Thoracic dermatomes and myotomes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thoracic dermatomes and myotomes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thoracic dermatomes and myotomes US Medical PG Question 1: A 63-year-old man presents to the clinic concerned about numbness and weakness in his bilateral shoulders and arms for the past 8 weeks. The symptoms started when he fell from scaffolding at work and landed on his back. Initial workup was benign and he returned to normal duty. However, his symptoms have progressively worsened since the fall. He denies fever, back pain, preceding vomiting, and diarrhea. He has a history of type 2 diabetes mellitus, hypertension, hypercholesterolemia, ischemic heart disease, and a 48-pack-year cigarette smoking history. He takes atorvastatin, hydrochlorothiazide, lisinopril, labetalol, and metformin. His blood pressure is 132/82 mm Hg, the pulse is 72/min, and the respiratory rate is 15/min. All cranial nerves are intact. Muscle strength is reduced in the upper limbs (4/5 bilaterally) but normal in the lower limbs. Perception of sharp stimuli and temperature is reduced on his shoulders and upper arms. The vibratory sense is preserved. Sensory examination is normal in the lower limbs. What is the most likely diagnosis?
- A. Anterior cord syndrome
- B. Central cord syndrome (Correct Answer)
- C. Guillain-Barre syndrome
- D. Vitamin B12 deficiency
- E. Pontine infarction
Thoracic dermatomes and myotomes Explanation: ***Central cord syndrome***
- This syndrome typically results from a **hyperextension injury** in patients with pre-existing cervical spinal stenosis, leading to damage to the central gray matter and surrounding tracts.
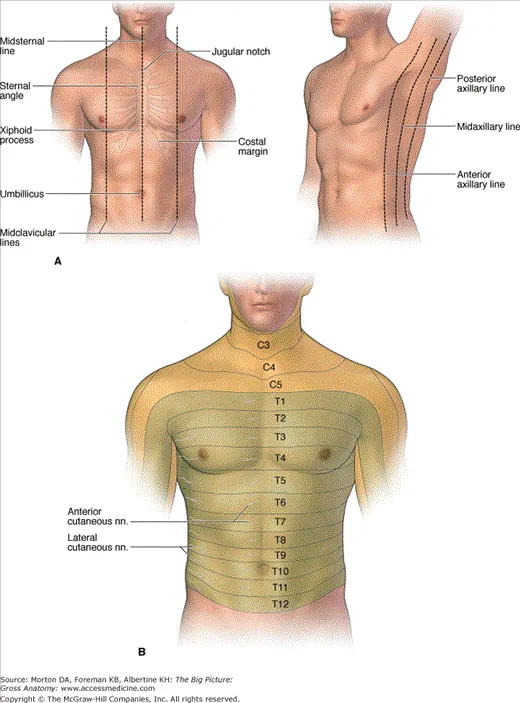
- It classically presents with greater **motor weakness in the upper extremities** than in the lower extremities, and a **"cape-like" distribution of sensory loss** (impaired pain and temperature sensation) over the shoulders and arms due to spinothalamic tract involvement, as seen in this patient.
*Anterior cord syndrome*
- This syndrome is characterized by **paraplegia/quadriplegia**, dissociated sensory loss (loss of **pain and temperature sensation**), and bowel/bladder dysfunction below the level of the lesion.
- It spares **proprioception and vibratory sensation** since the posterior columns remain intact, which is not fully consistent with the patient's presentation of primarily sensory symptoms in the upper limbs with normal strength.
*Guillain-Barre syndrome*
- This is an **acute demyelinating polyneuropathy** that typically presents with **progressive, ascending weakness** and often **areflexia**, usually following an infection.
- The patient's symptoms are primarily sensory, descending, and lack significant weakness or preceding infection, making this diagnosis less likely.
*Vitamin B12 deficiency*
- This deficiency can cause **subacute combined degeneration** of the spinal cord, affecting the **posterior columns** (vibratory and proprioception loss) and **corticospinal tracts** (weakness, spasticity).
- The patient primarily has loss of pain and temperature sensation with preserved vibratory sense and normal strength, which is inconsistent with B12 deficiency.
*Pontine infarction*
- A pontine infarction would present with a constellation of cranial nerve deficits, motor weakness (hemiparesis or quadriplegia), and cerebellar signs due to its location in the brainstem.
- The patient has intact cranial nerves, normal muscle strength, and specific sensory deficits limited to the shoulders and arms, which does not align with a brainstem stroke.
Thoracic dermatomes and myotomes US Medical PG Question 2: A healthy 22-year-old male participates in a research study you are leading to compare the properties of skeletal and cardiac muscle. You conduct a 3-phased experiment with the participant. In the first phase, you get him to lift up a 2.3 kg (5 lb) weight off a table with his left hand. In the second phase, you get him to do 20 burpees, taking his heart rate to 150/min. In the third phase, you electrically stimulate his gastrocnemius with a frequency of 50 Hz. You are interested in the tension and electrical activity of specific muscles as follows: Biceps in phase 1, cardiac muscle in phase 2, and gastrocnemius in phase 3. What would you expect to be happening in the phases and the respective muscles of interest?
- A. Increase of tension in experiments 2 and 3, with the same underlying mechanism
- B. Increase of tension in all phases (Correct Answer)
- C. Recruitment of large motor units followed by small motor units in experiment 1
- D. Fused tetanic contraction at the end of all three experiments
- E. Recruitment of small motor units at the start of experiments 1 and 2
Thoracic dermatomes and myotomes Explanation: ***Increase of tension in all phases***
- In **phase 1**, lifting a 2.3 kg weight requires the **biceps** to contract, generating sufficient force (**tension**) to overcome gravity.
- In **phase 2**, the **cardiac muscle** increases its contractile force (**tension**) to meet the metabolic demands of **exercise**, leading to a heart rate of 150/min.
- In **phase 3**, electrical stimulation of the **gastrocnemius** at 50 Hz triggers muscle contraction, leading to an increase in **tension**.
*Increase of tension in experiments 2 and 3, with the same underlying mechanism*
- While tension increases in phases 2 and 3, the **underlying mechanisms differ**: cardiac muscle tension increases due to increased sympathetic stimulation and preload, while skeletal muscle tension increases due to unfused or fused tetanus from electrical stimulation.
- Cardiac muscle contraction is regulated by **calcium-induced calcium release**, while skeletal muscle involves direct coupling of DHP receptor and ryanodine receptor.
*Recruitment of large motor units followed by small motor units in experiment 1*
- **Motor unit recruitment** follows the **size principle**, meaning smaller, more easily excitable motor units are activated first, followed by larger ones as more force is needed.
- Therefore, in phase 1, **small motor units** would be recruited first, not large ones.
*Fused tetanic contraction at the end of all three experiments*
- **Fused tetanic contraction** occurs in **skeletal muscle** when stimulation frequency is high enough that individual twitches summate completely, leading to sustained contraction.
- This phenomenon is **not possible in cardiac muscle** due to its long **refractory period**, which prevents sustained contraction and allows for adequate filling time.
*Recruitment of small motor units at the start of experiments 1 and 2*
- **Motor unit recruitment** applies to **skeletal muscle** (phase 1) and involves recruiting small motor units first for fine or gentle movements.
- **Cardiac muscle** (phase 2) does not have motor units; instead, it relies on the **Frank-Starling mechanism** and hormonal/nervous regulation to adjust its contractile force as a syncytium.
Thoracic dermatomes and myotomes US Medical PG Question 3: A 25-year-old man comes to the physician for severe back pain. He describes the pain as shooting and stabbing. On a 10-point scale, he rates the pain as a 9 to 10. The pain started after he lifted a heavy box at work; he works at a supermarket and recently switched from being a cashier to a storekeeper. The patient appears to be in severe distress. Vital signs are within normal limits. On physical examination, the spine is nontender without paravertebral muscle spasms. Range of motion is normal. A straight-leg raise test is negative. After the physical examination has been completed, the patient asks for a letter to his employer attesting to his inability to work as a storekeeper. Which of the following is the most appropriate response?
- A. “Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”
- B. You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing.
- C. I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job. (Correct Answer)
- D. The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional.
- E. The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy.
Thoracic dermatomes and myotomes Explanation: ***"I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job."***
- This response acknowledges the patient's reported discomfort while gently highlighting the **discrepancy between symptoms and objective findings**, which is crucial in cases of suspected **somatoform or functional pain**.
- It also opens communication about potential **psychosocial stressors** related to his job change, which could be contributing to his symptoms, without dismissing his pain or making a premature diagnosis.
*"You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing."*
- While this option correctly identifies the lack of physical findings, it can be perceived as dismissive of the patient's pain, potentially damaging the **physician-patient relationship**.
- Suggesting regular meetings without a clear plan for addressing his immediate concerns or exploring underlying issues might not be the most effective initial approach.
*“Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”*
- This response would **validate the patient's claim of severe pain** without objective evidence, potentially reinforcing illness behavior and avoiding addressing the underlying issue.
- Providing a doctor's note for inability to work without a clear diagnostic basis or understanding of the pain's origin is **medically inappropriate** and could set a precedent for future such requests.
*"The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional."*
- Directly labeling the problem as "psychological" can be **stigmatizing and alienating** to the patient, leading to distrust and resistance to care.
- While a psychological component might be present, immediately referring to mental health without further exploration of the patient's situation or current stressors is premature and lacks empathy.
*"The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy."*
- Similar to the previous option, explicitly stating a "psychological problem" can be **stigmatizing**.
- Jumping directly to recommending **cognitive-behavioral therapy (CBT)** without a comprehensive discussion and patient buy-in is premature and may lead to non-compliance.
Thoracic dermatomes and myotomes US Medical PG Question 4: A 51-year-old woman comes to the physician because of a 1-year history of occasional discoloration and tingling in her fingers. She has no history of major medical illness and takes no medications. Examination of the hands and fingers shows thickened, waxy skin and several firm white nodules on the fingertips. Further evaluation of this patient is most likely to show which of the following findings?
- A. Interstitial lung disease
- B. Upper eyelid rash
- C. Serositis
- D. Telangiectasia (Correct Answer)
- E. Endocardial immune complex deposition
Thoracic dermatomes and myotomes Explanation: ***Telangiectasia***
- This patient's symptoms (Raynaud phenomenon, thickened waxy skin, firm white nodules suggesting **calcinosis cutis**) are indicative of **CREST syndrome**, a limited form of systemic sclerosis.
- **Telangiectasias** (spider veins) are a common component of CREST syndrome, along with **Calcinosis**, **Raynaud phenomenon**, Esophageal dysmotility, and Sclerodactyly.
*Interstitial lung disease*
- While **interstitial lung disease** can occur in systemic sclerosis, it is more commonly associated with the **diffuse cutaneous form**, which typically presents with wider skin involvement and more severe internal organ disease.
- The patient's presentation with localized skin changes and classic CREST features makes telangiectasia a more direct and expected finding.
*Upper eyelid rash*
- An **upper eyelid rash**, specifically a **heliotrope rash**, is characteristic of **dermatomyositis**, a different connective tissue disease.
- The other symptoms described (Raynaud's, calcinosis, sclerodactyly) do not align with dermatomyositis.
*Serositis*
- **Serositis**, inflammation of the serous membranes (e.g., pleuritis, pericarditis), is a common manifestation of **systemic lupus erythematosus (SLE)**.
- The clinical picture of Raynaud's phenomenon, waxy skin, and calcinosis is not typical for SLE and points more strongly to systemic sclerosis.
*Endocardial immune complex deposition*
- **Endocardial immune complex deposition** is a hallmark of **Libman-Sacks endocarditis**, a non-infectious endocarditis primarily associated with **systemic lupus erythematosus (SLE)**.
- The patient's symptoms are inconsistent with SLE and more characteristic of systemic sclerosis.
Thoracic dermatomes and myotomes US Medical PG Question 5: A 54-year-old man comes to the emergency department because of a 3-week history of intermittent swelling of his left arm and feeling of fullness in his head that is exacerbated by lying down and bending over to tie his shoes. Physical examination shows left-sided facial edema and distention of superficial veins in the neck and left chest wall. Which of the following is the most likely cause of this patient's symptoms?
- A. Cervical rib
- B. Mediastinal lymphoma
- C. Subclavian steal syndrome
- D. Apical lung tumor (Correct Answer)
- E. Right heart failure
Thoracic dermatomes and myotomes Explanation: ***Apical lung tumor***
- The symptoms of **facial edema**, **neck vein distention**, and **swelling of the left arm**, particularly when exacerbated by positional changes such as lying down or bending over, are classic signs of **superior vena cava (SVC) syndrome**.
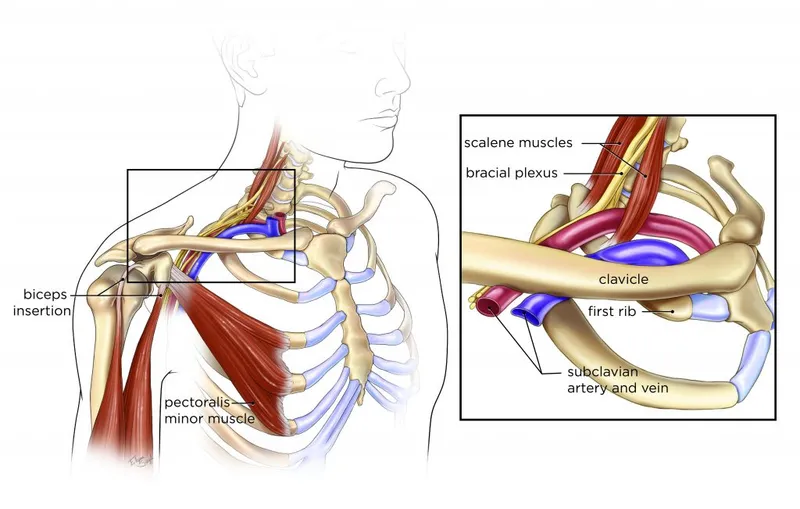
- An **apical lung tumor (Pancoast tumor)** is a common cause of SVC syndrome due to its proximity to the SVC and surrounding structures, leading to compression.
- The **left-sided predominance** (left arm swelling, left facial edema, left chest wall venous distention) specifically points to a left apical mass compressing the left brachiocephalic vein and/or SVC.
*Cervical rib*
- A cervical rib can cause **thoracic outlet syndrome**, leading to neurovascular compression, but it typically presents with neurological symptoms (pain, numbness, weakness in the arm/hand) or arterial insufficiency rather than widespread facial and neck edema.
- While it can cause *venous compression*, resulting in arm swelling, the **facial edema and neck vein distention** suggest a more central venous obstruction like SVC syndrome rather than peripheral thoracic outlet compression.
*Mediastinal lymphoma*
- Malignancies in the mediastinum, such as lymphoma, can indeed cause SVC syndrome by compressing the SVC.
- However, mediastinal lymphomas typically cause **bilateral** symptoms due to their central location, whereas this patient has **predominant left-sided findings** (left arm swelling, left facial edema, left chest wall veins), which more specifically suggests a left apical lung mass.
- Additionally, lymphoma commonly presents with systemic "B symptoms" (fever, night sweats, weight loss) and generalized lymphadenopathy, which are not mentioned here.
*Subclavian steal syndrome*
- This syndrome results from **subclavian artery stenosis** proximal to the vertebral artery origin, causing **retrograde blood flow** in the vertebral artery to supply the arm.
- It presents with **arm claudication**, dizziness, and syncope, especially with arm exercise, rather than venous congestion and swelling of the face, neck, and arm.
- This is an **arterial** syndrome, not a **venous** syndrome.
*Right heart failure*
- **Right heart failure** causes systemic venous congestion, leading to symptoms like **peripheral edema** (especially in the lower extremities), **jugular venous distention**, and **hepatomegaly**.
- While it can cause jugular venous distension, it typically presents with **bilateral lower extremity edema** and *rarely* causes unilateral arm swelling or predominant facial edema, as seen here.
- The **positional exacerbation** and **unilateral left-sided findings** are not characteristic of right heart failure.
Thoracic dermatomes and myotomes US Medical PG Question 6: A 55-year-old male bodybuilder presents to the emergency department with weakness of his right arm. The patient states he has experienced these symptoms for a few weeks; however, today his hand felt so weak he dropped his cup of tea. The patient has a past medical history of diabetes. He drinks 2-7 alcoholic drinks per day and has smoked 2 packs of cigarettes per day since he was 25. The patient admits to using anabolic steroids. He has lost 17 pounds since he last came to the emergency department 1 month ago. His temperature is 99.5°F (37.5°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam reveals decreased sensation in the right arm and 2/5 strength in the right arm and 5/5 strength in the left arm. The patient states that he is experiencing a dull aching and burning pain in his right arm during the exam. Which of the following is the most likely diagnosis?
- A. Brachial plexopathy
- B. Apical lung tumor (Correct Answer)
- C. Subclavian steal syndrome
- D. Cerebral infarction
- E. Scalenus anticus syndrome
Thoracic dermatomes and myotomes Explanation: ***Apical lung tumor***
- The patient's history of **heavy smoking** and **anabolic steroid use**, along with **unexplained weight loss**, **weakness**, and **sensory deficits in the arm**, are highly suggestive of an apical lung tumor (Pancoast tumor) compressing the brachial plexus.
- The **dull aching and burning pain** in the arm is a classic symptom of brachial plexus involvement caused by tumor invasion.
*Brachial plexopathy*
- While brachial plexopathy explains the **arm weakness and sensory changes**, it is a general term and doesn't identify the underlying cause.
- The patient's risk factors (smoking, weight loss) point to a more specific etiology than just idiopathic plexopathy.
*Subclavian steal syndrome*
- This condition involves **vertebrobasilar insufficiency** due to subclavian artery stenosis, typically presenting with neurologic symptoms like vertigo, syncope, and arm claudication, especially during arm exercise.
- It does not typically cause **unilateral arm weakness and sensory deficits** associated with unexplained weight loss.
*Cerebral infarction*
- A cerebral infarction (stroke) would cause **sudden-onset neurological deficits**, which is inconsistent with the patient's several weeks of symptoms progressing to severe weakness.
- While it can cause hemiparesis, the presentation of **dull aching and burning pain** in the arm suggests peripheral nerve involvement rather than a central lesion.
*Scalenus anticus syndrome*
- Also known as **thoracic outlet syndrome**, this typically involves compression of the brachial plexus or subclavian vessels, often due to anatomical variations or trauma.
- While it can cause arm pain and weakness, the patient's significant **smoking history** and **unexplained weight loss** strongly point to a more serious underlying malignancy.
Thoracic dermatomes and myotomes US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Thoracic dermatomes and myotomes Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Thoracic dermatomes and myotomes US Medical PG Question 8: You are seeing an otherwise healthy 66-year-old male in clinic who is complaining of localized back pain and a new rash. On physical exam, his vital signs are within normal limits. You note a vesicular rash restricted to the upper left side of his back. In order to confirm your suspected diagnosis, you perform a diagnostic test. What would you expect to find on the diagnostic test that was performed?
- A. Gram negative bacilli
- B. Branching pseudohyphae
- C. Pear shaped motile cells
- D. Multinucleated giant cells (Correct Answer)
- E. Gram positive cocci
Thoracic dermatomes and myotomes Explanation: ***Multinucleated giant cells***
- The patient's presentation of a **unilateral, vesicular rash** in an older adult, along with localized back pain, is highly suggestive of **herpes zoster (shingles)**.
- A Tzanck smear, a common diagnostic test for vesicular lesions, would reveal **multinucleated giant cells** and **intranuclear inclusions**, characteristic cytopathic effects of herpesviruses like VZV.
*Gram negative bacilli*
- This finding would suggest a **bacterial infection**, typically not associated with vesicular rashes like shingles.
- Gram-negative bacilli are often implicated in conditions such as **urinary tract infections** or **sepsis**, not dermatological viral infections.
*Branching pseudohyphae*
- This microscopic feature is characteristic of **fungal infections**, specifically **Candida species**, which present as a candidiasis rash, not a dermatomal vesicular rash.
- Fungal rashes are typically erythematous and can be pruritic but do not usually form discrete vesicles in a dermatomal distribution.
*Pear shaped motile cells*
- This describes **Trichomonas vaginalis**, a parasite causing sexually transmitted infections, primarily **vaginitis** or **urethritis**.
- This finding would be completely unrelated to a vesicular skin rash or the suspected diagnosis of shingles.
*Gram positive cocci*
- This finding is indicative of a **bacterial infection**, such as those caused by **Staphylococcus aureus** or **Streptococcus pyogenes**.
- While these bacteria can cause skin infections (e.g., impetigo, cellulitis), they do not produce the classic unilateral vesicular rash of shingles and would not involve multinucleated giant cells on microscopy.
Thoracic dermatomes and myotomes US Medical PG Question 9: A 59-year-old woman presents to the emergency room with severe low back pain. She reports pain radiating down her left leg into her left foot. She also reports intermittent severe lower back spasms. The pain started after lifting multiple heavy boxes at her work as a grocery store clerk. She denies bowel or bladder dysfunction. Her past medical history is notable for osteoporosis and endometrial cancer. She underwent a hysterectomy 20 years earlier. She takes alendronate. Her temperature is 99°F (37.2°C), blood pressure is 135/85 mmHg, pulse is 85/min, and respirations are 22/min. Her BMI is 21 kg/m^2. On exam, she is unable to bend over due to pain. Her movements are slowed to prevent exacerbating her muscle spasms. A straight leg raise elicits severe radiating pain into her left lower extremity. The patient reports that the pain is worst along the posterior thigh and posterolateral leg into the fourth and fifth toes. Palpation along the lumbar vertebral spines demonstrates mild tenderness. Patellar reflexes are 2+ bilaterally. The Achilles reflex is decreased on the left. Which nerve root is most likely affected in this patient?
- A. L5
- B. S2
- C. L3
- D. L4
- E. S1 (Correct Answer)
Thoracic dermatomes and myotomes Explanation: ***S1***
- Pain radiating to the **posterior thigh**, **posterolateral leg**, and into the **fourth and fifth toes** is characteristic of **S1 dermatome involvement**.
- A **decreased Achilles reflex** (ankle jerk reflex) specifically points to compromise of the **S1 nerve root**.
*L5*
- **L5 radiculopathy** typically causes pain and sensory deficits in the **dorsum of the foot** and into the **first, second, and third toes**.
- Motor weakness often affects **foot dorsiflexion** and **toe extension**, not primarily the Achilles reflex.
*S2*
- **S2 radiculopathy** would primarily affect sensation along the **posterior thigh** and **calf**, with possible involvement of the **plantar aspect of the foot**.
- It does not typically cause a decrease in the **Achilles reflex**, which is predominantly S1.
*L3*
- **L3 radiculopathy** typically presents with pain and sensory changes along the **anterior thigh** and possibly the **medial knee**.
- It can affect the **patellar reflex**, which is intact in this patient, and does not cause pain in the posterior leg or foot.
*L4*
- **L4 radiculopathy** typically causes pain and sensory changes over the **anterior thigh**, **medial leg**, and potentially the **medial malleolus**.
- It often presents with weakness in **quadriceps muscle** and can cause a diminished **patellar reflex**, which is normal in this patient.
Thoracic dermatomes and myotomes US Medical PG Question 10: A 32-year-old man comes to the physician because of episodic tingling and numbness in his right hand for the past 3 months. His symptoms are worse in the evening. There is no history of trauma. He is employed as a carpenter. He has smoked 1 pack of cigarettes daily for the past 10 years. He drinks a pint of vodka daily. He does not use illicit drugs. His vital signs are within normal limits. Physical examination shows decreased pinch strength in the right hand. Sensations are decreased over the little finger and both the dorsal and palmar surfaces of the medial aspect of the right hand. Which of the following is the most likely site of nerve compression?
- A. Guyon canal
- B. Quadrilateral space
- C. Carpal tunnel
- D. Cubital tunnel (Correct Answer)
- E. Radial groove
Thoracic dermatomes and myotomes Explanation: ***Cubital tunnel***
- Compression of the **ulnar nerve** at the cubital tunnel typically presents with paresthesias and numbness in the **little finger** and medial half of the ring finger, along with weakness in **intrinsic hand muscles** (decreased pinch strength).
- The carpenter's occupation may involve repetitive elbow flexion, exacerbating **ulnar nerve compression** at the elbow.
*Guyon canal*
- Compression in the **Guyon canal** affects the **ulnar nerve** at the wrist.
- While it can cause similar sensory and motor deficits in the hand, the cubital tunnel is a more common site of compression for the ulnar nerve, and symptoms worsen with **elbow flexion**.
*Carpal tunnel*
- **Carpal tunnel syndrome** involves compression of the **median nerve** and causes numbness and tingling in the thumb, index, middle, and radial half of the ring finger, sparing the little finger.
- It does not cause decreased sensation over the **little finger**.
*Quadrilateral space*
- **Quadrilateral space syndrome** involves compression of the **axillary nerve** and presents with shoulder pain, paresthesias over the lateral shoulder, and weakness in abduction and external rotation.
- This does not align with the patient's hand symptoms.
*Radial groove*
- Compression of the **radial nerve** in the radial groove (spiral groove) of the humerus typically results in **wrist drop**, weakness in forearm and hand extensors, and sensory loss over the dorsum of the hand, not the ulnar distribution described.
- This is not consistent with the patient's sensory and motor deficits.
More Thoracic dermatomes and myotomes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.