Specialized epithelial junctions US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Specialized epithelial junctions. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Specialized epithelial junctions US Medical PG Question 1: A scientist is studying a protein that is present on the plasma membrane of cells. He therefore purifies the protein in a lipid bilayer and subjects it to a number of conditions. His investigations show that the protein has the following properties:
1) It is able to change ion concentrations across the membrane without addition of ATP to the solution.
2) Its activity increases linearly with substrate concentration without any saturation even at mildly supraphysiologic conditions.
3) In some states the protein leads to an ion concentration change; whereas, it has no effect in other states.
4) Changing the electrical charge across the membrane does not affect whether the protein has activity.
5) Adding a small amount of an additional substance to the solution reliably increases the protein's activity.
These findings are consistent with a protein with which of the following functions?
- A. Maintenance of resting sodium and potassium concentrations
- B. Transporting water in the collecting duct of the kidney
- C. Reabsorption of glucose in the proximal kidney tubule
- D. Mediating neuronal to muscle end plate communication (Correct Answer)
- E. Causing depolarization during action potentials
Specialized epithelial junctions Explanation: **Mediating neuronal to muscle end plate communication**
- The properties described align with **ligand-gated ion channels**, which mediate communication at the neuromuscular junction. These channels open in response to a **neurotransmitter** (the "additional substance"), allowing ion flow without direct ATP hydrolysis.
- The "some states" where it has no effect and "other states" where it leads to ion concentration change refer to its closed and open conformational states, dependent on ligand binding. The lack of saturation and independence from electrical charge are features of some channel kinetics.
*Maintenance of resting sodium and potassium concentrations*
- This function is primarily carried out by the **Na+/K+ ATPase pump**, which is an **active transporter** requiring ATP hydrolysis for its function, contradicting property (1).
- The Na+/K+ ATPase transports ions against their concentration gradients and would be affected by changes in ATP availability.
*Reabsorption of glucose in the proximal kidney tubule*
- Glucose reabsorption primarily involves **Na+-glucose cotransporters (SGLTs)**, which are secondary active transporters. While they don't directly use ATP, their activity is linked to the Na+ gradient maintained by Na+/K+ ATPase, and they can show saturation kinetics.
- SGLTs are symporters that move glucose and Na+ in the same direction and exhibit saturation at high glucose concentrations.
*Transporting water in the collecting duct of the kidney*
- Water transport in the collecting duct is mediated by **aquaporins**, which are passive water channels. Their activity is regulated by **vasopressin** (ADH), but they primarily transport water, not ions.
- Aquaporins do not typically impact ion concentrations directly and their activity is usually quite specific to water movement.
*Causing depolarization during action potentials*
- Depolarization during action potentials is caused by the opening of **voltage-gated sodium channels**. These channels are directly affected by changes in **electrical charge** across the membrane, contradicting property (4).
- Voltage-gated channels exhibit specific thresholds for activation and inactivation based on membrane potential.
Specialized epithelial junctions US Medical PG Question 2: A 22-year-old woman presents to the emergency department with a 2-day history of severe blistering. She says that she woke up 2 days ago with a number of painful blisters in her mouth and has since been continuing to develop blisters of her cutaneous skin all over her body and the mucosa of her mouth. She has no past medical history and has never experienced these symptoms before. Physical exam reveals a diffuse vesicular rash with painful, flaccid blisters that separate easily with gentle rubbing. The function of which of the following proteins is most likely disrupted in this patient?
- A. T-cell receptor
- B. Cadherin (Correct Answer)
- C. Keratin
- D. Collagen
- E. Integrin
Specialized epithelial junctions Explanation: ***Cadherin***
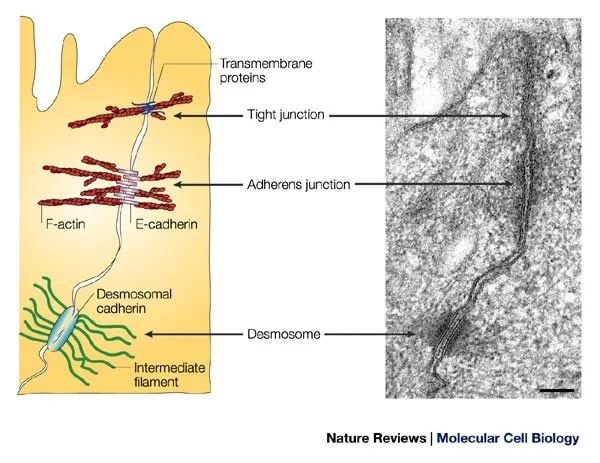
- The patient's presentation with **diffuse flaccid blisters** that separate easily with gentle rubbing (a positive **Nikolsky sign**) and **oral mucosal involvement** is highly suggestive of **pemphigus vulgaris**.
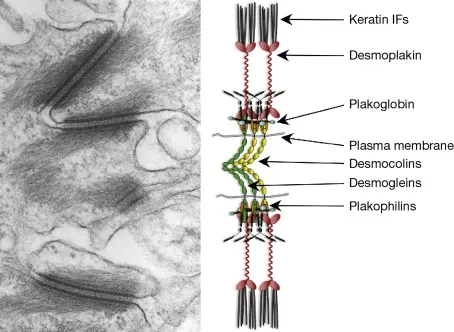
- **Pemphigus vulgaris** is an autoimmune blistering disease where autoantibodies target **desmoglein 1 and 3**, which are types of **cadherin cell adhesion proteins** responsible for cell-to-cell adhesion in the epidermis. Their disruption leads to **intraepidermal blistering**.
*T-cell receptor*
- **T-cell receptors** are involved in immune recognition and T-cell activation, but their primary disruption is not directly responsible for the blistering seen in pemphigus vulgaris, which is mediated by **autoantibodies against desmogleins**.
- Conditions involving T-cell receptor dysfunction typically manifest as **immunodeficiencies**, **autoimmune responses** directed at self-antigens via cellular immunity, or **lymphomas**, not primary blistering diseases of this type.
*Keratin*
- **Keratin** is an intermediate filament protein that provides structural integrity to epithelial cells. While disruptions in keratin can lead to blistering disorders (e.g., **epidermolysis bullosa simplex**), these often present with **intact, tense blisters** (due to basal cell layer separation) or mechanical fragility, unlike the flaccid blisters of pemphigus vulgaris.
- **Genetic defects in keratin** would typically present earlier in life and are not usually associated with an autoimmune mechanism causing acute onset flaccid blistering.
*Collagen*
- **Collagen** is a primary component of the extracellular matrix and is crucial for skin strength and integrity. Disorders involving collagen, such as **epidermolysis bullosa acquisita** or certain types of **dystrophic epidermolysis bullosa**, typically disrupt the **dermal-epidermal junction**, leading to **subepidermal blistering** and often **scarring**.
- The flaccid, intraepidermal blisters and positive Nikolsky sign described are not characteristic of collagen-related blistering disorders.
*Integrin*
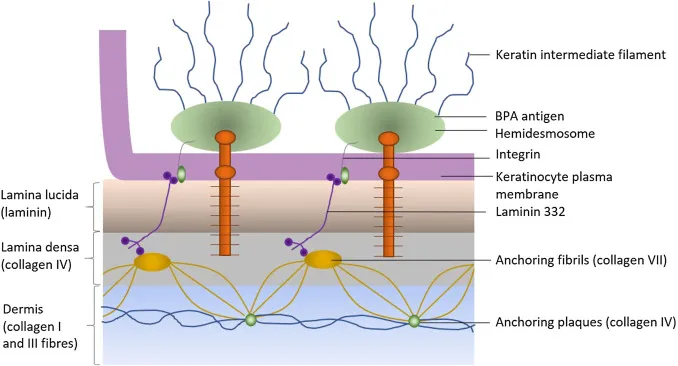
- **Integrins** are cell surface receptors involved in cell-to-extracellular matrix adhesion, particularly in forming **hemidesmosomes** that anchor basal keratinocytes to the basement membrane.
- Disruption of integrins or other hemidesmosomal components (e.g., in **bullous pemphigoid**) leads to **subepidermal blistering**, where blisters are typically tense and do not easily rupture with gentle pressure, which is distinct from the flaccid blisters of pemphigus vulgaris.
Specialized epithelial junctions US Medical PG Question 3: A researcher is studying proteins that contribute to intestinal epithelial permeability. He has isolated intestinal tissue from several mice. After processing the tissue into its individual components, he uses a Western blot analysis to identify a protein that forms part of a multi-protein complex at the apical aspect of epithelial cells. The complex is known to provide a diffusion barrier between the apical and basolateral aspects of epithelial cells. Which of the following proteins is this researcher most likely investigating?
- A. Integrin
- B. Connexon
- C. Desmoglein
- D. E-cadherin
- E. Claudin (Correct Answer)
Specialized epithelial junctions Explanation: ***Claudin***
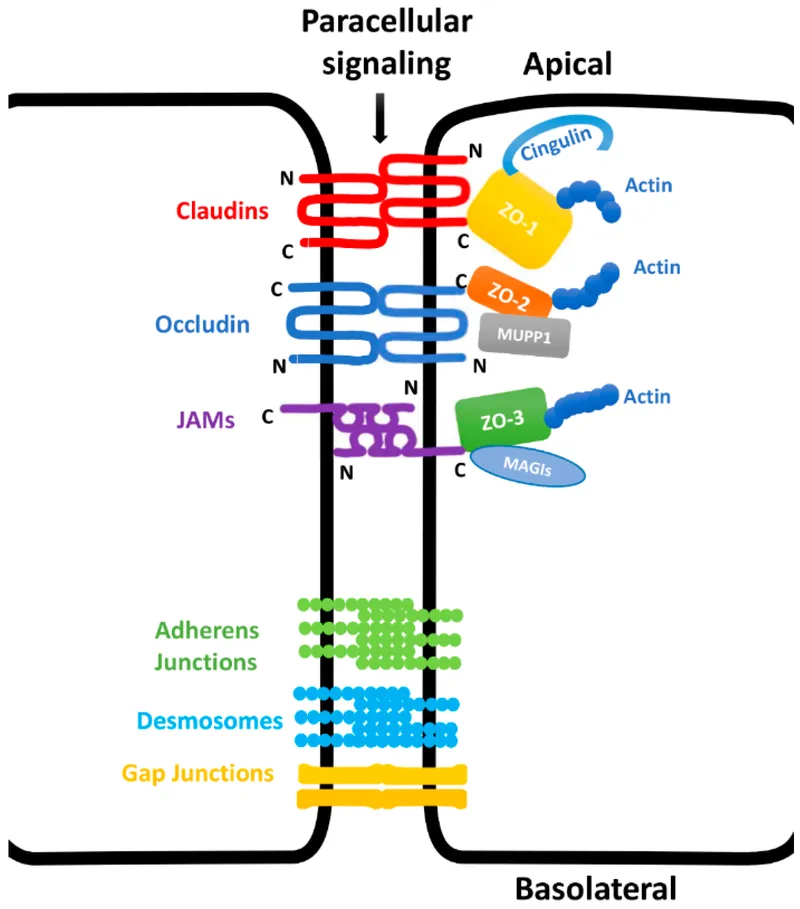
- **Claudins** are integral membrane proteins that are primary components of **tight junctions** (zonulae occludentes), which form a diffusion barrier at the **apical aspect** of epithelial cells.
- They regulate **paracellular permeability**, crucial for maintaining the integrity of the intestinal epithelial barrier.
*Integrin*
- **Integrins** are transmembrane receptors that mediate cell-extracellular matrix (ECM) adhesion and cell-cell adhesion, but they are not the primary components of tight junction diffusion barriers.
- They are involved in cell signaling and structural support, rather than forming a direct paracellular seal.
*Connexon*
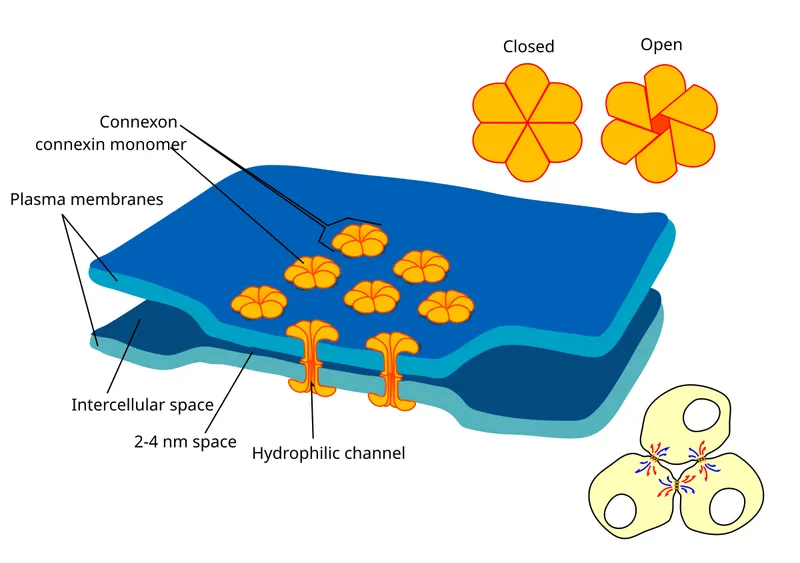
- A **connexon** is a protein assembly that forms a **gap junction**, allowing direct communication and passage of small molecules between adjacent cells.
- Gap junctions facilitate intercellular communication, but do not primarily contribute to sealing the paracellular space as a diffusion barrier.
*Desmoglein*
- **Desmoglein** is a cadherin family protein found in **desmosomes** (maculae adherens), which are cell-cell adhesion complexes that provide strong mechanical attachments between cells.
- Desmosomes resist shearing forces and provide structural integrity but do not regulate paracellular permeability as tight junctions do.
*E-cadherin*
- **E-cadherin** is a crucial component of **adherens junctions** (zonula adherens), which provide cell-cell adhesion and help establish and maintain cell polarity.
- While important for epithelial integrity, E-cadherin primarily links cells to the actin cytoskeleton and is not directly responsible for forming the selective diffusion barrier itself.
Specialized epithelial junctions US Medical PG Question 4: A 58-year-old woman presents with tense bullae on an erythematous base, primarily affecting her trunk and extremities. The lesions developed over the past 3 weeks. Nikolsky sign is negative. Skin biopsy shows subepidermal bullae with eosinophilic infiltrate. Direct immunofluorescence shows linear deposits of IgG and C3 at the basement membrane zone. Which of the following is the target antigen in this condition?
- A. Type IV collagen
- B. BP180/BP230 (Correct Answer)
- C. Type VII collagen
- D. Desmoglein-3
Specialized epithelial junctions Explanation: ***BP180/BP230***
- The clinical presentation of **tense bullae**, negative **Nikolsky sign**, subepidermal bullae with **eosinophilic infiltrate**, and **linear IgG and C3 deposition at the basement membrane zone** are classic features of **bullous pemphigoid**.
- **BP180** (also known as type XVII collagen) and **BP230** are hemidesmosomal proteins that serve as the primary target antigens in bullous pemphigoid.
*Type IV collagen*
- **Type IV collagen** is a major component of the **basement membrane**, but it is not the target antigen in bullous pemphigoid.
- Antibodies against type IV collagen may be involved in **Goodpasture syndrome**, which affects the kidneys and lungs, not primarily the skin in this manner.
*Type VII collagen*
- **Type VII collagen** is found in the **anchoring fibrils** beneath the basement membrane.
- Antibodies against **type VII collagen** are characteristic of **epidermolysis bullosa acquisita**, which typically presents with **fragile skin, trauma-induced blistering**, and scarring, differentiating it from this case.
*Desmoglein-3*
- **Desmoglein-3** is a **desmosomal protein** that is a primary target antigen in **pemphigus vulgaris**, especially the **mucosal dominant form**.
- **Pemphigus vulgaris** is characterized by **flaccid bullae, painful erosions**, and a **positive Nikolsky sign**, which are not consistent with the patient's presentation.
Specialized epithelial junctions US Medical PG Question 5: A 78-year-old man receives chemotherapy for advanced hepatocellular carcinoma. Despite appropriate therapy, he dies 4 months later. Histopathological examination of the cancer cells shows the presence of a transmembrane efflux pump protein that is known to cause decreased intracellular concentrations of chemotherapeutic drugs. Which of the following best describes this membrane protein?
- A. G protein
- B. Cadherin
- C. P-glycoprotein (Correct Answer)
- D. Tyrosine receptor
- E. Channel protein
Specialized epithelial junctions Explanation: **P-glycoprotein**
- **P-glycoprotein** (also known as **MDR1**) is a well-known **efflux pump** that actively transports many chemotherapy drugs out of cancer cells, leading to **multidrug resistance**.
- Its presence explains the **decreased intracellular concentrations** of chemotherapy drugs and the poor response to treatment in this patient.
*G protein*
- **G proteins** are intracellular signaling molecules that mediate responses to various extracellular stimuli, not primarily involved in drug efflux.
- They are typically associated with **G protein-coupled receptors** and downstream signaling pathways, not direct drug transport.
*Cadherin*
- **Cadherins** are cell adhesion molecules that play a crucial role in cell-cell binding and maintaining tissue structure.
- They are not involved in the active transport of drugs across the cell membrane.
*Tyrosine receptor*
- **Tyrosine kinase receptors** are transmembrane proteins that bind to growth factors and initiate intracellular signaling cascades, promoting cell growth and differentiation.
- They are involved in signaling, not in the active transport of chemotherapy drugs out of the cell.
*Channel protein*
- **Channel proteins** facilitate the passive diffusion of ions or small molecules across the cell membrane, typically down their electrochemical gradient.
- While they are transmembrane proteins, they do not actively pump drugs out against a concentration gradient, which is characteristic of multidrug resistance.
Specialized epithelial junctions US Medical PG Question 6: A 3-month-old infant presents with severe joint hypermobility, skin hyperextensibility, and delayed wound healing. Skin biopsy shows abnormal collagen fibril organization with irregular diameter and reduced tensile strength. Genetic testing reveals a mutation affecting lysyl hydroxylase, an enzyme involved in collagen post-translational modification. The family asks about prognosis and potential complications. Synthesize the biochemical defect with clinical manifestations to determine the most critical pathophysiological mechanism.
- A. Impaired collagen synthesis at the ribosomal level
- B. Defective hydroxylation of lysine residues preventing stable collagen cross-linking (Correct Answer)
- C. Excessive collagen degradation by matrix metalloproteinases
- D. Abnormal glycosylation affecting collagen secretion
- E. Impaired procollagen cleavage preventing fibril formation
Specialized epithelial junctions Explanation: ***Defective hydroxylation of lysine residues preventing stable collagen cross-linking***
- **Lysyl hydroxylase** is essential for the post-translational hydroxylation of lysine; its deficiency impairs the formation of **hydroxylysine**, which is crucial for stable **covalent cross-linking**.
- This biochemical defect results in **reduced tensile strength** of collagen fibrils, leading to the classic clinical triad of **joint hypermobility**, **skin hyperextensibility**, and **delayed wound healing** seen in Kyphoscoliotic Ehlers-Danlos Syndrome.
*Impaired collagen synthesis at the ribosomal level*
- Ribosomal synthesis pertains to the translation of **pre-procollagen** alpha chains; however, this patient has a post-translational enzyme mutation.
- Defects at the **ribosomal level** would lead to a quantitative lack of protein rather than the **abnormal fibril organization** and diameter irregularities described.
*Excessive collagen degradation by matrix metalloproteinases*
- **Matrix metalloproteinases (MMPs)** are involved in tissue remodeling and chronic inflammation, not primary genetic collagen disorders.
- While MMP activity can affect tissue integrity, the clinical presentation and **genetic testing** specifically point to a synthesis/modification defect, not an overactive degradation pathway.
*Abnormal glycosylation affecting collagen secretion*
- **Glycosylation** occurs on hydroxylysine residues in the Golgi apparatus; while related to post-translational modification, it is not the primary function of **lysyl hydroxylase**.
- Primary defects in collagen **glycosylation** or **secretion** usually present with more severe multi-systemic growth delays rather than the specific mechanical fragility seen here.
*Impaired procollagen cleavage preventing fibril formation*
- This mechanism describes **Arthrochalasia** or **Dermatosparaxis** types of EDS, where **procollagen N-peptidase** or C-peptidase is deficient.
- Failure to cleave **terminal propeptides** prevents the formation of insoluble tropocollagen, but this is distinct from the **lysyl hydroxylase** deficiency identified by this patient's genetic testing.
Specialized epithelial junctions US Medical PG Question 7: A 58-year-old woman undergoes cervical biopsy following an abnormal Pap smear. Histology shows full-thickness epithelial atypia with loss of cellular polarity, increased nuclear-to-cytoplasmic ratio, and numerous mitotic figures, but the basement membrane remains intact. Her oncologist discusses treatment options. The patient is concerned about progression risk versus overtreatment. Evaluate the most appropriate management strategy considering the tissue diagnosis and natural history.
- A. Observation only as basement membrane is intact
- B. Excisional procedure (LEEP or cone biopsy) with close surveillance (Correct Answer)
- C. Immediate radical hysterectomy
- D. Radiation therapy to prevent invasion
- E. Chemotherapy followed by reassessment
Specialized epithelial junctions Explanation: ***Excisional procedure (LEEP or cone biopsy) with close surveillance***
- The histology describes **CIN 3 (full-thickness atypia)**; since the **basement membrane is intact**, it is a high-grade pre-invasive lesion requiring definitive treatment to prevent progression to invasive cancer.
- An **excisional procedure** like **LEEP** or **cone biopsy** is the standard management to both treat the lesion and provide a complete specimen for histological review to rule out occult invasion.
*Observation only as basement membrane is intact*
- Observation is inappropriate for **CIN 3** because the risk of spontaneous progression to **invasive carcinoma** is significantly high.
- **Full-thickness atypia** necessitates active intervention, unlike lower-grade lesions (CIN 1) which may be monitored via surveillance.
*Immediate radical hysterectomy*
- A **radical hysterectomy** is considered overtreatment for a diagnosis where the **basement membrane is intact** (carcinoma in situ/CIN 3).
- Such invasive surgery is reserved for confirmed **invasive cervical cancer** cases, not for pre-invasive lesions that can be managed by local excision.
*Radiation therapy to prevent invasion*
- **Radiation therapy** is not indicated for **pre-invasive lesions** and is associated with significant long-term morbidity in the pelvic region.
- Primary management for **HSIL/CIN 3** is surgical excision, reserving radiation for higher-stage **invasive malignancies**.
*Chemotherapy followed by reassessment*
- There is no clinical role for **neoadjuvant chemotherapy** in the management of **cervical intraepithelial neoplasia (CIN)**.
- Management is strictly **surgical (excisional or ablative)** to remove the dysplastic cells before they can acquire the ability to invade the stroma.
Specialized epithelial junctions US Medical PG Question 8: A 42-year-old woman with Marfan syndrome presents to the emergency department with acute chest pain. CT angiography reveals a Type A aortic dissection. The cardiothoracic surgeon explains that her underlying connective tissue disorder predisposed her to this complication. During surgery, the aortic wall appears thin and fragile. Evaluate which molecular defect best explains the compromised structural integrity of her aortic wall.
- A. Deficient type I collagen synthesis reducing tensile strength
- B. Abnormal fibrillin-1 causing defective elastic fiber assembly and excessive TGF-β signaling (Correct Answer)
- C. Excessive collagenase activity degrading structural proteins
- D. Impaired proteoglycan synthesis reducing ground substance
- E. Defective type IV collagen affecting basement membrane stability
Specialized epithelial junctions Explanation: ***Abnormal fibrillin-1 causing defective elastic fiber assembly and excessive TGF-β signaling***
- **Marfan syndrome** results from mutations in the **FBN1 gene**, which codes for **fibrillin-1**, a glycoprotein that serves as a scaffold for **elastin** in the extracellular matrix.
- Defects in fibrillin-1 lead to impaired **microfibril** assembly and increased **TGF-β** bioavailability, causing **cystic medial necrosis** and structural failure of the aortic wall.
*Deficient type I collagen synthesis reducing tensile strength*
- This defect is the hallmark of **Osteogenesis Imperfecta**, which presents with **fragile bones**, blue sclerae, and hearing loss.
- While **Type I collagen** provides tensile strength to many tissues, it is not the primary molecular deficit responsible for the aortic fragility seen in **Marfan syndrome**.
*Excessive collagenase activity degrading structural proteins*
- Excessive **matrix metalloproteinase (MMP)** activity can contribute to tissue remodeling, but it is a secondary process rather than the primary genetic defect.
- This mechanism is more associated with inflammatory conditions or the late stages of **atherosclerotic aneurysm** formation rather than Marfan-specific dissection.
*Impaired proteoglycan synthesis reducing ground substance*
- While the aortic media in Marfan syndrome shows an accumulation of **glycosaminoglycans** (mucoid material), this is a result of the pathology (**cystic medial necrosis**) rather than impaired synthesis.
- Proteoglycans normally provide compressive strength, and their reduction is not the root cause of the **elastic fiber** fragmentation seen in this patient.
*Defective type IV collagen affecting basement membrane stability*
- Mutations in **Type IV collagen** are characteristic of **Alport syndrome**, which primarily affects the **glomerular basement membrane**, eyes, and inner ear.
- Type IV collagen is a major component of **basement membranes** and does not play a chief role in the large-vessel structural integrity of the **aortic media**.
Specialized epithelial junctions US Medical PG Question 9: A 67-year-old man undergoes tracheal reconstruction following long-term intubation injury. The surgeon explains that the graft must replicate the normal tracheal epithelium to maintain proper mucociliary clearance. Biopsy of normal trachea shows tall columnar cells with cilia, interspersed goblet cells, and small basal cells, all appearing to reach the basement membrane at different levels. Analyze which histological feature is most critical for proper graft function.
- A. Maintenance of pseudostratified architecture with ciliated cells and goblet cells (Correct Answer)
- B. Simple columnar epithelium for efficient secretion
- C. Stratified squamous epithelium for protection against air flow
- D. Keratinized epithelium for durability
- E. Transitional epithelium for distensibility during breathing
Specialized epithelial junctions Explanation: ***Maintenance of pseudostratified architecture with ciliated cells and goblet cells***
- The respiratory tract is lined by **pseudostratified ciliated columnar epithelium**, which is crucial for the **mucociliary escalator** to trap and remove foreign particles.
- The biopsy description confirms that all cells touch the **basement membrane** but appear at different heights, a histological hallmark necessary for **epithelial regeneration** via basal cells and secretion via goblet cells.
*Simple columnar epithelium for efficient secretion*
- This tissue consists of a single layer of uniform tall cells and is typically found in the **digestive tract**, not the trachea.
- It lacks the **basal stem cells** and specialized architecture required for the high-turnover environment and **clearance mechanisms** of the respiratory system.
*Stratified squamous epithelium for protection against air flow*
- Although durable, this epithelium would represent **squamous metaplasia** in the trachea, often seen in chronic smokers.
- It lacks **cilia and goblet cells**, which would lead to a failure of **mucociliary clearance** and persistent lung infections.
*Keratinized epithelium for durability*
- **Keratinization** is a feature of the **epidermis (skin)** designed to prevent desiccation and provide a physical barrier.
- In the trachea, keratinized tissue would be dysfunctional as it cannot produce **mucus** or facilitate the movement of debris via **ciliary action**.
*Transitional epithelium for distensibility during breathing*
- This specialized epithelium is unique to the **urinary tract** (urothelium) and allows for significant stretching.
- It does not possess the **cilia** necessary for airway hygiene and is not structurally suited for the **respiratory mucosa**.
Specialized epithelial junctions US Medical PG Question 10: A 4-year-old boy presents with multiple bone fractures from minor trauma, blue sclerae, and hearing loss. Genetic testing reveals a COL1A1 mutation affecting type I collagen synthesis. Bone biopsy shows thin, disorganized collagen fibrils. His parents ask about the prognosis and potential complications. Analyze the relationship between the molecular defect and clinical manifestations.
- A. Defective mineralization causes bone fragility despite normal collagen structure
- B. Abnormal type I collagen structure compromises tensile strength in multiple connective tissues (Correct Answer)
- C. Impaired osteoblast differentiation reduces bone formation
- D. Excessive osteoclast activity causes accelerated bone resorption
- E. Deficient proteoglycan synthesis weakens bone matrix
Specialized epithelial junctions Explanation: ***Abnormal type I collagen structure compromises tensile strength in multiple connective tissues***
- The **COL1A1 mutation** leads to an autosomal dominant defect in **type I collagen**, the predominant protein in **bone, teeth, and sclera**, reducing its quantity or quality.
- This molecular defect results in decreased **tensile strength** of the bone matrix, causing multiple fractures, while the thin sclera reveals the **underlying blue choroid**.
*Defective mineralization causes bone fragility despite normal collagen structure*
- This describes **Osteomalacia** or **Rickets**, where collagen is normal but **hydroxyapatite** deposition is impaired due to Vitamin D or phosphate deficiency.
- Unlike **Osteogenesis Imperfecta**, these conditions do not typically present with **blue sclerae** or specific collagen gene mutations.
*Impaired osteoblast differentiation reduces bone formation*
- Reduced osteoblast activity is characteristic of conditions like **Osteoporosis** or age-related bone loss, rather than a qualitative collagen defect.
- While **bone density** may be low, the primary issue in this patient is the **structural integrity** of the matrix components produced, not the differentiation of the lineage.
*Excessive osteoclast activity causes accelerated bone resorption*
- This mechanism is the hallmark of **Paget's disease of bone** or hyperparathyroidism, which affects bone remodeling cycles.
- **Osteogenesis Imperfecta** is primarily a **biosynthetic defect** of the matrix (the "bricks" of the bone), not a primary overactivity of the bone-resorbing cells.
*Deficient proteoglycan synthesis weakens bone matrix*
- Proteoglycan defects are more commonly associated with chondrodysplasias involving **cartilage** and growth plate development.
- **Type I collagen** provides the essential backbone for bone mineral deposition; its deficiency is the direct cause of both the **fragility** and the **conductive hearing loss** due to ossicle abnormalities.
More Specialized epithelial junctions US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.