Epithelial glands US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Epithelial glands. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Epithelial glands US Medical PG Question 1: A 15-year-old boy comes to the physician because of skin changes on his face, chest, and back over the past year. Treatment with over-the-counter benzoyl peroxide has been ineffective. Physical examination shows numerous open comedones, inflammatory papules, and pustules on his face, chest, and back. Which of the following is the most likely underlying mechanism of this patient’s skin condition?
- A. Hyperkeratinization of hair follicles (Correct Answer)
- B. Type IV hypersensitivity reaction
- C. Formation of superficial epidermal inclusion cyst
- D. Excess androgen production
- E. Hyperplasia of pilosebaceous glands
Epithelial glands Explanation: **Hyperkeratinization of hair follicles**
- The primary event in the pathogenesis of **acne vulgaris** is the **shedding of hyperkeratinized corneocytes** into the lumen of the hair follicle, which then combines with sebum to form a microcomedone.
- This process leads to the **obstruction of the pilosebaceous unit**, creating an anaerobic environment conducive to the proliferation of *Cutibacterium acnes* and the development of inflammatory lesions like papules and pustules.
*Type IV hypersensitivity reaction*
- This mechanism involves **T-cell mediated delayed hypersensitivity**, leading to conditions like **allergic contact dermatitis** or **tuberculosis**.
- Acne vulgaris is not primarily an allergic reaction mediated by T cells; its pathogenesis involves follicular obstruction, sebum production, bacterial colonization, and inflammation.
*Formation of superficial epidermal inclusion cyst*
- Epidermal inclusion cysts (also known as epidermoid cysts) are typically solitary, slow-growing cysts that result from the **implantation of epidermal cells into the dermis**, often due to trauma or blocked hair follicles, but they are not the underlying mechanism for widespread acne.
- While some severe acne lesions can rarely lead to cyst formation, the presence of numerous **comedones, papules, and pustules** indicates typical acne vulgaris, not primarily cyst formation.
*Excess androgen production*
- While **androgens stimulate sebum production**, which is a contributing factor to acne, they are not the initiating mechanism for the follicular obstruction itself.
- Most adolescents with acne have **normal androgen levels**; the skin's sebaceous glands are simply more sensitive to circulating androgens, leading to increased sebum.
*Hyperplasia of pilosebaceous glands*
- **Sebaceous gland hyperplasia** refers to an increase in the number and size of sebaceous glands, leading to an overproduction of sebum, which contributes to acne.
- However, the fundamental initiating event for comedone formation in acne is the **follicular hyperkeratinization and obstruction**, rather than simply the glands being hyperplastic.
Epithelial glands US Medical PG Question 2: A 58-year-old woman with refractory gastrointestinal complaints undergoes a bowel biopsy. On histology, the pathologist observes that submucosal glands of Brunner are present in the specimen. Which portion of the bowel was most likely biopsied?
- A. Descending colon
- B. Ileum
- C. Jejunum
- D. Cecum
- E. Duodenum (Correct Answer)
Epithelial glands Explanation: ***Duodenum***
- The presence of **Brunner's glands** in the submucosa is a **histological hallmark** of the duodenum.
- These glands produce an **alkaline mucus** that helps protect the duodenal wall from acidic chyme entering from the stomach.
*Descending colon*
- The descending colon is part of the **large intestine** and does not contain Brunner's glands.
- Its histology is characterized by numerous **goblet cells** and the absence of villi.
*Ileum*
- The ileum is the final section of the small intestine, characterized by the presence of **Peyer's patches** (lymphoid aggregates) in the lamina propria and submucosa.
- It lacks Brunner's glands.
*Jejunum*
- The jejunum is the middle section of the small intestine, known for its tall, finger-like villi, but it **does not contain Brunner's glands**.
- It is primarily involved in nutrient absorption and has a reduced number of goblet cells compared to the ileum.
*Cecum*
- The cecum is the beginning of the **large intestine** and is characterized by a high density of **goblet cells** and lymphoid tissue, but no Brunner's glands.
- It plays a role in absorption of fluids and electrolytes.
Epithelial glands US Medical PG Question 3: During a study on gastrointestinal hormones, a volunteer is administered the hormone secreted by S cells. Which of the following changes most likely represent the effect of this hormone on gastric and duodenal secretions?
$$$ Gastric H+ %%% Duodenal HCO3- %%% Duodenal Cl- $$$
- A. ↓ ↓ ↓
- B. ↑ ↓ no change
- C. ↑ ↑ ↓
- D. ↓ ↑ ↓ (Correct Answer)
- E. ↓ no change no change
Epithelial glands Explanation: ***↓ ↑ ↓***
- S cells secrete **secretin**, which primarily inhibits **gastric acid (H+) secretion** to protect the duodenal mucosa from acidic chyme.
- Secretin also stimulates the pancreas and bile ducts to secrete **bicarbonate (HCO3-)**, neutralizing the acidic chyme. Duodenal **chloride (Cl-) secretion is typically reduced** as it is often exchanged for bicarbonate or water follows bicarbonate secretion for osmotic balance.
*↓ ↓ ↓*
- While **gastric H+ decreases** due to secretin, **duodenal HCO3- secretion increases**, not decreases, making this option incorrect.
- **Duodenal Cl- secretion** would likely decrease, but the other components are inconsistent with secretin's effects.
*↑ ↓ no change*
- Secretin **inhibits gastric H+ secretion**, so an increase contradicts its primary function to protect the duodenum from acid.
- **Duodenal HCO3- secretion increases**, not decreases, and no change in Cl- is unlikely given the physiological responses to secretin.
*↑ ↑ ↓*
- Secretin **inhibits gastric H+ secretion**, so an increase is incorrect.
- While **duodenal HCO3- increases** and **Cl- decreases**, the initial change in gastric H+ makes this option wrong.
*↓ no change no change*
- While **gastric H+ is indeed decreased**, secretin significantly **increases duodenal HCO3- secretion** and likely decreases duodenal Cl- secretion, making "no change" in these parameters incorrect.
- Secretin has a pronounced effect on both bicarbonate and chloride transport in the duodenum.
Epithelial glands US Medical PG Question 4: A research team is studying certain congenital anomalies of the respiratory tract. The method consists of marking a certain germinal layer with an isotope, following its development stages in chicken embryos, and finally analyzing the specimen. A given specimen of tissue is presented in the exhibit. Which of the following germinal structures most likely gave rise to the epithelial lining of this specimen?
- A. Ectoderm
- B. Neural crest
- C. Mesoderm
- D. Endoderm (Correct Answer)
- E. Surface ectoderm
Epithelial glands Explanation: ***Endoderm***
- The **epithelial lining** of the entire respiratory tract, including the larynx, trachea, bronchi, and lungs, is derived from the **endoderm**.
- The **laryngotracheal groove** develops from the ventral wall of the primitive foregut, which is endodermal in origin, further differentiating into the respiratory tree.
*Ectoderm*
- The **ectoderm** primarily forms the epidermis, hair, nails, and the nervous system (brain and spinal cord).
- It does not contribute to the internal epithelial lining of the respiratory tract.
*Neural crest*
- **Neural crest cells** contribute to a wide variety of structures, including components of the peripheral nervous system, head mesenchyme, and melanocytes.
- They are not involved in forming the epithelial lining of the respiratory system.
*Mesoderm*
- The **mesoderm** forms the connective tissue, cartilage, and muscle components of the respiratory tract, such as the smooth muscle and cartilage rings of the trachea and bronchi, and the visceral pleura.
- However, it does not form the epithelial lining itself.
*Surface ectoderm*
- **Surface ectoderm** specifically gives rise to the epidermis, hair, nails, and glands of the skin, as well as the oral cavity epithelium.
- It does not contribute to the internal epithelial structures of the respiratory tract.
Epithelial glands US Medical PG Question 5: A group of scientists is studying the mechanism of action of various pancreatic hormones in rats. The scientists studied hormone A, which is secreted by the β-cells of the pancreas, and found that hormone A binds to a complex dimeric receptor on the cell membrane and exerts its effects via phosphorylation and subsequent downstream signaling that includes dephosphorylation of different intracellular proteins. Now they are studying hormone B, which is secreted by the α-cells and antagonizes the actions of hormone A. Which 2nd messenger system would hormone B utilize to exert its cellular effects?
- A. Direct cytoplasmic receptor binding
- B. Phospholipase C
- C. Tyrosine kinase
- D. Direct nuclear receptor binding
- E. Adenylyl cyclase-cyclic AMP (Correct Answer)
Epithelial glands Explanation: ***Adenylyl cyclase-cyclic AMP***
- Hormone B is **glucagon**, secreted by pancreatic α-cells, which antagonizes the effects of insulin (hormone A). Glucagon primarily acts through a **G protein-coupled receptor** that activates **adenylyl cyclase**, leading to an increase in intracellular **cyclic AMP (cAMP)**.
- Increased cAMP then activates **protein kinase A (PKA)**, which phosphorylates various intracellular proteins to promote **glycogenolysis** and **gluconeogenesis**, thereby raising blood glucose levels.
*Direct cytoplasmic receptor binding*
- This mechanism is characteristic of **steroid hormones**, which are lipid-soluble and can diffuse across the cell membrane to bind to receptors in the cytoplasm.
- Pancreatic hormones like glucagon are **peptide hormones**, which are water-soluble and typically bind to cell surface receptors.
*Phospholipase C*
- Activation of **phospholipase C (PLC)** leads to the production of **inositol triphosphate (IP3)** and **diacylglycerol (DAG)**, which mobilize intracellular calcium and activate protein kinase C, respectively.
- While some G protein-coupled receptors activate PLC, **glucagon's primary signaling pathway** involves adenylyl cyclase.
*Tyrosine kinase*
- **Tyrosine kinase receptors** are often associated with growth factors and insulin (hormone A) signaling, leading to phosphorylation of tyrosine residues on target proteins.
- Glucagon's receptor is a **G protein-coupled receptor**, not a receptor tyrosine kinase, and its actions are mediated through serine/threonine phosphorylation via PKA.
*Direct nuclear receptor binding*
- This mechanism is typical for **steroid hormones** and **thyroid hormones**, which are lipid-soluble and bind to receptors in the nucleus to directly influence gene transcription.
- As a peptide hormone, glucagon binds to cell surface receptors and does not directly interact with nuclear receptors.
Epithelial glands US Medical PG Question 6: A 48-year-old man has smoked approximately 3 packs of cigarettes per day for the past 12 years. Which of the following pathologic changes is most likely to occur in his bronchial epithelium?
- A. Metaplasia (Correct Answer)
- B. Hyperplasia
- C. Hypertrophy
- D. Dysplasia
- E. Atrophy
Epithelial glands Explanation: ***Metaplasia***
- Chronic irritation from **cigarette smoking** can cause the **bronchial epithelium** to change from ciliated columnar to stratified squamous, a process known as **metaplasia**.
- This adaptation makes the tissue more resistant to injury but results in the loss of important protective functions like **mucociliary clearance**.
*Hyperplasia*
- **Hyperplasia** involves an increase in the number of cells in a tissue or organ, often in response to increased demand or chronic stimulation.
- While smoking can cause hyperplasia of goblet cells and mucous glands in the bronchi, the direct epithelial change in response to chronic irritation is more specifically **metaplasia**.
*Hypertrophy*
- **Hypertrophy** is an increase in the size of individual cells, leading to an increase in the size of the organ or tissue.
- This is not the primary adaptive change seen in the bronchial epithelium in response to chronic smoking; instead, cells change their type.
*Dysplasia*
- **Dysplasia** refers to disorderly cell growth, often characterized by variations in cell size, shape, and organization; it is considered a precursor to cancer.
- While chronic smoking can eventually lead to dysplasia and then carcinoma, the initial and most common adaptive change in the bronchial epithelium is **metaplasia**.
*Atrophy*
- **Atrophy** is a decrease in cell size or number, leading to a reduction in the size of an organ or tissue, usually due to decreased workload, nutrition, or blood supply.
- This is not a typical response of the bronchial epithelium to chronic irritation from smoking, which tends to induce proliferative or adaptive changes.
Epithelial glands US Medical PG Question 7: A patient presents to the emergency room in an obtunded state. The patient is a known nurse within the hospital system and has no history of any medical problems. A finger stick blood glucose is drawn showing a blood glucose of 25 mg/dL.
The patient's daughter immediately arrives at the hospital stating that her mother has been depressed recently and that she found empty syringes in the bathroom at the mother's home. Which of the following is the test that will likely reveal the diagnosis?
- A. Fasting blood glucose
- B. Urine metanephrines
- C. Genetic testing
- D. 24 hr cortisol
- E. C-peptide level (Correct Answer)
Epithelial glands Explanation: ***C-peptide level***
- A **low C-peptide level** in the presence of **hypoglycemia** and high insulin levels confirms the diagnosis of **exogenous insulin administration** (factitious hypoglycemia).
- **C-peptide** is cleaved from **proinsulin** in equimolar amounts with endogenous insulin, making it an excellent marker to differentiate endogenous insulin production from exogenous insulin injection.
- In this case: **Low C-peptide + High insulin + Hypoglycemia** = exogenous insulin administration.
*Fasting blood glucose*
- The patient already has documented **hypoglycemia (25 mg/dL)**, so an additional fasting blood glucose test would not provide further diagnostic information about the **cause** of hypoglycemia.
- A single fasting blood glucose level indicates current glucose status but **does not differentiate** between endogenous insulin overproduction (insulinoma) and exogenous insulin administration.
*Urine metanephrines*
- **Urine metanephrines** are used to diagnose **pheochromocytoma**, a catecholamine-secreting tumor of the adrenal medulla.
- Pheochromocytoma presents with **hypertension**, palpitations, headaches, and diaphoresis—**not hypoglycemia**.
- This test is not relevant to the differential diagnosis of hypoglycemia.
*Genetic testing*
- **Genetic testing** might be considered for rare hereditary causes of hypoglycemia, such as congenital hyperinsulinism or genetic insulinoma syndromes (e.g., MEN1).
- Given the clinical context (depressed nurse with access to insulin and empty syringes found at home), **exogenous insulin administration** is far more likely than a genetic condition.
- Genetic testing is not the appropriate initial diagnostic step in this scenario.
*24 hr cortisol*
- A **24-hour urinary cortisol** test is used to diagnose **Cushing's syndrome** (cortisol excess), not hypoglycemia.
- While **adrenal insufficiency** (cortisol deficiency) can cause hypoglycemia, it typically presents with **hypotension**, **hyponatremia**, **hyperkalemia**, and **hyperpigmentation**—features not described in this case.
- The clinical presentation strongly suggests insulin-related hypoglycemia rather than adrenal insufficiency.
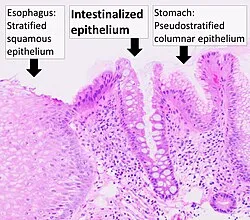
Epithelial glands US Medical PG Question 8: A 45-year-old African American male presents to his primary care physician complaining of difficulty swallowing that was initially limited to solids but has now progressed to liquids. Biopsy of the esophagus reveals dysplastic cells, but does not show evidence of glands or increased mucin. Which of the following most contributed to his condition?
- A. Gastroesophageal reflux disease
- B. Obesity
- C. Drinking extremely hot beverages
- D. Radiation exposure in the past 6 months
- E. Smoking (Correct Answer)
Epithelial glands Explanation: ***Smoking***
- **Smoking** is the most significant risk factor for **squamous cell carcinoma** of the esophagus, which is strongly suggested by the biopsy findings of **dysplastic cells without glands or mucin**.
- The combination of **progressive dysphagia** (solids to liquids) and smoking history in an **African American male** fits the classic demographic and presentation pattern for esophageal squamous cell carcinoma.
*Gastroesophageal reflux disease*
- **GERD** primarily leads to **esophageal adenocarcinoma** through **Barrett's esophagus**, which would show **glandular metaplasia** and **increased mucin production** on biopsy.
- The biopsy explicitly states **absence of glands and mucin**, making GERD-related adenocarcinoma unlikely as the primary pathologic process.
*Obesity*
- **Obesity** increases risk of **esophageal adenocarcinoma** by worsening **GERD** and promoting **Barrett's esophagus** development.
- Since the biopsy findings suggest **squamous cell carcinoma** rather than adenocarcinoma, obesity is not the most direct contributing factor in this case.
*Drinking extremely hot beverages*
- **Hot beverage consumption** is indeed a risk factor for **squamous cell carcinoma** of the esophagus, particularly in certain geographic regions.
- However, **smoking** remains the more prevalent and significant risk factor globally, especially when combined with **alcohol use**, making it the primary contributor.
*Radiation exposure in the past 6 months*
- **Radiation exposure** can increase risk of esophageal cancer, including **squamous cell carcinoma**, but typically requires a **longer latency period** (years to decades).
- A **6-month timeframe** is insufficient for radiation-induced carcinogenesis to manifest as advanced cancer with dysphagia and dysplastic changes.
Epithelial glands US Medical PG Question 9: A 37-year-old machinist presents to his primary care physician with eye problems. The patient states that he has had a mass in his eye that has persisted for the past month. The patient has a past medical history of blepharitis treated with eye cleansing and squamous cell carcinoma of the skin treated with Mohs surgery. His temperature is 99.5°F (37.5°C), blood pressure is 157/102 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a firm and rubbery nodule palpable inside the patient's left eyelid. Physical exam does not elicit any pain. Which of the following is the most likely diagnosis?
- A. Meibomian gland carcinoma
- B. Chalazion (Correct Answer)
- C. Hordeolum
- D. Ingrown eyelash follicle
- E. Foreign body
Epithelial glands Explanation: ***Chalazion***
- This patient's presentation of a **firm, rubbery, painless nodule** inside the eyelid, persistent for a month, is characteristic of a **chalazion**. It often develops after a hordeolum or **blepharitis** due to obstruction of a Meibomian gland.
- Chalazia are typically **non-tender** as they represent a chronic, sterile inflammation rather than an acute infection.
*Meibomian gland carcinoma*
- While a Meibomian gland carcinoma can present as a nodule, it often shows suggestive signs like **loss of eyelashes (madarosis)**, ulceration, or recurrent chalazion in an elderly patient. This patient's presentation does not describe these features.
- Carcinomas tend to be more **invasive** and may present with less defined borders or rapid growth, which are not mentioned here.
*Hordeolum*
- A **hordeolum (stye)** is an acute, painful, localized infection of an eyelash follicle (**external hordeolum**) or Meibomian gland (**internal hordeolum**).
- It would typically cause **pain, redness, and tenderness** which are absent in this patient's description.
*Ingrown eyelash follicle*
- An ingrown eyelash (trichiasis) primarily causes **irritation, foreign body sensation**, and possibly corneal abrasion from the misdirected lash rubbing against the eye.
- It does not typically present as a firm, rubbery, painless nodule *inside* the eyelid, but rather as an eyelash growing inwards.
*Foreign body*
- A foreign body in the eye would typically cause acute onset of **pain, irritation, tearing**, and potentially redness.
- The persistent, painless, firm nodule described is less consistent with a foreign body, which would usually be more symptomatic or eventually expelled.
Epithelial glands US Medical PG Question 10: A 55-year-old woman comes to the physician because of a 2-week history of painful swelling on the right side of her face. The pain worsens when she eats. Examination of the face shows a right-sided, firm swelling that is tender to palpation. Oral examination shows no abnormalities. Ultrasonography shows a stone located in a duct that runs anterior to the masseter muscle and passes through the buccinator muscle. Sialoendoscopy is performed to remove the stone. At which of the following sites is the endoscope most likely to be inserted during the procedure?
- A. Lateral to the lingual frenulum
- B. Into the floor of the mouth
- C. Lateral to the superior labial frenulum
- D. Into the mandibular foramen
- E. Opposite the second upper molar tooth (Correct Answer)
Epithelial glands Explanation: ***Opposite the second upper molar tooth***
- The description of the duct running anterior to the **masseter muscle** and through the **buccinator muscle** is characteristic of the **parotid duct (Stensen's duct)**.
- The parotid duct opens into the oral cavity on the buccal mucosa **opposite the second upper molar tooth**, which is the most likely entry point for sialoendoscopy to remove a stone from this duct.
*Lateral to the lingual frenulum*
- This location is where the **submandibular duct (Wharton's duct)** opens into the oral cavity.
- While stones can occur in the submandibular duct, the patient's symptoms and the duct's anatomical description do not match this location.
*Into the floor of the mouth*
- The floor of the mouth is the general area where the submandibular and sublingual ducts open.
- However, the specific anatomical description of the duct in relation to the masseter and buccinator muscles points away from the submandibular/sublingual glands.
*Lateral to the superior labial frenulum*
- This area is associated with the openings of minor salivary glands in the upper lip.
- These glands are typically too small to be the source of such a prominent swelling or a large stone requiring sialoendoscopy.
*Into the mandibular foramen*
- The **mandibular foramen** is an opening on the medial surface of the mandibular ramus.
- It is an anatomical landmark for the **inferior alveolar nerve and vessels** and has no direct involvement in salivary gland duct openings.
More Epithelial glands US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.