Cartilage types and structure US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cartilage types and structure. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
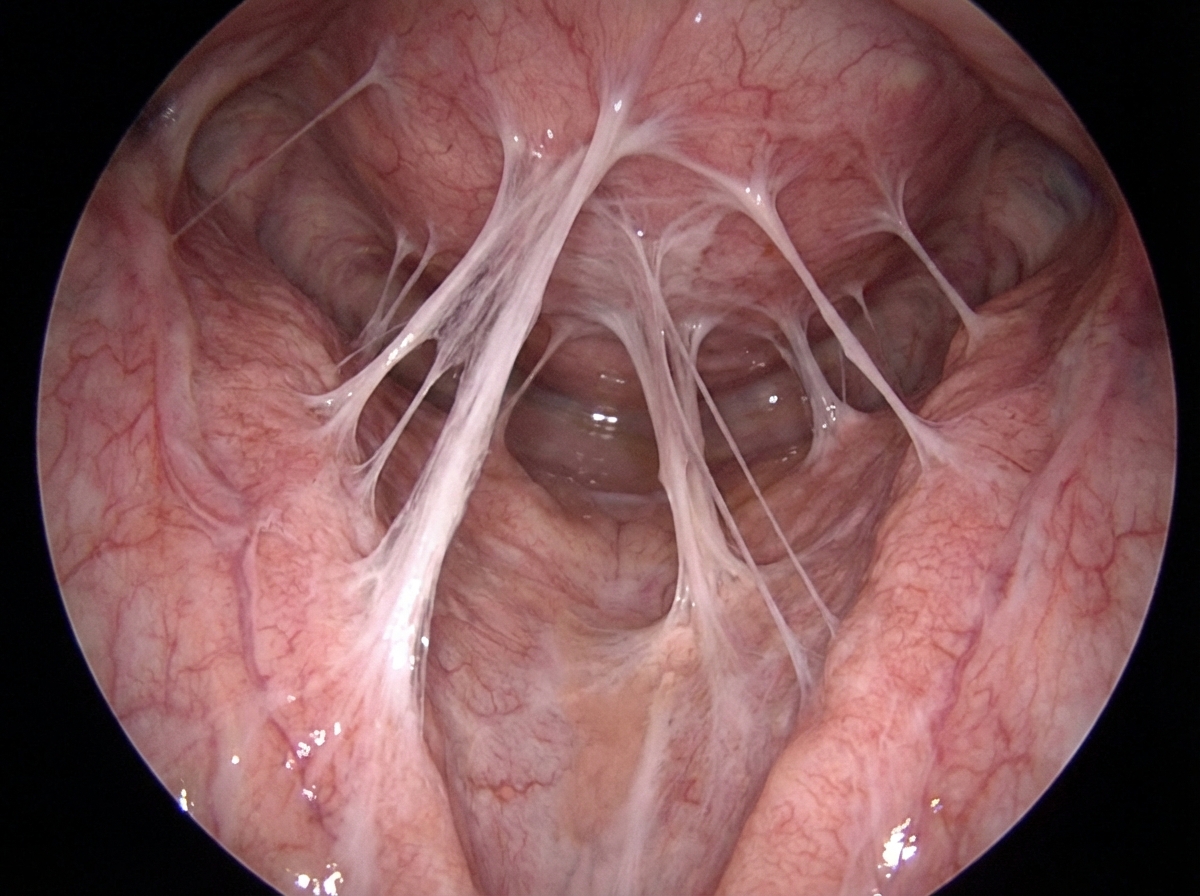
Cartilage types and structure US Medical PG Question 1: A 28-year-old woman and her husband are admitted to the office due to difficulties conceiving a child for the past year. Her menarche was at the age of 15 years, and her periods have been regular since then. Her medical history is positive for an abortion with curettage 5 years ago. A spermogram on the partner is performed, and it shows motile sperm cells. An ultrasound is performed on the patient and it is unremarkable. The laboratory results show that the FSH, LH, TSH, and prolactin levels are within normal ranges. A hysteroscopy is additionally performed and multiple adhesions are found in the uterus (refer to the image). Which of the following is the most likely composition of the scar tissue present in the uterus?
- A. Type 3 collagen
- B. Type 4 collagen
- C. Type 2 collagen
- D. Type 1 collagen (Correct Answer)
- E. Elastin
Cartilage types and structure Explanation: ***Type 1 collagen***
- This patient presents with **Asherman's syndrome**, characterized by intrauterine adhesions, often following uterine surgery like **curettage**. These adhesions are primarily composed of **Type 1 collagen**, which is the most abundant type of collagen in the human body and a major component of scar tissue.
- **Type 1 collagen** provides tensile strength and is crucial for wound healing and forming scar tissue in most connective tissues, including the uterus.
*Type 3 collagen*
- **Type 3 collagen** is found in distensible tissues like blood vessels, the uterus, and skin, and is important during the **early stages of wound healing**.
- While present in the uterus and initially involved in wound repair, **mature scar tissue** predominantly consists of **Type 1 collagen**.
*Type 4 collagen*
- **Type 4 collagen** is a major component of the **basal lamina**, a specialized extracellular matrix that underlies epithelial and endothelial cells.
- It does not form fibrillar structures and is not the primary component of robust scar tissue found in Asherman's syndrome.
*Type 2 collagen*
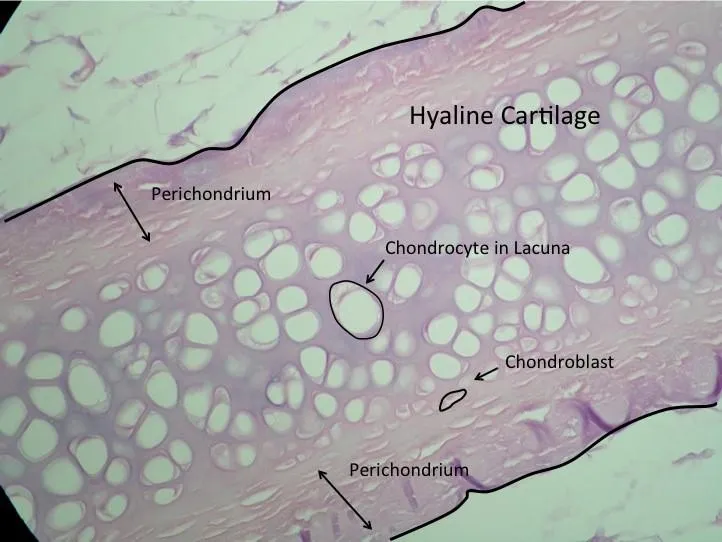
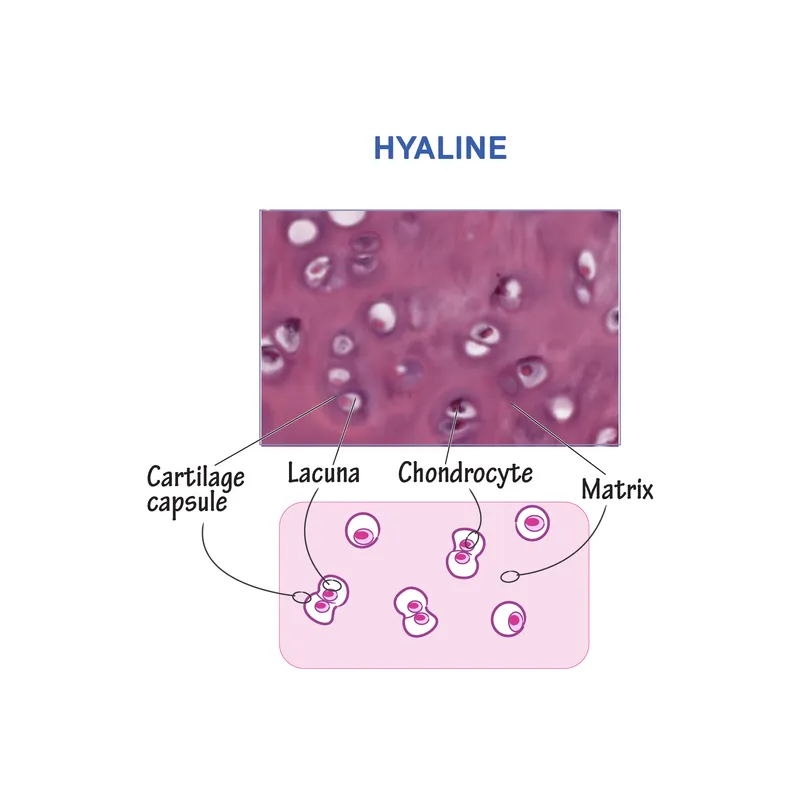
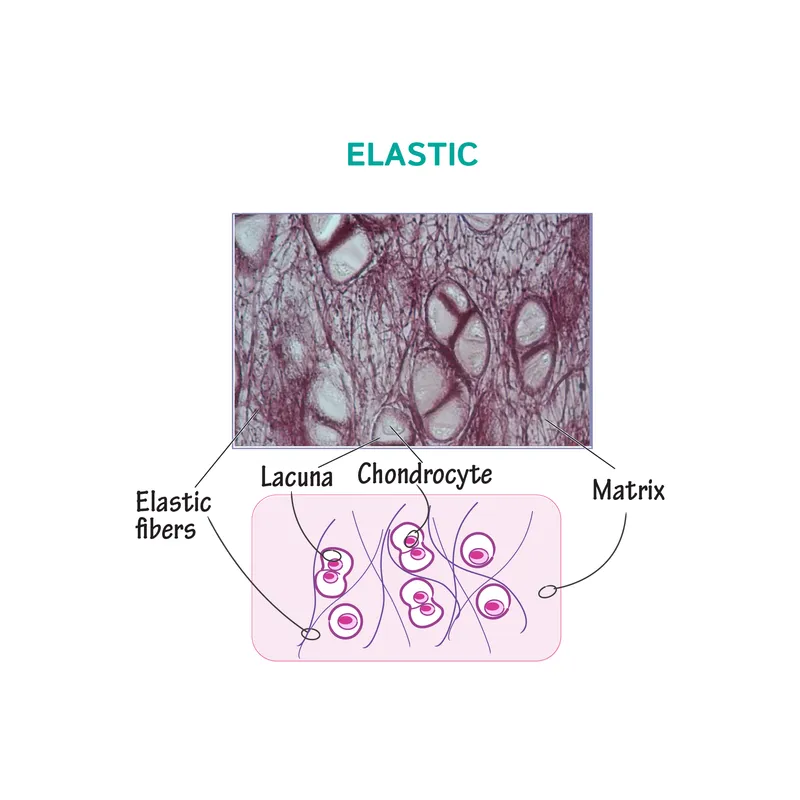
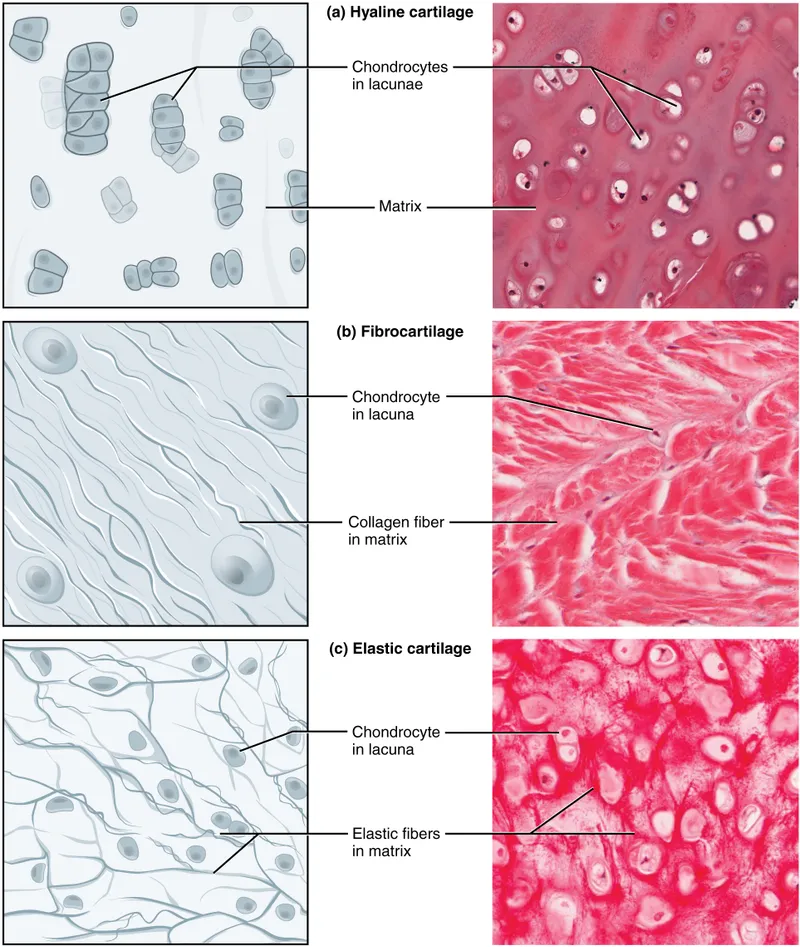
- **Type 2 collagen** is the main collagen type found in **hyaline cartilage** and elastic cartilage, providing resistance to pressure.
- It is not found in significant amounts in uterine tissue or scar tissue formed within the uterus.
*Elastin*
- **Elastin** is a protein that provides **elasticity** to tissues like blood vessels, skin, and lungs, allowing them to stretch and recoil.
- While present in the uterus for its contractile properties, it is not the primary constituent of **fibrotic scar tissue** forming adhesions.
Cartilage types and structure US Medical PG Question 2: A 59-year-old woman comes to the physician because of a 1-year history of pain and stiffness in her fingers and knees. The stiffness lasts for about 10 minutes after she wakes up in the morning. She also reports that her knee pain is worse in the evening. She drinks one glass of wine daily. Her only medication is acetaminophen. She is 175 cm (5 ft 9 in) tall and weighs 102 kg (225 lb); BMI is 33 kg/m2. Physical examination shows firm nodules on the distal interphalangeal joints of the index, ring, and little fingers of both hands. Which of the following is the most likely diagnosis?
- A. Septic arthritis
- B. Pseudogout
- C. Gout
- D. Rheumatoid arthritis
- E. Osteoarthritis (Correct Answer)
Cartilage types and structure Explanation: ***Osteoarthritis***
* The patient's age (59 years), obesity (BMI 33 kg/m2), short duration of morning stiffness (10 minutes), evening worsening of knee pain, and the presence of **firm nodules on the distal interphalangeal joints** (Heberden's nodes) are classic signs of **osteoarthritis**.
* This condition is a common **degenerative joint disease** associated with wear and tear, often affecting weight-bearing joints and small joints of the hands.
*Septic arthritis*
* **Septic arthritis** typically presents with an acutely painful, hot, and swollen joint, often with systemic symptoms like fever and chills, which are absent here.
* The chronic, progressive nature of the patient's symptoms and the presence of bony nodules point away from an infectious cause.
*Pseudogout*
* **Pseudogout**, or calcium pyrophosphate deposition disease, involves the deposition of calcium pyrophosphate crystals, leading to episodes of acute, painful arthritis, often in larger joints like the knee.
* While it can affect the knee, the insidious onset, chronic pain, and specific hand nodules seen in this case are not typical features of pseudogout.
*Gout*
* **Gout** is characterized by sudden, severe attacks of pain, redness, and swelling, often affecting a single joint (commonly the great toe) due to **uric acid crystal deposition**.
* The patient's chronic pain pattern, multiple joint involvement (fingers and knees), and the description of firm nodules (not tophi) make gout less likely.
*Rheumatoid arthritis*
* **Rheumatoid arthritis** typically presents with morning stiffness lasting longer than 30 minutes, symmetrical polyarthritis, and often affects the **proximal interphalangeal (PIP)** and **metacarpophalangeal (MCP) joints** of the hands, sparing the DIP joints.
* The patient's short morning stiffness, DIP joint involvement, and the absence of systemic inflammatory signs argue against rheumatoid arthritis.
Cartilage types and structure US Medical PG Question 3: A 5-year-old girl accompanied by her mother presents to the emergency department after suffering a fall on the elementary school playground. Her mother reports that a child on the playground pushed her daughter who fell on her right side, after which she screamed and was found clutching her right leg. The girl's past medical history is significant for a fracture of the left femur and right radius over the past 2 years and an auditory deficit requiring hearing aid use starting 6 months ago. Inspection reveals a relatively short girl in moderate distress. She has brown opalescent teeth. She refuses to bear weight on her right lower extremity. Radiography of the right lower extremity reveals a femoral midshaft fracture. Which of the following is the most likely etiology of the patient's condition?
- A. Decreased cystathionine beta synthase activity
- B. Vitamin D deficiency
- C. Fibrillin gene defect
- D. Defective type I collagen production (Correct Answer)
- E. Type III collagen gene defect
Cartilage types and structure Explanation: **Defective type I collagen production**
- The patient's history of **recurrent fractures** from minor trauma, **auditory deficit**, and **brown opalescent teeth** (dentinogenesis imperfecta) are classic manifestations of **osteogenesis imperfecta**, a genetic disorder characterized by **defective type I collagen production**.
- **Type I collagen** is a major component of bone, dentin, and the sclera, and its deficiency leads to brittle bones, hearing loss due to ossicle abnormalities, and dental defects.
*Decreased cystathionine beta synthase activity*
- This condition describes **homocystinuria**, which can present with skeletal abnormalities and developmental delays.
- However, typical features include **marfanoid habitus**, **lens luxation**, and **thromboembolic events**, which are not reported in this patient.
*Vitamin D deficiency*
- **Vitamin D deficiency** leads to **rickets** in children, characterized by bone pain, muscle weakness, and skeletal deformities but typically presents with **bowing of legs**, **rachitic rosary**, and **craniotabes**, not recurrent fractures from minor trauma or opalescent teeth.
- While it weakens bones, the constellation of symptoms here, especially dental and auditory deficits, points away from simple vitamin D deficiency.
*Fibrillin gene defect*
- A **fibrillin gene defect** is characteristic of **Marfan syndrome**, which presents with **long limbs**, **arachnodactyly**, **lens luxation**, and **aortic root dilation**.
- While it involves connective tissue, it does not typically cause the bone fragility and dental findings seen in this patient.
*Type III collagen gene defect*
- A **type III collagen gene defect** is associated with **Ehlers-Danlos syndrome, vascular type**, which features **easy bruising**, **fragile blood vessels**, and **organ rupture**.
- This condition leads to hypermobility and skin hyperextensibility, but not the specific combination of brittle bones, hearing loss, and dental defects seen in this patient.
Cartilage types and structure US Medical PG Question 4: A 35-year-old man comes to the physician for evaluation of a neck mass and hoarseness. He has no history of major medical illness. Physical examination shows a 2.5-cm fixed, irregular thyroid nodule. His serum calcitonin concentration is elevated. The nodule is most likely comprised of cells that are embryologically derived from which of the following structures?
- A. Second branchial pouch
- B. Fourth branchial arch
- C. Surface ectoderm
- D. Third branchial pouch
- E. Neural crest cells (Correct Answer)
Cartilage types and structure Explanation: ***Neural crest cells***
- The elevated **serum calcitonin** in the presence of a thyroid nodule is highly suggestive of **medullary thyroid carcinoma (MTC)**.
- **MTC** originates from the **parafollicular C cells** of the thyroid, which are embryologically derived from **neural crest cells** that migrate to the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) during development and subsequently integrate into the thyroid gland.
- This is the definitive embryological origin of calcitonin-producing C cells.
*Second branchial pouch*
- The second branchial pouch typically gives rise to the **palatine tonsil crypts** and **tonsillar fossa**.
- It is not associated with the development of the **parafollicular C cells** or thyroid malignancies.
*Fourth branchial arch*
- The fourth branchial arch gives rise to the **superior laryngeal nerve** and associated laryngeal cartilages.
- While the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) does contribute C cells to the thyroid, these cells themselves are derived from **neural crest cells** that migrate to this structure, not from the pouch itself.
- Therefore, the embryological origin is neural crest, not the branchial arch/pouch.
*Surface ectoderm*
- Surface ectoderm forms structures such as the **epidermis of the skin**, **hair**, **nails**, and **lens of the eye**.
- It does not contribute to the development of the **C cells** or the thyroid gland.
*Third branchial pouch*
- The third branchial pouch gives rise to the **inferior parathyroid glands** and the majority of the **thymus**.
- While it contributes to endocrine tissues, it does not form the **parafollicular C cells** of the thyroid.
Cartilage types and structure US Medical PG Question 5: Collagen is a very critical structural protein in many of our connective tissues. Defects in collagen produce diseases such as Ehlers-Danlos syndrome, where there is a defective lysyl hydroxylase gene, or osteogenesis imperfecta, where there is a defect in the production of type I collagen. Which of the following represents the basic repeating tripeptide of collagen?
- A. Gly-X-Y (Correct Answer)
- B. Asp-X-Y
- C. Met-X-Y
- D. Ser-X-Y
- E. Glu-X-Y
Cartilage types and structure Explanation: ***Gly-X-Y***
- The **basic repeating tripeptide unit of collagen** is **Glycine-X-Y**, where X and Y are often **proline** and **hydroxyproline**, respectively.
- **Glycine** is essential at every third position because its small side chain allows for the tight packing of the **collagen triple helix**.
*Asp-X-Y*
- **Aspartate (Asp)** is an **acidic amino acid** and is not typically found at the first position of the repeating tripeptide unit of collagen.
- Its bulky side chain would hinder the tight coiling of the **collagen helix**.
*Met-X-Y*
- **Methionine (Met)** is a **hydrophobic amino acid** and, while important in other proteins, it does not occupy the critical first position in the repeating collagen tripeptide.
- The unique structural requirements of collagen favor **glycine** at this position for optimal packing.
*Ser-X-Y*
- **Serine (Ser)** is a **polar, uncharged amino acid** and, like aspartate and methionine, is not the primary amino acid found at the first position of the repeating collagen tripeptide.
- The small size of **glycine** is crucial for collagen's characteristic triple helix.
*Glu-X-Y*
- **Glutamate (Glu)** is another **acidic amino acid** that is not typically found at the first position of the repeating tripeptide in collagen.
- Large or charged amino acids at this position would destabilize the **collagen secondary structure**.
Cartilage types and structure US Medical PG Question 6: An 11-year-old girl presents to her primary care physician because she has been having difficulty hearing her teachers at school. She says that the difficulty hearing started about a year ago, and it has slowly been getting worse. Her past medical history is significant for multiple fractures in both her upper and lower extremities. She also recently had a growth spurt and says that her friends say she is tall and lanky. A mutation in which of the following genes is most likely associated with this patient's condition?
- A. Type 4 collagen
- B. Type 3 collagen
- C. Fibrillin
- D. Type 1 collagen (Correct Answer)
- E. Fibroblast growth factor receptor
Cartilage types and structure Explanation: ***Type 1 collagen***
- This patient's symptoms—hearing difficulty, multiple fractures, and tall/lanky stature—are classic signs of **osteogenesis imperfecta (OI)**, a genetic disorder caused by mutations in genes encoding **Type I collagen**.
- **Type I collagen** is a major component of bone, so defects lead to fragile bones and susceptibility to fractures, and it also plays a role in the structure of the ear, affecting hearing.
*Type 4 collagen*
- Mutations in **Type 4 collagen** are primarily associated with **Alport syndrome**, which classically presents with **hematuria**, progressive renal failure, and hearing loss.
- While hearing loss is present, the patient's other key symptoms of **multiple fractures** and **tall, lanky stature** are not characteristic of Alport syndrome.
*Type 3 collagen*
- Defects in **Type 3 collagen** are linked to **Ehlers-Danlos syndrome, vascular type**, which is characterized by fragile blood vessels, organs, and skin, leading to easy bruising, arterial rupture, and bowel perforation.
- While Type 3 collagen is found in connective tissues, its primary clinical manifestations do not align with the patient's presentation of recurrent fractures and hearing loss.
*Fibrillin*
- Mutations in **fibrillin-1** are responsible for **Marfan syndrome**, which presents with tall stature, long limbs (**arachnodactyly**), and cardiovascular issues like aortic dilation.
- While tall stature is observed, the patient's primary complaints of **recurrent fractures** and hearing loss are not typical features of Marfan syndrome.
*Fibroblast growth factor receptor*
- Mutations in **fibroblast growth factor receptor 3 (FGFR3)** are most commonly associated with **achondroplasia**, a form of dwarfism characterized by short stature, short limbs, and a large head.
- This is inconsistent with the patient's **tall and lanky stature** and does not account for the recurrent fractures or hearing difficulties.
Cartilage types and structure US Medical PG Question 7: In which of the following pathological states would the oxygen content of the trachea resemble the oxygen content in the affected alveoli?
- A. Emphysema
- B. Exercise
- C. Pulmonary embolism (Correct Answer)
- D. Pulmonary fibrosis
- E. Foreign body obstruction distal to the trachea
Cartilage types and structure Explanation: ***Pulmonary embolism***
- A pulmonary embolism blocks **blood flow** to a portion of the lung, creating **dead space ventilation** (high V/Q ratio).
- In the affected alveoli, **no blood perfusion** means no oxygen extraction occurs, so the alveolar oxygen content remains **high and similar to tracheal/inspired air**.
- This is the classic physiological state where ventilation continues but perfusion is absent, preventing gas exchange.
*Foreign body obstruction distal to the trachea*
- A complete obstruction **prevents fresh air** from reaching the affected alveoli.
- The trapped gas undergoes **resorption atelectasis**: oxygen is absorbed into capillary blood, CO2 diffuses in, and alveolar gas equilibrates with **venous blood** composition.
- Alveolar oxygen content becomes **very low**, not similar to tracheal air.
*Emphysema*
- Emphysema involves destruction of **alveolar walls** and enlargement of airspaces with impaired gas exchange.
- While V/Q mismatch occurs, oxygen is still extracted by perfusing blood.
- Alveolar oxygen content is **lower than tracheal air** due to ongoing (though inefficient) gas exchange.
*Exercise*
- During exercise, **oxygen consumption increases** dramatically with enhanced cardiac output and oxygen extraction.
- Alveolar oxygen content is **significantly lower** than tracheal air due to increased oxygen uptake by blood.
*Pulmonary fibrosis*
- Pulmonary fibrosis causes **thickening of the alveolar-capillary membrane**, impairing oxygen diffusion.
- Despite diffusion limitation, blood still perfuses the alveoli and extracts oxygen.
- Alveolar oxygen content is **lower than tracheal air**, though the A-a gradient is increased.
Cartilage types and structure US Medical PG Question 8: An investigator is studying the structural integrity of collagen. Human fibroblasts are cultured on a medium and different enzymes are applied. One of the cultures is supplemented with an enzyme that inhibits lysyl oxidase, preventing the formation of covalent cross-links between collagen α-chains. Which of the following processes is most likely to be impaired as a result?
- A. Internal elastic lamina formation
- B. Ligament relaxation
- C. Osteoclast activation
- D. Bone matrix synthesis (Correct Answer)
- E. Cartilaginous growth plate mineralization
Cartilage types and structure Explanation: ***Bone matrix synthesis***
* **Collagen** is the primary organic component of the bone matrix (osteoid), and its proper cross-linking through **lysyl oxidase-mediated covalent bonds** is crucial for structural integrity and subsequent mineralization.
* **Lysyl oxidase** converts lysine and hydroxylysine residues to aldehydes (allysine and hydroxyallysine), which then form **aldol condensations and Schiff bases** to create stable cross-links between collagen fibrils.
* Inhibiting lysyl oxidase directly compromises the formation of stable collagen fibrils, which are essential for **osteoid production** and bone strength, leading to conditions like **lathyrism** (seen with β-aminopropionitrile exposure).
*Incorrect Option: Internal elastic lamina formation*
* The **internal elastic lamina** is primarily composed of **elastin**, not collagen, and provides arterial elasticity.
* While elastin also requires lysyl oxidase for cross-linking (desmosine and isodesmosine formation), the question specifically asks about **collagen α-chains**, making bone matrix synthesis the more direct answer.
*Incorrect Option: Ligament relaxation*
* **Ligament relaxation** refers to increased laxity, primarily influenced by hormones like relaxin during pregnancy.
* Impairing collagen cross-linking would lead to **ligament weakness and fragility** rather than physiologic relaxation, potentially causing joint instability.
*Incorrect Option: Osteoclast activation*
* **Osteoclast activation** involves bone resorption, regulated by **RANK/RANKL/OPG signaling**, and is independent of newly synthesized collagen cross-linking.
* While collagen integrity affects bone quality, lysyl oxidase inhibition impairs **osteoblast-mediated bone formation**, not osteoclast function.
*Incorrect Option: Cartilaginous growth plate mineralization*
* **Growth plate mineralization** involves calcium phosphate crystal deposition within cartilage matrix, regulated by chondrocytes and factors like alkaline phosphatase.
* While collagen integrity is important in cartilage, the defect in collagen cross-linking most critically affects **bone matrix (osteoid)** synthesis, where type I collagen predominates and provides the scaffold for mineralization.
Cartilage types and structure US Medical PG Question 9: An MRI of a patient with low back pain reveals compression of the L5 nerve root. Which of the following muscles would most likely show weakness during physical examination?
- A. Tibialis posterior
- B. Tibialis anterior (Correct Answer)
- C. Gastrocnemius
- D. Quadriceps femoris
Cartilage types and structure Explanation: ***Tibialis anterior***
- The **L5 nerve root** primarily innervates muscles responsible for **dorsiflexion** of the foot, with the **tibialis anterior** being the primary dorsiflexor.
- Weakness of the tibialis anterior would manifest as difficulty lifting the front of the foot, potentially leading to a **foot drop** gait.
*Tibialis posterior*
- The **tibialis posterior** is primarily innervated by the **tibial nerve** (S1-S2) and is responsible for **plantarflexion** and **inversion** of the foot.
- Weakness in this muscle would not be the most likely presentation of L5 nerve root compression.
*Gastrocnemius*
- The **gastrocnemius** muscle is primarily innervated by the **tibial nerve** (S1-S2) and is a powerful **plantarflexor** of the foot.
- Weakness in this muscle would indicate an S1 or S2 nerve root issue, not typically L5.
*Quadriceps femoris*
- The **quadriceps femoris** is innervated by the **femoral nerve**, predominantly originating from the **L2, L3, and L4 nerve roots**.
- Weakness would manifest as difficulty extending the knee, which is not characteristic of L5 compression.
Cartilage types and structure US Medical PG Question 10: A 3-month-old infant presents with severe joint hypermobility, skin hyperextensibility, and delayed wound healing. Skin biopsy shows abnormal collagen fibril organization with irregular diameter and reduced tensile strength. Genetic testing reveals a mutation affecting lysyl hydroxylase, an enzyme involved in collagen post-translational modification. The family asks about prognosis and potential complications. Synthesize the biochemical defect with clinical manifestations to determine the most critical pathophysiological mechanism.
- A. Impaired collagen synthesis at the ribosomal level
- B. Defective hydroxylation of lysine residues preventing stable collagen cross-linking (Correct Answer)
- C. Excessive collagen degradation by matrix metalloproteinases
- D. Abnormal glycosylation affecting collagen secretion
- E. Impaired procollagen cleavage preventing fibril formation
Cartilage types and structure Explanation: ***Defective hydroxylation of lysine residues preventing stable collagen cross-linking***
- **Lysyl hydroxylase** is essential for the post-translational hydroxylation of lysine; its deficiency impairs the formation of **hydroxylysine**, which is crucial for stable **covalent cross-linking**.
- This biochemical defect results in **reduced tensile strength** of collagen fibrils, leading to the classic clinical triad of **joint hypermobility**, **skin hyperextensibility**, and **delayed wound healing** seen in Kyphoscoliotic Ehlers-Danlos Syndrome.
*Impaired collagen synthesis at the ribosomal level*
- Ribosomal synthesis pertains to the translation of **pre-procollagen** alpha chains; however, this patient has a post-translational enzyme mutation.
- Defects at the **ribosomal level** would lead to a quantitative lack of protein rather than the **abnormal fibril organization** and diameter irregularities described.
*Excessive collagen degradation by matrix metalloproteinases*
- **Matrix metalloproteinases (MMPs)** are involved in tissue remodeling and chronic inflammation, not primary genetic collagen disorders.
- While MMP activity can affect tissue integrity, the clinical presentation and **genetic testing** specifically point to a synthesis/modification defect, not an overactive degradation pathway.
*Abnormal glycosylation affecting collagen secretion*
- **Glycosylation** occurs on hydroxylysine residues in the Golgi apparatus; while related to post-translational modification, it is not the primary function of **lysyl hydroxylase**.
- Primary defects in collagen **glycosylation** or **secretion** usually present with more severe multi-systemic growth delays rather than the specific mechanical fragility seen here.
*Impaired procollagen cleavage preventing fibril formation*
- This mechanism describes **Arthrochalasia** or **Dermatosparaxis** types of EDS, where **procollagen N-peptidase** or C-peptidase is deficient.
- Failure to cleave **terminal propeptides** prevents the formation of insoluble tropocollagen, but this is distinct from the **lysyl hydroxylase** deficiency identified by this patient's genetic testing.
More Cartilage types and structure US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.