Implantation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Implantation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
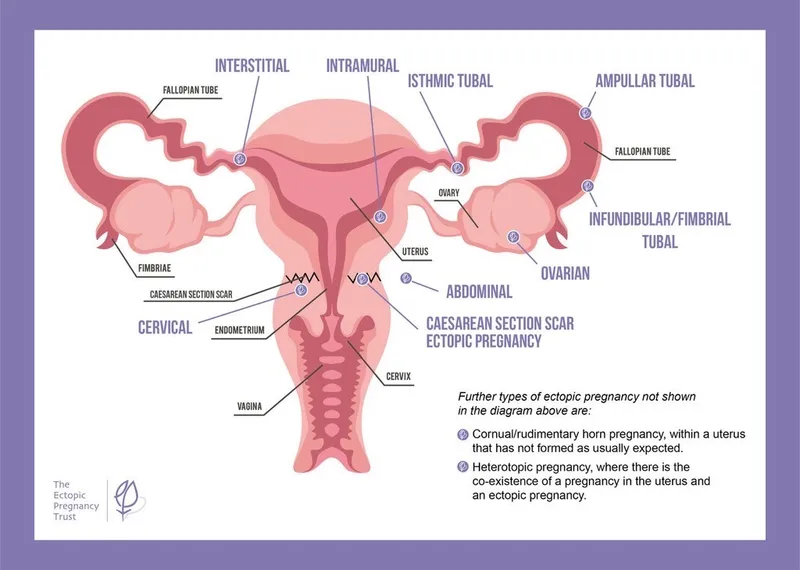
Implantation US Medical PG Question 1: A 25-year-old woman is brought to the emergency department by her roommate with severe right lower quadrant pain for the last 8 hours. The pain is progressively getting worse and is associated with vomiting. When you ask the patient about her last menstrual period, she tells you that although she stopped keeping track of her cycle after undergoing surgical sterilization 1 year ago, she recalls bleeding yesterday. The physical examination reveals a hemodynamically stable patient with a pulse of 90/min, respiratory rate of 14/min, blood pressure of 125/70 mm Hg, and temperature of 37.0°C (98.6°F). The abdomen is tender to touch (more tender in the lower quadrants), and tenderness at McBurney's point is absent. Which of the following is the best next step in the management of this patient?
- A. Complete blood count
- B. Urinalysis
- C. FAST ultrasound scan
- D. Appendectomy
- E. Urinary human chorionic gonadotropin (hCG) (Correct Answer)
Implantation Explanation: ***Urinary human chorionic gonadotropin (hCG)***
- Despite surgical sterilization, a **low risk of ectopic pregnancy** still exists, especially with symptoms like **severe right lower quadrant pain** and **vomiting**.
- A positive urinary hCG would necessitate further evaluation for an **ectopic pregnancy**, which is a **life-threatening condition**.
*Complete blood count*
- While a CBC assesses for **leukocytosis** (suggesting infection/inflammation) or **anemia** (suggesting blood loss), it's not the immediate priority given the potential for ectopic pregnancy symptoms.
- A CBC alone would not rule out the most critical diagnosis in this scenario.
*Urinalysis*
- A urinalysis helps rule out **urinary tract infection (UTI)** or **nephrolithiasis** (kidney stones).
- While important for differential diagnosis, the severity of pain and reproductive history make ectopic pregnancy a more immediate concern.
*FAST ultrasound scan*
- An ultrasound is useful for identifying **free fluid** in the abdomen or assessing the **uterus and adnexa** for an ectopic pregnancy.
- However, in a female of reproductive age, a **positive hCG** is generally a prerequisite for a targeted pelvic ultrasound to confirm or exclude an early ectopic pregnancy.
*Appendectomy*
- While **appendicitis** is in the differential for right lower quadrant pain, the absence of **McBurney's point tenderness** and the patient's reproductive history make other diagnoses more likely first.
- Surgery should only be considered after a thorough diagnostic workup, especially to rule out time-sensitive conditions like ectopic pregnancy.
Implantation US Medical PG Question 2: A researcher is studying physiologic and hormonal changes that occur during pregnancy. Specifically, they examine the behavior of progesterone over the course of the menstrual cycle and find that it normally decreases over time; however, during pregnancy this decrease does not occur in the usual time frame. The researcher identifies a circulating factor that appears to be responsible for this difference in progesterone behavior. In order to further examine this factor, the researcher denatures the circulating factor and examines the sizes of its components on a western blot as compared to several other hormones. One of the bands the researcher identifies in this circulating factor is identical to that of another known hormone with which of the following sites of action?
- A. Thyroid gland (Correct Answer)
- B. Adrenal gland
- C. Adipocytes
- D. Bones
- E. Kidney tubules
Implantation Explanation: ***Correct: Thyroid gland***
- The circulating factor described is **human chorionic gonadotropin (hCG)**, which maintains the corpus luteum and progesterone production during early pregnancy
- hCG is a **glycoprotein hormone** composed of an **α subunit** and a **β subunit**
- The **α subunit of hCG is identical** to the α subunits of **TSH (thyroid-stimulating hormone)**, **LH (luteinizing hormone)**, and **FSH (follicle-stimulating hormone)**
- When denatured and examined on Western blot, one of the bands (the α subunit) would be identical to that of **TSH**
- **TSH acts on the thyroid gland** to stimulate thyroid hormone synthesis and release
- This structural similarity explains why very high levels of hCG (as in molar pregnancy or hyperemesis gravidarum) can sometimes cause **thyrotoxicosis** due to cross-reactivity with TSH receptors
*Incorrect: Adrenal gland*
- **ACTH (adrenocorticotropic hormone)** acts on the adrenal cortex to stimulate cortisol production
- ACTH is a **peptide hormone** derived from POMC (pro-opiomelanocortin) and does **NOT share any structural components** with hCG
- There is no identical band between hCG and ACTH on Western blot
*Incorrect: Adipocytes*
- Adipocytes are regulated by hormones like **insulin** and **leptin**
- Neither of these hormones share structural components with hCG
*Incorrect: Bones*
- Bones are primarily regulated by **PTH (parathyroid hormone)**, **calcitonin**, and **vitamin D**
- None of these hormones share structural components with hCG
*Incorrect: Kidney tubules*
- Kidney tubules are regulated by **ADH (antidiuretic hormone/vasopressin)** and **aldosterone**
- Neither shares structural components with hCG
Implantation US Medical PG Question 3: A 39-year-old woman, gravida 3, para 2, at 32 weeks' gestation comes to the emergency department 1 hour after the sudden onset of severe abdominal pain and nausea. She has had one episode of nonbloody vomiting. Pregnancy has been uncomplicated, except for a blood pressure measurement of 150/90 mm Hg on her last prenatal visit. Her first child was delivered vaginally; her second child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. She appears anxious and pale. Her temperature is 36.1°C (96°F), pulse is 115/min, and blood pressure is 92/65 mm Hg. Extremities are cool and clammy. Pelvic examination shows a rigid, tender uterus. The cervix is 30% effaced and 1 cm dilated; the vertex is at -1 station. The fetal heart rate is 100/min. Which of the following is the most likely diagnosis?
- A. Ruptured vasa previa
- B. Placenta accreta
- C. Abruptio placentae (Correct Answer)
- D. Ruptured uterus
- E. Placenta previa
Implantation Explanation: ***Abruptio placentae***
- The sudden onset of **severe abdominal pain**, **uterine rigidity and tenderness**, maternal hypovolemic shock (tachycardia, hypotension, cool and clammy extremities), and **fetal bradycardia** are classic signs of **abruptio placentae**.
- **Hypertension** (150/90 mm Hg) is a risk factor, and a prior **cesarean section** may slightly increase the risk as well, although the primary risk factor here is hypertension.
*Ruptured vasa previa*
- **Vasa previa** typically presents with **painless vaginal bleeding** when membranes rupture, accompanied by rapid fetal deterioration due to fetal blood loss, and would not cause severe maternal abdominal pain and shock.
- The bleeding in vasa previa originates from fetal vessels, leading to a profound impact on fetal heart rate *before* significant maternal symptoms.
*Placenta accreta*
- **Placenta accreta** is typically diagnosed prenatally via ultrasound or suspected at delivery due to difficulty with placental separation. It does not usually present with acute, severe abdominal pain and hypovolemic shock during pregnancy.
- Patients with placenta accreta are at high risk for significant hemorrhage *after* delivery of the fetus, but before placental delivery.
*Ruptured uterus*
- While a prior **cesarean section** is a risk factor for uterine rupture, the presentation of **rigid and tender uterus** is more characteristic of abruptio placentae. Uterine rupture often involves a **sudden cessation of contractions**, palpable fetal parts outside the uterus, and often severe, sharp pain, but not typically a rigid uterus.
- The fetal heart rate in uterine rupture often shows a **sudden, profound deceleration** or absence, but the specific finding of a rigid, tender uterus with ongoing severe pain points away from frank rupture.
*Placenta previa*
- **Placenta previa** typically presents with **painless vaginal bleeding** in the second or third trimester.
- It does not usually cause severe abdominal pain, uterine tenderness, or maternal hypovolemic shock unless accompanied by abruptio placentae, which is the more dominant and acute finding here.
Implantation US Medical PG Question 4: A 28-year-old woman and her husband are admitted to the office due to difficulties conceiving a child for the past year. Her menarche was at the age of 15 years, and her periods have been regular since then. Her medical history is positive for an abortion with curettage 5 years ago. A spermogram on the partner is performed, and it shows motile sperm cells. An ultrasound is performed on the patient and it is unremarkable. The laboratory results show that the FSH, LH, TSH, and prolactin levels are within normal ranges. A hysteroscopy is additionally performed and multiple adhesions are found in the uterus (refer to the image). Which of the following is the most likely composition of the scar tissue present in the uterus?
- A. Type 3 collagen
- B. Type 4 collagen
- C. Type 2 collagen
- D. Type 1 collagen (Correct Answer)
- E. Elastin
Implantation Explanation: ***Type 1 collagen***
- This patient presents with **Asherman's syndrome**, characterized by intrauterine adhesions, often following uterine surgery like **curettage**. These adhesions are primarily composed of **Type 1 collagen**, which is the most abundant type of collagen in the human body and a major component of scar tissue.
- **Type 1 collagen** provides tensile strength and is crucial for wound healing and forming scar tissue in most connective tissues, including the uterus.
*Type 3 collagen*
- **Type 3 collagen** is found in distensible tissues like blood vessels, the uterus, and skin, and is important during the **early stages of wound healing**.
- While present in the uterus and initially involved in wound repair, **mature scar tissue** predominantly consists of **Type 1 collagen**.
*Type 4 collagen*
- **Type 4 collagen** is a major component of the **basal lamina**, a specialized extracellular matrix that underlies epithelial and endothelial cells.
- It does not form fibrillar structures and is not the primary component of robust scar tissue found in Asherman's syndrome.
*Type 2 collagen*
- **Type 2 collagen** is the main collagen type found in **hyaline cartilage** and elastic cartilage, providing resistance to pressure.
- It is not found in significant amounts in uterine tissue or scar tissue formed within the uterus.
*Elastin*
- **Elastin** is a protein that provides **elasticity** to tissues like blood vessels, skin, and lungs, allowing them to stretch and recoil.
- While present in the uterus for its contractile properties, it is not the primary constituent of **fibrotic scar tissue** forming adhesions.
Implantation US Medical PG Question 5: A 36-year-old woman, gravida 2, para 1, at 30 weeks' gestation comes to the physician for evaluation of increased urinary frequency. She has no history of major medical illness. Physical examination shows no abnormalities. Laboratory studies show an increased serum C-peptide concentration. Ultrasonography shows polyhydramnios and a large for gestational age fetus. Which of the following hormones is predominantly responsible for the observed laboratory changes in this patient?
- A. Human placental lactogen (Correct Answer)
- B. Adrenocorticotropic hormone
- C. Human chorionic gonadotropin
- D. Progesterone
- E. Estrogen
Implantation Explanation: ***Human placental lactogen***
- **Human placental lactogen (hPL)**, also known as **chorionic somatomammotropin**, is produced by the placenta and has **anti-insulin effects**, increasing maternal blood glucose to prioritize fetal nutrient supply.
- This **insulin resistance** leads to increased maternal insulin production (reflected by **elevated C-peptide**) to compensate, and if inadequate, results in **gestational diabetes mellitus (GDM)**, which explains the **polyhydramnios** and **large for gestational age fetus**.
*Adrenocorticotropic hormone*
- **ACTH** stimulates the **adrenal cortex** to produce **cortisol**, which also has diabetogenic effects.
- However, **hPL** is the primary hormone responsible for the **insulin resistance** of pregnancy and the associated elevated C-peptide and GDM features (polyhydramnios and large for gestational age fetus) in this context.
*Human chorionic gonadotropin*
- **hCG** is crucial for maintaining the **corpus luteum** in early pregnancy, stimulating **progesterone** production, and is used as a marker for pregnancy.
- It does not directly cause the **insulin resistance** or significantly elevate C-peptide that leads to the observed findings of **polyhydramnios** and a **large for gestational age fetus**.
*Progesterone*
- **Progesterone** is essential for maintaining pregnancy by promoting **endometrial growth** and suppressing uterine contractions.
- While it plays a role in some metabolic changes during pregnancy, it is not the primary hormone responsible for the **insulin-antagonistic effects** that lead to the elevated C-peptide and signs of GDM described.
*Estrogen*
- **Estrogen** promotes uterine growth, maintains the **endometrium**, and plays a role in fetal development and the development of maternal secondary sexual characteristics.
- While it contributes to metabolic changes in pregnancy, it is not the main hormone responsible for the **insulin resistance** and related features like elevated C-peptide, polyhydramnios, and a large for gestational age fetus seen in this patient.
Implantation US Medical PG Question 6: A 34-year-old G3P2 presents at 33 weeks gestation with vaginal bleeding that started last night while she was asleep. She denies uterine contractions or abdominal pain. She had a cesarean delivery in her previous pregnancy. She also reports a 10 pack-year smoking history. The vital signs are as follows: blood pressure, 130/80 mm Hg; heart rate, 84/min; respiratory rate, 12/min; and temperature, 36.8℃ (98.2℉). The physical examination is negative for abdominal tenderness or palpable uterine contractions. The perineum is mildly bloody. On speculum examination, no vaginal or cervical lesions are seen. A small amount of blood continues to pass through the cervix. Which of the following findings would you expect on ultrasound examination?
- A. Partial covering of the internal cervical os by the placental edge (Correct Answer)
- B. Cysts on the placental surface
- C. Retroplacental blood accumulation
- D. Placental calcification
- E. Loss of the clear retroplacental space
Implantation Explanation: ***Partial covering of the internal cervical os by the placental edge***
- This presentation, with painless vaginal bleeding in the third trimester in a patient with a **history of prior C-section** (a major risk factor) and **smoking history**, is highly suggestive of **placenta previa**.
- **Placenta previa** is diagnosed when the placenta implants either completely or partially over the **internal cervical os**, which an ultrasound would confirm.
*Cysts on the placental surface*
- **Placental cysts** are usually benign findings and are not typically associated with active painless vaginal bleeding in the third trimester.
- They tend to be **asymptomatic** and are rarely the cause of significant obstetric complications.
*Retroplacental blood accumulation*
- **Retroplacental blood accumulation** is characteristic of **placental abruption**, which typically presents with painful vaginal bleeding, uterine tenderness, and contractions, none of which are present here.
*Placental calcification*
- **Placental calcification** is a common, normal finding as pregnancy progresses and the placenta matures; it is not a cause of third-trimester vaginal bleeding.
- It indicates **placental aging** and is generally not associated with adverse outcomes unless severe and accompanied by other issues.
*Loss of the clear retroplacental space*
- **Loss of the clear retroplacental space** is an ultrasound sign indicative of **placenta accreta spectrum**, where the placenta abnormally adheres to the uterine wall.
- While a prior C-section is a risk factor for accreta, the primary presenting symptom leading to diagnosis is usually **hemorrhage during placental delivery**, not painless third-trimester bleeding, and it would need further specific imaging features to confirm.
Implantation US Medical PG Question 7: A 23-year-old woman comes to the emergency department because of a 5-day history of nausea and vomiting. There is no associated fever, abdominal pain, constipation, diarrhea, or dysuria. She is sexually active and uses condoms inconsistently. Her last menstrual period was 10 weeks ago. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 18/min, and blood pressure is 110/70 mm Hg. There is no rebound tenderness or guarding. A urine pregnancy test is positive. Ultrasonography shows an intrauterine pregnancy consistent in size with an 8-week gestation. The hormone that was measured in this patient's urine to detect the pregnancy is also directly responsible for which of the following processes?
- A. Hypertrophy of the uterine myometrium
- B. Fetal angiogenesis
- C. Maintenance of the corpus luteum (Correct Answer)
- D. Inhibition of ovulation
- E. Stimulation of uterine contractions at term
Implantation Explanation: ***Maintenance of the corpus luteum***
- The hormone measured in the urine pregnancy test is **human chorionic gonadotropin (hCG)**. hCG's primary role early in pregnancy is to **maintain the corpus luteum**, which in turn produces progesterone to support the uterine lining.
- The **corpus luteum** is essential for progesterone production until the placenta is sufficiently developed to take over this function, typically around 8-10 weeks gestation.
*Hypertrophy of the uterine myometrium*
- **Estrogen** and **progesterone** are primarily responsible for the hypertrophy and hyperplasia of the uterine myometrium during pregnancy.
- While hCG indirectly supports this by maintaining the corpus luteum (which produces estrogen and progesterone), it does not directly cause myometrial hypertrophy itself.
*Fetal angiogenesis*
- **Vascular endothelial growth factor (VEGF)** and **fibroblast growth factor (FGF)** are key factors directly involved in fetal angiogenesis (the formation of new blood vessels in the fetus).
- While proper placental function, supported by hCG, is critical for fetal growth, hCG itself is not the direct mediator of fetal angiogenesis.
*Inhibition of ovulation*
- High levels of **estrogen** and **progesterone** (produced by the corpus luteum, maintained by hCG) provide **negative feedback** to the hypothalamus and pituitary, thus inhibiting the release of GnRH, FSH, and LH, which prevents further ovulation.
- hCG itself does not directly inhibit ovulation; rather, it sets in motion the hormonal cascade that leads to its inhibition.
*Stimulation of uterine contractions at term*
- **Oxytocin** is the primary hormone responsible for stimulating uterine contractions, particularly at term, often in conjunction with prostaglandins.
- hCG levels peak early in pregnancy and then decline, and it plays no direct role in stimulating labor contractions.
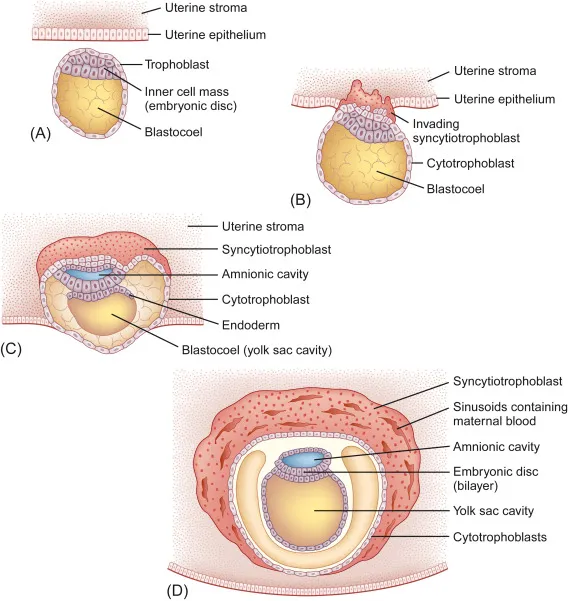
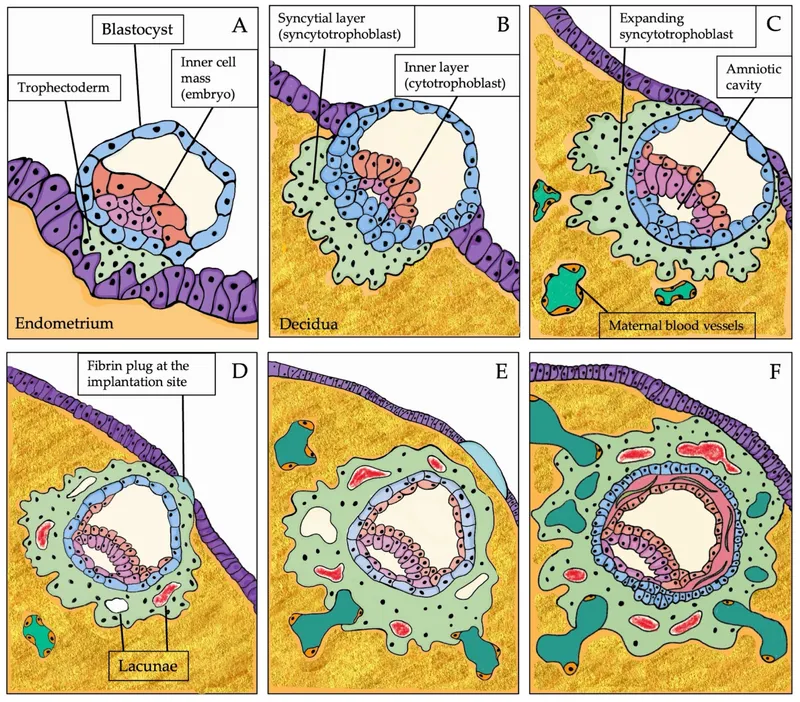
Implantation US Medical PG Question 8: Research is being conducted on embryoblasts. The exact date of fertilization is unknown. There is the presence of a cytotrophoblast and syncytiotrophoblast, marking the time when implantation into the uterus would normally occur. Within the embryoblast, columnar and cuboidal cells are separated by a membrane. Which of these cell layers begins to line the yolk sac cavity?
- A. Hypoblast (Correct Answer)
- B. Epiblast
- C. Syncytiotrophoblast
- D. Inner cell mass
- E. Endoderm
Implantation Explanation: ***Hypoblast***
- The **hypoblast** is a layer of cuboidal cells that forms from the inner cell mass around day 8 post-fertilization.
- It plays a crucial role in forming the **primary yolk sac** by migrating to line the exocoelomic cavity.
*Epiblast*
- The **epiblast** is composed of columnar cells located dorsal to the hypoblast and forms the floor of the **amniotic cavity**.
- It is the source of the **three primary germ layers** during gastrulation (ectoderm, mesoderm, and endoderm), not the yolk sac lining itself.
*Syncytiotrophoblast*
- The **syncytiotrophoblast** is the outer, invasive layer of the trophoblast that facilitates implantation and forms the fetal component of the placenta.
- It is not involved in lining the yolk sac cavity but rather in **invading the uterine endometrium** and producing hCG.
*Inner cell mass*
- The **inner cell mass (ICM)** is the cluster of cells within the blastocyst that gives rise to the embryoblast (which further differentiates into epiblast and hypoblast).
- The ICM itself does not line the yolk sac; rather, its derivative, the hypoblast, does.
*Endoderm*
- The **endoderm** is one of the three primary germ layers that forms during gastrulation from the epiblast derivative.
- It ultimately forms the linings of the **gastrointestinal and respiratory tracts**, not the primary yolk sac lining.
Implantation US Medical PG Question 9: A 26-year-old woman comes to the physician because she has not had a menstrual period for 5 weeks. Menarche was at the age of 14 years and menses occurred at regular 30-day intervals. She reports having unprotected sexual intercourse 3 weeks ago. A urine pregnancy test is positive. Which of the following best describes the stage of development of the embryo at this time?
- A. Fetal heart is beating, but cardiac activity is not yet visible on ultrasound
- B. Limb buds have formed, but fetal movements have not begun
- C. Sexual differentiation has begun, but fetal movement has not started
- D. Neural crest has formed, but limb buds have not yet formed (Correct Answer)
- E. Implantation has occurred, but notochord has not yet formed
Implantation Explanation: ***Neural crest has formed, but limb buds have not yet formed***
- At **5 weeks gestational age (3 weeks post-fertilization)**, neurulation is completing or recently completed
- **Neural crest cells** migrate from the neural folds during weeks 3-4 post-fertilization and are definitely present by this time
- **Limb buds** appear later, around week 4-5 post-fertilization (week 6-7 gestational age), making this the most accurate description for the current developmental stage
*Fetal heart is beating, but cardiac activity is not yet visible on ultrasound*
- The primitive heart tube begins contracting around day 22-23 post-fertilization (early week 4)
- At 3 weeks post-fertilization (5 weeks gestational age), the heart may just be starting to beat, but this timing is less precise
- Cardiac activity becomes visible on transvaginal ultrasound around 5.5-6 weeks gestational age, so this option is close but less precise than the correct answer
*Limb buds have formed, but fetal movements have not begun*
- **Limb buds** typically appear around week 4-5 post-fertilization (week 6-7 gestational age)
- This is **too advanced** for 3 weeks post-fertilization
- While fetal movements aren't perceptible to the mother until 16-20 weeks, they begin much later than the current stage
*Sexual differentiation has begun, but fetal movement has not started*
- **Sexual differentiation** of the gonads begins around week 7 post-fertilization (week 9 gestational age)
- External genitalia differentiation occurs even later (weeks 9-12 post-fertilization)
- This stage is **far too advanced** for the current 3-week post-fertilization timeframe
*Implantation has occurred, but notochord has not yet formed*
- **Implantation** occurs 6-12 days after fertilization, which is approximately 2-3 weeks before a positive pregnancy test
- The **notochord** forms during gastrulation in the **3rd week post-fertilization** (5th week gestational age)
- By the time of this positive pregnancy test (5 weeks gestational age), the notochord has **already formed**, making this statement incorrect
Implantation US Medical PG Question 10: What is the pattern of inheritance in neural tube defects?
- A. Multifactorial inheritance (Correct Answer)
- B. Autosomal recessive
- C. X-linked dominant
- D. Autosomal dominant
- E. X-linked recessive
Implantation Explanation: ***Multifactorial inheritance***
- Neural tube defects (NTDs) are a classic example of **multifactorial inheritance**, meaning they result from a combination of **genetic predispositions** and **environmental factors**.
- Risk is influenced by multiple genes, and environmental factors like **folate deficiency** play a significant role.
*Autosomal recessive*
- This pattern involves two copies of an altered gene to cause disease, typically resulting in a **25% recurrence risk** for siblings.
- While some rare isolated NTDs might have an autosomal recessive component, the general presentation of NTDs does not fit this classic mendelian pattern.
*X-linked dominant*
- Involves genes on the **X chromosome** where one altered copy is sufficient to cause disease; affected fathers pass it to all daughters, but no sons.
- This inheritance pattern is very rare for NTDs and would present with a distinct sex-linked pattern of affected individuals.
*Autosomal dominant*
- Requires only one copy of an altered gene to cause disease, leading to a **50% recurrence risk** for offspring.
- While some syndromes associated with NTDs can be autosomal dominant, the primary mechanism for isolated NTDs is not solely due to a single dominant gene.
*X-linked recessive*
- Involves genes on the **X chromosome** where two altered copies are needed in females, but only one in males; typically affects males predominantly.
- This inheritance pattern does not account for the observed familial clustering and environmental contribution seen in NTDs.
More Implantation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.