Sensory testing of dermatomes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sensory testing of dermatomes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
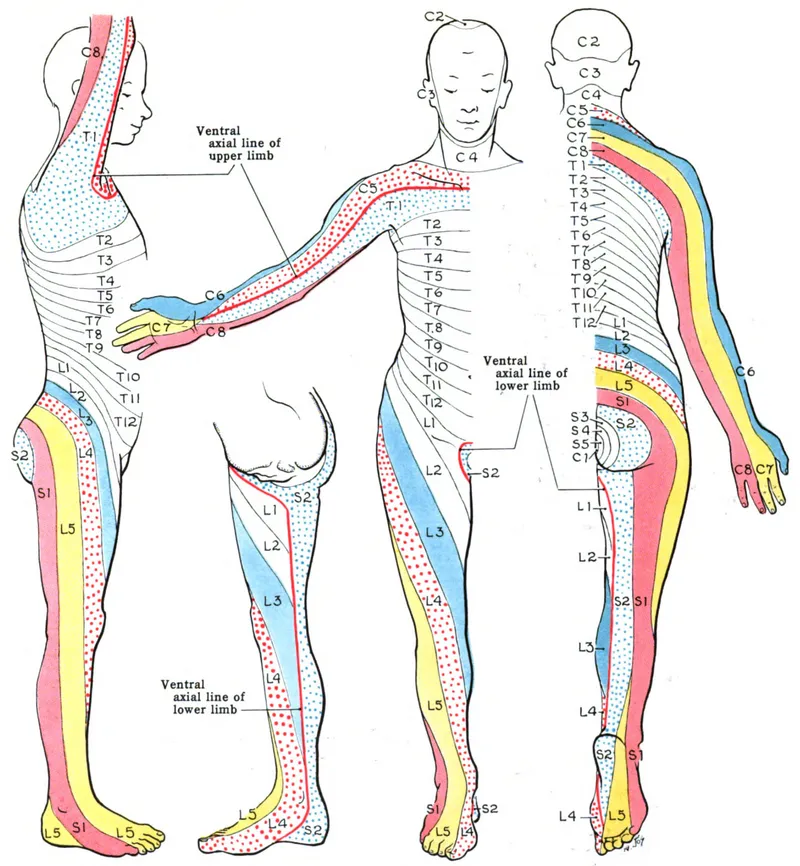
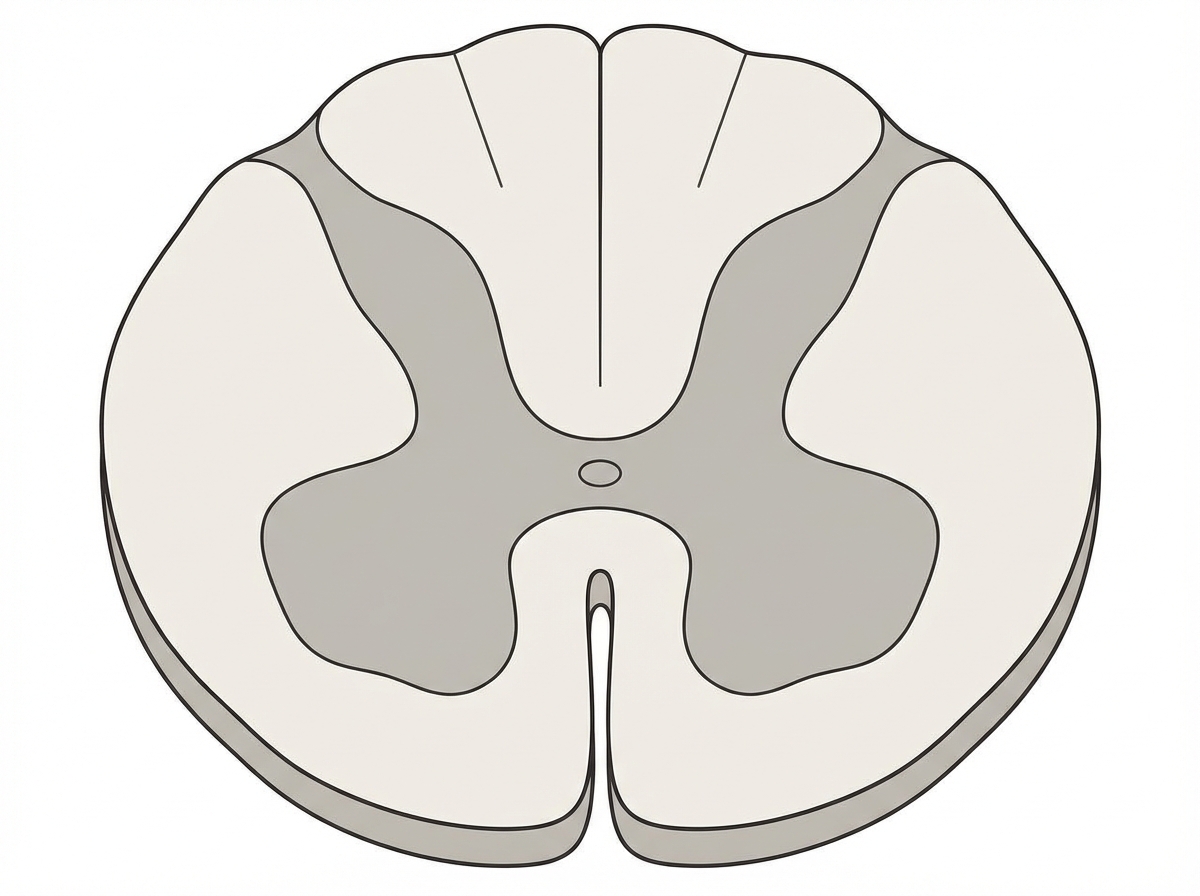
Sensory testing of dermatomes US Medical PG Question 1: A 45-year-old man is brought to the emergency department by ambulance after a motor vehicle collision. He is not responsive to verbal commands and is unable to provide any history. His pulse is 108/min and regular. Physical examination shows ecchymoses over the neck and back. Neurological examination indicates damage to the spinal cord at the level shown in the illustration. This patient's injury is most likely located at which of the following levels of the spinal cord?
- A. C2
- B. S2
- C. L4
- D. T6 (Correct Answer)
- E. S4
Sensory testing of dermatomes Explanation: ***T6***
- The correct answer depends on identifying the spinal cord level shown in the illustration (cross-sectional anatomy).
- Injury at **T6** (mid-thoracic level) can present with:
- **Paraplegia** with loss of lower extremity function
- **Sensory level** at approximately the xiphoid process (T6 dermatome)
- Risk of **autonomic dysreflexia** if injury is complete (occurs with injuries at or above T6)
- Preserved upper extremity function and respiratory capacity
- The mid-thoracic spinal cord cross-section would show the characteristic butterfly-shaped gray matter with surrounding white matter tracts.
*C2*
- **C2** injury is a high cervical lesion that would result in:
- **Quadriplegia** (tetraplegia) affecting all four extremities
- Severe **respiratory compromise** requiring mechanical ventilation (phrenic nerve C3-C5)
- High mortality if untreated
- Cross-sectional anatomy at C2 shows enlarged gray matter for upper limb innervation.
*S2*
- **S2** injury is at the level of the conus medullaris/cauda equina and would cause:
- **Bowel and bladder dysfunction** (loss of parasympathetic control)
- **Saddle anesthesia** (loss of perineal sensation)
- Possible lower extremity weakness
- No significant autonomic instability
- Would not explain the clinical presentation in the upper body.
*L4*
- **L4** injury affects the lumbar enlargement and would cause:
- **Lower extremity weakness** (quadriceps, tibialis anterior)
- **Diminished patellar reflex**
- Sensory loss in the medial leg and foot
- Bowel/bladder may be affected
- Cross-section shows prominent gray matter for lower limb innervation.
*S4*
- **S4** is the lowest sacral level and injury would cause:
- Very limited dysfunction: **anal sphincter weakness**
- **Loss of anocutaneous reflex**
- Minimal motor or sensory deficits elsewhere
- Would not cause systemic neurological compromise.
Sensory testing of dermatomes US Medical PG Question 2: A 25-year-old woman comes to the physician because of pain and weakness in her right forearm and hand for several months. Two years ago, she sustained a fracture of her ulnar shaft with dislocation of the radial head that was treated surgically. Physical examination shows mild tenderness a few centimeters distal to the lateral epicondyle. She has marked weakness when attempting to extend her right middle finger. There is radial deviation on extension of the wrist. Sensation is not impaired. Which of the following nerves is most likely affected in this patient?
- A. Ulnar nerve
- B. Musculocutaneous nerve
- C. Posterior interosseous nerve (Correct Answer)
- D. Superficial radial nerve
- E. Anterior interosseous nerve
Sensory testing of dermatomes Explanation: ***Posterior interosseous nerve***
- The symptoms, including weakness in **middle finger extension** and **radial deviation of the wrist on extension**, are classic signs of **posterior interosseous nerve** (PIN) palsy. This nerve primarily innervates the muscles responsible for **finger and thumb extension**, as well as **extensor carpi ulnaris** (ECU) for wrist extension.
- The **radial deviation on wrist extension** occurs because the radial-sided wrist extensors (**extensor carpi radialis longus** and **brevis**) are innervated by the **radial nerve proper** before it branches into PIN, so they remain intact. With loss of ECU (ulnar-sided wrist extensor), unopposed action of ECRL and ECRB causes radial deviation.
- PIN palsy can result from **trauma** or compression, and the patient's history of a **radial head dislocation** two years prior is a significant risk factor for nerve damage in this region, particularly as PIN passes through the **supinator muscle** (arcade of Frohse). Tenderness distal to the **lateral epicondyle** also points to the region where PIN can be compressed.
*Ulnar nerve*
- An **ulnar nerve** injury would primarily cause weakness in **finger adduction and abduction** (especially the little finger and ring finger), **flexion of the ulnar half of the profundus**, and **intrinsic hand muscles**, leading to a "claw hand" deformity if severe.
- Sensation would also be affected in the **palmar and dorsal aspects of the 5th digit** and the **medial half of the 4th digit**, which is not described.
*Musculocutaneous nerve*
- The **musculocutaneous nerve** primarily innervates the **biceps brachii** and **brachialis muscles**, responsible for **elbow flexion** and **forearm supination**.
- Sensory deficits would be noted on the **lateral forearm**, none of which align with the patient's symptoms.
*Superficial radial nerve*
- The **superficial radial nerve** is purely sensory and provides sensation to the **dorsum of the hand** and parts of the thumb, index, and middle fingers.
- It does not have any motor function, so motor weakness would not be a symptom of its injury.
*Anterior interosseous nerve*
- The **anterior interosseous nerve** (AIN) is a purely motor branch of the median nerve, responsible for innervating the **flexor pollicis longus**, **flexor digitorum profundus (index and middle fingers)**, and **pronator quadratus**.
- Injury to the AIN would result in an inability to form an "OK" sign (due to impaired flexion of the thumb IP joint and index finger DIP joint) and no sensory loss.
Sensory testing of dermatomes US Medical PG Question 3: A 30-year-old man presents with weakness in his right hand. He says he has been an avid cyclist since the age of 20. He denies any recent trauma. Physical examination reveals decreased sensations over the 4th and 5th digits with difficulty extending the 4th and 5th digits. Strength is 4 out of 5 in the extensor muscles of the right hand and wrist. When the patient is asked to extend his fingers, the result is shown in the image. Which of the following nerves is most likely damaged in this patient?
- A. Median nerve
- B. Musculocutaneous nerve
- C. Axillary nerve
- D. Ulnar nerve (Correct Answer)
- E. Radial nerve
Sensory testing of dermatomes Explanation: ***Ulnar nerve***
- The symptoms, including weakness in the **right hand**, decreased sensation over the **4th and 5th digits**, and difficulty extending the 4th and 5th digits (which suggests **ulnar claw**), are characteristic of **ulnar nerve damage**.
- **Avid cycling** can lead to compression of the ulnar nerve in the **Guyon's canal** (handlebar palsy) or at the **cubital tunnel** in the elbow, causing these specific signs.
*Median nerve*
- Damage to the median nerve typically affects the **thumb**, **index**, **middle finger**, and radial half of the ring finger, causing **ape hand deformity** or **carpal tunnel syndrome**.
- It controls movements like **thumb opposition** and **flexion of the first three digits**, which are not primarily described as impaired here.
*Musculocutaneous nerve*
- This nerve primarily innervates the **biceps brachii**, **brachialis**, and **coracobrachialis muscles**, affecting **elbow flexion** and **forearm supination**.
- It provides sensory innervation to the **lateral forearm**, symptoms not consistent with this patient's presentation.
*Axillary nerve*
- Damage to the axillary nerve results in weakness of the **deltoid** and **teres minor muscles**, leading to impaired **shoulder abduction** and external rotation.
- Sensory loss would be over the **lateral aspect of the shoulder**, which is unrelated to the described hand symptoms.
*Radial nerve*
- Radial nerve damage typically results in **wrist drop** and impaired **extension of the fingers and thumb** due to innervation of the extensors.
- While there is difficulty extending the 4th and 5th digits, the sensory loss pattern (4th and 5th digits) and specific **ulnar claw** appearance are more indicative of ulnar nerve involvement.
Sensory testing of dermatomes US Medical PG Question 4: A 51-year-old woman comes to the physician because of progressively worsening lower back pain. The pain radiates down the right leg to the lateral side of the foot. She has had no trauma, urinary incontinence, or fever. An MRI of the lumbar spine shows disc degeneration and herniation at the level of L5–S1. Which of the following is the most likely finding on physical examination?
- A. Difficulty walking on heels
- B. Exaggerated patellar tendon reflex
- C. Diminished sensation of the anus and genitalia
- D. Diminished sensation of the anterior lateral thigh
- E. Weak Achilles tendon reflex (Correct Answer)
Sensory testing of dermatomes Explanation: ***Weak Achilles tendon reflex***
- A herniated disc at **L5-S1** typically compresses the **S1 nerve root**, which is responsible for the **Achilles tendon reflex**.
- **S1 radiculopathy** presents with weakness in plantarflexion, diminished or absent Achilles reflex, and sensory loss in the **lateral foot** (matching the patient's symptoms).
*Difficulty walking on heels*
- Difficulty walking on heels (**dorsiflexion weakness**) is primarily associated with **L4-L5 disc herniation** compressing the **L5 nerve root**.
- This symptom indicates **L5 radiculopathy**, which affects the tibialis anterior muscle, not S1.
*Exaggerated patellar tendon reflex*
- An exaggerated patellar tendon reflex (**hyperreflexia**) indicates an **upper motor neuron lesion** or spinal cord compression above the lumbar region.
- A disc herniation at **L5-S1** causes a **lower motor neuron lesion** with diminished reflexes, not hyperreflexia.
*Diminished sensation of the anus and genitalia*
- This symptom, along with urinary incontinence and saddle anesthesia, is characteristic of **cauda equina syndrome**, a surgical emergency.
- The patient lacks urinary incontinence and the specific unilateral pain pattern points to isolated **S1 radiculopathy**, not cauda equina syndrome.
*Diminished sensation of the anterior lateral thigh*
- Sensory loss in the **anterior lateral thigh** is associated with compression of the **lateral femoral cutaneous nerve** or **L2-L4 nerve roots**.
- This pattern is not consistent with **L5-S1 disc herniation**, which causes sensory changes in the lateral foot and posterior leg.
Sensory testing of dermatomes US Medical PG Question 5: A 29-year-old woman presents to the primary care office for a recent history of falls. She has fallen 5 times over the last year. These falls are not associated with any preceding symptoms; she specifically denies dizziness, lightheadedness, or visual changes. However, she has started noticing that both of her legs feel weak. She's also noticed that her carpet feels strange beneath her bare feet. Her mother and grandmother have a history of similar problems. On physical exam, she has notable leg and foot muscular atrophy and 4/5 strength throughout her bilateral lower extremities. Sensation to light touch and pinprick is decreased up to the mid-calf. Ankle jerk reflex is absent bilaterally. Which of the following is the next best diagnostic test for this patient?
- A. MRI brain
- B. Ankle-brachial index
- C. Electromyography (including nerve conduction studies) (Correct Answer)
- D. Lumbar puncture
- E. Hemoglobin A1c
Sensory testing of dermatomes Explanation: ***Electromyography (including nerve conduction studies)***
- The patient's symptoms of **progressive weakness**, **sensory deficits** (carpet feels strange, decreased sensation up to mid-calf), **muscular atrophy**, and **absent ankle reflexes**, along with a **family history**, are highly suggestive of a **hereditary peripheral neuropathy** (e.g., Charcot-Marie-Tooth disease).
- **Electromyography (EMG)** and **nerve conduction studies (NCS)** are essential for confirming peripheral neuropathy, differentiating between demyelinating and axonal involvement, and localizing the lesion.
*MRI brain*
- An MRI brain would be indicated for central nervous system pathology, but the patient's symptoms (distal weakness, sensory loss with a "stocking-glove" distribution, absent reflexes) are highly suggestive of a **peripheral neuropathy**.
- There is no indication of upper motor neuron signs or other CNS involvement to warrant a brain MRI at this stage.
*Ankle-brachial index*
- Ankle-brachial index (ABI) is used to diagnose **peripheral artery disease (PAD)**, which typically presents with claudication (pain with exertion) and ischemic changes.
- The patient's symptoms of sensory changes and progressive weakness are not characteristic of PAD.
*Lumbar puncture*
- A lumbar puncture is primarily used to analyze **cerebrospinal fluid (CSF)** for inflammatory, infectious, or neoplastic conditions affecting the CNS or nerve roots (e.g., Guillain-Barré syndrome, which has acute onset).
- Given the chronic and progressive nature of her symptoms and a positive family history, it is less likely to be an acute inflammatory process of the nerve roots.
*Hemoglobin A1c*
- Hemoglobin A1c is used to screen for or monitor **diabetes mellitus**, which can cause a **diabetic neuropathy**.
- While diabetes can cause peripheral neuropathy, the patient's young age, lack of typical diabetic risk factors, and strong family history point more strongly towards a hereditary condition. Glycemic control does not fully explain her presentation.
Sensory testing of dermatomes US Medical PG Question 6: A 72-year-old woman is brought in to the emergency department after her husband noticed that she appeared to be choking on her dinner. He performed a Heimlich maneuver but was concerned that she may have aspirated something. The patient reports a lack of pain and temperature on the right half of her face, as well as the same lack of sensation on the left side of her body. She also states that she has been feeling "unsteady" on her feet. On physical exam you note a slight ptosis on the right side. She is sent for an emergent head CT. Where is the most likely location of the neurological lesion?
- A. Pons
- B. Internal capsule
- C. Cervical spinal cord
- D. Medulla (Correct Answer)
- E. Midbrain
Sensory testing of dermatomes Explanation: ***Medulla***
- This presentation describes **Wallenberg syndrome** (lateral medullary syndrome), characterized by **ipsilateral facial sensory loss**, **contralateral body sensory loss**, and **ataxia** due to involvement of the spinothalamic tracts, trigeminal nucleus, and cerebellar pathways.
- **Dysphagia** (choking) and **Horner's syndrome** (ptosis, miosis, anhidrosis) are also classic signs, specifically the ptosis seen here, pointing to an infarct in the **lateral medulla**.
*Pons*
- Lesions in the pons typically present with varying degrees of **cranial nerve deficits** (e.g., trigeminal, abducens, facial) and **motor or sensory deficits** affecting both sides of the body due to the decussation of tracts.
- The specific combination of **crossed sensory loss** and other symptoms seen here is not characteristic of isolated pontine lesions.
*Internal capsule*
- A lesion in the internal capsule would primarily cause **contralateral motor weakness (hemiparesis)** and **sensory loss** affecting both the face and body on the same side, without the ipsilateral facial involvement.
- It would not explain the **ataxia** or specific cranial nerve signs like ptosis.
*Cervical spinal cord*
- Spinal cord lesions result in **sensory and motor deficits below the level of the lesion**, affecting both sides of the body symmetrically, or ipsilaterally depending on the tract involved.
- They do not cause **facial sensory disturbances**, **dysphagia**, or **ataxia** in the manner described.
*Midbrain*
- Midbrain lesions typically involve the **oculomotor nerve** (CN III), causing eye movement abnormalities, and can result in **contralateral hemiparesis**.
- They do not produce the **crossed sensory deficits** (ipsilateral face, contralateral body) or **ataxia** characteristic of this case.
Sensory testing of dermatomes US Medical PG Question 7: A 40-year-old woman presents with a ‘tingling’ feeling in the toes of both feet that started 5 days ago. She says that the feeling varies in intensity but has been there ever since she recovered from a stomach flu last week. Over the last 2 days, the tingling sensation has started to spread up her legs. She also reports feeling weak in the legs for the past 2 days. Her past medical history is unremarkable, and she currently takes no medications. Which of the following diagnostic tests would most likely be abnormal in this patient?
- A. Noncontrast CT of the head
- B. Serum hemoglobin concentration
- C. Nerve conduction studies (Correct Answer)
- D. Serum calcium concentration
- E. Transthoracic echocardiography
Sensory testing of dermatomes Explanation: ***Nerve conduction studies***
- The patient's ascending **motor weakness** and **sensory paresthesias** following a gastrointestinal infection are classic symptoms of **Guillain-Barré Syndrome (GBS)**, which is characterized by **demyelination** of peripheral nerves.
- **Nerve conduction studies** would reveal **markedly slowed conduction velocities**, **conduction block**, and **prolonged distal latencies**, indicating the demyelinating neuropathy characteristic of GBS.
*Noncontrast CT of the head*
- This test is primarily used to evaluate **acute neurological deficits** suggestive of stroke, hemorrhage, or mass lesions within the brain.
- The patient's symptoms are consistent with a **peripheral neuropathy** and do not suggest a central nervous system pathology.
*Serum hemoglobin concentration*
- This measures the concentration of **hemoglobin in the blood** and is used to diagnose **anemia**.
- While anemia can cause fatigue, it does not typically cause the **ascending paralysis** and **paresthesias** described, nor is it directly related to a recent stomach flu in this manner.
*Serum calcium concentration*
- This measures the level of **calcium in the blood**, which is important for muscle and nerve function.
- While extreme imbalances can cause neurological symptoms, there is no direct indication or typical association between the patient's symptoms and a primary calcium disorder.
*Transthoracic echocardiography*
- This imaging test evaluates the **structure and function of the heart**.
- The patient's symptoms are neurological and do not suggest a primary cardiac etiology or complication that would warrant an echocardiogram.
Sensory testing of dermatomes US Medical PG Question 8: A 59-year-old woman presents to the emergency room with severe low back pain. She reports pain radiating down her left leg into her left foot. She also reports intermittent severe lower back spasms. The pain started after lifting multiple heavy boxes at her work as a grocery store clerk. She denies bowel or bladder dysfunction. Her past medical history is notable for osteoporosis and endometrial cancer. She underwent a hysterectomy 20 years earlier. She takes alendronate. Her temperature is 99°F (37.2°C), blood pressure is 135/85 mmHg, pulse is 85/min, and respirations are 22/min. Her BMI is 21 kg/m^2. On exam, she is unable to bend over due to pain. Her movements are slowed to prevent exacerbating her muscle spasms. A straight leg raise elicits severe radiating pain into her left lower extremity. The patient reports that the pain is worst along the posterior thigh and posterolateral leg into the fourth and fifth toes. Palpation along the lumbar vertebral spines demonstrates mild tenderness. Patellar reflexes are 2+ bilaterally. The Achilles reflex is decreased on the left. Which nerve root is most likely affected in this patient?
- A. L5
- B. S2
- C. L3
- D. L4
- E. S1 (Correct Answer)
Sensory testing of dermatomes Explanation: ***S1***
- Pain radiating to the **posterior thigh**, **posterolateral leg**, and into the **fourth and fifth toes** is characteristic of **S1 dermatome involvement**.
- A **decreased Achilles reflex** (ankle jerk reflex) specifically points to compromise of the **S1 nerve root**.
*L5*
- **L5 radiculopathy** typically causes pain and sensory deficits in the **dorsum of the foot** and into the **first, second, and third toes**.
- Motor weakness often affects **foot dorsiflexion** and **toe extension**, not primarily the Achilles reflex.
*S2*
- **S2 radiculopathy** would primarily affect sensation along the **posterior thigh** and **calf**, with possible involvement of the **plantar aspect of the foot**.
- It does not typically cause a decrease in the **Achilles reflex**, which is predominantly S1.
*L3*
- **L3 radiculopathy** typically presents with pain and sensory changes along the **anterior thigh** and possibly the **medial knee**.
- It can affect the **patellar reflex**, which is intact in this patient, and does not cause pain in the posterior leg or foot.
*L4*
- **L4 radiculopathy** typically causes pain and sensory changes over the **anterior thigh**, **medial leg**, and potentially the **medial malleolus**.
- It often presents with weakness in **quadriceps muscle** and can cause a diminished **patellar reflex**, which is normal in this patient.
Sensory testing of dermatomes US Medical PG Question 9: A 75-year-old man comes to the physician because of a 2-week history of sharp, stabbing pain in the lower back that radiates to the back of his left leg. He also has had a loss of sensitivity around his buttocks and inner thighs as well as increased trouble urinating the last week. Two years ago, he was diagnosed with prostate cancer and was treated with radiation therapy. Neurologic examination shows reduced strength and reflexes in the left lower extremity; the right side is normal. The resting anal sphincter tone is normal but the squeeze tone is reduced. Which of the following is the most likely diagnosis?
- A. Central cord syndrome
- B. Conus medullaris syndrome
- C. Anterior spinal cord syndrome
- D. Brown-sequard syndrome
- E. Cauda equina syndrome (Correct Answer)
Sensory testing of dermatomes Explanation: ***Cauda equina syndrome***
- The patient presents with **bilateral sensory loss in the perineal region** (**saddle anesthesia**) and **new-onset urinary dysfunction** (trouble urinating, reduced squeeze tone), which are classic symptoms of cauda equina syndrome.
- The **sharp, stabbing radicular pain** radiating down the leg indicates nerve root involvement, characteristic of cauda equina rather than conus medullaris.
- The **asymmetric motor weakness** (left leg only) supports cauda equina syndrome, as compression can preferentially affect specific nerve roots, whereas conus medullaris typically causes more symmetric bilateral deficits.
- The history of **prostate cancer** and **radiation therapy** suggests a potential metastatic lesion compressing the cauda equina nerves.
*Central cord syndrome*
- This syndrome primarily affects the **upper extremities more than the lower extremities** and typically results from hyperextension injuries in older individuals.
- It often presents with **dissociated sensory loss** (loss of pain and temperature sensation) below the level of the lesion, which is not the primary complaint here.
*Conus medullaris syndrome*
- Affects the **sacral spinal cord segments (S3-S5)**, leading to **symmetrical motor and sensory deficits**, often with prominent early **bowel and bladder dysfunction**.
- While it causes saddle anesthesia and urinary symptoms, the **asymmetrical motor weakness** (left leg only) and **prominent radicular pain** extending down the leg are more characteristic of cauda equina syndrome.
- Conus lesions typically present with more **symmetric bilateral deficits** rather than the unilateral pattern seen here.
*Anterior spinal cord syndrome*
- Characterized by **bilateral motor paralysis** and **loss of pain and temperature sensation** below the lesion, with **preservation of proprioception and vibratory sensation**.
- It would not typically present with the isolated **saddle anesthesia** and **radicular pain** described in the patient.
*Brown-sequard syndrome*
- Results from a **hemicord lesion**, causing **ipsilateral motor paralysis** and loss of proprioception/vibration below the lesion, and **contralateral loss of pain and temperature sensation**.
- The patient's symptoms of **bilateral saddle anesthesia** and **bowel/bladder dysfunction** do not align with the characteristic unilateral sensory and motor presentation of Brown-Sequard syndrome.
Sensory testing of dermatomes US Medical PG Question 10: A 35-year-old woman, gravida 2, para 1, at 40 weeks' gestation, presents to the hospital with contractions spaced 2 minutes apart. Her past medical history is significant for diabetes, which she has controlled with insulin during this pregnancy. Her pregnancy has otherwise been unremarkable. A baby boy is born via a spontaneous vaginal delivery. Physical examination shows he weighs 4.5 kg (9 lb), the pulse is 140/min, the respirations are 40/min, and he has good oxygen saturation on room air. His left arm is pronated and medially rotated. He is unable to move it away from his body. The infant’s right arm functions normally and he is able to move his wrists and all 10 digits. Which of the following nerve roots were most likely damaged during delivery?
- A. C4 and C5
- B. C7 and C8
- C. C5 and C6 (Correct Answer)
- D. C8 and T1
- E. C6 and C7
Sensory testing of dermatomes Explanation: ***C5 and C6***
- The presentation of the infant's left arm being **pronated**, **medially rotated**, and unable to be moved away from the body is characteristic of **Erb-Duchenne palsy** (also called "waiter's tip" deformity).
- This condition results from damage to the **upper trunk of the brachial plexus**, specifically involving the **C5 and C6 nerve roots**.
- These roots innervate muscles responsible for **shoulder abduction** (deltoid, supraspinatus), **external rotation** (infraspinatus), and **elbow flexion/supination** (biceps brachii).
- The preserved wrist and digit function confirms the injury is limited to the upper trunk, sparing C7-T1.
*C4 and C5*
- While C5 is involved in Erb's palsy, the **C4 root** primarily contributes to the **phrenic nerve** (diaphragm innervation) and provides sensation to the neck and shoulder region.
- C4 does not significantly contribute to the brachial plexus motor function, so damage to C4 would not explain the shoulder and elbow deficits observed.
*C7 and C8*
- Damage to **C7 and C8** would primarily affect **wrist extension** (C7) and **finger flexion** (C8), not the shoulder abduction and elbow flexion deficits seen here.
- This pattern would be inconsistent with Erb's palsy and more suggestive of middle-to-lower trunk injury.
*C8 and T1*
- Injury to **C8 and T1** nerve roots causes **Klumpke's palsy**, affecting the **intrinsic hand muscles** and wrist flexors, leading to a "claw hand" deformity.
- The infant's preserved ability to move all wrists and digits rules out C8-T1 injury, as this would severely impair hand function and potentially cause **Horner's syndrome** (if T1 is involved).
*C6 and C7*
- While **C6** is involved in Erb's palsy, adding **C7** damage would extend the injury to affect **wrist extensors** (extensor carpi radialis) and **triceps** (elbow extension).
- The clinical presentation described is most consistent with isolated upper trunk (C5-C6) injury, not extended involvement of C7.
More Sensory testing of dermatomes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.