*Moist dressings and discharge*
- This option is completely inappropriate for a patient with **extensive deep burns** (approximately 40% TBSA) including full-thickness injuries requiring hospitalization and specialized burn care.
- Discharge would lead to severe complications including infection, inadequate fluid resuscitation, compartment syndrome, and potential limb loss.
*Additional fluids and admission to the ICU*
- While ICU admission and additional fluids are necessary components of care, this option is **incomplete** because it omits **escharotomy**, which is urgently needed for the circumferential full-thickness burns.
- Escharotomy is a time-sensitive procedure that must be performed promptly to prevent ischemic injury to the limbs from vascular compromise.
Compartment syndrome pathophysiology US Medical PG Question 10: A 23-year-old patient presents to the emergency department after a motor vehicle accident. The patient was an unrestrained driver involved in a head-on collision. The patient is heavily intoxicated on what he claims is only alcohol. An initial trauma assessment is performed, and is notable for significant bruising of the right forearm. The patient is in the trauma bay, and complains of severe pain in his right forearm. A physical exam is performed and is notable for pallor, decreased sensation, and cool temperature of the skin of the right forearm. Pain is elicited upon passive movement of the right forearm and digits. A thready radial pulse is palpable. A FAST exam is performed, and is negative for signs of internal bleeding. The patient's temperature is 99.5°F (37.5°C), pulse is 100/min, blood pressure is 110/70 mmHg, respirations are 12/min, and oxygen saturation is 98% on room air. Radiography of the right forearm is ordered. The patient is still heavily intoxicated. Which of the following is the best next step in management?
- A. Fasciotomy (Correct Answer)
- B. IV fluids
- C. Analgesics
- D. Pressure measurement
- E. Detoxification
Compartment syndrome pathophysiology Explanation: ***Fasciotomy***
- The patient exhibits classic signs of **acute compartment syndrome**, including severe pain out of proportion to injury, pain on passive stretch, pallor, decreased sensation, and cool extremity, despite a palpable pulse. These symptoms necessitate immediate surgical intervention to relieve pressure.
- A **fasciotomy** is the definitive treatment for acute compartment syndrome to prevent irreversible muscle and nerve damage, and potentially limb loss.
*IV fluids*
- While fluid resuscitation is important in trauma, the patient's current vital signs (BP 110/70 mmHg, pulse 100/min) do not indicate immediate shock requiring aggressive IV fluid administration over addressing the limb-threatening compartment syndrome.
- Prioritizing IV fluids without addressing **compartment syndrome** could lead to permanent loss of limb function.
*Analgesics*
- Administering analgesics might mask the escalating pain a key symptom of compartment syndrome, which could delay diagnosis and definitive treatment.
- While pain control is important, it should not supersede measures to prevent irreversible tissue damage.
*Pressure measurement*
- While compartment pressure measurement can confirm the diagnosis of compartment syndrome, the clinical presentation in this case is so compelling that delaying definitive treatment for pressure measurement is not the best next step.
- Clinical signs and symptoms are often sufficient for diagnosis, and surgical intervention should not be deferred pending pressure readings in clear-cut cases.
*Detoxification*
- Detoxification for alcohol intoxication is not an emergent and immediate priority in comparison to the limb-threatening condition of acute compartment syndrome.
- Addressing the **compartment syndrome** is critical for preserving limb viability, whereas detoxification can be managed once acute medical emergencies are controlled.
More Compartment syndrome pathophysiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.