Loose connective tissue US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Loose connective tissue. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Loose connective tissue US Medical PG Question 1: A 55-year-old female presents with pain in both hands and wrists for the past several years. It is associated with morning stiffness that lasts for almost an hour. Physical examination reveals tenderness and swelling in both hands and wrists, most severe over the proximal interphalangeal joints. Laboratory investigation reveals the presence of anti-cyclic citrullinated peptide (anti-CCP). Which of the following immune-mediated injuries is responsible for this patient’s condition?
- A. Both type II and III hypersensitivities
- B. Type IV hypersensitivity (Correct Answer)
- C. Type III hypersensitivity
- D. Self-tolerance
- E. IgE-mediated immune responses only
Loose connective tissue Explanation: ***Type IV hypersensitivity***
- **Rheumatoid arthritis** is primarily a **Type IV (delayed-type, cell-mediated) hypersensitivity** reaction involving **T-cells, macrophages, and cytokine-mediated inflammation**.
- The synovial membrane is infiltrated by **CD4+ T-cells (Th1 and Th17)** that recognize self-antigens (citrullinated peptides), leading to activation of macrophages and release of inflammatory cytokines **(TNF-α, IL-1, IL-6, IL-17)**.
- This **chronic T-cell driven inflammation** results in synovial hyperplasia, pannus formation, and progressive joint destruction—the hallmark pathology of RA.
- **Anti-CCP antibodies** are highly specific diagnostic markers indicating immune targeting of citrullinated proteins, but the actual joint damage mechanism is **cell-mediated immunity** (Type IV).
*Both type II and III hypersensitivities*
- While **immune complexes** (Type III) involving rheumatoid factor can be present in RA, and there may be minor antibody-mediated effects (Type II), these are **secondary phenomena**.
- The **primary pathogenic mechanism** driving synovial inflammation and joint destruction is **Type IV hypersensitivity** with T-cell and macrophage activation.
- This option is incorrect because it does not identify the predominant mechanism.
*IgE-mediated immune responses only*
- **IgE-mediated immune responses** characterize **Type I hypersensitivity**, seen in allergic conditions such as asthma, allergic rhinitis, and anaphylaxis.
- Rheumatoid arthritis involves **chronic autoimmune inflammation** with T-cell activation and cytokine release, not acute IgE-mediated mast cell degranulation.
- The clinical presentation does not align with Type I hypersensitivity.
*Type III hypersensitivity*
- **Type III hypersensitivity** involves **immune complex deposition** causing tissue damage, as seen in serum sickness, post-streptococcal glomerulonephritis, and systemic lupus erythematosus.
- While **rheumatoid factor immune complexes** can form in RA (particularly in seropositive patients), immune complex deposition is a **secondary feature**, not the primary driver of joint destruction.
- The **dominant pathophysiology** of RA is **T-cell mediated chronic inflammation** (Type IV), making this option incorrect.
*Self-tolerance*
- **Self-tolerance** refers to the immune system's normal ability to **not react** against the body's own tissues.
- RA results from a **breakdown of self-tolerance**, leading to autoimmunity—this is the **underlying defect**, not the **mechanism of tissue injury**.
- The question asks for the **immune-mediated injury mechanism**, which is Type IV hypersensitivity, not the state of tolerance itself.
Loose connective tissue US Medical PG Question 2: A 30-year-old man comes to the physician for a follow-up examination 1 month after sustaining a chemical burn over the dorsum of his right hand and forearm. Physical examination shows hyperextension of the hand at the wrist. The skin over the dorsum of the wrist is tense and there is a thick, epithelialized scar. Range of motion of the right wrist is restricted. This patient's contracture is most likely due to activity of which of the following cells?
- A. Fibroblasts
- B. Myofibroblasts (Correct Answer)
- C. Neutrophils
- D. Macrophages
- E. Endothelial cells
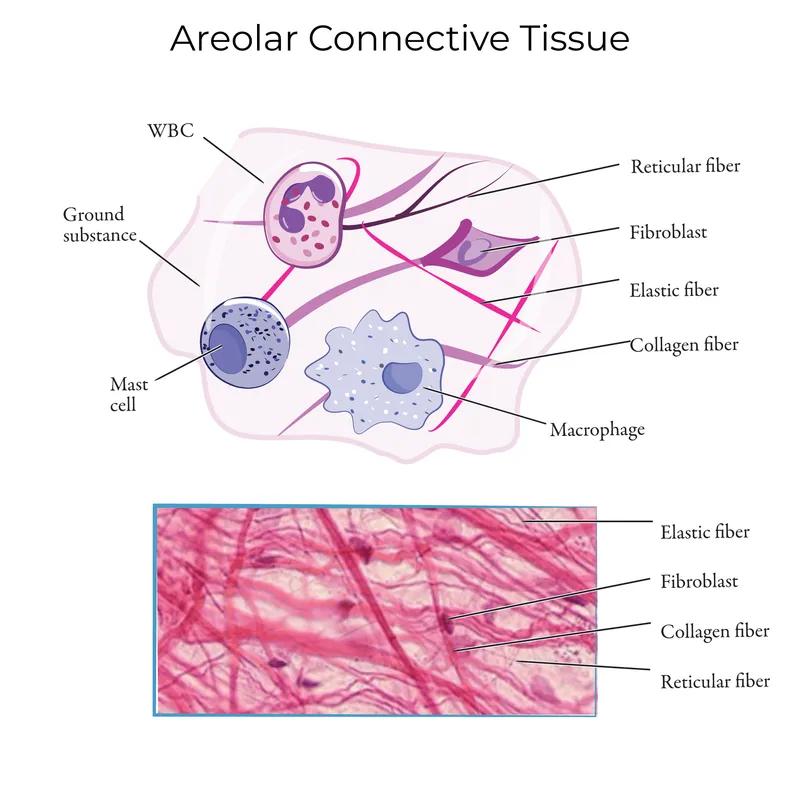
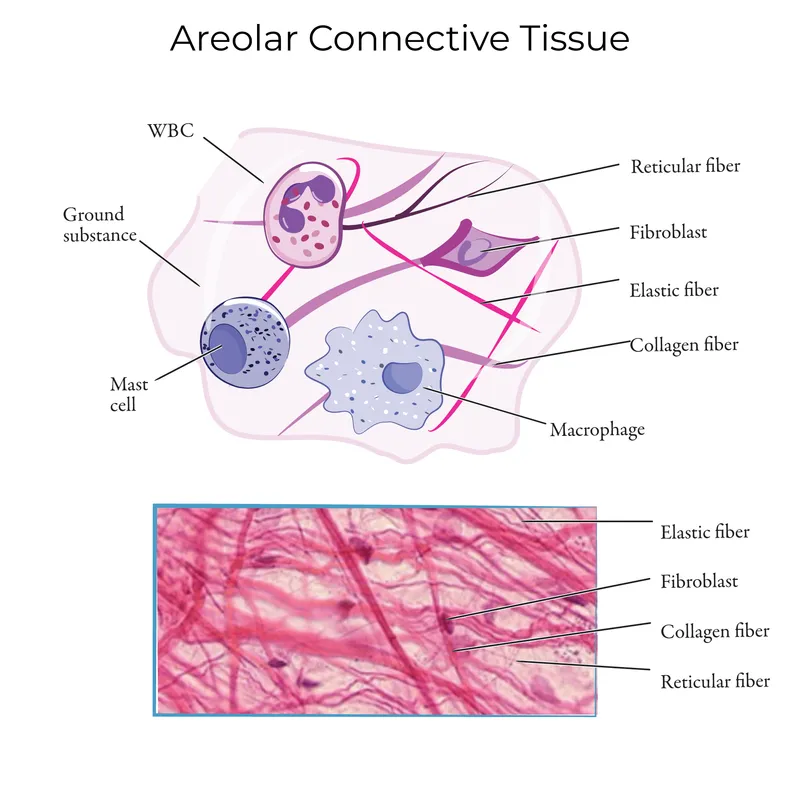
Loose connective tissue Explanation: ***Myofibroblasts***
- The patient presents with a **contracture** (restricted range of motion and hyperextension of the hand due to a thick scar) after a burn, which is characteristic of the action of **myofibroblasts**.
- Myofibroblasts are specialized cells that possess features of both fibroblasts (synthesizing **collagen** and extracellular matrix) and smooth muscle cells (containing **actin microfilaments**), allowing them to exert contractile force which leads to scar contraction.
*Fibroblasts*
- While fibroblasts are crucial for **wound healing** by producing collagen and other extracellular matrix components, they primarily lay down the foundation for scar tissue.
- They lack the strong contractile capabilities that lead to significant **tissue retraction** and contracture.
*Neutrophils*
- Neutrophils are **acute inflammatory cells** that primarily function in the early stages of wound healing to phagocytose debris and pathogens.
- They do not play a direct role in the formation of **scar tissue** or **contractures**.
*Macrophages*
- Macrophages are important **immune cells** involved in clearing debris, presenting antigens, and releasing growth factors during the later stages of wound healing.
- They also influence fibroblast activity, but they do not directly cause **tissue contraction** or scar formation.
*Endothelial cells*
- Endothelial cells line **blood vessels** and are essential for **angiogenesis** (formation of new blood vessels) during wound healing.
- They are not involved in the **contractile process** that leads to scar contracture.
Loose connective tissue US Medical PG Question 3: A 15-year-old boy presents with shortness of breath on exertion for the past 2 weeks. Although he does not have any other complaints, he is concerned about not gaining much weight despite a good appetite. His height is 188 cm (6 ft 2 in) and weight is 58 kg (124 lb). His blood pressure is 134/56 mm Hg and his pulse rate is 78/min. On cardiac auscultation, his apex beat is displaced laterally with a diastolic murmur lateral to the left sternal border. Slit-lamp examination shows an upward and outward displacement of both lenses. Synthesis of which of the following proteins is most likely defective in this patient?
- A. Fibronectin
- B. Elastin
- C. Fibrillin (Correct Answer)
- D. Reticular fibers
- E. Laminin
Loose connective tissue Explanation: ***Fibrillin***
- The patient's presentation with **tall stature**, **arachnodactyly** (implied by tall, thin build), **ectopia lentis** (upward and outward lens displacement), and a **diastolic murmur** (suggesting aortic root dilation or dissection, or mitral valve prolapse) are classic features of **Marfan syndrome**.
- **Marfan syndrome** is caused by a defect in the gene encoding **fibrillin-1**, a glycoprotein essential for the formation of elastic fibers and connective tissue integrity.
*Fibronectin*
- **Fibronectin** is involved in cell adhesion, growth, migration, and differentiation, and plays a crucial role in wound healing and embryonic development.
- While essential for connective tissue, defects in fibronectin are not typically associated with the constellation of symptoms seen in Marfan syndrome.
*Elastin*
- **Elastin** works in conjunction with fibrillin to provide elasticity to tissues like the skin, lungs, and blood vessels.
- While Marfan syndrome affects elastic fibers, the primary defect is in fibrillin, which then impairs the proper formation and function of elastin-containing microfibrils.
*Reticular fibers*
- **Reticular fibers** are fine collagen fibers (primarily type III collagen) that form a delicate supporting network in various tissues and organs.
- Defects in reticular fibers are not characteristic of Marfan syndrome; Marfan syndrome is specifically linked to fibrillin defects.
*Laminin*
- **Laminins** are major proteins of the **basal lamina**, essential for cell adhesion and differentiation in epithelial and endothelial tissues.
- Genetic defects in laminin components are often associated with muscular dystrophies or epidermolysis bullosa, not the Marfanoid features presented.
Loose connective tissue US Medical PG Question 4: A 48-year-old man is brought to the emergency department with a stab wound to his chest. The wound is treated in the emergency room. Three months later he develops a firm 4 x 3 cm nodular mass with intact epithelium over the site of the chest wound. On local examination, the scar is firm, non-tender, and there is no erythema. The mass is excised and microscopic examination reveals fibroblasts with plentiful collagen. Which of the following processes is most likely related to the series of events mentioned above?
- A. Development of a fibrosarcoma
- B. Foreign body response from suturing
- C. Staphylococcal wound infection
- D. Poor wound healing from diabetes mellitus
- E. Keloid scar formation (Correct Answer)
Loose connective tissue Explanation: ***Keloid scar formation***
- A **keloid** is a raised, firm, nodular scar that extends beyond the original wound boundaries and is characterized by excessive collagen deposition from **fibroblasts**.
- The delayed presentation (3 months), firm nature, absence of inflammation (no erythema, non-tender), and microscopic findings of fibroblasts with plentiful collagen are classic features of a keloid.
*Development of a fibrosarcoma*
- A fibrosarcoma is a **malignant tumor** of fibroblasts, which would typically present with more aggressive growth, often pain, and possibly ulceration, none of which are described.
- While composed of fibroblasts, fibrosarcomas exhibit **cellular atypia**, mitotic activity, and invasion, which are not mentioned in the microscopic description.
*Foreign body response from suturing*
- A foreign body response usually involves a **granulomatous inflammation** around foreign material, such as suture remnants.
- The microscopic description of "fibroblasts with plentiful collagen" without mention of inflammatory cells or foreign bodies makes this less likely.
*Staphylococcal wound infection*
- A **bacterial infection** would typically present with signs of acute inflammation such as erythema, warmth, pain, and possibly pus, shortly after the wound.
- The mass is described as non-tender with no erythema, and the 3-month delay makes an active infection less probable.
*Poor wound healing from diabetes mellitus*
- Poor wound healing in diabetes often manifests as **delayed closure**, chronic ulcers, and increased susceptibility to infection, rather than an overgrowth of fibrous tissue in the form of a nodular mass.
- While diabetes can affect wound healing, the specific description of a firm, nodular mass with excessive collagen points away from typical diabetic wound complications.
Loose connective tissue US Medical PG Question 5: In a routine medical examination, a young man is noted to be tall with slight scoliosis and pectus excavatum. He had been told that he was over the 95% percentile for height as a child. Auscultation reveals a heart murmur, and transthoracic echocardiography shows an enlarged aortic root and mitral valve prolapse. Blood screening for fibrillin-1 (FBN1) gene mutation is positive and plasma homocysteine is normal. This patient is at high risk for which of the following complications?
- A. Intravascular thrombosis
- B. Infertility
- C. Aortic dissection (Correct Answer)
- D. Spontaneous pneumothorax
- E. Mucosal neuromas
Loose connective tissue Explanation: ***Aortic dissection***
- The constellation of **tall stature**, **scoliosis**, **pectus excavatum**, **enlarged aortic root**, **mitral valve prolapse**, and a **positive FBN1 gene mutation** is highly indicative of **Marfan syndrome**.
- **Aortic dissection** is the most life-threatening complication of Marfan syndrome due to the weakened connective tissue in the aortic wall, a direct consequence of the FBN1 mutation affecting fibrillin-1 protein.
- Patients with Marfan syndrome require regular cardiovascular surveillance and prophylactic beta-blocker therapy to reduce aortic wall stress.
*Intravascular thrombosis*
- This complication is more characteristic of conditions like **homocystinuria**, which is ruled out by the **normal plasma homocysteine** level.
- Marfan syndrome primarily affects connective tissue strength, not coagulation pathways or endothelial function.
*Infertility*
- Marfan syndrome does not inherently cause **infertility** in males or females.
- The primary health risks for Marfan patients are cardiovascular, musculoskeletal, and ophthalmologic (lens dislocation).
*Spontaneous pneumothorax*
- While **spontaneous pneumothorax** can occur in Marfan syndrome due to apical blebs and weakened pleural tissue, it is far less immediately life-threatening than aortic dissection.
- The question asks for the "high risk" complication, and cardiovascular complications (particularly aortic dissection and rupture) are the leading cause of mortality in Marfan syndrome.
*Mucosal neuromas*
- **Mucosal neuromas** are characteristic of **Multiple Endocrine Neoplasia type 2B (MEN2B)**, not Marfan syndrome.
- MEN2B involves RET proto-oncogene mutations and is associated with medullary thyroid cancer, pheochromocytoma, and a marfanoid habitus, which can be mistaken for Marfan syndrome.
Loose connective tissue US Medical PG Question 6: An investigator is studying the interaction between epithelial cells and calcium ion concentration. When the calcium ion concentration available to a sample of epithelial tissue is decreased, an increased gap between adjacent epithelial cells is seen on electron microscopy. This observed decrease in cell adhesion is most likely due to an effect on which of the following proteins?
- A. Actin
- B. Integrin
- C. Cadherin (Correct Answer)
- D. Claudin
- E. Cytokeratin
Loose connective tissue Explanation: ***Cadherin***
- **Cadherins** are calcium-dependent adhesion proteins that mediate cell-to-cell adhesion, particularly in epithelial tissues.
- A decrease in calcium concentration would directly impair cadherin function, leading to reduced cell adhesion and increased intercellular gaps.
*Actin*
- **Actin** is a component of the cell's cytoskeleton, involved in cell shape, motility, and intracellular transport, but not directly responsible for calcium-dependent cell adhesion between epithelial cells.
- While actin filaments interact with adhesion junctions, their primary role is structural and dynamic rather than adhesive.
*Integrin*
- **Integrins** are primarily involved in cell-to-extracellular matrix adhesion, connecting the cell to the surrounding matrix, not directly mediating calcium-dependent cell-to-cell adhesion between epithelial cells.
- They can be affected by intracellular calcium signaling but do not directly bind calcium to mediate their adhesive function in the same way cadherins do.
*Claudin*
- **Claudins** are key components of **tight junctions**, which regulate paracellular permeability and form a barrier between cells, but they are not directly responsible for calcium-dependent cell-to-cell adhesion, which is characteristic of adherens junctions.
- While tight junctions contribute to overall cell-cell contact, the observation of an *increased gap* suggests an issue with adhesive complexes like adherens junctions, where cadherins are prominent.
*Cytokeratin*
- **Cytokeratins** are intermediate filaments found in epithelial cells, providing structural support and mechanical strength.
- They are linked to desmosomes and hemidesmosomes but are not directly involved in calcium-dependent cell-to-cell adhesion.
Loose connective tissue US Medical PG Question 7: An 8-year old boy is brought into clinic for evaluation of possible scoliosis that was newly found on a routine exam at school. On exam, he is also noted to be in the 99th percentile for height and 70th percentile for weight. He appears to have abnormally long extremities as well as an upward lens dislocation on ophthalmologic exam. A mutation leading to a defect in which of the following proteins is the most likely cause of his condition?
- A. Type IV collagen
- B. Type I collagen
- C. Elastin
- D. Fibrillin (Correct Answer)
- E. ATP7A
Loose connective tissue Explanation: ***Fibrillin***
- The patient's clinical features, including **scoliosis**, being in the **99th percentile for height**, having **abnormally long extremities** (arachnodactyly), and **upward lens dislocation**, are classic signs of **Marfan syndrome**.
- **Marfan syndrome** is an autosomal dominant disorder caused by a mutation in the *FBN1* gene, which codes for **fibrillin-1**, a glycoprotein essential for the formation of elastic fibers in connective tissue.
*Type I collagen*
- Defects in **Type I collagen** are primarily associated with **osteogenesis imperfecta**, characterized by **bone fragility**, multiple fractures, blue sclera, and hearing loss.
- While it can present with skeletal abnormalities, it does not typically cause the extreme height, arachnodactyly, or lens dislocation seen in this patient.
*Type IV collagen*
- Defects in **Type IV collagen** are linked to conditions like **Alport syndrome**, which primarily affects the kidneys (glomerulonephritis), ears (hearing loss), and eyes (ocular defects including lenticonus), but not typically the skeletal features described.
- It is a major component of **basement membranes**, important for filtration and structural support in various organs.
*Elastin*
- Mutations in **elastin** are associated with conditions like **supravalvular aortic stenosis** (Williams syndrome) or cutis laxa, which affect the skin and cardiovascular system.
- It does not explain the characteristic skeletal and ocular findings of Marfan syndrome.
*ATP7A*
- A mutation in the *ATP7A* gene, which codes for an ATPase involved in copper transport, is responsible for **Menkes disease**.
- **Menkes disease** is characterized by **sparse, kinky hair**, failure to thrive, neurological degeneration, and connective tissue abnormalities due to copper deficiency, which does not align with the patient's presentation.
Loose connective tissue US Medical PG Question 8: A 37-year-old man presents to the clinic because of painful, severe blistering over his buttocks for the past week. About a year ago, he noticed a similar outbreak on his inner thighs, but it receded within a few days on its own. Physical examination shows the blisters are tense, and rubbing the affected skin does not result in ‘popping’ of the blisters. A biopsy shows the entire epidermis lifting away from the basal lamina with extensive inflammatory infiltrates abundant with eosinophils. Immunofluorescence shows a linear pattern of immune complex deposits. Which of the following cellular structures, if defective, is most likely involved in the formation of these blisters?
- A. Gap junctions
- B. Hemidesmosomes (Correct Answer)
- C. Lamellar bodies
- D. Zonula occludens
- E. Macula adherens
Loose connective tissue Explanation: ***Hemidesmosomes***
- The clinical picture of **tense blisters** that do not pop with rubbing (**negative Nikolsky sign**), along with the histological finding of the **entire epidermis lifting away from the basal lamina** (subepidermal blistering), strongly suggests **bullous pemphigoid**.
- **Immunofluorescence showing linear deposits** along the basement membrane zone is characteristic of bullous pemphigoid, which is caused by autoantibodies targeting proteins within the hemidesmosomes.
*Gap junctions*
- **Gap junctions** are involved in **intercellular communication** and the passage of small molecules between cells.
- Defects in gap junctions do not typically lead to blistering skin disorders.
*Lamellar bodies*
- **Lamellar bodies** are organelles in **keratinocytes** that release lipids to form the **skin barrier**.
- Defects in lamellar bodies are associated with disorders like **ichthyosis**, not blistering as described.
*Zonula occludens*
- **Zonula occludens**, also known as **tight junctions**, are crucial for forming a **seal between epithelial cells**, regulating paracellular transport.
- Dysfunctional tight junctions can lead to increased permeability but are not directly involved in the formation of subepidermal blisters.
*Macula adherens*
- **Macula adherens**, or **desmosomes**, are cell-to-cell adhesion structures that provide strong mechanical attachments between keratinocytes.
- Defects in desmosomes are associated with **pemphigus vulgaris** and **pemphigus foliaceus**, which typically present with **flaccid blisters** that show a **positive Nikolsky sign** and involve intraepidermal cleavage.
Loose connective tissue US Medical PG Question 9: A 31-year-old woman scrapes her finger on an exposed nail and sustains a minor laceration. Five minutes later, her finger is red, swollen, and painful. She has no past medical history and does not take any medications. She drinks socially with her friends and does not smoke. The inflammatory cell type most likely to be prominent in this patient's finger has which of the following characteristics?
- A. Segmented nuclei (Correct Answer)
- B. Dramatically expanded endoplasmic reticulum
- C. Large cell with amoeboid movement
- D. Multiple peripheral processes
- E. Dark histamine containing granules
Loose connective tissue Explanation: ***Segmented nuclei***
- This scenario describes **acute inflammation** following a minor injury, with classic signs of **redness, swelling, and pain** within minutes.
- **Neutrophils** are the primary inflammatory cells in acute inflammation and are characterized by their **segmented (multi-lobed) nuclei.**
*Dramatically expanded endoplasmic reticulum*
- An expanded endoplasmic reticulum is characteristic of cells highly active in protein synthesis and secretion, such as **plasma cells** producing antibodies.
- Plasma cells are typically involved in **chronic inflammation** and adaptive immune responses, not rapid acute inflammation.
*Large cell with amoeboid movement*
- This describes **macrophages**, which are phagocytic cells important in both acute and chronic inflammation, and in cleaning up debris.
- While macrophages are present, **neutrophils** are the predominant early responders in acute bacterial infections and tissue injury.
*Multiple peripheral processes*
- This description is characteristic of **dendritic cells**, which are antigen-presenting cells that initiate adaptive immune responses.
- Dendritic cells play a role in linking innate and adaptive immunity but are not the primary inflammatory cell type in the immediate acute response.
*Dark histamine containing granules*
- This description applies to **mast cells** and **basophils**, which release histamine and other mediators in allergic reactions and acute inflammation.
- While mast cells are involved in the immediate response by releasing mediators, **neutrophils** are the main cellular players migrating to the site of injury.
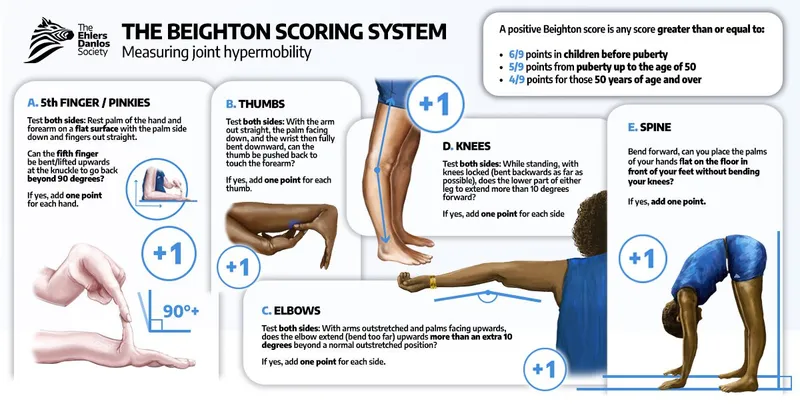
Loose connective tissue US Medical PG Question 10: A 25-year-old man presents to the emergency department with sudden-onset severe pain in the right shoulder that occurred when he threw a bowling ball 2 hours ago. He has a history of dislocations in both shoulders and subluxation of the right knee and left wrist. There is no history of fractures. On physical examination, the right arm is slightly abducted and externally rotated. An anterior bulge is seen near the shoulder joint. The neurovascular examination of the right arm shows no abnormalities. The skin examination shows multiple widened atrophic scars around the knees, elbows, and ankles. The skin of the neck and around the elbow can easily be extended up to 4 cm. The sclera is white. The remainder of the physical examination shows no abnormalities. A defect in which of the following proteins is the most likely cause of the findings in this patient?
- A. Collagen (Correct Answer)
- B. Keratin
- C. Fibrillin-1
- D. Tau
- E. Elastin
Loose connective tissue Explanation: ***Collagen***
- This patient's symptoms, including **recurrent dislocations**, easy **skin extensibility**, and **atrophic scars**, are classic signs of **Ehlers-Danlos syndrome (EDS)**, which is primarily caused by defects in **collagen synthesis or processing**.
- The shoulder dislocation from a minor activity (throwing a bowling ball), along with multisystem hypermobility (shoulders, knee, wrist), strongly points to a **connective tissue disorder** affecting collagen.
*Keratin*
- **Keratin** is a structural protein primarily found in **epithelial cells**, forming hair, skin, and nails.
- Defects in keratin typically manifest as disorders of **skin fragility**, such as **epidermolysis bullosa**, not joint hypermobility or tissue extensibility.
*Fibrillin-1*
- **Fibrillin-1** defects cause **Marfan syndrome**, characterized by **tall stature**, **arachnodactyly**, **aortic root dilation**, and **lens dislocation**.
- While Marfan syndrome involves connective tissue, the patient's presentation of easy skin extensibility and atrophic scars is not characteristic of fibrillin-1 defects, and there is no mention of cardiovascular or ocular issues typical of Marfan.
*Tau*
- **Tau protein** is a **microtubule-associated protein** primarily found in neurons and is involved in stabilizing microtubules.
- Defects or abnormal aggregation of tau protein are associated with **neurodegenerative diseases** like **Alzheimer's disease** and **frontotemporal dementia**, not connective tissue disorders.
*Elastin*
- **Elastin** provides elasticity to tissues, allowing them to stretch and recoil. Defects can lead to conditions like **cutis laxa** or **Williams syndrome**.
- While some features of increased skin extensibility might overlap, the constellation of recurrent joint dislocations and specific atrophic scars seen in this patient is more indicative of **collagen defects** common in Ehlers-Danlos syndrome.
More Loose connective tissue US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.