Bone structure and types US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bone structure and types. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bone structure and types US Medical PG Question 1: A scientist is studying the anatomy and function of bone growth. He is able to create a cell line of osteocytes with a mutation that prevents the osteocytes from exchanging nutrients and waste products within neighboring lamellae. This mutation most likely affected which of the following cell structures?
- A. Dynein
- B. Gap junctions (Correct Answer)
- C. Endoplasmic reticulum
- D. Plasma membrane
- E. Kinesin
Bone structure and types Explanation: ***Gap junctions***
- **Gap junctions** are specialized intercellular connections that permit direct communication and exchange of small molecules and ions between adjacent cells.
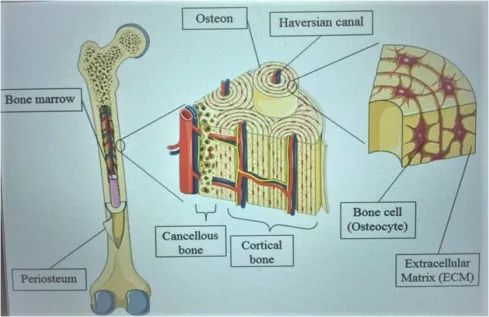
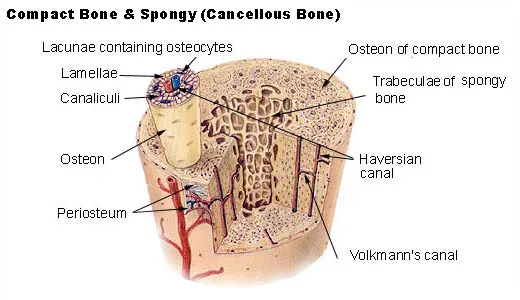
- In osteocytes, **gap junctions** located in the **canaliculi** are crucial for the exchange of nutrients, waste, and signaling molecules within and between lamellae, allowing for synchronous activity and maintaining bone health.
- These connexin-based channels physically connect the cytoplasm of neighboring osteocytes embedded in bone matrix.
*Dynein*
- **Dynein** is a motor protein involved in intracellular transport towards the minus end of **microtubules**, playing a role in moving organelles and vesicles.
- It is not directly responsible for the intercellular exchange of nutrients and waste products between cells.
*Endoplasmic reticulum*
- The **endoplasmic reticulum** is an organelle involved in protein synthesis and lipid metabolism, playing a critical role in cellular function.
- It does not directly mediate the exchange of nutrients and waste products between adjacent cells.
*Plasma membrane*
- While **gap junctions** are embedded within the **plasma membrane**, the membrane itself does not facilitate direct cytoplasmic continuity between cells.
- The question specifically refers to structures that enable direct cell-to-cell exchange; the mutation affects the gap junction channels themselves (connexins), not the general plasma membrane structure.
- Without functional gap junctions, the plasma membrane alone cannot support the intercellular communication required for osteocyte networks.
*Kinesin*
- **Kinesin** is a motor protein that moves cargo along **microtubules** towards the plus end, involved in fundamental cellular processes like cell division and organelle transport.
- It is not involved in direct intercellular communication for nutrient and waste exchange but rather internal cellular trafficking.
Bone structure and types US Medical PG Question 2: A researcher is studying physiologic and hormonal changes that occur during pregnancy. Specifically, they examine the behavior of progesterone over the course of the menstrual cycle and find that it normally decreases over time; however, during pregnancy this decrease does not occur in the usual time frame. The researcher identifies a circulating factor that appears to be responsible for this difference in progesterone behavior. In order to further examine this factor, the researcher denatures the circulating factor and examines the sizes of its components on a western blot as compared to several other hormones. One of the bands the researcher identifies in this circulating factor is identical to that of another known hormone with which of the following sites of action?
- A. Thyroid gland (Correct Answer)
- B. Adrenal gland
- C. Adipocytes
- D. Bones
- E. Kidney tubules
Bone structure and types Explanation: ***Correct: Thyroid gland***
- The circulating factor described is **human chorionic gonadotropin (hCG)**, which maintains the corpus luteum and progesterone production during early pregnancy
- hCG is a **glycoprotein hormone** composed of an **α subunit** and a **β subunit**
- The **α subunit of hCG is identical** to the α subunits of **TSH (thyroid-stimulating hormone)**, **LH (luteinizing hormone)**, and **FSH (follicle-stimulating hormone)**
- When denatured and examined on Western blot, one of the bands (the α subunit) would be identical to that of **TSH**
- **TSH acts on the thyroid gland** to stimulate thyroid hormone synthesis and release
- This structural similarity explains why very high levels of hCG (as in molar pregnancy or hyperemesis gravidarum) can sometimes cause **thyrotoxicosis** due to cross-reactivity with TSH receptors
*Incorrect: Adrenal gland*
- **ACTH (adrenocorticotropic hormone)** acts on the adrenal cortex to stimulate cortisol production
- ACTH is a **peptide hormone** derived from POMC (pro-opiomelanocortin) and does **NOT share any structural components** with hCG
- There is no identical band between hCG and ACTH on Western blot
*Incorrect: Adipocytes*
- Adipocytes are regulated by hormones like **insulin** and **leptin**
- Neither of these hormones share structural components with hCG
*Incorrect: Bones*
- Bones are primarily regulated by **PTH (parathyroid hormone)**, **calcitonin**, and **vitamin D**
- None of these hormones share structural components with hCG
*Incorrect: Kidney tubules*
- Kidney tubules are regulated by **ADH (antidiuretic hormone/vasopressin)** and **aldosterone**
- Neither shares structural components with hCG
Bone structure and types US Medical PG Question 3: A 3-year-old child is brought to the emergency department with multiple bruises in various stages of healing. X-rays reveal several metaphyseal fractures and posterior rib fractures. The parents claim the injuries resulted from normal play activities. Which of the following patterns would most strongly suggest non-accidental trauma?
- A. Circular bruises on the knees
- B. Loop-shaped bruises on the back (Correct Answer)
- C. Linear bruises on the shins
- D. Irregular bruises on the forehead
Bone structure and types Explanation: ***Loop-shaped bruises on the back***
- **Loop-shaped bruises** are highly suspicious for **non-accidental trauma** as they are pathognomonic for impact with an object like a looped cord or belt
- Bruises on the **back** of a young child are particularly concerning as the back is a non-bony prominence and less likely to be injured during normal play activities
- Combined with the metaphyseal and posterior rib fractures already identified, patterned bruises strongly indicate inflicted trauma
*Circular bruises on the knees*
- Circular bruises on the knees are very common in toddlers and young children due to normal falls and play, which typically involve kneeling and crawling
- This pattern is generally considered consistent with accidental injury and not indicative of abuse
*Linear bruises on the shins*
- Linear bruises on the shins can result from bumping into objects while playing or exploring, which is common in active children
- The shins are bony prominences frequently injured during normal play activities
*Irregular bruises on the forehead*
- Irregular bruises on the forehead can result from accidental falls or bumps, which are common in young children learning to walk or play
- While head injuries should always be carefully evaluated, irregular bruises on the forehead are common accidental injuries in ambulatory toddlers
Bone structure and types US Medical PG Question 4: A 7-year-old girl presents to her primary care physician for a routine check-up. The physician allows the medical student to perform a physical examination. The medical student notes hearing impairment as well as the findings show in Figures A and B. Radiographs show indications of multiple old fractures of the humerus that have healed. After questioning the girl’s parents, the medical student learns that in addition, the patient is extremely picky with her food and eats a diet consisting mainly of cereal and pasta. What is the most likely etiology of the patient’s disease?
- A. Dietary deficiency of ascorbic acid
- B. Defect in type I collagen (Correct Answer)
- C. Defective mineralization of cartilage
- D. Decreased bone mineral density
- E. Non-accidental trauma
Bone structure and types Explanation: ***Defect in type I collagen***
- The constellation of **frequent fractures**, **hearing impairment**, and **blue sclerae** (as indicated by Figure A, which shows a bluish tint to the white part of the eye) is characteristic of **osteogenesis imperfecta (OI)**, a genetic disorder caused by mutations in COL1A1 or COL1A2 genes leading to **defective type I collagen synthesis**.
- Type I collagen is the primary structural protein in bone, and defects result in brittle bones, blue sclerae (due to thin sclera allowing choroid visibility), and conductive hearing loss (from ossicle abnormalities).
- While the patient's diet is described as "picky," the primary features point towards a genetic collagen defect rather than a nutritional deficiency as the underlying cause for the bone and connective tissue abnormalities.
*Dietary deficiency of ascorbic acid*
- A deficiency in **ascorbic acid (vitamin C)** leads to **scurvy**, characterized by **gingivitis**, **poor wound healing**, **petechiae**, and easy bruising due to impaired collagen synthesis.
- While collagen synthesis is affected, the specific presentation of blue sclerae, hearing impairment, and multiple fractures as primary symptoms is not typical for scurvy.
*Defective mineralization of cartilage*
- **Defective mineralization of cartilage** often points to **rickets in children** or **osteomalacia in adults**, usually due to **vitamin D deficiency** or disorders of phosphate metabolism.
- While these conditions can cause bone fragility, they do not typically present with blue sclerae or hearing impairment as defining features. The "old fractures" suggest a chronic bone fragility predating any acute nutritional issues.
*Decreased bone mineral density*
- **Decreased bone mineral density (BMD)** is a general term seen in many conditions, including **osteoporosis** and **osteogenesis imperfecta**.
- While the patient likely has decreased BMD due to their frequent fractures, this option describes a symptom rather than the **underlying etiology** of the disorder.
*Non-accidental trauma*
- **Non-accidental trauma (child abuse)** should always be considered in a child with multiple fractures.
- However, the presence of other systemic findings like **blue sclerae** and **hearing impairment** strongly suggests an underlying genetic disorder like osteogenesis imperfecta, making non-accidental trauma less likely as the primary cause for all observed symptoms.
Bone structure and types US Medical PG Question 5: A 35-year-old man comes to the physician for evaluation of a neck mass and hoarseness. He has no history of major medical illness. Physical examination shows a 2.5-cm fixed, irregular thyroid nodule. His serum calcitonin concentration is elevated. The nodule is most likely comprised of cells that are embryologically derived from which of the following structures?
- A. Second branchial pouch
- B. Fourth branchial arch
- C. Surface ectoderm
- D. Third branchial pouch
- E. Neural crest cells (Correct Answer)
Bone structure and types Explanation: ***Neural crest cells***
- The elevated **serum calcitonin** in the presence of a thyroid nodule is highly suggestive of **medullary thyroid carcinoma (MTC)**.
- **MTC** originates from the **parafollicular C cells** of the thyroid, which are embryologically derived from **neural crest cells** that migrate to the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) during development and subsequently integrate into the thyroid gland.
- This is the definitive embryological origin of calcitonin-producing C cells.
*Second branchial pouch*
- The second branchial pouch typically gives rise to the **palatine tonsil crypts** and **tonsillar fossa**.
- It is not associated with the development of the **parafollicular C cells** or thyroid malignancies.
*Fourth branchial arch*
- The fourth branchial arch gives rise to the **superior laryngeal nerve** and associated laryngeal cartilages.
- While the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) does contribute C cells to the thyroid, these cells themselves are derived from **neural crest cells** that migrate to this structure, not from the pouch itself.
- Therefore, the embryological origin is neural crest, not the branchial arch/pouch.
*Surface ectoderm*
- Surface ectoderm forms structures such as the **epidermis of the skin**, **hair**, **nails**, and **lens of the eye**.
- It does not contribute to the development of the **C cells** or the thyroid gland.
*Third branchial pouch*
- The third branchial pouch gives rise to the **inferior parathyroid glands** and the majority of the **thymus**.
- While it contributes to endocrine tissues, it does not form the **parafollicular C cells** of the thyroid.
Bone structure and types US Medical PG Question 6: A 42-year-old woman comes to the physician with acute, severe pain in the middle of her lower back. She also complains of constipation and trouble sleeping recently. Menses occur regularly at 28-day intervals. Examination shows localized tenderness to palpation over the lumbar spine. Serum calcium is 14 mg/dL and serum phosphorus is 1.5 mg/dL. An x-ray of the lumbar spine shows a compression fracture of the L4 vertebral body and osteopenia. Which of the following is the most likely underlying cause of this patient's decreased bone mineral density?
- A. Increase in parathyroid hormone secretion (Correct Answer)
- B. Decrease in RANKL expression
- C. Decrease in osteoblast activity
- D. Increase in calcitonin secretion
- E. Decrease in estrogen production
Bone structure and types Explanation: ***Increase in parathyroid hormone secretion***
- This patient presents with the classic triad of **primary hyperparathyroidism**: hypercalcemia (14 mg/dL), hypophosphatemia (1.5 mg/dL), and bone disease (compression fracture with osteopenia).
- **PTH excess** causes increased bone resorption by stimulating osteoclast activity, leading to decreased bone mineral density and pathologic fractures.
- PTH increases renal phosphate excretion (causing hypophosphatemia) and increases calcium reabsorption and bone resorption (causing hypercalcemia).
- The **constipation is a manifestation of hypercalcemia** ("stones, bones, abdominal groans, and psychiatric overtones").
- Primary hyperparathyroidism is the most common cause of hypercalcemia in outpatients and frequently presents with osteopenia/osteoporosis.
*Decrease in estrogen production*
- While estrogen deficiency causes osteoporosis in postmenopausal women, this patient has **regular menses at 28-day intervals**, indicating she is not menopausal.
- Estrogen deficiency causes **normocalcemic osteoporosis**, not the hypercalcemia (14 mg/dL) and hypophosphatemia (1.5 mg/dL) seen in this patient.
- The laboratory abnormalities clearly point to a different etiology.
*Decrease in RANKL expression*
- RANKL (receptor activator of nuclear factor-κB ligand) stimulates osteoclast differentiation and activity.
- A **decrease** in RANKL would **reduce** osteoclast activity and **increase** bone mineral density, which is opposite to this patient's presentation.
- PTH actually works partly by increasing RANKL expression, further supporting hyperparathyroidism as the diagnosis.
*Decrease in osteoblast activity*
- While decreased osteoblast activity can contribute to low bone density, this is typically seen in conditions like multiple myeloma or aging.
- This mechanism does not explain the **hypercalcemia and hypophosphatemia** seen in this patient.
- The primary pathology here is **increased osteoclast activity** driven by excess PTH.
*Increase in calcitonin secretion*
- Calcitonin **lowers** serum calcium by inhibiting osteoclast activity.
- An increase in calcitonin would cause **hypocalcemia**, not the hypercalcemia (14 mg/dL) observed in this patient.
- This is physiologically opposite to the patient's presentation.
Bone structure and types US Medical PG Question 7: A 55-year-old male presents with left hip pain and stiffness. Radiographs are shown in Figures A and B. Serum alkaline phosphatase levels are elevated. A biopsy of the left femur is performed and shown in Figure C. Which of the following cells are initially responsible for this condition?
- A. T-Cells
- B. Fibroblasts
- C. Osteoblasts
- D. Osteoclasts (Correct Answer)
- E. Neutrophils
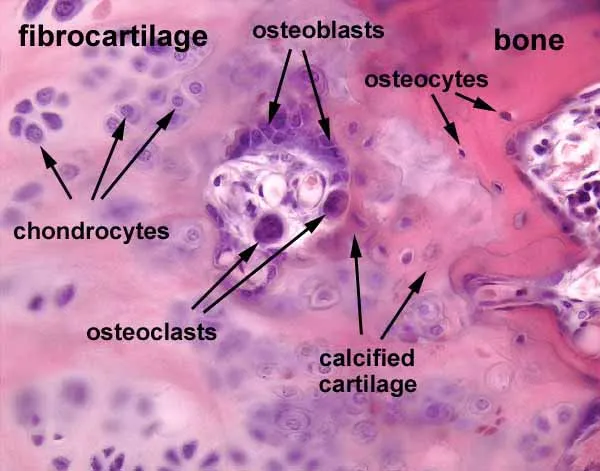
Bone structure and types Explanation: ***Osteoclasts***
- The presented images and elevated **alkaline phosphatase** strongly suggest **Paget's disease of bone**, which is characterized by abnormal bone remodeling initially driven by excessive osteoclastic activity.
- In Paget's disease, the initial phase involves a chaotic increase in **osteoclast** number and activity, leading to focal areas of excessive bone resorption.
*T-Cells*
- **T-cells** are primarily involved in immune responses and cell-mediated immunity rather than direct bone remodeling in Paget's disease.
- While immune factors may play a role in the pathogenesis of Paget's disease, **T-cells** are not the primary cells responsible for the initial destructive phase.
*Fibroblasts*
- **Fibroblasts** are connective tissue cells involved in producing collagen and extracellular matrix, important for tissue repair and scarring.
- They are not the main cells responsible for the initial abnormal bone resorption observed in Paget's disease.
*Osteoblasts*
- **Osteoblasts** are bone-forming cells responsible for synthesizing and depositing new bone matrix.
- In Paget's disease, osteoblastic activity is increased in a compensatory and disorganized manner following the initial osteoclastic hyperactivity, but they are not the cells _initially_ responsible for the condition.
*Neutrophils*
- **Neutrophils** are a type of white blood cell primarily involved in acute inflammatory responses to infections.
- They have no direct role in the primary pathogenesis of Paget's disease of bone.
Bone structure and types US Medical PG Question 8: A 33-year-old man presents to his primary care physician with shoulder pain. He states that he can't remember a specific instance when the injury occurred. He is a weight lifter and competes in martial arts. The patient has no past medical history and is currently taking a multivitamin. Physical exam demonstrates pain with abduction of the patient's right shoulder and with external rotation of the right arm. There is subacromial tenderness with palpation. His left arm demonstrates 10/10 strength with abduction as compared to 4/10 strength with abduction of the right arm. Which of the following best confirms the underlying diagnosis?
- A. Ultrasound
- B. Radiography
- C. MRI (Correct Answer)
- D. CT
- E. Physical exam and history
Bone structure and types Explanation: ***MRI***
- An **MRI is the gold standard** for diagnosing soft tissue injuries of the shoulder, including **rotator cuff pathology**, which is highly suspected given the patient's symptoms (pain with abduction and external rotation, subacromial tenderness, and weakness).
- It provides detailed imaging of tendons, ligaments, and cartilage, allowing for precise identification of **tears, inflammation, or impingement**.
*Ultrasound*
- While ultrasound can assess **rotator cuff integrity** and identify fluid collections, it is highly operator-dependent and may not provide the same level of detail as MRI for complex tears or associated pathologies.
- It can be a good initial screening tool but might **underestimate the extent** of an injury compared to MRI.
*Radiography*
- **Radiography (X-rays)** primarily visualizes bone structures and would be useful for detecting fractures, dislocations, or significant degenerative joint disease.
- It would **not directly visualize** the soft tissue injuries of the rotator cuff or other tendons that are likely causing this patient's symptoms.
*CT*
- **CT scans** provide excellent detail of bone structures and can identify subtle fractures, erosions, or bony impingement.
- However, like X-rays, they are **less effective for visualizing soft tissues** like tendons and ligaments compared to MRI.
*Physical exam and history*
- The **physical exam and history** are crucial for narrowing down the differential diagnosis and guiding further imaging.
- While strongly suggestive of a rotator cuff injury, they alone **cannot definitively confirm the extent or nature** of the underlying soft tissue pathology.
Bone structure and types US Medical PG Question 9: A 3-month-old infant presents with severe joint hypermobility, skin hyperextensibility, and delayed wound healing. Skin biopsy shows abnormal collagen fibril organization with irregular diameter and reduced tensile strength. Genetic testing reveals a mutation affecting lysyl hydroxylase, an enzyme involved in collagen post-translational modification. The family asks about prognosis and potential complications. Synthesize the biochemical defect with clinical manifestations to determine the most critical pathophysiological mechanism.
- A. Impaired collagen synthesis at the ribosomal level
- B. Defective hydroxylation of lysine residues preventing stable collagen cross-linking (Correct Answer)
- C. Excessive collagen degradation by matrix metalloproteinases
- D. Abnormal glycosylation affecting collagen secretion
- E. Impaired procollagen cleavage preventing fibril formation
Bone structure and types Explanation: ***Defective hydroxylation of lysine residues preventing stable collagen cross-linking***
- **Lysyl hydroxylase** is essential for the post-translational hydroxylation of lysine; its deficiency impairs the formation of **hydroxylysine**, which is crucial for stable **covalent cross-linking**.
- This biochemical defect results in **reduced tensile strength** of collagen fibrils, leading to the classic clinical triad of **joint hypermobility**, **skin hyperextensibility**, and **delayed wound healing** seen in Kyphoscoliotic Ehlers-Danlos Syndrome.
*Impaired collagen synthesis at the ribosomal level*
- Ribosomal synthesis pertains to the translation of **pre-procollagen** alpha chains; however, this patient has a post-translational enzyme mutation.
- Defects at the **ribosomal level** would lead to a quantitative lack of protein rather than the **abnormal fibril organization** and diameter irregularities described.
*Excessive collagen degradation by matrix metalloproteinases*
- **Matrix metalloproteinases (MMPs)** are involved in tissue remodeling and chronic inflammation, not primary genetic collagen disorders.
- While MMP activity can affect tissue integrity, the clinical presentation and **genetic testing** specifically point to a synthesis/modification defect, not an overactive degradation pathway.
*Abnormal glycosylation affecting collagen secretion*
- **Glycosylation** occurs on hydroxylysine residues in the Golgi apparatus; while related to post-translational modification, it is not the primary function of **lysyl hydroxylase**.
- Primary defects in collagen **glycosylation** or **secretion** usually present with more severe multi-systemic growth delays rather than the specific mechanical fragility seen here.
*Impaired procollagen cleavage preventing fibril formation*
- This mechanism describes **Arthrochalasia** or **Dermatosparaxis** types of EDS, where **procollagen N-peptidase** or C-peptidase is deficient.
- Failure to cleave **terminal propeptides** prevents the formation of insoluble tropocollagen, but this is distinct from the **lysyl hydroxylase** deficiency identified by this patient's genetic testing.
Bone structure and types US Medical PG Question 10: A 58-year-old woman undergoes cervical biopsy following an abnormal Pap smear. Histology shows full-thickness epithelial atypia with loss of cellular polarity, increased nuclear-to-cytoplasmic ratio, and numerous mitotic figures, but the basement membrane remains intact. Her oncologist discusses treatment options. The patient is concerned about progression risk versus overtreatment. Evaluate the most appropriate management strategy considering the tissue diagnosis and natural history.
- A. Observation only as basement membrane is intact
- B. Excisional procedure (LEEP or cone biopsy) with close surveillance (Correct Answer)
- C. Immediate radical hysterectomy
- D. Radiation therapy to prevent invasion
- E. Chemotherapy followed by reassessment
Bone structure and types Explanation: ***Excisional procedure (LEEP or cone biopsy) with close surveillance***
- The histology describes **CIN 3 (full-thickness atypia)**; since the **basement membrane is intact**, it is a high-grade pre-invasive lesion requiring definitive treatment to prevent progression to invasive cancer.
- An **excisional procedure** like **LEEP** or **cone biopsy** is the standard management to both treat the lesion and provide a complete specimen for histological review to rule out occult invasion.
*Observation only as basement membrane is intact*
- Observation is inappropriate for **CIN 3** because the risk of spontaneous progression to **invasive carcinoma** is significantly high.
- **Full-thickness atypia** necessitates active intervention, unlike lower-grade lesions (CIN 1) which may be monitored via surveillance.
*Immediate radical hysterectomy*
- A **radical hysterectomy** is considered overtreatment for a diagnosis where the **basement membrane is intact** (carcinoma in situ/CIN 3).
- Such invasive surgery is reserved for confirmed **invasive cervical cancer** cases, not for pre-invasive lesions that can be managed by local excision.
*Radiation therapy to prevent invasion*
- **Radiation therapy** is not indicated for **pre-invasive lesions** and is associated with significant long-term morbidity in the pelvic region.
- Primary management for **HSIL/CIN 3** is surgical excision, reserving radiation for higher-stage **invasive malignancies**.
*Chemotherapy followed by reassessment*
- There is no clinical role for **neoadjuvant chemotherapy** in the management of **cervical intraepithelial neoplasia (CIN)**.
- Management is strictly **surgical (excisional or ablative)** to remove the dysplastic cells before they can acquire the ability to invade the stroma.
More Bone structure and types US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.