Gametogenesis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gametogenesis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gametogenesis US Medical PG Question 1: Fertilization begins when sperm binds to the corona radiata of the egg. Once the sperm enters the cytoplasm, a cortical reaction occurs which prevents other sperm from entering the oocyte. The oocyte then undergoes an important reaction. What is the next reaction that is necessary for fertilization to continue?
- A. The second meiotic division (Correct Answer)
- B. Degeneration of the sperm tail
- C. Release of a polar body
- D. Formation of the spindle apparatus
- E. Acrosome reaction
Gametogenesis Explanation: ***The second meiotic division***
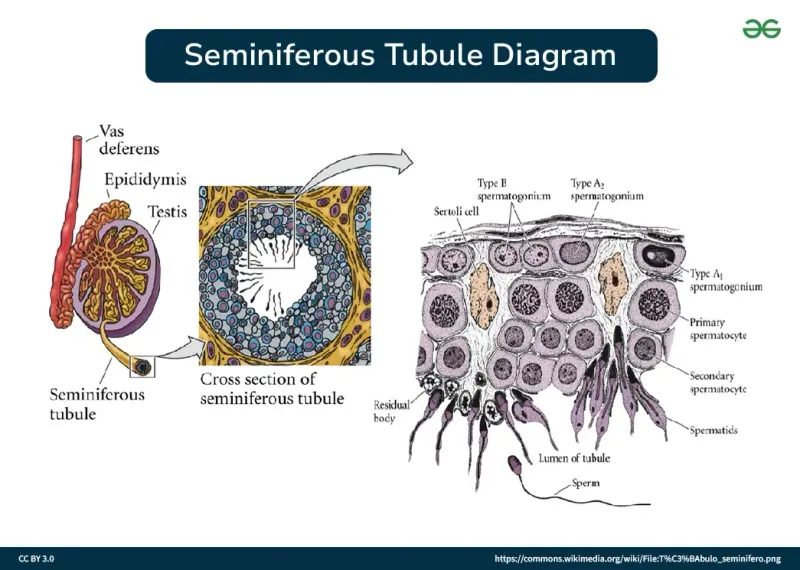
- Upon **sperm penetration**, the secondary oocyte completes its **meiosis II**, forming a mature ovum and a second polar body.
- This completion of meiosis II is a critical step for the pronuclear fusion and subsequent **zygote formation**.
*Degeneration of the sperm tail*
- While the sperm tail does degenerate within the ooplasm, it occurs **after** the genetic material has been released and is not the immediate next critical reaction for continued fertilization.
- This is a process of degradation and assimilation, not an active cellular reaction of the oocyte vital for fertilization progression.
*Release of a polar body*
- The first polar body is released **before fertilization** (at the completion of meiosis I), and the second polar body is released **concomitantly with the completion of meiosis II**, which is the required reaction.
- Releasing a polar body is a consequence of meiotic division, not an independent reaction that drives fertilization forward.
*Formation of the spindle apparatus*
- The **spindle apparatus** is formed during both meiotic divisions to separate chromosomes, but its formation itself is not the immediate "next reaction" necessary for fertilization to continue after cortical reaction.
- The key event is the progression of meiosis, which the spindle facilitates, not the mere formation of the apparatus.
*Acrosome reaction*
- The **acrosome reaction** occurs **before** the sperm binds to the zona pellucida and penetrates the oocyte, enabling the release of enzymes to digest the egg's outer layers.
- This reaction has already taken place for the sperm to have entered the oocyte and initiated the cortical reaction.
Gametogenesis US Medical PG Question 2: A 32-year-old woman, gravida 2, para 1, at 14-weeks' gestation comes to the physician for a prenatal visit. Routine first trimester screening shows increased nuchal translucency, decreased β-hCG concentration, and decreased levels of pregnancy-associated plasma protein A. Amniocentesis shows trisomy of chromosome 13. This fetus is at increased risk for which of the following?
- A. Duodenal atresia
- B. Cutis aplasia (Correct Answer)
- C. Cystic hygroma
- D. Optic glioma
- E. Prominent occiput
Gametogenesis Explanation: ***Cutis aplasia***
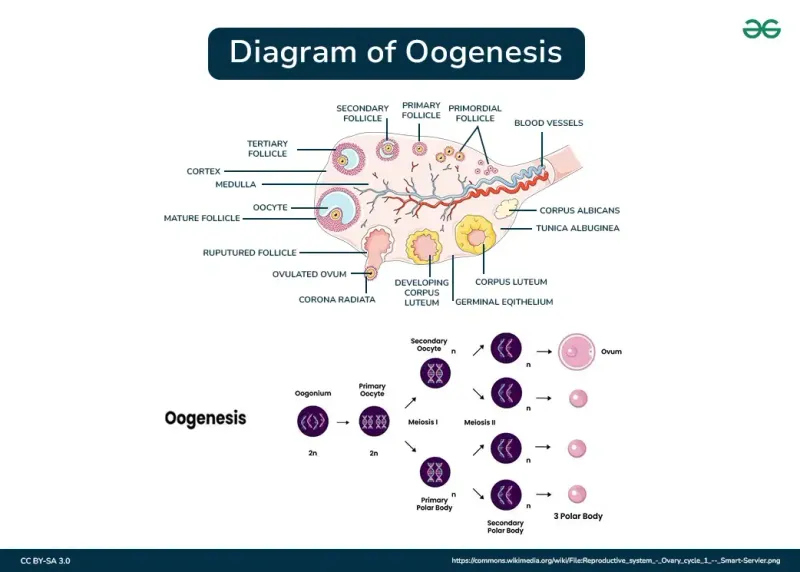
- **Trisomy 13 (Patau syndrome)** is characterized by **cutis aplasia**, which is a congenital absence of skin, typically on the scalp.
- Other common features of Trisomy 13 include **midline defects**, microphthalmia, cleft lip/palate, polydactyly, and severe intellectual disability.
*Duodenal atresia*
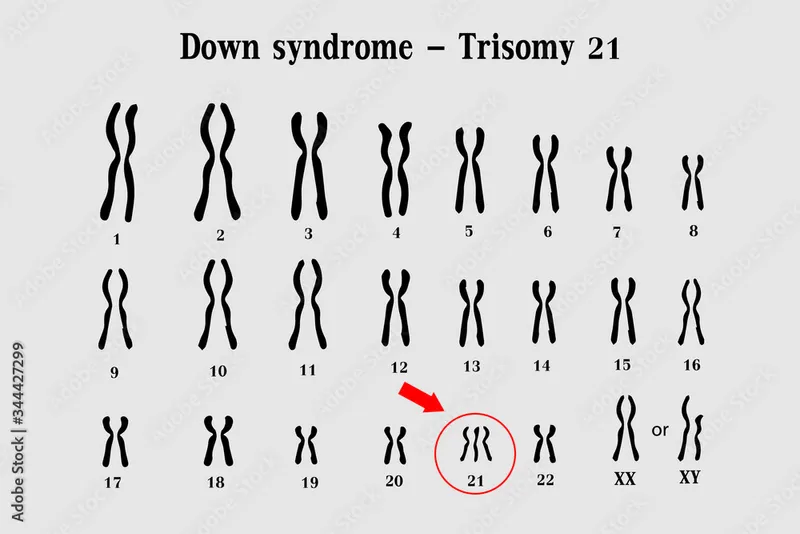
- **Duodenal atresia** is strongly associated with **Trisomy 21 (Down syndrome)**, not Trisomy 13.
- It presents with a "double bubble" sign on imaging due to dilation of the stomach and proximal duodenum.
*Cystic hygroma*
- **Cystic hygromas**, which are lymphatic malformations, are a common finding in **Turner syndrome (XO)** and **Trisomy 18 (Edwards syndrome)**.
- While increased nuchal translucency is noted, a cystic hygroma itself is not a specific finding for Trisomy 13.
*Optic glioma*
- **Optic gliomas** are tumors of the optic nerve most frequently associated with **neurofibromatosis type 1**, an autosomal dominant disorder.
- They are not a characteristic finding of Trisomy 13.
*Prominent occiput*
- A **prominent occiput** is a classic feature of **Trisomy 18 (Edwards syndrome)**.
- This condition is also associated with rocker-bottom feet, micrognathia, and clenched hands with overlapping fingers.
Gametogenesis US Medical PG Question 3: A 19-year-old male from rural West Virginia presents to his family medicine doctor to discuss why he is having trouble getting his wife pregnant. On exam, he is 6 feet 2 inches with a frail frame and broad hips for a male his size. He is noted to have mild gynecomastia, no facial hair, and small, underdeveloped testes. He claims that although he has a lower libido than most of his friends, he does have unprotected sex with his wife. His past medical history is notable for developmental delay and difficulties in school. What is the most likely chromosomal abnormality in this patient?
- A. Trisomy 13
- B. 45: XO
- C. Trisomy 21
- D. 47: XYY
- E. 47: XXY (Correct Answer)
Gametogenesis Explanation: ***47: XXY***
- The patient's presentation with **infertility**, small testes, **gynecomastia**, eunuchoid body habitus (tall, frail frame, broad hips), lack of facial hair, and **developmental delay** are classic features of **Klinefelter syndrome (47, XXY)**.
- This chromosomal abnormality leads to primary **hypogonadism** due to the presence of an extra X chromosome in males.
*Trisomy 13*
- Trisomy 13, or **Patau syndrome**, is characterized by severe developmental anomalies, including **cleft lip and palate**, polydactyly, and severe neurological defects.
- Infants with Trisomy 13 rarely survive beyond the first year and do not present with the described signs of hypogonadism or gynecomastia in adolescence.
*45: XO*
- **45, XO** or **Turner syndrome** affects females and is characterized by **short stature**, primary amenorrhea, webbed neck, and **gonadal dysgenesis (streak gonads)**.
- This karyotype is incompatible with a male phenotype and the symptoms described.
*Trisomy 21*
- Trisomy 21, or **Down syndrome**, is associated with distinct facial features, intellectual disability, and congenital heart defects.
- While individuals with Down syndrome may have fertility issues, they do not typically present with the specific combination of **gynecomastia**, eunuchoid habitus, and **small testes** seen in this patient.
*47: XYY*
- **47, XYY syndrome** is associated with increased height and potentially some learning difficulties, but typically does not cause the significant **hypogonadism**, **gynecomastia**, or **small testes** seen in this patient.
- Men with 47, XYY usually have normal sexual development and fertility, though some may experience learning disabilities or behavioral problems.
Gametogenesis US Medical PG Question 4: A 36-year-old G4P0A3 woman presents at the prenatal diagnostic center at 18 weeks of gestation for the scheduled fetal anomaly scan. The patient's past medical history reveals spontaneous abortions. She reports that her 1st, 2nd, and 3rd pregnancy losses occurred at 8, 10, and 12 weeks of gestation, respectively. Ultrasonography indicates a female fetus with cystic hygroma (measuring 4 cm x 5 cm in size) and fetal hydrops. Which of the following karyotypes does her fetus most likely carry?
- A. 45 X0 (Correct Answer)
- B. Monosomy 18
- C. Trisomy 13
- D. Trisomy 21
- E. Monosomy 13
Gametogenesis Explanation: ***45 X0***
- The presence of **cystic hygroma** and **fetal hydrops** strongly suggests **Turner syndrome (45, X0)**, as these are classic sonographic findings.
- The history of **recurrent early pregnancy losses** is also consistent with chromosomal aneuploidies, with 45, X0 being a common cause of such losses.
*Monosomy 18*
- **Monosomy 18** is a very rare and usually lethal chromosomal abnormality, typically resulting in **early miscarriage**.
- Its clinical presentation, if live-born, is distinct and does not primarily feature **cystic hygroma** or **hydrops** as the main diagnostic clues.
*Trisomy 13*
- **Trisomy 13 (Patau syndrome)** is associated with severe malformations, including **cleft lip/palate**, **polydactyly**, and **holoprosencephaly**.
- While it can cause fetal hydrops and other structural anomalies, **cystic hygroma** is not its most characteristic or common sonographic marker in the way it is for Turner syndrome.
*Trisomy 21*
- **Trisomy 21 (Down syndrome)** is characterized by **nuchal translucency** and **cardiac defects**, but **cystic hygroma** and **hydrops** are less common and less severe than in Turner syndrome.
- The constellation of findings in this case points more strongly to Turner syndrome.
*Monosomy 13*
- **Monosomy 13** is an extremely rare and usually **lethal** chromosomal anomaly, often leading to early spontaneous abortion.
- It would typically result in more severe generalized developmental defects rather than the specific combination of **cystic hygroma** and **hydrops** seen here.
Gametogenesis US Medical PG Question 5: A couple brings their 1-year-old child to a medical office for a follow-up evaluation of his small, empty scrotum. The scrotum has been empty since birth and the physician asked them to follow up with a pediatrician. There are no other complaints. The immunization history is up to date and his growth and development have been excellent. On examination, he is a playful, active child with a left, non-reducible, non-tender inguinal mass, an empty and poorly rugated hemiscrotal sac, and a testis within the right hemiscrotal sac. Which of the following hormones would likely be deficient in this patient by puberty if the condition is left untreated?
- A. LH
- B. Testosterone (Correct Answer)
- C. FSH
- D. Inhibin
- E. Prolactin
Gametogenesis Explanation: ***Testosterone***
- **Testosterone** is produced by the **Leydig cells** in the testes. In untreated cryptorchidism, the elevated temperature in the inguinal canal causes progressive damage to both Sertoli cells and **Leydig cells** over time.
- By **puberty**, if left untreated for 11-13 years, the undescended testis will have significant irreversible Leydig cell dysfunction, leading to **reduced testosterone production**.
- While unilateral cryptorchidism may allow the contralateral descended testis to partially compensate, this compensation is often **incomplete during the high testosterone demands of puberty**, resulting in relative testosterone deficiency.
- This is the most clinically significant hormonal deficiency that develops with prolonged untreated cryptorchidism.
*LH*
- **Luteinizing hormone (LH)** is produced by the anterior pituitary and stimulates Leydig cells to produce testosterone. In cryptorchidism with resulting testosterone deficiency, LH levels would be **elevated** (not deficient) as a compensatory response.
- The pituitary responds normally to low testosterone with increased LH secretion via loss of negative feedback.
*Inhibin*
- **Inhibin** is produced by **Sertoli cells** in the seminiferous tubules. While cryptorchidism impairs Sertoli cell function and spermatogenesis, inhibin itself is not typically **deficient**.
- The primary consequence is **impaired spermatogenesis**, which leads to reduced negative feedback and **elevated FSH** levels, but inhibin levels may remain normal or only modestly reduced.
*FSH*
- **Follicle-stimulating hormone (FSH)** is produced by the anterior pituitary. In cryptorchidism, FSH is typically **elevated** (not deficient) due to impaired Sertoli cell function and loss of negative feedback from the seminiferous tubules.
- Elevated FSH is a marker of tubular dysfunction but is not itself deficient.
*Prolactin*
- **Prolactin** is produced by the anterior pituitary and primarily regulates lactation. It has no direct role in testicular function or the pathophysiology of cryptorchidism.
- There is no association between cryptorchidism and prolactin deficiency.
Gametogenesis US Medical PG Question 6: An investigator is studying human genetics and cell division. A molecule is used to inhibit the exchange of genetic material between homologous chromosomes. Which of the following phases of the cell cycle does the molecule target?
- A. Prophase II
- B. Prophase I (Correct Answer)
- C. Metaphase II
- D. Telophase I
- E. Anaphase I
Gametogenesis Explanation: ***Prophase I***
- **Crossing over** (genetic recombination) occurs specifically during **Prophase I** of meiosis, particularly during the pachytene stage
- During this phase, homologous chromosomes pair up (synapsis) and exchange genetic material through recombination
- Inhibiting this exchange means targeting the phase where this critical genetic recombination takes place
*Prophase II*
- Prophase II is a stage in meiosis II where chromosomes condense again after a brief interkinesis
- **Crossing over does not occur** in Prophase II - genetic recombination has already been completed in Prophase I
- Homologous chromosomes are no longer paired at this stage
*Metaphase II*
- During Metaphase II, individual chromosomes (not homologous pairs) align along the metaphase plate
- There is **no exchange of genetic material** between homologous chromosomes at this stage
- This phase prepares for the separation of sister chromatids
*Telophase I*
- Telophase I involves decondensation of chromosomes and reformation of nuclear envelopes around the separated homologous chromosomes
- This marks the end of meiosis I, **after** genetic exchange has already occurred in Prophase I
- No crossing over occurs during this phase
*Anaphase I*
- In Anaphase I, **homologous chromosomes separate** and move to opposite poles of the cell
- This phase is characterized by segregation of chromosomes, **not genetic exchange**
- Crossing over has already been completed by this stage
Gametogenesis US Medical PG Question 7: Research is being conducted on embryoblasts. The exact date of fertilization is unknown. There is the presence of a cytotrophoblast and syncytiotrophoblast, marking the time when implantation into the uterus would normally occur. Within the embryoblast, columnar and cuboidal cells are separated by a membrane. Which of these cell layers begins to line the yolk sac cavity?
- A. Hypoblast (Correct Answer)
- B. Epiblast
- C. Syncytiotrophoblast
- D. Inner cell mass
- E. Endoderm
Gametogenesis Explanation: ***Hypoblast***
- The **hypoblast** is a layer of cuboidal cells that forms from the inner cell mass around day 8 post-fertilization.
- It plays a crucial role in forming the **primary yolk sac** by migrating to line the exocoelomic cavity.
*Epiblast*
- The **epiblast** is composed of columnar cells located dorsal to the hypoblast and forms the floor of the **amniotic cavity**.
- It is the source of the **three primary germ layers** during gastrulation (ectoderm, mesoderm, and endoderm), not the yolk sac lining itself.
*Syncytiotrophoblast*
- The **syncytiotrophoblast** is the outer, invasive layer of the trophoblast that facilitates implantation and forms the fetal component of the placenta.
- It is not involved in lining the yolk sac cavity but rather in **invading the uterine endometrium** and producing hCG.
*Inner cell mass*
- The **inner cell mass (ICM)** is the cluster of cells within the blastocyst that gives rise to the embryoblast (which further differentiates into epiblast and hypoblast).
- The ICM itself does not line the yolk sac; rather, its derivative, the hypoblast, does.
*Endoderm*
- The **endoderm** is one of the three primary germ layers that forms during gastrulation from the epiblast derivative.
- It ultimately forms the linings of the **gastrointestinal and respiratory tracts**, not the primary yolk sac lining.
Gametogenesis US Medical PG Question 8: What is the pattern of inheritance in neural tube defects?
- A. Multifactorial inheritance (Correct Answer)
- B. Autosomal recessive
- C. X-linked dominant
- D. Autosomal dominant
- E. X-linked recessive
Gametogenesis Explanation: ***Multifactorial inheritance***
- Neural tube defects (NTDs) are a classic example of **multifactorial inheritance**, meaning they result from a combination of **genetic predispositions** and **environmental factors**.
- Risk is influenced by multiple genes, and environmental factors like **folate deficiency** play a significant role.
*Autosomal recessive*
- This pattern involves two copies of an altered gene to cause disease, typically resulting in a **25% recurrence risk** for siblings.
- While some rare isolated NTDs might have an autosomal recessive component, the general presentation of NTDs does not fit this classic mendelian pattern.
*X-linked dominant*
- Involves genes on the **X chromosome** where one altered copy is sufficient to cause disease; affected fathers pass it to all daughters, but no sons.
- This inheritance pattern is very rare for NTDs and would present with a distinct sex-linked pattern of affected individuals.
*Autosomal dominant*
- Requires only one copy of an altered gene to cause disease, leading to a **50% recurrence risk** for offspring.
- While some syndromes associated with NTDs can be autosomal dominant, the primary mechanism for isolated NTDs is not solely due to a single dominant gene.
*X-linked recessive*
- Involves genes on the **X chromosome** where two altered copies are needed in females, but only one in males; typically affects males predominantly.
- This inheritance pattern does not account for the observed familial clustering and environmental contribution seen in NTDs.
Gametogenesis US Medical PG Question 9: The covering of an omphalocele is derived from which of the following layers?
- A. Amnion (Correct Answer)
- B. Chorion
- C. Mesoderm
- D. Endoderm
- E. Ectoderm
Gametogenesis Explanation: ***Amnion***
- An **omphalocele** is a congenital abdominal wall defect where abdominal contents protrude through the umbilical ring, covered by a sac derived from the **amnion** and peritoneum.
- The covering of an omphalocele defect is an intact peritoneal sac that is covered externally by **amnion**.
*Chorion*
- The **chorion** is the outermost membrane surrounding an embryo, providing protection and nourishment, but it does not form the covering of an omphalocele.
- It works in conjunction with the decidua to form the **placenta** and has finger-like projections called villi on its outer surface.
*Mesoderm*
- The **mesoderm** is one of the three primary germ layers in embryonic development, giving rise to connective tissue, muscle, and blood cells.
- **Fetal skin**, not the omphalocele covering, develops from the mesoderm and ectoderm.
*Endoderm*
- The **endoderm** is the innermost of the three primary germ layers, giving rise to the lining of the digestive tract and respiratory system.
- The omphalocele covering is derived from the amnion, not the endoderm, which is involved in forming internal organs.
*Ectoderm*
- The **ectoderm** is the outermost of the three primary germ layers, giving rise to the nervous system, skin epidermis, and sensory organs.
- While ectoderm contributes to skin development, the omphalocele sac is specifically covered by amnion, not ectodermal derivatives.
Gametogenesis US Medical PG Question 10: Scientists are studying human lung development by trying to identify which proteins and signaling factors trigger lung bud division and bronchiole branching. Their main focus is particularly around the 20th week of gestation, during which terminal bronchioles branch into respiratory bronchioles and further into alveolar ducts. Which of the following phases of embryonic lung development is the stage in which the scientists are interested in studying?
- A. Canalicular (Correct Answer)
- B. Alveolar
- C. Pseudoglandular
- D. Saccular
- E. Embryonic
Gametogenesis Explanation: ***Canalicular***
- The **canalicular stage**, occurring from weeks 16 to 26, is characterized by the formation of **respiratory bronchioles**, alveolar ducts, and the beginning of vascularization.
- This stage is crucial for the development of blood-air barrier precursors, making it relevant for studying branching and differentiation into gas exchange structures.
*Alveolar*
- The **alveolar stage** begins much later (late fetal period, 32 weeks, continuing for several years postpartum) and primarily involves the maturation of **alveoli** and increase in their numbers.
- While essential for complete lung function, it does not describe the initial branching and differentiation of bronchioles that occurs around 20 weeks.
*Pseudoglandular*
- The **pseudoglandular stage**, from weeks 6 to 16, involves the formation of the major conducting airways (bronchi and terminal bronchioles) but not yet respiratory bronchioles or alveolar ducts.
- The description of terminal bronchioles branching into respiratory bronchioles places it beyond this stage.
*Saccular*
- The **saccular stage**, from weeks 26 to 32, is marked by the formation of saccules (primitive alveoli) and further thinning of the blood-air barrier.
- While it involves growth of the respiratory tree, the detailed branching into respiratory bronchioles and alveolar ducts is primarily a feature of the preceding canalicular stage.
*Embryonic*
- The **embryonic stage**, from weeks 3 to 6, is the earliest phase where the lung bud emerges from the foregut and begins to divide into main bronchi.
- This stage is too early for the significant branching described, which involves terminal and respiratory bronchioles.
More Gametogenesis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.