Sacral dermatomes and myotomes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sacral dermatomes and myotomes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sacral dermatomes and myotomes US Medical PG Question 1: A 68-year-old man presents to his primary care physician complaining of a bulge in his scrotum that has enlarged over the past several months. He is found to have a right-sided inguinal hernia and undergoes elective hernia repair. At his first follow-up visit, he complains of a tingling sensation on his scrotum. Which of the following nerve roots communicates with the injured tissues?
- A. S1-S3
- B. L1-L2 (Correct Answer)
- C. S2-S4
- D. L4-L5
- E. L2-L3
Sacral dermatomes and myotomes Explanation: ***L1-L2***
- The **ilioinguinal nerve** and **genitofemoral nerve**, which are commonly injured during inguinal hernia repair, arise from the **L1 and L2 spinal nerves**.
- These nerves provide sensory innervation to the **scrotum**, **inguinal region**, and **medial thigh**, explaining the patient's tingling sensation.
*S1-S3*
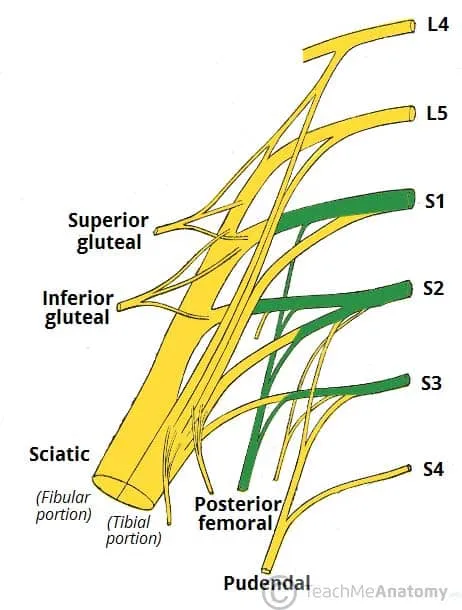
- These nerve roots typically contribute to the **sciatic nerve** and innervate the posterior thigh, leg, and foot, and are not directly involved in scrotal sensation relevant to an inguinal hernia repair.
- They also contribute to the **pudendal nerve**, which primarily supplies the perineum and external genitalia, but injury to this nerve is less common in routine inguinal hernia repair.
*S2-S4*
- These nerve roots primarily form the **pudendal nerve**, which innervates the **perineum** and external genitalia (including some scrotal sensation), but injury to these specific nerves is not a typical complication of routine inguinal hernia repair.
- They also contribute to the **pelvic splanchnic nerves**, controlling bladder and bowel function, which are unrelated to the described sensory deficit.
*L4-L5*
- These nerve roots primarily contribute to nerves supplying the **lower limb**, such as the **femoral nerve** and **sciatic nerve**, and do not directly innervate the scrotum.
- Injury to these roots would typically result in motor or sensory deficits of the **thigh and leg**, not isolated scrotal tingling.
*L2-L3*
- While L2 contributes to nerves supplying the inguinal region and scrotum (genitofemoral nerve), the **ilioinguinal nerve** originates from L1.
- The **lateral femoral cutaneous nerve**, which originates from L2-L3, innervates the **lateral thigh**, and its injury would cause tingling there, not in the scrotum.
Sacral dermatomes and myotomes US Medical PG Question 2: A 59-year-old woman presents to the emergency room with severe low back pain. She reports pain radiating down her left leg into her left foot. She also reports intermittent severe lower back spasms. The pain started after lifting multiple heavy boxes at her work as a grocery store clerk. She denies bowel or bladder dysfunction. Her past medical history is notable for osteoporosis and endometrial cancer. She underwent a hysterectomy 20 years earlier. She takes alendronate. Her temperature is 99°F (37.2°C), blood pressure is 135/85 mmHg, pulse is 85/min, and respirations are 22/min. Her BMI is 21 kg/m^2. On exam, she is unable to bend over due to pain. Her movements are slowed to prevent exacerbating her muscle spasms. A straight leg raise elicits severe radiating pain into her left lower extremity. The patient reports that the pain is worst along the posterior thigh and posterolateral leg into the fourth and fifth toes. Palpation along the lumbar vertebral spines demonstrates mild tenderness. Patellar reflexes are 2+ bilaterally. The Achilles reflex is decreased on the left. Which nerve root is most likely affected in this patient?
- A. L5
- B. S2
- C. L3
- D. L4
- E. S1 (Correct Answer)
Sacral dermatomes and myotomes Explanation: ***S1***
- Pain radiating to the **posterior thigh**, **posterolateral leg**, and into the **fourth and fifth toes** is characteristic of **S1 dermatome involvement**.
- A **decreased Achilles reflex** (ankle jerk reflex) specifically points to compromise of the **S1 nerve root**.
*L5*
- **L5 radiculopathy** typically causes pain and sensory deficits in the **dorsum of the foot** and into the **first, second, and third toes**.
- Motor weakness often affects **foot dorsiflexion** and **toe extension**, not primarily the Achilles reflex.
*S2*
- **S2 radiculopathy** would primarily affect sensation along the **posterior thigh** and **calf**, with possible involvement of the **plantar aspect of the foot**.
- It does not typically cause a decrease in the **Achilles reflex**, which is predominantly S1.
*L3*
- **L3 radiculopathy** typically presents with pain and sensory changes along the **anterior thigh** and possibly the **medial knee**.
- It can affect the **patellar reflex**, which is intact in this patient, and does not cause pain in the posterior leg or foot.
*L4*
- **L4 radiculopathy** typically causes pain and sensory changes over the **anterior thigh**, **medial leg**, and potentially the **medial malleolus**.
- It often presents with weakness in **quadriceps muscle** and can cause a diminished **patellar reflex**, which is normal in this patient.
Sacral dermatomes and myotomes US Medical PG Question 3: A 36-year-old man is seen in the emergency department for back pain that has been getting progressively worse over the last 4 days. Upon further questioning, he also notes that he has been having a tingling and burning sensation rising up from his feet to his knees bilaterally. The patient states he is having difficulty urinating and having bowel movements over the last several days. His temperature is 97.4°F (36.3°C), blood pressure is 122/80 mmHg, pulse is 85/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for weak leg flexion bilaterally along with decreased anal sphincter tone. Which of the following is the best next step in management?
- A. Emergency surgery
- B. CT
- C. Pulmonary function tests
- D. Lumbar puncture
- E. MRI (Correct Answer)
Sacral dermatomes and myotomes Explanation: ***MRI***
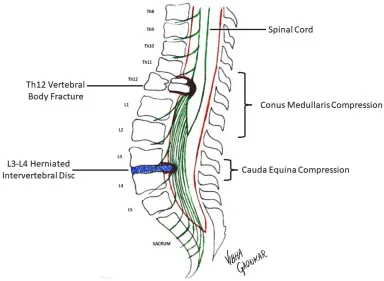
- The patient's symptoms (back pain, ascending paresthesias, bladder/bowel dysfunction, and decreased anal sphincter tone) are highly suggestive of **cauda equina syndrome**. An **MRI of the spine** is the gold standard for diagnosing this condition, as it can visualize the spinal cord and nerve roots directly.
- Early diagnosis and intervention with MRI are crucial to prevent **permanent neurological deficits** in cauda equina syndrome.
*Emergency surgery*
- While emergency surgery might be the next step *after* diagnosis, it is **not the initial diagnostic step**. The cause of the cauda equina syndrome (e.g., disc herniation, tumor) must first be identified.
- Performing surgery without proper imaging could lead to operating on the wrong level or for the wrong pathology.
*CT*
- A **CT scan** can provide information about bony structures but is generally **inferior to MRI** for visualizing soft tissue structures like the spinal cord, nerve roots, and intervertebral discs, which are critical in cauda equina syndrome.
- It may miss subtle compressions or pathologies of the nerve roots.
*Pulmonary function tests*
- **Pulmonary function tests** are used to assess lung function and are **irrelevant** to the patient's acute neurological symptoms and back pain.
- This test would not provide any diagnostic information for suspected cauda equina syndrome.
*Lumbar puncture*
- A **lumbar puncture** is primarily used to analyze cerebrospinal fluid for conditions like infection or inflammation (e.g., meningitis, Guillain-Barré syndrome).
- While Guillain-Barré can cause ascending paralysis, the prominent back pain, bowel/bladder dysfunction, and decreased anal sphincter tone make **cauda equina syndrome** a more likely diagnosis, for which LP is not the primary diagnostic tool.
Sacral dermatomes and myotomes US Medical PG Question 4: A 51-year-old woman comes to the physician because of progressively worsening lower back pain. The pain radiates down the right leg to the lateral side of the foot. She has had no trauma, urinary incontinence, or fever. An MRI of the lumbar spine shows disc degeneration and herniation at the level of L5–S1. Which of the following is the most likely finding on physical examination?
- A. Difficulty walking on heels
- B. Exaggerated patellar tendon reflex
- C. Diminished sensation of the anus and genitalia
- D. Diminished sensation of the anterior lateral thigh
- E. Weak Achilles tendon reflex (Correct Answer)
Sacral dermatomes and myotomes Explanation: ***Weak Achilles tendon reflex***
- A herniated disc at **L5-S1** typically compresses the **S1 nerve root**, which is responsible for the **Achilles tendon reflex**.
- **S1 radiculopathy** presents with weakness in plantarflexion, diminished or absent Achilles reflex, and sensory loss in the **lateral foot** (matching the patient's symptoms).
*Difficulty walking on heels*
- Difficulty walking on heels (**dorsiflexion weakness**) is primarily associated with **L4-L5 disc herniation** compressing the **L5 nerve root**.
- This symptom indicates **L5 radiculopathy**, which affects the tibialis anterior muscle, not S1.
*Exaggerated patellar tendon reflex*
- An exaggerated patellar tendon reflex (**hyperreflexia**) indicates an **upper motor neuron lesion** or spinal cord compression above the lumbar region.
- A disc herniation at **L5-S1** causes a **lower motor neuron lesion** with diminished reflexes, not hyperreflexia.
*Diminished sensation of the anus and genitalia*
- This symptom, along with urinary incontinence and saddle anesthesia, is characteristic of **cauda equina syndrome**, a surgical emergency.
- The patient lacks urinary incontinence and the specific unilateral pain pattern points to isolated **S1 radiculopathy**, not cauda equina syndrome.
*Diminished sensation of the anterior lateral thigh*
- Sensory loss in the **anterior lateral thigh** is associated with compression of the **lateral femoral cutaneous nerve** or **L2-L4 nerve roots**.
- This pattern is not consistent with **L5-S1 disc herniation**, which causes sensory changes in the lateral foot and posterior leg.
Sacral dermatomes and myotomes US Medical PG Question 5: A 75-year-old man comes to the physician because of a 2-week history of sharp, stabbing pain in the lower back that radiates to the back of his left leg. He also has had a loss of sensitivity around his buttocks and inner thighs as well as increased trouble urinating the last week. Two years ago, he was diagnosed with prostate cancer and was treated with radiation therapy. Neurologic examination shows reduced strength and reflexes in the left lower extremity; the right side is normal. The resting anal sphincter tone is normal but the squeeze tone is reduced. Which of the following is the most likely diagnosis?
- A. Central cord syndrome
- B. Conus medullaris syndrome
- C. Anterior spinal cord syndrome
- D. Brown-sequard syndrome
- E. Cauda equina syndrome (Correct Answer)
Sacral dermatomes and myotomes Explanation: ***Cauda equina syndrome***
- The patient presents with **bilateral sensory loss in the perineal region** (**saddle anesthesia**) and **new-onset urinary dysfunction** (trouble urinating, reduced squeeze tone), which are classic symptoms of cauda equina syndrome.
- The **sharp, stabbing radicular pain** radiating down the leg indicates nerve root involvement, characteristic of cauda equina rather than conus medullaris.
- The **asymmetric motor weakness** (left leg only) supports cauda equina syndrome, as compression can preferentially affect specific nerve roots, whereas conus medullaris typically causes more symmetric bilateral deficits.
- The history of **prostate cancer** and **radiation therapy** suggests a potential metastatic lesion compressing the cauda equina nerves.
*Central cord syndrome*
- This syndrome primarily affects the **upper extremities more than the lower extremities** and typically results from hyperextension injuries in older individuals.
- It often presents with **dissociated sensory loss** (loss of pain and temperature sensation) below the level of the lesion, which is not the primary complaint here.
*Conus medullaris syndrome*
- Affects the **sacral spinal cord segments (S3-S5)**, leading to **symmetrical motor and sensory deficits**, often with prominent early **bowel and bladder dysfunction**.
- While it causes saddle anesthesia and urinary symptoms, the **asymmetrical motor weakness** (left leg only) and **prominent radicular pain** extending down the leg are more characteristic of cauda equina syndrome.
- Conus lesions typically present with more **symmetric bilateral deficits** rather than the unilateral pattern seen here.
*Anterior spinal cord syndrome*
- Characterized by **bilateral motor paralysis** and **loss of pain and temperature sensation** below the lesion, with **preservation of proprioception and vibratory sensation**.
- It would not typically present with the isolated **saddle anesthesia** and **radicular pain** described in the patient.
*Brown-sequard syndrome*
- Results from a **hemicord lesion**, causing **ipsilateral motor paralysis** and loss of proprioception/vibration below the lesion, and **contralateral loss of pain and temperature sensation**.
- The patient's symptoms of **bilateral saddle anesthesia** and **bowel/bladder dysfunction** do not align with the characteristic unilateral sensory and motor presentation of Brown-Sequard syndrome.
Sacral dermatomes and myotomes US Medical PG Question 6: A 41-year-old woman presents with back pain for the past 2 days. She says that the pain radiates down along the posterior right thigh and leg. She says the pain started suddenly after lifting a heavy box 2 days ago. Past medical history is irrelevant. Physical examination reveals a straight leg raise (SLR) test restricted to 30°, inability to walk on her toes, decreased sensation along the lateral border of her right foot, and diminished ankle jerk on the same side. Which of the following nerve roots is most likely compressed?
- A. Fourth lumbar nerve root (L4)
- B. Second sacral nerve root (S2)
- C. Third sacral nerve root (S3)
- D. Fifth lumbar nerve root (L5)
- E. First sacral nerve root (S1) (Correct Answer)
Sacral dermatomes and myotomes Explanation: ***First sacral nerve root (S1)***
- **Inability to walk on toes** (weakness of gastrocnemius and soleus), **decreased sensation along the lateral border of the foot**, and a **diminished ankle jerk** are classic signs of S1 radiculopathy.
- The radiating pain down the posterior leg, restricted straight leg raise due to a sudden onset after lifting, points towards a **disc herniation** compressing the S1 nerve root.
*Fourth lumbar nerve root (L4)*
- Compression of L4 typically causes **weakness in knee extension** (quadriceps), diminished patellar reflex, and sensory loss over the medial aspect of the shin.
- The patient's symptoms (inability to walk on toes, diminished ankle jerk) are not consistent with L4 nerve root involvement.
*Second sacral nerve root (S2)*
- S2 radiculopathy primarily affects sensation in the posterior thigh and calf and can cause **weakness in knee flexion** and **plantarflexion**, but the complete constellation of symptoms (especially ankle jerk reflex) is more indicative of S1.
- Isolated S2 compression without S1 involvement is less common with these specific signs.
*Third sacral nerve root (S3)*
- S3 nerve root compression typically presents with **perineal numbness** and issues with bowel or bladder function due to its involvement in these functions.
- The described motor and sensory deficits are not characteristic of S3 radiculopathy.
*Fifth lumbar nerve root (L5)*
- L5 radiculopathy is characterized by **weakness in foot dorsiflexion** (foot drop) and toe extension, leading to inability to walk on heels, and sensory loss on the dorsum of the foot.
- While L5 compression can cause radiating pain and a restricted straight leg raise, the specific deficit of **inability to walk on toes** and a **diminished ankle jerk** are not typical of L5 involvement.
Sacral dermatomes and myotomes US Medical PG Question 7: One day after undergoing surgery for a traumatic right pelvic fracture, a 73-year-old man has pain over his buttocks and scrotum and urinary incontinence. Physical examination shows right-sided perineal hypesthesia and absence of anal sphincter contraction when the skin around the anus is touched. This patient is most likely to have which of the following additional neurological deficits?
- A. Impaired hip flexion
- B. Paralysis of hip adductors
- C. Absent cremasteric reflex
- D. Impaired psychogenic erection
- E. Absent reflex erection (Correct Answer)
Sacral dermatomes and myotomes Explanation: ***Absent reflex erection***
- The patient's symptoms (buttock/scrotal pain, perineal hypesthesia, urinary incontinence, absent anal sphincter contraction) suggest **damage to the sacral plexus and pudendal nerve**, consistent with a **cauda equina syndrome**.
- **Reflex erections** are primarily mediated by the **sacral parasympathetic outflow (S2-S4)**, which are likely compromised given the other sacral nerve deficits.
*Impaired hip flexion*
- **Hip flexion** is primarily controlled by the **L1-L3 nerve roots** (e.g., iliopsoas muscle), and while a severe pelvic fracture could cause widespread nerve damage, the current symptoms localize more strongly to the sacral region.
- The described symptoms are more indicative of **sacral nerve involvement** rather than higher lumbar segments that govern hip flexion.
*Paralysis of hip adductors*
- **Hip adduction** is mainly innervated by the **obturator nerve (L2-L4)**.
- The patient's symptoms point to **S2-S4 nerve dysfunction** (perineal sensation, anal sphincter, bladder), which are distinct from the obturator nerve's primary innervations.
*Absent cremasteric reflex*
- The **cremasteric reflex** is mediated by the **genitofemoral nerve (L1-L2)**.
- The symptoms presented are more consistent with **sacral nerve damage**, specifically S2-S4, rather than the higher lumbar segments responsible for the cremasteric reflex.
*Impaired psychogenic erection*
- **Psychogenic erections** are initiated by **supraspinal input** descending through the thoracolumbar spinal cord (T10-L2) to activate sympathetic pathways.
- While sacral nerve damage can affect the final efferent pathway for all erections, the direct impairment of psychogenic initiation is linked to higher centers and **thoracolumbar sympathetic outflow**, not purely sacral damage.
Sacral dermatomes and myotomes US Medical PG Question 8: A 23-year-old woman presents to the emergency department with an acute exacerbation of her 3-month history of low back and right leg pain. She says she has had similar symptoms in the past, but this time the pain was so excruciating, it took her breath away. She describes the pain as severe, shock-like, and localized to her lower back and radiating straight down the back of her right thigh and to her calf, stopping at the ankle. Her pain is worse in the morning, and, sometimes, the pain wakes her up at night with severe buttock and posterior thigh pain but walking actually makes the pain subside somewhat. The patient reports no smoking history or alcohol or drug use. She has been working casually as a waitress and does find bending over tables a strain. She is afebrile, and her vital signs are within normal limits. On physical examination, her left straight leg raise test is severely limited and reproduces her buttock pain at 20° of hip flexion. Pain is worsened by the addition of ankle dorsiflexion. The sensation is intact. Her L4 and L5 reflexes are normal, but her S1 reflex is absent on the right side. A CT of the lumbar spine shows an L5–S1 disc protrusion with right S1 nerve root compression. Which of the following muscle-nerve complexes is involved in producing an S1 reflex?
- A. Adductors-obturator nerve
- B. Gastrocnemius/soleus-tibial nerve (Correct Answer)
- C. Sartorius-femoral nerve
- D. Tibialis posterior-tibial nerve
- E. Quadriceps femoris-femoral nerve
Sacral dermatomes and myotomes Explanation: ***Gastrocnemius/soleus-tibial nerve***
- The S1 reflex (also known as the **Achilles reflex**) tests the integrity of the **S1 nerve root**.
- This reflex arc involves the **gastrocnemius and soleus muscles**, which are innervated by the **tibial nerve** (derived primarily from S1).
*Adductors-obturator nerve*
- The **adductor muscles** of the thigh are primarily innervated by the **obturator nerve** (L2-L4).
- This complex is not involved in generating the **Achilles reflex**.
*Sartorius-femoral nerve*
- The **sartorius muscle** is innervated by the **femoral nerve** (L2-L4).
- This muscle and nerve are not part of the **S1 reflex arc**.
*Tibialis posterior-tibial nerve*
- The **tibialis posterior muscle** is innervated by the **tibial nerve** (L4-S3), but its primary role is in ankle inversion and plantarflexion, not the main component of the **Achilles reflex**.
- While the tibial nerve is involved in the S1 reflex, the **gastrocnemius and soleus** are the primary muscles for this reflex.
*Quadriceps femoris-femoral nerve*
- The **quadriceps femoris muscle** is responsible for the **patellar reflex** (knee jerk reflex), which tests the integrity of the **L3-L4 nerve roots**.
- It is innervated by the **femoral nerve** and is not involved in the **S1 reflex**.
Sacral dermatomes and myotomes US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Sacral dermatomes and myotomes Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Sacral dermatomes and myotomes US Medical PG Question 10: A 6-year-old boy is brought to the physician because he has a limp for 3 weeks. He was born at term and has been healthy since. His immunization are up-to-date; he received his 5th DTaP vaccine one month ago. He is at 50th percentile for height and weight. His temperature is 37°C (98.6°F), pulse is 80/min and respirations are 28/min. When asked to stand only on his right leg, the left pelvis sags. The remainder of the examination shows no abnormalities. Which of the following is the most likely cause of these findings?
- A. L5 radiculopathy
- B. Damage to the right common peroneal nerve
- C. Damage to the left inferior gluteal nerve
- D. Spinal abscess
- E. Damage to the right superior gluteal nerve (Correct Answer)
Sacral dermatomes and myotomes Explanation: ***Damage to the right superior gluteal nerve***
- The patient exhibits a **positive Trendelenburg sign**, where the pelvis drops on the unsupported side (left side) when standing on the affected leg (right side). This indicates weakness of the **contralateral gluteus medius and minimus muscles**, which are innervated by the superior gluteal nerve.
- Therefore, damage to the **right superior gluteal nerve** would lead to weakness of the right gluteus medius and minimus, causing the left pelvis to sag when standing on the right leg.
*L5 radiculopathy*
- L5 radiculopathy would primarily affect muscles innervated by the L5 nerve root, including the **tibialis anterior** (foot dorsiflexion) and **extensor hallucis longus**, which would present differently (e.g., foot drop) rather than isolated gluteal weakness.
- While the gluteus medius and minimus receive some innervation from L5, isolated L5 radiculopathy is less likely to cause a pure Trendelenburg gait without other significant neurological deficits.
*Damage to the right common peroneal nerve*
- Damage to the common peroneal nerve primarily affects muscles of the **anterior and lateral compartments of the leg**, leading to **foot drop** and sensory loss over the dorsum of the foot.
- It does not directly innervate the gluteal muscles and therefore would not cause a Trendelenburg gait.
*Damage to the left inferior gluteal nerve*
- The inferior gluteal nerve innervates the **gluteus maximus**, which is responsible for hip extension.
- Damage to the left inferior gluteal nerve would cause weakness in hip extension on the left side, not the characteristic pelvic drop seen with the Trendelenburg sign (which involves the gluteus medius/minimus).
*Spinal abscess*
- A spinal abscess would typically present with severe back pain, fever, neurological deficits such as motor weakness or sensory loss, and possibly bladder/bowel dysfunction.
- While it can cause weakness, it would usually be accompanied by systemic symptoms and more diffuse neurological signs, which are absent in this case.
More Sacral dermatomes and myotomes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.