Fertilization and zygote formation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fertilization and zygote formation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fertilization and zygote formation US Medical PG Question 1: Fertilization begins when sperm binds to the corona radiata of the egg. Once the sperm enters the cytoplasm, a cortical reaction occurs which prevents other sperm from entering the oocyte. The oocyte then undergoes an important reaction. What is the next reaction that is necessary for fertilization to continue?
- A. The second meiotic division (Correct Answer)
- B. Degeneration of the sperm tail
- C. Release of a polar body
- D. Formation of the spindle apparatus
- E. Acrosome reaction
Fertilization and zygote formation Explanation: ***The second meiotic division***
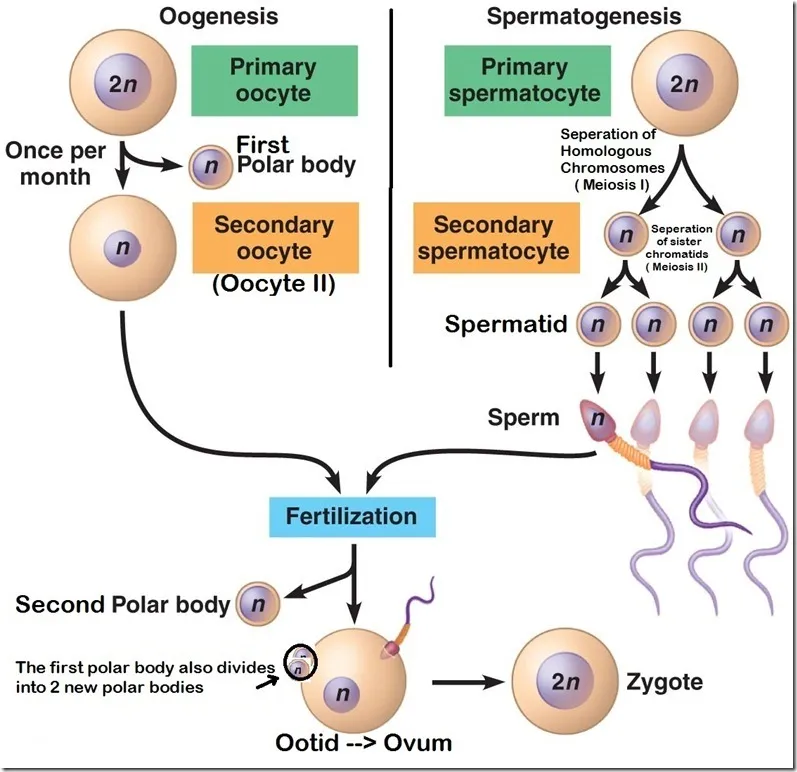
- Upon **sperm penetration**, the secondary oocyte completes its **meiosis II**, forming a mature ovum and a second polar body.
- This completion of meiosis II is a critical step for the pronuclear fusion and subsequent **zygote formation**.
*Degeneration of the sperm tail*
- While the sperm tail does degenerate within the ooplasm, it occurs **after** the genetic material has been released and is not the immediate next critical reaction for continued fertilization.
- This is a process of degradation and assimilation, not an active cellular reaction of the oocyte vital for fertilization progression.
*Release of a polar body*
- The first polar body is released **before fertilization** (at the completion of meiosis I), and the second polar body is released **concomitantly with the completion of meiosis II**, which is the required reaction.
- Releasing a polar body is a consequence of meiotic division, not an independent reaction that drives fertilization forward.
*Formation of the spindle apparatus*
- The **spindle apparatus** is formed during both meiotic divisions to separate chromosomes, but its formation itself is not the immediate "next reaction" necessary for fertilization to continue after cortical reaction.
- The key event is the progression of meiosis, which the spindle facilitates, not the mere formation of the apparatus.
*Acrosome reaction*
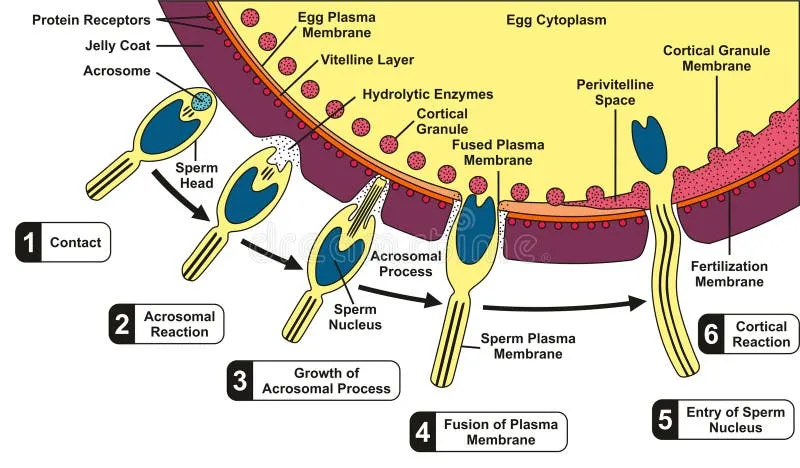
- The **acrosome reaction** occurs **before** the sperm binds to the zona pellucida and penetrates the oocyte, enabling the release of enzymes to digest the egg's outer layers.
- This reaction has already taken place for the sperm to have entered the oocyte and initiated the cortical reaction.
Fertilization and zygote formation US Medical PG Question 2: A 25-year-old woman is brought to the emergency department by her roommate with severe right lower quadrant pain for the last 8 hours. The pain is progressively getting worse and is associated with vomiting. When you ask the patient about her last menstrual period, she tells you that although she stopped keeping track of her cycle after undergoing surgical sterilization 1 year ago, she recalls bleeding yesterday. The physical examination reveals a hemodynamically stable patient with a pulse of 90/min, respiratory rate of 14/min, blood pressure of 125/70 mm Hg, and temperature of 37.0°C (98.6°F). The abdomen is tender to touch (more tender in the lower quadrants), and tenderness at McBurney's point is absent. Which of the following is the best next step in the management of this patient?
- A. Complete blood count
- B. Urinalysis
- C. FAST ultrasound scan
- D. Appendectomy
- E. Urinary human chorionic gonadotropin (hCG) (Correct Answer)
Fertilization and zygote formation Explanation: ***Urinary human chorionic gonadotropin (hCG)***
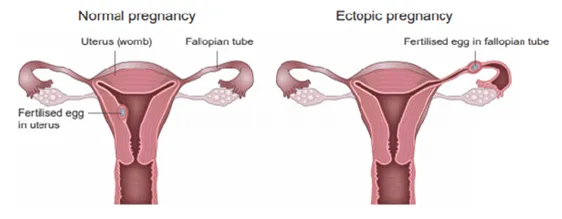
- Despite surgical sterilization, a **low risk of ectopic pregnancy** still exists, especially with symptoms like **severe right lower quadrant pain** and **vomiting**.
- A positive urinary hCG would necessitate further evaluation for an **ectopic pregnancy**, which is a **life-threatening condition**.
*Complete blood count*
- While a CBC assesses for **leukocytosis** (suggesting infection/inflammation) or **anemia** (suggesting blood loss), it's not the immediate priority given the potential for ectopic pregnancy symptoms.
- A CBC alone would not rule out the most critical diagnosis in this scenario.
*Urinalysis*
- A urinalysis helps rule out **urinary tract infection (UTI)** or **nephrolithiasis** (kidney stones).
- While important for differential diagnosis, the severity of pain and reproductive history make ectopic pregnancy a more immediate concern.
*FAST ultrasound scan*
- An ultrasound is useful for identifying **free fluid** in the abdomen or assessing the **uterus and adnexa** for an ectopic pregnancy.
- However, in a female of reproductive age, a **positive hCG** is generally a prerequisite for a targeted pelvic ultrasound to confirm or exclude an early ectopic pregnancy.
*Appendectomy*
- While **appendicitis** is in the differential for right lower quadrant pain, the absence of **McBurney's point tenderness** and the patient's reproductive history make other diagnoses more likely first.
- Surgery should only be considered after a thorough diagnostic workup, especially to rule out time-sensitive conditions like ectopic pregnancy.
Fertilization and zygote formation US Medical PG Question 3: A 30-year-old woman comes to the primary care physician because she has felt nauseous and fatigued for 3 weeks. Menses occur at irregular 24- to 33-day intervals and last for 4–6 days. Her last menstrual period was 7 weeks ago. Her temperature is 37°C (98.6°F), pulse is 95/min, and blood pressure is 100/70 mm Hg. Pelvic examination shows an enlarged uterus. Her serum β-hCG concentration is 96,000 mIU/mL (N < 5). An abdominal ultrasound is shown. Which of the following is the most likely diagnosis?
- A. Partial hydatidiform mole
- B. Bicornuate uterus pregnancy
- C. Abdominal pregnancy
- D. Complete hydatid mole (Correct Answer)
- E. Dichorionic-diamniotic twins
Fertilization and zygote formation Explanation: ***Complete hydatid mole***
- The ultrasound image shows a **\"snowstorm\" appearance** with multiple anechoic cysts, typical of a complete hydatidiform mole, consistent with **grape-like vesicles**.
- The significantly elevated **β-hCG level (96,000 mIU/mL)** and symptoms like nausea in conjunction with an enlarged uterus and irregular menses, are highly indicative of gestational trophoblastic disease.
*Partial hydatidiform mole*
- A partial mole typically shows evidence of **fetal tissue** or a **fetus** with associated placental changes, which is absent in this image and clinical presentation.
- While β-hCG levels can be elevated, they are often lower than in complete moles and less likely to show the classic **\"snowstorm\" appearance** in the absence of fetal parts.
*Bicornuate uterus pregnancy*
- A bicornuate uterus is a **uterine anomaly** where the uterus has two horns, and pregnancy would typically occur in one of these horns, appearing as a normal or atypical intrauterine pregnancy on ultrasound.
- The ultrasound image does not show a normally developing pregnancy within a horn of a bicornuate uterus, but rather a characteristic vesicular pattern within the uterus.
*Abdominal pregnancy*
- Abdominal pregnancy involves an **ectopic implantation** outside the uterus, in the abdominal cavity, often showing abnormal fetal presentation and placental attachment to abdominal organs.
- The ultrasound clearly shows an **intrauterine mass** with the characteristic vesicular pattern, ruling out an abdominal pregnancy.
*Dichorionic-diamniotic twins*
- This refers to a **twin pregnancy** with two separate placentas and two separate amniotic sacs, which would be visible as two distinct gestational sacs and two fetuses on ultrasound.
- The image shows a **single mass** with a vesicular pattern, not two separate gestational sacs or fetuses, nor two distinct placentas.
Fertilization and zygote formation US Medical PG Question 4: A 34-year-old woman comes to the fertility clinic with her husband for infertility treatment. The couple has been having unprotected intercourse for the past 2 years without any pregnancies. This is their first time seeking fertility treatment. The patient's past medical history includes asthma. She denies any menstrual irregularities, menstrual pain, abnormal bleeding or past sexually transmitted infections. The husband reports that "he would get sick easily and would always have some upper respiratory infections." Physical examination of the wife demonstrates nasal polyps bilaterally; vaginal examination is unremarkable. Physical examination of the husband is unremarkable. Semen analysis results are shown below:
Semen analysis:
Volume: 1.9 mL (Normal > 1.5 mL)
pH: 7.4 (Normal: > 7.2)
Sperm concentration: 0 million/mL (Normal: > 15 million/mL)
Total sperm count: 0 million/mL (Normal: > 39 million/mL)
Total motility: N/A (Normal: > 40%)
Morphology: N/A (Normal: > 4% normal forms)
What is the most likely explanation for this couple's infertility?
- A. XO chromosome in wife
- B. Undescended testes in husband
- C. XXY chromosome in husband
- D. Deletion of Phe508 in husband (Correct Answer)
- E. Deletion of Phe508 in wife
Fertilization and zygote formation Explanation: ***Deletion of Phe508 in husband***
- The husband's history of recurrent respiratory infections combined with **complete azoospermia** (zero sperm despite normal semen volume) is highly suggestive of **Cystic Fibrosis** due to **CFTR gene mutation**, with **deletion of Phe508 (ΔF508)** being the most common mutation.
- CFTR mutations frequently cause **congenital bilateral absence of the vas deferens (CBAVD)**, resulting in obstructive azoospermia where sperm are produced but cannot be ejaculated due to absent vas deferens.
- This provides a **unifying diagnosis** explaining both the male infertility and respiratory symptoms.
*XO chromosome in wife*
- **Turner syndrome (45,XO)** presents with **primary amenorrhea**, **streak gonads**, short stature, and absent secondary sexual characteristics.
- The wife has **normal menstrual history** and unremarkable fertility evaluation, making this diagnosis incompatible with her presentation.
- The semen analysis clearly identifies **male-factor infertility** as the cause.
*Undescended testes in husband*
- **Cryptorchidism** can impair spermatogenesis due to elevated testicular temperature, typically causing **oligospermia** (reduced sperm count) rather than complete azoospermia.
- Physical examination of the husband was unremarkable, making undescended testes unlikely.
- This diagnosis does not explain the recurrent respiratory infections.
*XXY chromosome in husband*
- **Klinefelter syndrome (47,XXY)** causes **primary hypogonadism** with azoospermia, small firm testes, gynecomastia, and often tall stature with eunuchoid proportions.
- While it explains the azoospermia, it **does not account for the recurrent respiratory infections**, whereas CFTR mutation explains both features.
- Physical exam was unremarkable, without typical Klinefelter stigmata.
*Deletion of Phe508 in wife*
- While the wife has asthma and nasal polyps (which can be seen in CF or overlap with asthma-related conditions), her **normal menstrual history** indicates she is likely fertile.
- The **male-factor infertility** (complete azoospermia in the husband) is the direct cause of the couple's inability to conceive.
- Even if the wife has CF, this would not explain the husband's azoospermia, which is the primary barrier to conception.
Fertilization and zygote formation US Medical PG Question 5: A research team is studying certain congenital anomalies of the respiratory tract. The method consists of marking a certain germinal layer with an isotope, following its development stages in chicken embryos, and finally analyzing the specimen. A given specimen of tissue is presented in the exhibit. Which of the following germinal structures most likely gave rise to the epithelial lining of this specimen?
- A. Ectoderm
- B. Neural crest
- C. Mesoderm
- D. Endoderm (Correct Answer)
- E. Surface ectoderm
Fertilization and zygote formation Explanation: ***Endoderm***
- The **epithelial lining** of the entire respiratory tract, including the larynx, trachea, bronchi, and lungs, is derived from the **endoderm**.
- The **laryngotracheal groove** develops from the ventral wall of the primitive foregut, which is endodermal in origin, further differentiating into the respiratory tree.
*Ectoderm*
- The **ectoderm** primarily forms the epidermis, hair, nails, and the nervous system (brain and spinal cord).
- It does not contribute to the internal epithelial lining of the respiratory tract.
*Neural crest*
- **Neural crest cells** contribute to a wide variety of structures, including components of the peripheral nervous system, head mesenchyme, and melanocytes.
- They are not involved in forming the epithelial lining of the respiratory system.
*Mesoderm*
- The **mesoderm** forms the connective tissue, cartilage, and muscle components of the respiratory tract, such as the smooth muscle and cartilage rings of the trachea and bronchi, and the visceral pleura.
- However, it does not form the epithelial lining itself.
*Surface ectoderm*
- **Surface ectoderm** specifically gives rise to the epidermis, hair, nails, and glands of the skin, as well as the oral cavity epithelium.
- It does not contribute to the internal epithelial structures of the respiratory tract.
Fertilization and zygote formation US Medical PG Question 6: A 24-year-old woman presents to the emergency department for evaluation of lower abdominal pain. She endorses 6 hours of progressively worsening pain. She denies any significant past medical history and her physical examination is positive for non-specific, diffuse pelvic discomfort. She denies the possibility of pregnancy given her consistent use of condoms with her partner. The vital signs are: blood pressure, 111/68 mm Hg; pulse, 71/min; and respiratory rate, 15/min. She is afebrile. Which of the following is the next best step in her management?
- A. Surgical consultation
- B. Admission and observation
- C. Obtain a pelvic ultrasound
- D. Serum hCG (Correct Answer)
- E. Abdominal CT scan
Fertilization and zygote formation Explanation: ***Serum hCG***
- Despite the patient's claim of consistent condom use, **pregnancy must be ruled out** in any woman of reproductive age presenting with lower abdominal pain. **Ectopic pregnancy** is a life-threatening condition that can present this way.
- A **serum hCG** is more sensitive than a urine test and can detect very early pregnancies, which is crucial for prompt diagnosis and management.
*Surgical consultation*
- Surgical consultation would be premature without a definitive diagnosis or clear signs of an acute surgical abdomen, such as peritonitis or hemodynamic instability.
- Initial diagnostic steps are necessary to identify the cause of the pain before considering surgical intervention.
*Admission and observation*
- While observation might be necessary, it's not the immediate next best step. Without a diagnosis, observation alone may delay critical interventions for conditions like ectopic pregnancy.
- Admission for observation typically follows initial diagnostic workup when the diagnosis is uncertain but not immediately life-threatening.
*Obtain a pelvic ultrasound*
- A pelvic ultrasound is an important diagnostic tool for evaluating pelvic pain, but it should be performed only **after pregnancy has been ruled out** or confirmed.
- If the patient is pregnant, a pelvic ultrasound would be used to assess for intrauterine or ectopic pregnancy. If she is not pregnant, the ultrasound would help identify other gynecological causes of pain.
*Abdominal CT scan*
- An abdominal CT scan is less specific for gynecological causes of pain and exposes the patient to **ionizing radiation**, making it a less ideal initial step compared to ruling out pregnancy.
- It might be considered if the initial workup for gynecological causes is negative or if there are concerns for other intra-abdominal pathology.
Fertilization and zygote formation US Medical PG Question 7: A 38-year-old woman presents to her primary care physician concerned about her inability to get pregnant for the past year. She has regular menstrual cycles and has unprotected intercourse with her husband daily. She is an immigrant from Australia and her past medical history is not known. She is currently taking folic acid and multivitamins. The patient's husband has had a sperm count that was determined to be within the normal range twice. She is very concerned about her lack of pregnancy and that she is too old. Which of the following is the most appropriate next step in management for this patient?
- A. Repeat semen count
- B. Assess ovulation with an ovulation calendar
- C. Perform hysterosalpingogram (Correct Answer)
- D. Advise against pregnancy given the patient's age
- E. Continue regular intercourse for 1 year
Fertilization and zygote formation Explanation: ***Perform hysterosalpingogram***
- Given the patient’s age and duration of infertility (1 year at age 38, typically evaluation starts earlier for those over 35), assessing **tubal patency** with a **hysterosalpingogram (HSG)** is an essential step in the infertility workup.
- HSG can identify structural abnormalities like **blocked fallopian tubes** or **uterine anomalies**, which are common causes of infertility.
*Repeat semen count*
- The husband has already had **two normal semen analyses**, making further repeated testing at this stage less likely to yield new information or be the most appropriate next step.
- While male factor infertility is common, it has been reasonably excluded here, shifting the focus to female factors.
*Assess ovulation with an ovulation calendar*
- The patient reports having **regular menstrual cycles**, which strongly suggests she is **ovulating regularly**.
- Ovulation calendars are often used to identify the fertile window but are less useful for confirming ovulation in someone with regular cycles when investigating infertility causes.
*Advise against pregnancy given the patient's age*
- While **fertility declines with age**, advising against pregnancy is inappropriate and **premature** without a proper infertility workup.
- Many women in their late 30s and early 40s successfully conceive with appropriate management and intervention.
*Continue regular intercourse for 1 year*
- For women aged 35 or older, an infertility evaluation is typically initiated after **6 months of unprotected intercourse** without conception.
- The patient is 38 and has been trying for a year, so further delay is not recommended; an immediate workup is warranted.
Fertilization and zygote formation US Medical PG Question 8: Research is being conducted on embryoblasts. The exact date of fertilization is unknown. There is the presence of a cytotrophoblast and syncytiotrophoblast, marking the time when implantation into the uterus would normally occur. Within the embryoblast, columnar and cuboidal cells are separated by a membrane. Which of these cell layers begins to line the yolk sac cavity?
- A. Hypoblast (Correct Answer)
- B. Epiblast
- C. Syncytiotrophoblast
- D. Inner cell mass
- E. Endoderm
Fertilization and zygote formation Explanation: ***Hypoblast***
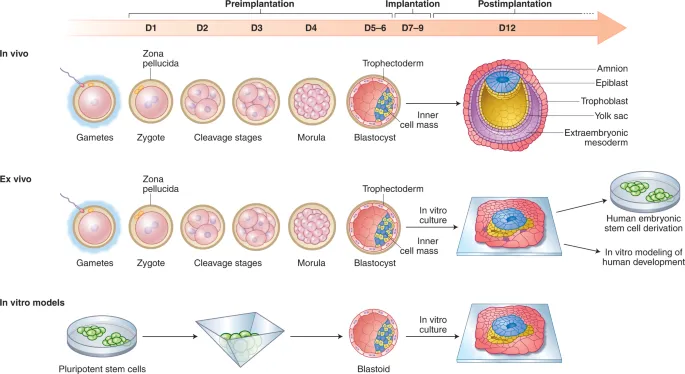
- The **hypoblast** is a layer of cuboidal cells that forms from the inner cell mass around day 8 post-fertilization.
- It plays a crucial role in forming the **primary yolk sac** by migrating to line the exocoelomic cavity.
*Epiblast*
- The **epiblast** is composed of columnar cells located dorsal to the hypoblast and forms the floor of the **amniotic cavity**.
- It is the source of the **three primary germ layers** during gastrulation (ectoderm, mesoderm, and endoderm), not the yolk sac lining itself.
*Syncytiotrophoblast*
- The **syncytiotrophoblast** is the outer, invasive layer of the trophoblast that facilitates implantation and forms the fetal component of the placenta.
- It is not involved in lining the yolk sac cavity but rather in **invading the uterine endometrium** and producing hCG.
*Inner cell mass*
- The **inner cell mass (ICM)** is the cluster of cells within the blastocyst that gives rise to the embryoblast (which further differentiates into epiblast and hypoblast).
- The ICM itself does not line the yolk sac; rather, its derivative, the hypoblast, does.
*Endoderm*
- The **endoderm** is one of the three primary germ layers that forms during gastrulation from the epiblast derivative.
- It ultimately forms the linings of the **gastrointestinal and respiratory tracts**, not the primary yolk sac lining.
Fertilization and zygote formation US Medical PG Question 9: A researcher is studying gamete production and oogenesis. For her experiment, she decides to cultivate primary oocytes in their arrested state and secondary oocytes just prior to fertilization. When she examines these gametes, she will find that the primary oocytes and secondary oocytes are arrested in which phases of meiosis, respectively?
- A. Anaphase I; anaphase II
- B. Interphase I; prophase II
- C. Metaphase I; metaphase II
- D. Metaphase I; prophase II
- E. Prophase I; metaphase II (Correct Answer)
Fertilization and zygote formation Explanation: ***Prophase I; metaphase II***
- **Primary oocytes** are arrested in **prophase I** from embryonic development until puberty, when they resume meiosis in preparation for ovulation.
- **Secondary oocytes** are immediately arrested in **metaphase II** after completing meiosis I, and they will remain in this stage until fertilization occurs.
*Anaphase I; anaphase II*
- **Anaphase I** involves the separation of **homologous chromosomes**, and **anaphase II** involves the separation of **sister chromatids**. Neither primary nor secondary oocytes are arrested in these stages.
- Meiotic arrest occurs at earlier stages to prevent further division until specific triggers (ovulation or fertilization) are met.
*Interphase I; prophase II*
- **Interphase I** precedes meiosis I, during which DNA replication occurs, and it is not a stage of meiotic arrest for primary oocytes.
- **Prophase II** is a transient stage in meiosis II, and secondary oocytes are arrested later in **metaphase II**, not prophase II.
*Metaphase I; metaphase II*
- While **secondary oocytes** are indeed arrested in **metaphase II**, **primary oocytes** are arrested much earlier in **prophase I**, not metaphase I.
- The arrest in metaphase I is temporary for primary oocytes as they complete meiosis I to form secondary oocytes upon hormonal signaling.
*Metaphase I; prophase II*
- **Primary oocytes** are arrested in **prophase I**, not metaphase I. Meiosis I is completed before ovulation, leading to the formation of secondary oocytes.
- **Secondary oocytes** are arrested in **metaphase II**, not prophase II, awaiting fertilization to complete meiosis II.
Fertilization and zygote formation US Medical PG Question 10: A 26-year-old woman comes to the physician because she has not had a menstrual period for 5 weeks. Menarche was at the age of 14 years and menses occurred at regular 30-day intervals. She reports having unprotected sexual intercourse 3 weeks ago. A urine pregnancy test is positive. Which of the following best describes the stage of development of the embryo at this time?
- A. Fetal heart is beating, but cardiac activity is not yet visible on ultrasound
- B. Limb buds have formed, but fetal movements have not begun
- C. Sexual differentiation has begun, but fetal movement has not started
- D. Neural crest has formed, but limb buds have not yet formed (Correct Answer)
- E. Implantation has occurred, but notochord has not yet formed
Fertilization and zygote formation Explanation: ***Neural crest has formed, but limb buds have not yet formed***
- At **5 weeks gestational age (3 weeks post-fertilization)**, neurulation is completing or recently completed
- **Neural crest cells** migrate from the neural folds during weeks 3-4 post-fertilization and are definitely present by this time
- **Limb buds** appear later, around week 4-5 post-fertilization (week 6-7 gestational age), making this the most accurate description for the current developmental stage
*Fetal heart is beating, but cardiac activity is not yet visible on ultrasound*
- The primitive heart tube begins contracting around day 22-23 post-fertilization (early week 4)
- At 3 weeks post-fertilization (5 weeks gestational age), the heart may just be starting to beat, but this timing is less precise
- Cardiac activity becomes visible on transvaginal ultrasound around 5.5-6 weeks gestational age, so this option is close but less precise than the correct answer
*Limb buds have formed, but fetal movements have not begun*
- **Limb buds** typically appear around week 4-5 post-fertilization (week 6-7 gestational age)
- This is **too advanced** for 3 weeks post-fertilization
- While fetal movements aren't perceptible to the mother until 16-20 weeks, they begin much later than the current stage
*Sexual differentiation has begun, but fetal movement has not started*
- **Sexual differentiation** of the gonads begins around week 7 post-fertilization (week 9 gestational age)
- External genitalia differentiation occurs even later (weeks 9-12 post-fertilization)
- This stage is **far too advanced** for the current 3-week post-fertilization timeframe
*Implantation has occurred, but notochord has not yet formed*
- **Implantation** occurs 6-12 days after fertilization, which is approximately 2-3 weeks before a positive pregnancy test
- The **notochord** forms during gastrulation in the **3rd week post-fertilization** (5th week gestational age)
- By the time of this positive pregnancy test (5 weeks gestational age), the notochord has **already formed**, making this statement incorrect
More Fertilization and zygote formation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.