Clinical correlations of fascial spaces US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Clinical correlations of fascial spaces. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Clinical correlations of fascial spaces US Medical PG Question 1: A 4-year-old girl is brought to the physician for a painless lump on her neck. She has no history of serious illness and her vital signs are within normal limits. On examination, there is a firm, 2-cm swelling at the midline just below the level of the hyoid bone. The mass moves cranially when she is asked to protrude her tongue. Which of the following is the most likely diagnosis?
- A. Cystic hygroma
- B. Thyroglossal cyst (Correct Answer)
- C. Ranula
- D. Dermoid cyst
Clinical correlations of fascial spaces Explanation: Thyroglossal cyst
- A midline neck mass that moves cranially with tongue protrusion is the classic presentation of a thyroglossal duct cyst.
- These cysts arise from the remnant of the thyroglossal duct, the embryonic tract along which the thyroid gland descends from the foramen cecum to its final position [1].
Cystic hygroma
- This is a lymphatic malformation typically appearing as a soft, compressible, transilluminant mass, often in the posterior triangle of the neck.
- It does not move with tongue protrusion and is usually not midline.
Ranula
- A ranula is a mucocele that forms in the floor of the mouth, usually due to obstruction of a sublingual salivary gland.
- It presents as a swelling in the oral cavity, below the tongue, and not as an external neck mass.
Dermoid cyst
- A dermoid cyst in the neck is typically a painless, doughy, subcutaneous mass that is also usually midline but does not move with tongue protrusion.
- These cysts are often found above the hyoid bone, unlike the typical position of a thyroglossal cyst.
Clinical correlations of fascial spaces US Medical PG Question 2: A 27-year-old soldier stationed in Libya sustains a shrapnel injury during an attack, causing a traumatic above-elbow amputation. The resulting arterial bleed is managed with a tourniquet prior to transport to the military treatment facility. On arrival, he is alert and oriented to person, place, and time. His armor and clothing are removed. His pulse is 145/min, respirations are 28/min, and blood pressure is 95/52 mm Hg. Pulmonary examination shows symmetric chest rise. The lungs are clear to auscultation. Abdominal examination shows no abnormalities. There are multiple shrapnel wounds over the upper and lower extremities. A tourniquet is in place around the right upper extremity; the right proximal forearm has been amputated. One large-bore intravenous catheter is placed in the left antecubital fossa. Despite multiple attempts, medical staff is unable to establish additional intravenous access. Which of the following is the most appropriate next step in management?
- A. Irrigate the shrapnel wounds
- B. Perform endotracheal intubation
- C. Establish intraosseous access (Correct Answer)
- D. Establish central venous access
- E. Replace the tourniquet with a pressure dressing
Clinical correlations of fascial spaces Explanation: ***Establish intraosseous access***
- The patient is in **hemorrhagic shock** (tachycardia, hypotension) and requires rapid fluid resuscitation, but peripheral intravenous access is difficult to obtain. **Intraosseous (IO) access** provides a rapid and reliable route for fluids and medications, especially in emergencies when IV access is challenging.
- IO access is a **bridge to definitive venous access** and is crucial for immediate life-saving interventions in trauma.
*Irrigate the shrapnel wounds*
- While wound irrigation is important for preventing infection, it is **not the immediate priority** when the patient is in hemorrhagic shock.
- Addressing the circulatory compromise takes precedence over local wound care.
*Perform endotracheal intubation*
- The patient is **alert and oriented** with symmetric chest rise and clear lungs, indicating he does not currently have an airway crisis requiring intubation.
- Intubation is an invasive procedure that carries risks and should only be performed when indicated for airway protection or respiratory failure.
*Establish central venous access*
- While central venous access is useful for long-term fluid management and monitoring, it is generally **more time-consuming and technically challenging** to establish than IO access, especially in an emergent, unstable patient.
- Given the urgency of rapid fluid administration, IO access is preferred as the immediate next step.
*Replace the tourniquet with a pressure dressing*
- The patient has an above-elbow amputation, suggesting significant injury, and the tourniquet is currently controlling the bleed. Removing the tourniquet prematurely without proximal surgical control can lead to **recurrent catastrophic hemorrhage**.
- A definitive surgical approach is needed to manage the amputation, not simply replacing the tourniquet with a pressure dressing, which may be insufficient to control arterial bleeding.
Clinical correlations of fascial spaces US Medical PG Question 3: A 7-month-old boy is brought to the ED by his mother because of abdominal pain. Two weeks ago, she noticed he had a fever and looser stools, but both resolved after a few days. One week ago, he began to experience periodic episodes during which he would curl up into a ball, scream, and cry. The episodes lasted a few minutes, and were occasionally followed by vomiting. Between events, he was completely normal. She says the episodes have become more frequent over time, and this morning, she noticed blood in his diaper. In the ED, his vitals are within normal ranges, and his physical exam is normal. After confirming the diagnosis with an abdominal ultrasound, what is the next step in management?
- A. Supportive care
- B. Broad-spectrum antibiotics
- C. Air contrast enema (Correct Answer)
- D. Abdominal laparotomy
- E. Abdominal CT scan
Clinical correlations of fascial spaces Explanation: ***Air contrast enema***
- An **air contrast enema** is both diagnostic and therapeutic for **intussusception**, which is strongly suggested by the patient's symptoms (colicky abdominal pain, drawing legs to chest, currant jelly stools).
- It uses air pressure to **reduce the intussusception**, avoiding surgery if successful and the bowel is not compromised.
*Supportive care*
- While supportive care (IV fluids, pain control) is important, it does not address the underlying mechanical issue of **intussusception** and would not resolve the condition.
- Delaying definitive treatment for intussusception can lead to **bowel ischemia, necrosis, and perforation**, which are life-threatening.
*Broad-spectrum antibiotics*
- Antibiotics are not the primary treatment for **intussusception**, as it is a mechanical obstruction, not typically a primary infection.
- They might be considered if there are signs of **perforation or peritonitis**, but the immediate goal is reduction.
*Abdominal laparotomy*
- An **abdominal laparotomy** is a surgical intervention reserved for cases where **non-operative reduction** (like an air enema) fails or if there are signs of **bowel perforation or gangrene**.
- It is not the *first-line* next step after diagnosis, especially if non-invasive options remain viable.
*Abdominal CT scan*
- An **abdominal CT scan** can diagnose intussusception but is typically not the preferred initial imaging because it involves **radiation exposure** and **does not offer therapeutic benefit**, unlike an air contrast enema.
- Abdominal ultrasound is usually sufficient for diagnosis and safer for pediatric patients.
Clinical correlations of fascial spaces US Medical PG Question 4: An experiment to determine the effects of gravity on blood pressure is conducted on 3 individuals of equal height and blood pressure oriented in different positions in space. Participant A is strapped in a supine position on a bed turned upside down in a vertical orientation with his head towards the floor and his feet towards the ceiling. Participant B is strapped in a supine position on a bed turned downwards in a vertical orientation with his head towards the ceiling and his feet just about touching the floor. Participant C is strapped in a supine position on a bed in a horizontal orientation. Blood pressure readings are then taken at the level of the head, heart, and feet from all 3 participants. Which of these positions will have the lowest recorded blood pressure reading?
- A. Participant B: at the level of the feet
- B. Participant A: at the level of the head
- C. Participant C: at the level of the heart
- D. Participant A: at the level of the feet (Correct Answer)
- E. Participant C: at the level of the feet
Clinical correlations of fascial spaces Explanation: ***Participant A: at the level of the feet***
- In Participant A, the feet are positioned **highest vertically** relative to the heart and are also above the head due to the upside-down vertical orientation. Due to gravity, blood pressure decreases with increasing height above the heart.
- This position would result in the lowest hydrostatic pressure at the feet, leading to the **lowest recorded blood pressure reading**.
*Participant B: at the level of the feet*
- In Participant B, the feet are positioned **below the heart** (towards the floor) in a vertical orientation.
- This position would experience some of the **highest hydrostatic pressure** due to gravity, leading to a high blood pressure reading, not the lowest.
*Participant A: at the level of the head*
- In Participant A, the head is positioned **below the heart** (towards the floor) in an upside-down vertical orientation.
- This position would experience increased hydrostatic pressure, hence a **higher blood pressure** compared to the feet.
*Participant C: at the level of the heart*
- Participant C is in a horizontal position, meaning all body parts are at roughly the same hydrostatic level relative to the heart.
- Blood pressure readings would be **similar across all points** (head, heart, feet) and would reflect the systemic arterial pressure without significant hydrostatic effects, thus not the lowest compared to other extreme positions.
*Participant C: at the level of the feet*
- In Participant C (horizontal), the feet are at approximately the **same hydrostatic level** as the heart.
- The reading at the feet in this position would be close to the **baseline arterial pressure**, not the lowest, as there's minimal hydrostatic gradient.
Clinical correlations of fascial spaces US Medical PG Question 5: A 14-year-old boy is brought to the emergency department because of acute left-sided chest pain and dyspnea following a motor vehicle accident. His pulse is 122/min and blood pressure is 85/45 mm Hg. Physical examination shows distended neck veins and tracheal displacement to the right side. The left chest is hyperresonant to percussion and there are decreased breath sounds. This patient would most benefit from needle insertion at which of the following anatomical sites?
- A. 5th left intercostal space along the midclavicular line
- B. 8th left intercostal space along the posterior axillary line
- C. 2nd left intercostal space along the midclavicular line (Correct Answer)
- D. Subxiphoid space in the left sternocostal margin
- E. 5th left intercostal space along the midaxillary line
Clinical correlations of fascial spaces Explanation: ***2nd left intercostal space along the midclavicular line***
- The patient's symptoms (chest pain, dyspnea, hypotension, distended neck veins, tracheal deviation, hyperresonance, and decreased breath sounds on the left) are classic signs of a **tension pneumothorax**.
- Immediate treatment for **tension pneumothorax** involves needle decompression at the **2nd intercostal space** in the midclavicular line to relieve pressure and restore hemodynamic stability.
*5th left intercostal space along the midclavicular line*
- This location is typically used for **chest tube insertion** in a more controlled setting, not for emergent needle decompression of a tension pneumothorax.
- While it's a safe location for pleural access, it is not the **first-line site** for immediate life-saving decompression.
*8th left intercostal space along the posterior axillary line*
- This site is too low and posterior for effective needle decompression of a tension pneumothorax, which requires rapid access to the **apex of the lung**.
- It is more commonly used for **thoracentesis** to drain fluid from the pleural cavity.
*Subxiphoid space in the left sternocostal margin*
- This location is primarily used for **pericardiocentesis** to drain fluid from the pericardial sac in cases of cardiac tamponade.
- It is not appropriate for addressing a **pneumothorax**, which involves air in the pleural space.
*5th left intercostal space along the midaxillary line*
- This site is a common alternative for **chest tube insertion** but is not the preferred or most immediate site for needle decompression of a tension pneumothorax.
- While it offers pleural access, the **2nd intercostal space** anteriorly is chosen for expediency and safety in an emergency.
Clinical correlations of fascial spaces US Medical PG Question 6: A 35-year-old man is brought to the emergency department from a kitchen fire. The patient was cooking when boiling oil splashed on his exposed skin. His temperature is 99.7°F (37.6°C), blood pressure is 127/82 mmHg, pulse is 120/min, respirations are 12/min, and oxygen saturation is 98% on room air. He has dry, nontender, and circumferential burns over his arms bilaterally, burns over the anterior portion of his chest and abdomen, and tender spot burns with blisters on his shins. A 1L bolus of normal saline is administered and the patient is given morphine and his pulse is subsequently 80/min. A Foley catheter is placed which drains 10 mL of urine. What is the best next step in management?
- A. Additional fluids and escharotomy (Correct Answer)
- B. Escharotomy
- C. Continuous observation
- D. Moist dressings and discharge
- E. Additional fluids and admission to the ICU
Clinical correlations of fascial spaces Explanation: ***Additional fluids and escharotomy***
- The patient has **circumferential full-thickness burns** on both arms (dry, nontender), which require **escharotomy** to prevent compartment syndrome and vascular compromise to the limbs.
- The **oliguria** (10 mL urine output) despite a 1L fluid bolus indicates **inadequate fluid resuscitation** from burn shock. With approximately 40% TBSA burns, the patient requires aggressive fluid resuscitation per the Parkland formula (4 mL/kg/% TBSA), which would be approximately 11 liters in the first 24 hours. Adequate resuscitation targets urine output of 0.5-1 mL/kg/hr (35-70 mL/hr for this patient).
- Both interventions are immediately necessary: fluids for burn shock and escharotomy for circumferential burns.
*Escharotomy*
- While **escharotomy** is essential for the circumferential full-thickness burns to prevent compartment syndrome, it alone will not address the **severe fluid deficit** causing oliguria and hypoperfusion.
- The low urine output reflects systemic hypovolemia from burn shock, not just local compartment issues, requiring aggressive fluid resuscitation.
*Continuous observation*
- **Continuous observation** is inappropriate given the patient's critical findings: circumferential full-thickness burns requiring urgent escharotomy and oliguria indicating inadequate resuscitation.
- Delaying escharotomy can lead to irreversible ischemic damage to the limbs, and inadequate fluid resuscitation can progress to multiorgan failure.
*Moist dressings and discharge*
- This option is completely inappropriate for a patient with **extensive deep burns** (approximately 40% TBSA) including full-thickness injuries requiring hospitalization and specialized burn care.
- Discharge would lead to severe complications including infection, inadequate fluid resuscitation, compartment syndrome, and potential limb loss.
*Additional fluids and admission to the ICU*
- While ICU admission and additional fluids are necessary components of care, this option is **incomplete** because it omits **escharotomy**, which is urgently needed for the circumferential full-thickness burns.
- Escharotomy is a time-sensitive procedure that must be performed promptly to prevent ischemic injury to the limbs from vascular compromise.
Clinical correlations of fascial spaces US Medical PG Question 7: A 23-year-old patient presents to the emergency department after a motor vehicle accident. The patient was an unrestrained driver involved in a head-on collision. The patient is heavily intoxicated on what he claims is only alcohol. An initial trauma assessment is performed, and is notable for significant bruising of the right forearm. The patient is in the trauma bay, and complains of severe pain in his right forearm. A physical exam is performed and is notable for pallor, decreased sensation, and cool temperature of the skin of the right forearm. Pain is elicited upon passive movement of the right forearm and digits. A thready radial pulse is palpable. A FAST exam is performed, and is negative for signs of internal bleeding. The patient's temperature is 99.5°F (37.5°C), pulse is 100/min, blood pressure is 110/70 mmHg, respirations are 12/min, and oxygen saturation is 98% on room air. Radiography of the right forearm is ordered. The patient is still heavily intoxicated. Which of the following is the best next step in management?
- A. Fasciotomy (Correct Answer)
- B. IV fluids
- C. Analgesics
- D. Pressure measurement
- E. Detoxification
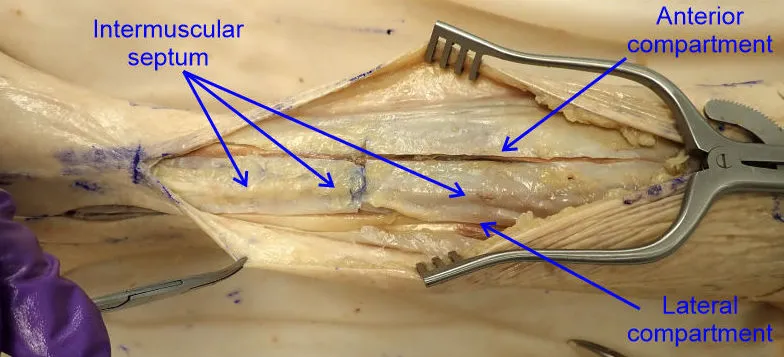
Clinical correlations of fascial spaces Explanation: ***Fasciotomy***
- The patient exhibits classic signs of **acute compartment syndrome**, including severe pain out of proportion to injury, pain on passive stretch, pallor, decreased sensation, and cool extremity, despite a palpable pulse. These symptoms necessitate immediate surgical intervention to relieve pressure.
- A **fasciotomy** is the definitive treatment for acute compartment syndrome to prevent irreversible muscle and nerve damage, and potentially limb loss.
*IV fluids*
- While fluid resuscitation is important in trauma, the patient's current vital signs (BP 110/70 mmHg, pulse 100/min) do not indicate immediate shock requiring aggressive IV fluid administration over addressing the limb-threatening compartment syndrome.
- Prioritizing IV fluids without addressing **compartment syndrome** could lead to permanent loss of limb function.
*Analgesics*
- Administering analgesics might mask the escalating pain a key symptom of compartment syndrome, which could delay diagnosis and definitive treatment.
- While pain control is important, it should not supersede measures to prevent irreversible tissue damage.
*Pressure measurement*
- While compartment pressure measurement can confirm the diagnosis of compartment syndrome, the clinical presentation in this case is so compelling that delaying definitive treatment for pressure measurement is not the best next step.
- Clinical signs and symptoms are often sufficient for diagnosis, and surgical intervention should not be deferred pending pressure readings in clear-cut cases.
*Detoxification*
- Detoxification for alcohol intoxication is not an emergent and immediate priority in comparison to the limb-threatening condition of acute compartment syndrome.
- Addressing the **compartment syndrome** is critical for preserving limb viability, whereas detoxification can be managed once acute medical emergencies are controlled.
Clinical correlations of fascial spaces US Medical PG Question 8: A previously healthy 33-year-old woman comes to the physician because of pain and sometimes numbness in her right thigh for the past 2 months. She reports that her symptoms are worse when walking or standing and are better while sitting. Three months ago, she started going to a fitness class a couple times a week. She is 163 cm (5 ft 4 in) tall and weighs 88 kg (194 lb); BMI is 33.1 kg/m2. Her vital signs are within normal limits. Examination of the skin shows no abnormalities. Sensation to light touch is decreased over the lateral aspect of the right anterior thigh. Muscle strength is normal. Tapping the right inguinal ligament leads to increased numbness of the affected thigh. The straight leg test is negative. Which of the following is the most appropriate next step in management of this patient?
- A. Advise patient to wear looser pants (Correct Answer)
- B. Reduction of physical activity
- C. MRI of the lumbar spine
- D. X-ray of the hip
- E. Blood work for inflammatory markers
Clinical correlations of fascial spaces Explanation: ***Advise patient to wear looser pants***
- This patient presents with symptoms consistent with **meralgia paresthetica**, a condition caused by compression of the **lateral femoral cutaneous nerve (LFCN)**. Modifying clothing or belts that compress the inguinal ligament can relieve pressure on the nerve.
- Her increased weight, a recent increase in physical activity, and a positive Tinel's sign at the inguinal ligament (tapping leads to increased numbness) support this diagnosis.
*Reduction of physical activity*
- While excessive physical activity can contribute to meralgia paresthetica, simply reducing it without addressing the underlying compression might not fully resolve symptoms.
- The patient has recently increased physical activity, which could be a contributing factor, but it's not the primary or most direct intervention for nerve compression.
*MRI of the lumbar spine*
- An MRI of the lumbar spine would be considered if there were signs of **radiculopathy** or other spinal pathology, such as weakness, reflex changes, or a positive straight leg test, which are absent here.
- The symptoms are localized to the distribution of the LFCN, and the physical exam points away from a central spinal cause.
*X-ray of the hip*
- An X-ray of the hip would be indicated for suspected **hip joint pathology** or **bony abnormalities**, which are not suggested by the patient's symptoms (pain and numbness in the thigh, not hip joint pain).
- Meralgia paresthetica is a nerve entrapment syndrome, not a structural issue of the hip joint.
*Blood work for inflammatory markers*
- Inflammatory markers like **ESR** or **CRP** would be relevant if an **inflammatory arthritis**, infection, or systemic inflammatory condition was suspected, but the patient's symptoms are purely neurological and localized.
- There is no clinical evidence of inflammation, fever, or joint swelling to suggest an underlying inflammatory process.
Clinical correlations of fascial spaces US Medical PG Question 9: A 72-year-old male presents to a cardiac surgeon for evaluation of severe aortic stenosis. He has experienced worsening dyspnea with exertion over the past year. The patient also has a history of poorly controlled hypertension, diabetes mellitus, and hyperlipidemia. An echocardiogram revealed a thickened calcified aortic valve. The surgeon is worried that the patient will be a poor candidate for open heart surgery and decides to perform a less invasive transcatheter aortic valve replacement. In order to perform this procedure, the surgeon must first identify the femoral pulse just inferior to the inguinal ligament and insert a catheter into the vessel in order to gain access to the arterial system. Which of the following structures is immediately lateral to this structure?
- A. Lymphatic vessels
- B. Femoral vein
- C. Sartorius muscle
- D. Pectineus muscle
- E. Femoral nerve (Correct Answer)
Clinical correlations of fascial spaces Explanation: ***Femoral nerve***
- The **femoral nerve** lies lateral to the **femoral artery** within the **femoral triangle**.
- The order of structures from **lateral to medial** under the inguinal ligament is remembered by the mnemonic **NAVEL**: **N**erve, **A**rtery, **V**ein, **E**mpty space, **L**ymphatics.
*Lymphatic vessels*
- **Lymphatic vessels** and nodes are located most medially within the femoral triangle, medial to the femoral vein.
- This position is not immediately lateral to the femoral artery.
*Femoral vein*
- The **femoral vein** is located immediately medial to the **femoral artery**.
- It would not be found immediately lateral to the femoral artery.
*Sartorius muscle*
- The **sartorius muscle** forms the lateral boundary of the **femoral triangle** but is not immediately adjacent and lateral to the femoral artery within the triangle itself.
- The femoral nerve is enclosed within the iliopsoas fascial compartment, which runs deep to the sartorius.
*Pectineus muscle*
- The **pectineus muscle** forms part of the floor of the **femoral triangle**, but it is deep to the neurovascular structures.
- It is not immediately lateral to the femoral artery.
Clinical correlations of fascial spaces US Medical PG Question 10: Arrange in sequence the structures involved in the direct pathway (1=Striatum, 2=GPi, 3=Thalamus, 4=Cortex output, 5=Cortex input):-
- A. 1,3,4,2,5
- B. 5,1,2,3,4 (Correct Answer)
- C. 1,2,3,4,5
- D. 5,4,2,3,1
- E. 5,1,3,2,4
Clinical correlations of fascial spaces Explanation: ***5,1,2,3,4***
- The direct pathway of the basal ganglia begins with the **cortex** (5) sending excitatory signals to the **striatum** (1).
- The striatum then inhibits the **internal globus pallidus (GPi)** (2), which disinhibits the **thalamus** (3), leading to excitation of the **cortex** (4).
- This is the correct sequence: **Cortex input → Striatum → GPi → Thalamus → Cortex output**.
*1,3,4,2,5*
- This sequence is incorrect as it starts with the striatum instead of cortical input.
- The direct pathway does not begin with striatal activity; the cortex must first activate the striatum.
*1,2,3,4,5*
- This order is incorrect because it implies the pathway starts at the striatum rather than the cortex.
- The cortex should be the starting point (5) and the ending point (4) of the motor loop.
*5,4,2,3,1*
- This sequence is incorrect as it places cortex output (4) before the striatum receives input.
- This reverses the functional flow and does not follow the **disinhibitory mechanism** of the direct pathway.
*5,1,3,2,4*
- This sequence incorrectly places the thalamus (3) before the GPi (2).
- In the direct pathway, the striatum must first inhibit the GPi before the thalamus can be disinhibited.
More Clinical correlations of fascial spaces US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.