Placenta and fetal membranes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Placenta and fetal membranes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Placenta and fetal membranes US Medical PG Question 1: A 42-year-old woman presents to the emergency department in active labor. She has had no prenatal care and is unsure of the gestational age. Labor progresses rapidly and spontaneous vaginal delivery of a baby boy occurs 3 hours after presentation. On initial exam, the child is 1.9 kg (4.2 lb) with a small head and jaw. A sac-like structure containing intestine, as can be seen in the picture, protrudes from the abdominal wall. What complication is closely associated with this presentation?
- A. Lack of abdominal wall muscles
- B. Dehydration and necrosis of bowel
- C. Duodenal atresia
- D. Twisting of the bowel around itself
- E. Cardiac defect (Correct Answer)
Placenta and fetal membranes Explanation: ***Cardiac defect***
- The presentation of a **sac-like structure containing intestine protruding from the abdominal wall** (suggesting an **omphalocele**) along with **microcephaly** (small head), **micrognathia** (small jaw), and **low birth weight** are classic features of **Patau syndrome (Trisomy 13)** or **Edwards syndrome (Trisomy 18)**.
- These chromosomal abnormalities are strongly associated with various significant anomalies, including severe **cardiac defects** (e.g., ventricular septal defects, patent ductus arteriosus, atrial septal defects), which occur in **>80% of cases**.
- **Omphalocele** itself is associated with cardiac anomalies in approximately **30-50% of cases**, making cardiac defects the most closely associated complication.
*Lack of abdominal wall muscles*
- This description is more indicative of **prune belly syndrome (Eagle-Barrett syndrome)**, characterized by absence or deficiency of abdominal wall musculature.
- With **gastroschisis**, there is also an abdominal wall defect, but the defect is typically lateral to the umbilicus and there is no protective sac covering the bowel.
*Dehydration and necrosis of bowel*
- This complication is more characteristic of **gastroschisis** due to the direct exposure of the unprotected bowel to amniotic fluid, leading to inflammation, thickening, and potential vascular compromise.
- In an **omphalocele**, the bowel is protected by a sac (containing peritoneum and amnion), significantly reducing the immediate risk of dehydration and necrosis unless the sac ruptures.
*Duodenal atresia*
- **Duodenal atresia** is strongly associated with **Down syndrome (Trisomy 21)**, characterized by a "double bubble" sign on imaging.
- While omphalocele can occasionally occur with Trisomy 21, the constellation of findings in this case (microcephaly, micrognathia, low birth weight) is more consistent with Trisomy 13 or 18 rather than Trisomy 21.
*Twisting of the bowel around itself*
- **Volvulus** refers to the twisting of a loop of intestine around its mesentery, which can lead to bowel obstruction and ischemia.
- While volvulus can occur with intestinal malrotation (which may be present with omphalocele), it is not the most closely associated **congenital** complication of the chromosomal syndrome suggested by this clinical presentation.
Placenta and fetal membranes US Medical PG Question 2: A 35-year-old G3P2 woman currently 39 weeks pregnant presents to the emergency department with painful vaginal bleeding shortly after a motor vehicle accident in which she was a passenger. She had her seat belt on and reports that the airbag deployed immediately upon her car's impact against a tree. She admits that she actively smokes cigarettes. Her prenatal workup is unremarkable. Her previous pregnancies were remarkable for one episode of chorioamnionitis that resolved with antibiotics. Her temperature is 98.6°F (37°C), blood pressure is 90/60 mmHg, pulse is 130/min, and respirations are 20/min. The fetal pulse is 110/min. Her uterus is tender and firm. The remainder of her physical exam is unremarkable. What is the most likely diagnosis?
- A. Placental abruption (Correct Answer)
- B. Eclampsia
- C. Vasa previa
- D. Preterm labor
- E. Preeclampsia
Placenta and fetal membranes Explanation: ***Placental abruption***
- The patient's presentation with **painful vaginal bleeding** after blunt abdominal trauma (motor vehicle accident), a **tender and firm uterus**, maternal **hypotension** and **tachycardia**, and fetal **bradycardia** is highly characteristic of placental abruption.
- Risk factors like **smoking** and trauma further increase the likelihood of placental abruption.
*Eclampsia*
- Eclampsia is characterized by **new-onset grand mal seizures** in a pregnant woman with preeclampsia, which is not present in this scenario.
- While the patient's low blood pressure and tachycardia are concerning, they do not point to eclampsia.
*Vasa previa*
- Vasa previa involves **fetal blood vessels** running within the fetal membranes over the internal cervical os, risking rupture during labor or membrane rupture, leading to **painless vaginal bleeding** and **fetal distress**.
- The bleeding in this case is described as painful, and the uterine tenderness and firmness are not typical of vasa previa.
*Preterm labor*
- Preterm labor is defined by **regular uterine contractions** causing cervical changes before 37 weeks of gestation, which is not aligned with the patient being 39 weeks pregnant or her symptoms.
- While trauma can initiate labor, the severity of the bleeding and maternal/fetal distress point away from isolated preterm labor.
*Preeclampsia*
- Preeclampsia is characterized by **new-onset hypertension** (blood pressure ≥140/90 mmHg) and **proteinuria** after 20 weeks of gestation.
- This patient presents with hypotension and no mention of hypertension or proteinuria, making preeclampsia unlikely.
Placenta and fetal membranes US Medical PG Question 3: A 31-year-old G3P0 is admitted to the hospital with profuse vaginal bleeding and abdominal pain at 34 weeks gestation. She reports passing bright blood with clots and no water in the discharge. She denies recent trauma or medical illnesses. She had no prenatal care. Her previous pregnancies culminated in spontaneous abortions in the second trimester. She has a 6-year history of drug abuse and cocaine smoking 2 hours prior to the onset of her symptoms. Her blood pressure is 160/90 mm Hg, the heart rate is 93/min, the respiratory rate is 19/min, and the temperature is 36.9℃ (98.4℉). The fetal heart rate is 110/min. On examination, the patient is lethargic. Her pupils are constricted, but reactive to light bilaterally. There are no signs of trauma. Abdominal palpation identifies lower abdominal tenderness and strong uterine contractions. The fundus of the uterus is between the xiphoid process and umbilicus. The patient’s perineum is grossly bloody. On pelvic examination, the vaginal canal is without lesions. The cervix is almost completely effaced and 2 cm dilated. Which of the following options is the most likely cause of the patient’s pregnancy-related condition?
- A. Thrombosis of the placental vessels
- B. Dramatic decrease in thrombocytes
- C. Premature rupture of the membranes
- D. Rupture of the placental vessels
- E. Abrupt constriction of maternal and placental vessels (Correct Answer)
Placenta and fetal membranes Explanation: ***Abrupt constriction of maternal and placental vessels***
- The patient's presentation with **profuse vaginal bleeding**, **abdominal pain**, **strong uterine contractions**, **hypertension**, and a history of **cocaine use** strongly points to **placental abruption**. Cocaine causes abrupt and severe vasoconstriction, leading to placental detachment.
- The **firm and tender uterus**, coupled with **fetal distress** (fetal heart rate of 110/min), is characteristic of placental abruption due to the accumulation of blood behind the placenta and uterine hypertonicity.
*Thrombosis of the placental vessels*
- While thrombosis can affect the placenta, it typically leads to **placental insufficiency** and **fetal growth restriction**, not acute, profuse vaginal bleeding with contractions.
- **Thrombosis** alone does not explain the sudden onset of severe abdominal pain and uterine hypertonicity seen in this case.
*Dramatic decrease in thrombocytes*
- A dramatic decrease in thrombocytes (thrombocytopenia) would cause **generalized bleeding diathesis**, often with petechiae, purpura, or bleeding from other sites, not typically isolated profuse vaginal bleeding with uterine pain and contractions.
- While severe **placental abruption** can lead to **disseminated intravascular coagulation (DIC)** and secondary thrombocytopenia, the primary cause of bleeding here is the placental detachment, not a pre-existing low platelet count.
*Premature rupture of the membranes*
- **Premature rupture of membranes (PROM)** involves the leakage of **amniotic fluid** ("water breaking"), which the patient explicitly denies.
- Although PROM can precede preterm labor, it does not directly cause profuse vaginal bleeding, severe abdominal pain, and uterine hypertonicity in the absence of placental abruption.
*Rupture of the placental vessels*
- **Rupture of placental vessels** without abruption (e.g., vasa previa) typically presents with **painless vaginal bleeding** and rapid **fetal compromise**, but usually without significant maternal abdominal pain or strong uterine contractions.
- The context of **cocaine use** and its known effect on vasoconstriction directly points to placental abruption rather than isolated vessel rupture.
Placenta and fetal membranes US Medical PG Question 4: A researcher is studying the interactions between foreign antigens and human immune cells. She has isolated a line of lymphocytes that is known to bind antigen-presenting cells. From this cell line, she has isolated a cell surface protein that binds to class I major histocompatibility complex molecules. The continued activation, proliferation and survival of this specific cell line requires which of the following signaling molecules?
- A. Interleukin 1
- B. Interleukin 4
- C. Interleukin 2 (Correct Answer)
- D. Interleukin 8
- E. Interleukin 6
Placenta and fetal membranes Explanation: ***Interleukin 2***
- The description of the lymphocyte binding the **constant portion of MHC class I** and requiring a signaling molecule for activation, proliferation, and survival points to a **T cell**.
- **Interleukin-2 (IL-2)** is a crucial cytokine for the proliferation, differentiation, and survival of T lymphocytes, acting in an autocrine or paracrine fashion after T cell activation.
*Interleukin 1*
- **Interleukin-1 (IL-1)** is primarily involved in inflammation and fever, produced by macrophages and other innate immune cells.
- While it can act as a costimulator for T cells, it is not the primary cytokine required for their sustained proliferation and survival after initial activation.
*Interleukin 4*
- **Interleukin-4 (IL-4)** is a key cytokine in humoral immunity, promoting B cell proliferation and differentiation, and inducing IgE class switching.
- It also plays a role in the differentiation of naive T cells into **Th2 cells**, but it is not the main cytokine for general T cell proliferation and survival.
*Interleukin 8*
- **Interleukin-8 (IL-8)**, also known as CXCL8, is a chemokine primarily responsible for attracting and activating neutrophils to sites of infection or inflammation.
- It does not have a direct role in the sustained proliferation and survival of activated lymphocytes.
*Interleukin 6*
- **Interleukin-6 (IL-6)** is a pleiotropic cytokine involved in acute phase reactions, hematopoiesis, and the immune response, particularly B cell differentiation and antibody production.
- Although it can influence T cell responses, it is not the primary growth factor for activated T lymphocytes as IL-2 is.
Placenta and fetal membranes US Medical PG Question 5: A 39-year-old woman, gravida 3, para 2, at 32 weeks' gestation comes to the emergency department 1 hour after the sudden onset of severe abdominal pain and nausea. She has had one episode of nonbloody vomiting. Pregnancy has been uncomplicated, except for a blood pressure measurement of 150/90 mm Hg on her last prenatal visit. Her first child was delivered vaginally; her second child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. She appears anxious and pale. Her temperature is 36.1°C (96°F), pulse is 115/min, and blood pressure is 92/65 mm Hg. Extremities are cool and clammy. Pelvic examination shows a rigid, tender uterus. The cervix is 30% effaced and 1 cm dilated; the vertex is at -1 station. The fetal heart rate is 100/min. Which of the following is the most likely diagnosis?
- A. Ruptured vasa previa
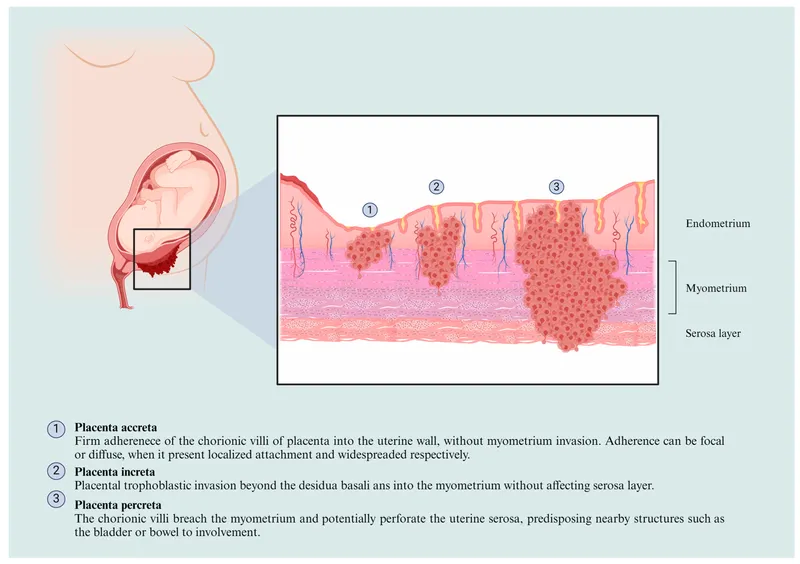
- B. Placenta accreta
- C. Abruptio placentae (Correct Answer)
- D. Ruptured uterus
- E. Placenta previa
Placenta and fetal membranes Explanation: ***Abruptio placentae***
- The sudden onset of **severe abdominal pain**, **uterine rigidity and tenderness**, maternal hypovolemic shock (tachycardia, hypotension, cool and clammy extremities), and **fetal bradycardia** are classic signs of **abruptio placentae**.
- **Hypertension** (150/90 mm Hg) is a risk factor, and a prior **cesarean section** may slightly increase the risk as well, although the primary risk factor here is hypertension.
*Ruptured vasa previa*
- **Vasa previa** typically presents with **painless vaginal bleeding** when membranes rupture, accompanied by rapid fetal deterioration due to fetal blood loss, and would not cause severe maternal abdominal pain and shock.
- The bleeding in vasa previa originates from fetal vessels, leading to a profound impact on fetal heart rate *before* significant maternal symptoms.
*Placenta accreta*
- **Placenta accreta** is typically diagnosed prenatally via ultrasound or suspected at delivery due to difficulty with placental separation. It does not usually present with acute, severe abdominal pain and hypovolemic shock during pregnancy.
- Patients with placenta accreta are at high risk for significant hemorrhage *after* delivery of the fetus, but before placental delivery.
*Ruptured uterus*
- While a prior **cesarean section** is a risk factor for uterine rupture, the presentation of **rigid and tender uterus** is more characteristic of abruptio placentae. Uterine rupture often involves a **sudden cessation of contractions**, palpable fetal parts outside the uterus, and often severe, sharp pain, but not typically a rigid uterus.
- The fetal heart rate in uterine rupture often shows a **sudden, profound deceleration** or absence, but the specific finding of a rigid, tender uterus with ongoing severe pain points away from frank rupture.
*Placenta previa*
- **Placenta previa** typically presents with **painless vaginal bleeding** in the second or third trimester.
- It does not usually cause severe abdominal pain, uterine tenderness, or maternal hypovolemic shock unless accompanied by abruptio placentae, which is the more dominant and acute finding here.
Placenta and fetal membranes US Medical PG Question 6: A 36-year-old woman, gravida 2, para 1, at 30 weeks' gestation comes to the physician for evaluation of increased urinary frequency. She has no history of major medical illness. Physical examination shows no abnormalities. Laboratory studies show an increased serum C-peptide concentration. Ultrasonography shows polyhydramnios and a large for gestational age fetus. Which of the following hormones is predominantly responsible for the observed laboratory changes in this patient?
- A. Human placental lactogen (Correct Answer)
- B. Adrenocorticotropic hormone
- C. Human chorionic gonadotropin
- D. Progesterone
- E. Estrogen
Placenta and fetal membranes Explanation: ***Human placental lactogen***
- **Human placental lactogen (hPL)**, also known as **chorionic somatomammotropin**, is produced by the placenta and has **anti-insulin effects**, increasing maternal blood glucose to prioritize fetal nutrient supply.
- This **insulin resistance** leads to increased maternal insulin production (reflected by **elevated C-peptide**) to compensate, and if inadequate, results in **gestational diabetes mellitus (GDM)**, which explains the **polyhydramnios** and **large for gestational age fetus**.
*Adrenocorticotropic hormone*
- **ACTH** stimulates the **adrenal cortex** to produce **cortisol**, which also has diabetogenic effects.
- However, **hPL** is the primary hormone responsible for the **insulin resistance** of pregnancy and the associated elevated C-peptide and GDM features (polyhydramnios and large for gestational age fetus) in this context.
*Human chorionic gonadotropin*
- **hCG** is crucial for maintaining the **corpus luteum** in early pregnancy, stimulating **progesterone** production, and is used as a marker for pregnancy.
- It does not directly cause the **insulin resistance** or significantly elevate C-peptide that leads to the observed findings of **polyhydramnios** and a **large for gestational age fetus**.
*Progesterone*
- **Progesterone** is essential for maintaining pregnancy by promoting **endometrial growth** and suppressing uterine contractions.
- While it plays a role in some metabolic changes during pregnancy, it is not the primary hormone responsible for the **insulin-antagonistic effects** that lead to the elevated C-peptide and signs of GDM described.
*Estrogen*
- **Estrogen** promotes uterine growth, maintains the **endometrium**, and plays a role in fetal development and the development of maternal secondary sexual characteristics.
- While it contributes to metabolic changes in pregnancy, it is not the main hormone responsible for the **insulin resistance** and related features like elevated C-peptide, polyhydramnios, and a large for gestational age fetus seen in this patient.
Placenta and fetal membranes US Medical PG Question 7: A 34-year-old G3P2 presents at 33 weeks gestation with several episodes of bloody spotting and mild vaginal bleeding over the past 2 weeks. The bleeding has no specific triggers and resolves spontaneously. She does not report abdominal pain or uterine contractions. She has had two cesarean deliveries. At 20 weeks gestation, the ultrasound examination showed the placental edge to be 5 cm away from the internal cervical os. On examination at this visit, the vital signs are as follows: blood pressure, 110/70 mm Hg; heart rate, 89/min; respiratory rate, 15/min; and temperature, 36.6℃ (97.9℉). The uterus is tender with no palpable contractions and streaks of blood are noted on the perineum, but there is no active bleeding. An ultrasound evaluation shows the placental edge 1 cm from the internal cervical os. Which of the following options best describes the placental position at each ultrasound?
- A. Low-lying placenta → partial previa
- B. Normally placed placenta → low-lying placenta
- C. Normally lying placenta → marginal previa (Correct Answer)
- D. Marginal previa → partial previa
- E. Low-lying placenta → marginal previa
Placenta and fetal membranes Explanation: ***Normally lying placenta → marginal previa***
- At 20 weeks, the placental edge was 5 cm from the internal cervical os, categorizing it as a **normally placed placenta** (greater than 2 cm from the os).
- At 33 weeks, the placental edge is 1 cm from the internal cervical os, which is consistent with a **marginal previa** (within 2 cm of the os but not covering it).
*Low-lying placenta → partial previa*
- A **low-lying placenta** is defined as one whose edge is within 2 cm of the internal cervical os but not covering it. At 20 weeks, the placenta was 5 cm away, so it was not low-lying.
- A **partial previa** implies the placenta partially covers the internal os, which is not indicated by the 1 cm distance from the os at 33 weeks.
*Normally placed placenta → low-lying placenta*
- The initial ultrasound at 20 weeks showed the placenta 5 cm away, which is indeed a **normally placed placenta**.
- However, at 33 weeks, the placental edge 1 cm from the os is more specifically defined as a **marginal previa**, not just a low-lying placenta.
*Marginal previa → partial previa*
- A **marginal previa** is defined as the placental edge being within 2 cm of the internal os but not covering it. At 20 weeks, the placenta was 5 cm away, so it was not a marginal previa.
- A **partial previa** means the placenta partially covers the os, which is not consistent with an edge 1 cm away.
*Low-lying placenta → marginal previa*
- The placenta was 5 cm away from the os at 20 weeks, which is a **normally placed placenta**, not a low-lying placenta.
- The 1 cm distance at 33 weeks is consistent with a **marginal previa**.
Placenta and fetal membranes US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Placenta and fetal membranes Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Placenta and fetal membranes US Medical PG Question 9: Research is being conducted on embryoblasts. The exact date of fertilization is unknown. There is the presence of a cytotrophoblast and syncytiotrophoblast, marking the time when implantation into the uterus would normally occur. Within the embryoblast, columnar and cuboidal cells are separated by a membrane. Which of these cell layers begins to line the yolk sac cavity?
- A. Hypoblast (Correct Answer)
- B. Epiblast
- C. Syncytiotrophoblast
- D. Inner cell mass
- E. Endoderm
Placenta and fetal membranes Explanation: ***Hypoblast***
- The **hypoblast** is a layer of cuboidal cells that forms from the inner cell mass around day 8 post-fertilization.
- It plays a crucial role in forming the **primary yolk sac** by migrating to line the exocoelomic cavity.
*Epiblast*
- The **epiblast** is composed of columnar cells located dorsal to the hypoblast and forms the floor of the **amniotic cavity**.
- It is the source of the **three primary germ layers** during gastrulation (ectoderm, mesoderm, and endoderm), not the yolk sac lining itself.
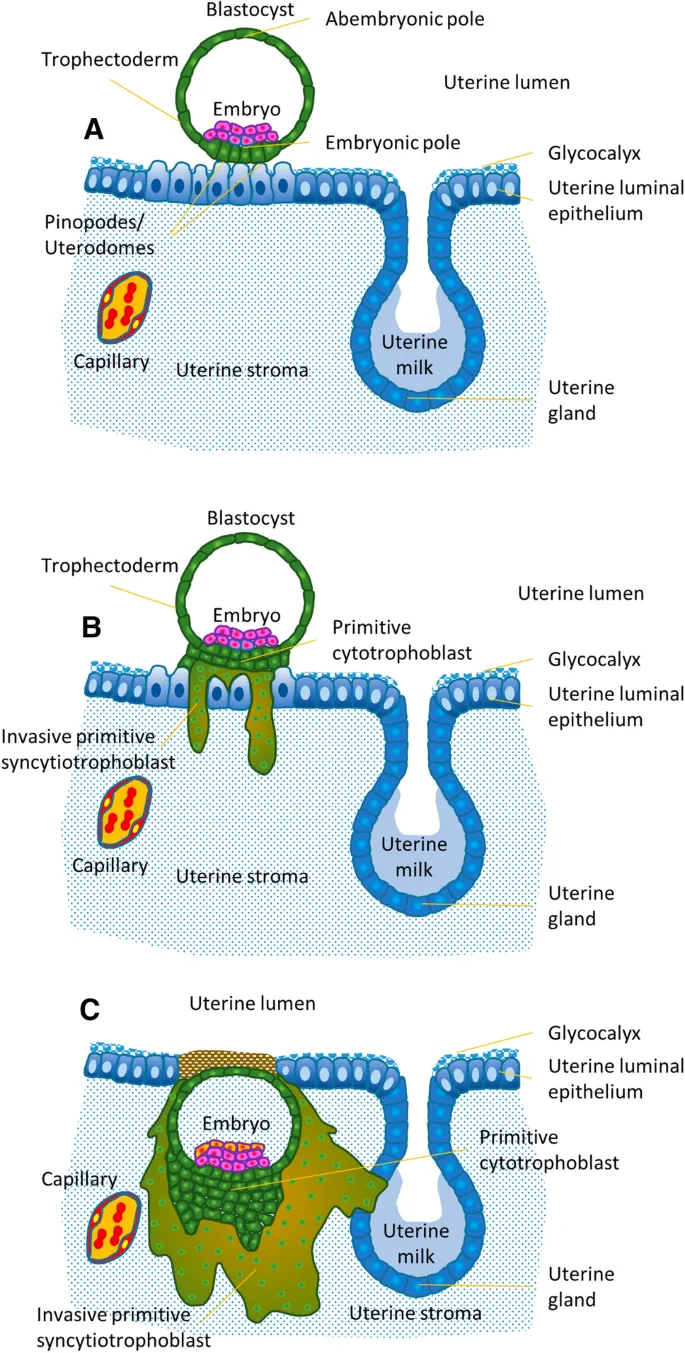
*Syncytiotrophoblast*
- The **syncytiotrophoblast** is the outer, invasive layer of the trophoblast that facilitates implantation and forms the fetal component of the placenta.
- It is not involved in lining the yolk sac cavity but rather in **invading the uterine endometrium** and producing hCG.
*Inner cell mass*
- The **inner cell mass (ICM)** is the cluster of cells within the blastocyst that gives rise to the embryoblast (which further differentiates into epiblast and hypoblast).
- The ICM itself does not line the yolk sac; rather, its derivative, the hypoblast, does.
*Endoderm*
- The **endoderm** is one of the three primary germ layers that forms during gastrulation from the epiblast derivative.
- It ultimately forms the linings of the **gastrointestinal and respiratory tracts**, not the primary yolk sac lining.
Placenta and fetal membranes US Medical PG Question 10: An 11-year-old girl is brought to the office by her mother due to complaint of intermittent and severe periumbilical pain for 1 day. She does not have any significant past medical history. She provides a history of a recent school trip to the suburbs. On physical examination, there is a mild tenderness around the umbilicus without any distension or discharge. There is no rebound tenderness. Bowel sounds are normal. An abdominal imaging shows enlarged mesenteric lymph nodes, and she is diagnosed with mesenteric lymphadenitis. However, incidentally, a mass of tissue was seen joining the inferior pole of both kidneys as shown in the image. Which of the following best describes this renal anomaly?
- A. Fused kidneys ascend beyond superior mesenteric artery.
- B. Rapid progression to acute renal failure
- C. Kidneys are usually non-functional.
- D. Increased risk of developing renal vein thrombosis
- E. Association with ureteropelvic junction obstruction (UPJO) (Correct Answer)
Placenta and fetal membranes Explanation: ***Association with ureteropelvic junction obstruction (UPJO)***
- **Horseshoe kidney** is characterized by the fusion of the lower poles (most common) or upper poles of the kidneys, forming a U-shape. This anomaly is associated with an increased incidence of **ureteropelvic junction obstruction (UPJO)** due to the abnormal course of the ureters over the isthmus.
- The abnormal ascent of the fused kidneys can also lead to an increased incidence of other anomalies such as **vesicoureteral reflux**, **renal calculi**, and recurrent urinary tract infections.
*Fused kidneys ascend beyond superior mesenteric artery.*
- The **horseshoe kidney** typically **fails to ascend** completely during development because its isthmus (the fused part) can get trapped under the **inferior mesenteric artery**.
- Therefore, fused kidneys in horseshoe kidney are often found in a **lower position** than normal, not ascended beyond the superior mesenteric artery.
*Rapid progression to acute renal failure*
- While horseshoe kidney can be associated with an increased risk of complications (like UPJO, stones, infections), it does not inherently lead to **rapid progression to acute renal failure**.
- Many individuals with a horseshoe kidney have **normal renal function** without significant clinical manifestations.
*Kidneys are usually non-functional.*
- The presence of a horseshoe kidney **does not typically mean the kidneys are non-functional**.
- In most cases, both renal units of a horseshoe kidney are **functional**, although they may be at increased risk for complications that could impact function over time.
*Increased risk of developing renal vein thrombosis*
- There is **no established increased risk** of developing **renal vein thrombosis** specifically associated with horseshoe kidney.
- The primary vascular anomalies associated with horseshoe kidney relate to the arterial supply and variations in the number and origin of renal arteries, not typically venous thrombosis.
More Placenta and fetal membranes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.